Abstract
Background
Esophageal perforations historically are associated with significant morbidity and mortality and generally require emergent intervention. The influence of improved diagnostic and therapeutic modalities available in recent years on management has not been examined. This study examined the surgical treatments and outcomes of a modern cohort.
Methods
Patients with esophageal perforation management in the 2005-2020 American College of Surgeons National Surgical Quality Improvement Program database were stratified into three eras (2005-2009, 2010-2014, and 2015-2020). Surgical management was classified as primary repair, resection, diversion, or drainage alone based on procedure codes. The distribution of procedure use, morbidity, and mortality across eras was examined.
Results
Surgical management of 378 identified patients was primary repair (n=193,51%), drainage (n=89,24%), resection (n=70,18%), and diversion (n=26,7%). Thirty-day mortality in the cohort was 9.5% (n=36/378) and 268 patients (71%) had at least one complication. The median length of stay was 15 days. Both morbidity (Era 1 65% [n=42/60] versus Era 2 69% [n=92/131] versus Era 3 72% [n=135/187], p=0.3) and mortality (Era 1 11% [n=7/65] versus Era 2 9% [n=12/131] versus Era 3 10% [n=19/187], p=0.9) did not change significantly over the three defined eras. Treatment over time evolved such that primary repair was more frequently utilized (43% in Era 1 to 51% in Era 3) while diversion was less often performed (13% in Era 1 to 7% in Era 3) (p=0.009).
Conclusions
Esophageal perforation management in recent years uses diversion less often but remains associated with significant morbidity and mortality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Esophageal perforations that occur spontaneously from increased intra-esophageal pressure or due to iatrogenic injury, foreign body ingestion, or trauma are associated with high morbidity and mortality.1, 2 Clinical presentations vary with location of injury and time to presentation, and can range from neck pain, dysphagia, and dysphonia with proximal perforations to chest pain, abdominal pain, or frank sepsis with intra-thoracic and intra-abdominal perforations. Prompt diagnosis is key to good prognosis as any delay to treatment is associated with worse outcomes.2, 3 Outcomes historically were dismal at 40-60% mortality but improved to 18% mortality in a series of patients from 1990-2003 and more recently have been reported as low as 7-10% in a study of patients from 2010-2015.1,2,3,4,5
Historically, the gold standard of treatment has been emergent invasive surgery with repair, drainage, or esophageal diversion.6,7,8 Presentations like septic shock, respiratory failure, and extensive mediastinal emphysema simplify the decision-making process as patients are appropriately shunted towards emergent surgical management. On the other hand, patients with contained perforations who are clinically stable present an opportunity for or less invasive or even nonoperative management such a conservative approach including nothing by mouth, broad spectrum antibiotics, esophageal stenting, and minimally invasive drainage procedures.9,10,11
Evidence to guide esophageal perforation management is generally limited to relatively small retrospective reviews, given that single centers typically see only a few patients annually as well as the difficulty in evaluating management in a randomized control trial given the urgency and variability of clinical presentation.12, 13 Clinicians often rely on their own clinical intuition and experience on how to best manage patients. The primary aim of this study was to use a modern cohort from a diverse collection of institutions and surgeons to examine the trend of surgical management and outcomes of esophageal perforation over the last fifteen years. We hypothesize that the morbidity and mortality of surgery for esophageal perforation has improved over time, even when including lower volume centers into the analysis, due to advancements in surgical technology and techniques.
Patients and Methods
Data Source
The American College of Surgeons National Quality Surgical Improvement (ACS-NSQIP) database captures patient demographics, comorbidities, lab values, and procedures to study 30-day surgical morbidity and mortality. NSQIP collects these specified variables on patients using random sampling to provide an overarching hospital-level quality assessment, which limits data analysis and introduces potential biases. Nevertheless, studies have shown that the database does significantly improve surgical outcomes and decrease costs among participating hospitals. As all Participant Use Data Files are de-identified, this study was considered exempt by the Stanford University Institutional Review Board.
