Abstract
Background
Open surgical resection with regional lymphadenectomy is the standard of care for small bowel neuroendocrine tumors (SBNETs). There is no consensus on the role of minimally invasive surgery (MIS). This study aims to evaluate the current national trends for MIS in treating SBNETs and its association with lymph node (LN) yield.
Methods
The National Cancer Database was queried for patients with Stage I-III SBNETs who underwent surgery from 2010–2017. Time trends were examined using the Cochran–Armitage test. Chi-square tests, t test, and multivariable logistic regression assessed associations of surgical approach with patient, clinical, and facility characteristics. Kaplan–Meier curves and propensity score weighted Cox proportional hazards model were used to examine survival.
Results
Of the 11,367 patients with Stage I-III SBNETs, 46.5% (N = 5,298) underwent MIS. From 2010–2017, the proportion of MIS increased from 35.6% to 57.7% (P < 0.001). Patients of Stage I disease (OR = 1.23), Caucasian race (OR = 1.18), private insurance (OR = 1.29), and higher volume centers (OR = 1.29) were more likely to undergo MIS (all P < 0.02). The average number of LN harvested in the MIS cohort was greater than in the open surgery cohort (13.3 vs 11.8 LN, P < 0.001). MIS patients had shorter length of stay by 2 days compared to open surgery (5.4 vs 7.6 days, P < 0.001). LN yield ≥ 8 was associated with better survival (HR = 0.77, P < 0.001).
Conclusion
The utilization of a MIS approach to treat Stage I-III SBNETs has increased, especially at higher volume centers. We did not observe an inferior LN harvest with the MIS cohort compared to the open surgery cohort.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Small bowel neuroendocrine tumors (SBNETs) are the most common small bowel cancer in the USA, and its prevalence and incidence continue to rise.1,2 The initial treatment for locoregional disease in the jejunum or ileum is segmental small bowel resection of the mass with regional lymphadenectomy, which has been more commonly performed under an open approach.3,4,5 A minimally invasive surgery (MIS) approach via laparoscopy continues to be controversial due to concern for inadequate examination for multi-focal and occult sub-centimeter tumors or for lymph node (LN) metastases (which are thought to be more easily detected by manual palpation), and technical difficulties of performing oncologically appropriate and safe resection of masses near the mesenteric root.4,5,6,7 The indolent nature and the rarity of SBNETs (12 cases per 100,000) have been a major barrier in conducting randomized controlled trials on optimal surgical management for this disease.8 Previous studies have reported positive short-term clinical outcomes with laparoscopic resection of SBNETs (and even occult disease) and concluded that there is a role for laparoscopy.7,9,10,11,12,13 However, data are limited to small, single institutional studies with small sample sizes and relatively short follow-up times.
With a large national cancer database, the primary aims of this study were to identify factors associated with the MIS approach to SBNET resection and lymphadenectomy and to examine the association between surgical approach and LN yield. The secondary aims were to determine the national trends of the surgical approaches to SBNETs and evaluate clinical outcomes for the two surgical approaches. We hypothesized that the utilization of MIS for SBNET resection and lymphadenectomy has increased over time and LN harvest as well as short-term surgical outcomes would be non-inferior in patients with Stage I-III SBNET undergoing the MIS approach when compared to the open surgery option.
Methods
Data Source
This retrospective cohort study used the National Cancer Database (NCDB), a national collaboration sponsored by the American Cancer Society and the American College of Surgeons. The NCDB captures about 70% of all new cancer diagnoses in the USA.14 Patient data and data definitions are collected from Commission on Cancer accredited facilities to create this clinical oncology database. The study was exempt from institutional review board approval by the Human Subject Protection Office at the Penn State College of Medicine as all patient information in the NCDB is de-identified.
Case Selection Criteria
The NCDB was queried for non-duodenal SBNETs from 2010 to 2017 using the PUF 2017 data dictionary. International Classification of Disease site [ICD] topography codes analyzed included: C17.1, C17.2, C17.3, C17.8, C17.9. Histology codes analyzed included: 8240–8242, 8246, 8249. Duodenal tumors (C17.0) were excluded secondary to having more complex and different presentation and treatment strategies than jejunoileal SBNETs. Additional inclusion criteria involved patients diagnosed with pathological Stage I (T1N0M0), Stage II (T2-3N0M0), and Stage III (T4N0M0 or TxN1-2M0) SBNETs who underwent surgical resection of the primary tumor site. Staging was determined based on the American Joint Committee on Cancer (AJCC) Staging Manual, seventh edition. Patients with unknown staging status, and missing sociodemographic status (age, insurance status, facility type, facility location, distance traveled to hospital, and urban–rural status) were excluded. Stage IV disease, which may require more extensive resection and surgical cytoreduction of metastatic lesions, was excluded to avoid potential palliative cases. The cohort was divided between patients who underwent minimally invasive surgery (laparoscopic and robotic assisted) and patients who underwent open surgery (Fig. 1). Cases that reported conversion from MIS to open surgery were included in the MIS cohort for intention to treat trend analysis but converted cases were included in the open cohort in the other statistical analyses on associations and perioperative outcomes.