Patient Selection and Management Characterization
In this study, all patients over the age of 18 diagnosed with emergent esophageal perforation in the 2005-2020 ACS-NSQIP database were identified using ICD 9 and 10 codes 530.4 and K22.3. Patients were assigned to a categorical treatment group based on surgical management: primary repair, resection, diversion, or drainage. This was performed in a hierarchical fashion using Current Procedural Terminology codes (Supplemental table 1). Patients were assigned to the primary repair category if they had a CPT code specifically related to primary repair, while resection, diversion, and drainage patients, respectively, had CPTs specifically related to those procedures. Resection included CPT codes with procedures such as partial or total removal of the esophagus or stomach. Diversion included procedures such as esophagostomy or external fistulization of the esophagus, ligation of the esophagus, or surgical opening of the throat. Drainage included procedures such as chest tube placement, thoracotomy and washout, video assisted thoracoscopic surgery and washout, and chest exploration. Patients presenting in an elective setting were excluded. Patients over the age of 90 were excluded due to their categorization as a special population.
Specific patient characteristics including pre-operative demographics and comorbidities such as smoking status, diabetes, cardiopulmonary disease, and renal dysfunction were tabulated and compared across the four treatment strategies. Peri-operative and thirty-day post-operative outcomes such as operation time, length of hospital stay, readmission rate, and complications were also categorized and compared based on management strategy. Thirty-day morbidity and mortality were calculated for both entire cohort as well as for each management strategy.
Treatment over Time
The stratification of different eras in the overall study period was based on both literature reports of esophageal perforation management as well as by the authors’ clinical experience, including our observations of the integration of esophageal stents more routinely into practice. Using these criteria, patients were stratified into three different treatment eras: Era 1 from 2005-2009; Era 2 from 2010-2014; and Era 3 from 2015-2020. The distribution of procedures across these eras was plotted to allow for qualitative assessment in management changes and the Cochrane Armitage trend test was used to evaluate for statistically significant changes over time. Morbidity and mortality across those eras were similarly evaluated and compared for significant changes, and we compared changes in management strategy across eras via Cochrane Armitage tests.
Predictors of Management Strategy and Outcomes
Logistic regression was performed to evaluate predictors of therapy, to allow insight on how patient and clinical variables influenced treatment selection. This model included procedure-type as the outcome (primary repair [historical gold-standard] versus the rest), and included patient age, sex, race, body mass index (BMI), American Society of Anesthesiologists (ASA) classification, chronic obstructive pulmonary disease (COPD), heart failure, steroid use, diabetes, and smoking status as potential predictors. Era was included to test our primary hypothesis that management significantly changed over time. In addition, predictors of complications and death were similarly evaluated with logistic regression, to assess if certain characteristics in each group are associated with poor outcomes. We used management strategy as the outcome and used drainage as the reference group to determine if certain management strategies were more likely to face postoperative complications. We assessed the presence of a trend across in rates of morbidity and mortality for each procedure type.
Statistical Analysis
All statistical tests were 2-sided with an α value of 0.05. Analyses were performed using R version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient Cohort and Treatment
Overall, 378 patients met the inclusion criteria and were included in the analysis. Preoperative characteristics are described in Table 1. The median age was 60 (48, 71), 30% of the cohort was female, and the majority were obese and of white ethnicity. The majority of patients (51.1%, n=193) underwent primary repair, while there were 26 (6.9%) patients managed with diversion, 89 (23.5%) managed with drainage, and 70 (18.5%) managed with resection. The risk factor profiles across the four groups were similar; but the diversion patients were better surgical candidates, while the resection patients were worse surgical candidates (p=0.002). Table 2 is logistic regression performed and shows that history of COPD was the only statistically significant predictor for primary repair. Otherwise, there were no statistically significant associations between preoperative characteristics and management strategy chosen.
Patient Outcomes
Table 3 shows perioperative and postoperative outcomes for the entire cohort as well as stratified by management strategy. Median length of stay (LOS) for the entire cohort was 15 days. The resection group had the longest LOS at 20.5 days and the longest operative duration (262 minutes) (p<0.001). Overall, 254 patients (71%) had at least one complication. The resection group had the highest rate of postoperative complications, including surgical site infection, pneumonia, unplanned intubation or failure to wean from the ventilator, deep venous thrombosis, pulmonary embolism, and cardiac arrest.
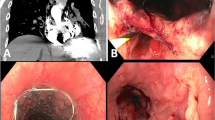
Figure 1 shows that drainage had the highest mortality rate and resection had the highest morbidity rate, but the observed differences were not statistically significant. Thirty-day mortality was 9.5% (n=36) and thirty-day morbidity was 71% (n=268) across all four groups with no significant difference between management strategies. Return to OR was the highest in the resection group at 43% and lowest in the drainage group at 19%. Readmission rates were 5.2% overall, highest in the resection group and lowest in the diversion group.
Multivariable logistic regression was used to determine if certain types of procedures are more likely to have complications, using drainage as a reference group. Table 4 shows that resection patients had a higher odds of experiencing complications compared to drainage patients OR=3.05 (95% CI: [1.41 – 7.09], p =.006). However, there were no significant differences between diversion OR=0.81 (95% [CI 0.33 – 2.06]) p= 0.655 or primary repair OR = 1.13 (95% CI [0.66 – 1.92]), p= 0.661 when compared to drainage. We also examined the rate of death within 30 days using logistic regression, but found no significant differences of diversion, primary repair, or resection when compared to drainage.
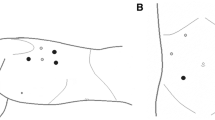
Management over Time
Figure 2 shows the distribution of management strategies over the three defined eras. Cochrane armitage trend test revealed that treatment overtime evolved such that primary repair was more frequently utilized while diversion was less often performed (p=0.009). There was no significant difference in utilization of drainage compared to primary repair (p= 0.244) nor resection vs primary repair (p= 0.91). Figure 3 demonstrates that both morbidity (Era 1 65% [n=42/60] versus Era 2 69% [n=92/131] versus Era 3 72% [n=135/187], p=0.3) and mortality (Era1 11% [n=7/65] versus Era 29% [n=12/131] versus Era 3 10% [n=19/187], p=0.9) did not significantly change over the three defined eras. Lastly, Figure 4 aggregates the data and shows that mortality in Era 1 was highest in the primary repair group, while in Era 2 and 3, mortality was highest in the drainage group. Morbidity in all eras was highest in the resection group.
Outcomes of management over time across eras
We performed Cochrane Armitage tests to assess how rates of morbidity and mortality varied for each procedure across eras. For morbidity we failed to observe statistically significant changes across eras in the rates of morbidity for primary repair (p= 0.881), drainage (p= 0.176), diversion (p= 0.744), or resection (p=0.0665). Similarly, for mortality we failed to observe statistically significant changes in primary repair (p= 0.122), resection (p= 0.212), drainage (p= 0.887), and diversion (p= 0.37).
Discussion
This study analyzed emergent surgical management of esophageal perforation from 2005 to 2020 using the ACS-NSQIP database, providing a review of contemporary management in a time period with changing clinical practices. Among a cohort of 378 patients, we found that primary repair was increasingly utilized and diversion decreasingly utilized in treatment for esophageal perforation over the time period of the study. As shown in our study, all techniques utilized to manage esophageal perforation continue to be associated with long hospital stays and significant morbidity and mortality in a recent period, with minor improvements over a 15-year period contributed as much by better perioperative care as by advancements in medical technology.
Currently, existing literature on esophageal perforation management agree on the overall approach to initial management of esophageal perforation, including fluid resuscitation, nil per os, and antibiotics to minimize the systemic spread of infection.14,15,16 Figure 1A demonstrates that drainage has a much higher mortality rate than other surgical options. This should serve as an important reminder that simple drainage is not effective in the management of this complicated disease process. Drainage should be treated as an adjunctive treatment, rather than a complete solution to esophageal perforation and methods to obtain source control in a more definitive way is key to improving outcomes.
Primary repair has traditionally been the ‘gold standard’ of treatment, and Fig. 2 shows the temporal increase in primary repair over time. Although the trends of morbidity and mortality rates across eras were not statistically significant upon further analysis, this study was underpowered to detect such a change. Nevertheless, the encouraging decrease in mortality rates from primary repair as shown in Fig. 4A are likely due to better perioperative care and major advancements in evidence-based critical care medicine; and these improved outcomes have influenced the general mortality trends as shown in Fig. 3A. However, patients can still develop grave complications like leaks if their initial presentation includes extensive necrosis and edema, precluding healthy esophageal tissue for a durable primary repair.17,18,19 The leak rate after primary repair has been cited to be as high as 30-40%, with many patients needing a secondary drainage procedure to control subsequent contamination.20, 21 When patients cannot have or fail a primary repair, the alternative options of drainage, diversion, or resection are all associated with both morbidity and long recoveries.1, 3, 17 Patients who need resections or diversions have historically been sicker and more comorbid, and this observation has persisted throughout the eras as seen in Fig. 3B and Fig. 4B.
The advancement of biomedical technology allowing the development of self-expanding stents has provided a new tool that can be used to manage esophageal perforations.11, 22, 23 The availability of stents may explain the increasing rate of primary repair overtime as surgeons may have been more aggressive in attempting repair when knowing that postoperative stenting could be an option if a continued esophageal leak was subsequently found. Stenting availability could also at least partly explain the decreased use of diversion as seen in Fig. 2, as another less drastic method to decrease mediastinal soilage is now available. However, the study’s findings also suggest that patients are having multiple procedures for their management, and that patient care could be more efficient if stents were placed in the operating room at the time of surgical management by surgeons. The clinical ramifications of this study are to highlight the importance of adapting management strategies based on individual presentation.
The major limitation of this study includes the lack of data on the number of patients stented overall and in each era; thus we were unable to correlate stent use with different surgical procedures received and therefore evaluate the direct impact of stent availability and use on management and outcomes. Moreover, we acknowledge that the availability of stents may have led to a selection bias where patients with more extensive perforations or complicated clinical scenarios were more likely to get surgery, such that the cohort of surgical patients in a more modern cohort were perhaps more high risk for morbidity because lower risk patients underwent endoscopic management rather than surgery. Subsequently, our results are not generalizable across the new spectrum of esophageal perforation management, but only those who ultimately undergo surgical intervention. Another limitation is the lack of granular data on several important predictors of outcomes, which are the location of perforation, the timing of intervention relative to the injury, and specific details on the work-up and management performed prior to surgery as well as the specifics regarding any additional procedures performed after the primary surgery, which limited our ability to conduct subgroup analyses and account for confounding factors. Lastly, we realize that only having 30-day postoperative data may miss episodes of major morbidity or death in esophageal perforation patients.
Conclusion
Our findings, amassed from a relatively large cohort, provide an important snapshot in time on the management of esophageal perforation in the United States over the last fifteen years. The focus on temporal trends is novel and pertinent in a diagnosis that is experiencing ongoing changing practices. This disease process has historically been difficult to study due to the generally low incidence at single centers and its emergent nature that limit controlled studies, and our study aims to add evidence to support individualized treatment decisions in an area that has largely been experience-based. To this date, there are no randomized controlled trials comparing outcomes from various surgical approaches or esophageal stenting, and the nature of the condition and the management procedures required make it extremely unlikely those would ever be done. Our findings show that esophageal perforation still has poor overall outcomes even in a modern era. However, a bright side of our study is the finding that diversion use is decreasing, which is very likely at least improving patients’ quality of life in addition to decreasing the need for subsequent procedures such as restoring gastrointestinal continuity. These results strongly suggest surgeons must be actively involved early and throughout the treatment decision process even when non-operative therapy is possible, and that management across institutions should be as standardized as possible to ensure the availability of both surgery and stenting to all patients.
References
Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004 77(4):1475-83. https://doi.org/10.1016/j.athoracsur.2003.08.037.
Lampridis S, Mitsos S, Hayward M, Lawrence D, Panagiotopoulos N. The insidious presentation and challenging management of esophageal perforation following diagnostic and therapeutic interventions. J Thorac Dis. 2020 12(5):2724-2734. https://doi.org/10.21037/jtd-19-4096.
Nesbitt JC, Sawyers JL. Surgical management of esophageal perforation . Am Surg. 1987;53:183-191.
Cameron JL, Kieffer RF, Hendrix TR, Mehigan DG, Baker RR. Selective nonoperative management of contained intratho-racic esophageal disruptions. Ann Thorac Surg 1979;27:404-8.
Sohda M, Kuwano H, Sakai M, Miyazaki T, Kakeji Y, Toh Y, Matsubara H. A national survey on esophageal perforation: study of cases at accredited institutions by the Japanese Esophagus Society. Esophagus. 2020 17(3):230-238. https://doi.org/10.1007/s10388-020-00744-7. Epub 2020 May 15.
Skinner DB, Little AG, DeMeester TR. Management of esophageal perforation . Am J Surg. 1980;139:760-764.
Freeman RK, Ascioti AJ, Giannini T, Mahidhara RJ. Analysis of unsuccessful esophageal stent placements for esophageal perforation, fistula, or anastomotic leak. Ann Thorac Surg. 2012; 94(3):959-64; https://doi.org/10.1016/j.athoracsur.2012.05.047.
Raff LA, Schinnerer EA, Maine RG, Jansen J, Noorbakhsh MR, Spigel Z, Campion E, Coleman J, Saquib S, Carroll JT, Jacobson LE, Williams J, Young AJ, Pascual J, Burruss S, Gordon D, Robinson BRH, Nahmias J, Kutcher ME, Bugaev N, Jeyamurugan K, Bosarge P. Contemporary management of traumatic cervical and thoracic esophageal perforation: The results of an Eastern Association for the Surgery of Trauma multi-institutional study. J Trauma Acute Care Surg. 2020 89(4):691-697. https://doi.org/10.1097/TA.0000000000002841.
Sdralis EIK, Petousis S, Rashid F, Lorenzi B, Charalabopoulos A. Epidemiology, diagnosis, and management of esophageal perforations: systematic review. Dis Esophagus. 2017;30(8):1-6. https://doi.org/10.1093/dote/dox013.
Herrera A, Freeman RK. The Evolution and Current Utility of Esophageal Stent Placement for the Treatment of Acute Esophageal Perforation. Thorac Surg Clin. 2016 26(3):305-14
Thornblade LW, Cheng AM, Wood DE, et al. A Nationwide Rise in the Use of Stents for Benign Esophageal Perforation. Ann Thorac Surg. 2017;104(1):227-233.
David EA, Kim MP, Blackmon SH.Esophageal salvage with removable covered self-expanding metal stents in the setting of intrathoracic esophageal leakage. Am J Surg. 2011 202(6):796-801
Dickinson KJ, Buttar N, Wong Kee Song LM, Gostout CJ, Cassivi SD, Allen MS, Nichols FC, Shen KR, Wigle DA, Blackmon SH.Utility of endoscopic therapy in the management of Boerhaave syndrome. Endosc Int Open. 2016 4(11):E1146-E1150
Eroglu A, Turkyilmaz A, Aydin Y, Yekeler E, Karaoglanoglu N. Current management of esophageal perforation: 20 years experience. Dis Esophagus. 2009;22(4):374-380.
Ceppa DP, Rosati CM, Chabtini L, et al. Development of a Multidisciplinary Program to Expedite Care of Esophageal Emergencies. Ann Thorac Surg. 2017;104(3):1054-1061.
Connelly CL, Lamb PJ, Paterson-Brown S. Outcomes following Boerhaave's syndrome. Ann R Coll Surg Engl. 2013;95(8):557-560.
Axtell AL, Gaissert HA, Morse CR, Premkumar A, Schumacher L, Muniappan A, Ott H, Allan JS, Lanuti M, Mathisen DJ, Wright CD. Management and outcomes of esophageal perforation. Dis Esophagus. 2022. https://doi.org/10.1093/dote/doab039.
Amir AI, van Dullemen H, Plukker JT. Selective approach in the treatment of esophageal perforations. Scand J Gastroenterol. 2004;39(5):418-422.
Huu Vinh V, Viet Dang Quang N, Van Khoi N. Surgical management of esophageal perforation: role of primary closure. Asian Cardiovasc Thorac Ann. 2019;27(3):192-198. https://doi.org/10.1177/0218492319827439. Epub 2019 Jan 21.
Muir AD, White J, McGuigan JA, McManus KG, Graham AN. Treatment and outcomes of oesophageal perforation in a tertiary referral centre. Eur J Cardiothorac Surg. 2003;23(5):799-804; discussion 804.
Markar SR, Mackenzie H, Wiggins T, et al. Management and Outcomes of Esophageal Perforation: A National Study of 2,564 Patients in England. Am J Gastroenterol. 2015;110(11):1559-1566.
Horwitz B, Krevsky B, Buckman RF, Fisher RS, Dabezies MA. Endoscopic evaluation of penetrating esophageal injuries. Am J Gastroenterol. 1993;88(8):1249-1253.
Sudarshan M, Elharram M, Spicer J, Mulder D, Ferri LE. Management of esophageal perforation in the endoscopic era: Is operative repair still relevant? Surgery. 2016;160(4):1104-1110.
Acknowledgments
American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors have no conflicts of interest or funding sources related to this manuscript. All listed authors contributed substantially to the design, drafting, approval, and accountability of this work. Word count: 4,737
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This project has been presented as a poster at the General Thoracic Surgical Club’s 34th Annual Meeting, Bonita Springs, FL, March 10-13, 2022
Supplementary information
ESM 1
(DOCX 13 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wong, LY., Leipzig, M., Liou, D.Z. et al. Surgical Management of Esophageal Perforation: Examining Trends in a Multi-Institutional Cohort. J Gastrointest Surg 27, 1757–1765 (2023). https://doi.org/10.1007/s11605-023-05700-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05700-1