Factors Considered
Patient demographics and characteristics analyzed included age, sex, race, insurance status, median household income status, percentage with no high school degree within area of residence, Charlson–Deyo Comorbidity Index (CDCI),15 and metropolitan/rural status. Facility-related characteristics included distance traveled to treatment facility from home zip code, facility type (academic, comprehensive community, and community), and facility case volume (< 50th percentile vs ≥ 50th percentile). Tumor characteristics included primary tumor site location, histologic grade (well, moderately, poorly differentiated, unknown), tumor size (< 1 cm, 1–2 cm, > 2 cm), AJCC staging category, and surgical margin status. Surgical outcomes included number of LNs resected, length of hospital stay after surgery, unplanned 30-day readmission from initial operation, and 90-day mortality after initial operation. A binary variable for optimal lymph node yield (≥ 8 lymph nodes) was based on previous literature on the minimum of lymph nodes needed to identify node positive patients.16
Statistical Analysis
Patient characteristics, treatment facility features, and tumor characteristics were stratified by surgical approach. A Chi-square test was performed to examine the subgroup differences. Cochran–Armitage test was used to analyze trends of both surgical approaches over time. The trend in cases requiring conversion from MIS to open surgery over the same study period was evaluated separately. Multivariable logistic regression analysis was used to evaluate the likelihood of undergoing MIS based on factors mentioned above. Additional logistic regression analysis on surgical outcomes after propensity score weighting was performed. Propensity score, adjusting for age, sex, race, insurance status, median household income, high school education, facility cancer program type, facility surgical case volume, distance traveled to hospital, urban–rural status, CDCI, stage group, was estimated from prior multivariable logistic regression. Overall survival (OS) rates were estimated using Kaplan–Meier method using log-rank test. Multivariable survival analysis was performed using Cox proportional hazard model with inverse probability of treatment weight based on propensity score. Sensitivity analysis for logistic regression and Cox proportional hazard model excluded patients who required readmission within 30 days from initial operation or who died within 90 days of initial operation. All statistical tests were two-sided and alpha was set at a significance level of 0.05. All analyses were conducted using SAS statistical software (version 9.4).
Results
Univariate Analysis
A total of 11,367 patients with Stage I-III non-duodenal SBNETs who underwent surgical intervention from 2010 to 2017 were captured in the NCDB. Of these patients, 38.3% (N = 4,356) underwent MIS only, 53.4% (N = 6,078) underwent open surgery only, and 8.2% (N = 933) had a conversion from MIS to open surgery. The total case volume increased by 17.0% between 2010 and 2017. Attempted minimally invasive cases increased by 90.0% over the same study period (p < 0.001). When compared to an open surgical approach, the proportion of MIS significantly increased from 35.6% in 2010 to 57.7% in 2017, and became the larger annual proportion of total cases by 2016 (51.2% vs. 48.8%, P < 0.001). From 2010–2017, 8.2% (N = 933) reported a surgery requiring conversion from MIS to open. Under an intention to treat analysis, the conversion rate was calculated to be 17.7% (N = 933/5,289). The percentage of cases requiring conversion remained stable from 2010 to 2017 (p = 0.491). (Fig. 2).
Table 1 summarizes all patient demographics and disease characteristics stratified by surgical procedure. Regardless of surgical approach utilized, the majority of patients were white non-Hispanic, received care in facilities with case volume ≥ 50th percentile, traveled < 50 miles to the hospital, resided in metropolitan areas, and had one or no comorbidities. Facilities with SBNET case volumes ≥ 50th percentile performed a median of 27 cases (IQR: 17–47) from 2010–2017, while facilities with case volumes < 50th percentile performed a median of 5 cases (IQR: 4–7) cases from 2010–2017 (p < 0.001). The majority of SBNET cases for both techniques had well-differentiated histology, Stage III disease, and negative surgical margin status. The majority of the final cohort had lymph nodes examined but the open surgery subgroup had more cases with no LN harvested compared to the MIS subgroup (12.8% vs. 10.3%, p < 0.001). The median number of LNs examined was greater in the MIS cohort (13 LNs [IQR 5, 19]) than in the open surgery cohort (10 LNs [IQR 3, 17]) (p < 0.001). The median length of hospital stay was 2 days shorter for the MIS cohort (4 days [IQR 3, 6]) compared to the open surgery cohort (6 days [IQR 4, 8]) (p < 0.001). Unplanned 30-day re-admission (5.5% for open vs 4.2% for MIS, p = 0.002) and 90-day mortality (4.6% for open vs 1.6% for MIS, p < 0.001) were low for both subgroups.
Multivariable Logistic Regression Analysis
Patients were more likely to undergo a MIS approach for SBNET resection and lymphadenectomy if they were < 56 years old (OR 1.20, 95% CI 1.080–1.34), female (OR 1.27, 95% CI 1.18–1.37), have private insurance (OR 1.29, 95% CI 1.14–1.45) when compared to patients ≥ 56 years old, male, and have government-issued insurance. Black patients (OR 0.84, 95% CI 0.74–0.95), uninsured patients (OR 0.56, 95% CI 0.41–0.77), and patients receiving care at community cancer programs (OR 0.71, 95% 0.59–0.84) were less likely to receive MIS when compared to white non-Hispanic patients, patients on a government-issued insurance, and patients at academic centers (all P < 0.05). Patients receiving care at facilities with SBNET surgical case volume ≥ 50th percentile (OR 1.29, 95% CI 1.11–1.49) and facilities < 50 miles away (OR 1.31, 95% CI 1.12–1.53) were more likely to receive MIS when compared to patients at facilities with case volume < 50th percentile and facilities ≥ 50 miles away (all P < 0.001). Patients with ≤ 1 comorbidity (OR 1.17, 95% CI 1.01–1.36) and Stage I disease (OR 1.23, 95% CI 1.07–1.41) were more likely to receive MIS when compared to patients with multiple comorbidities or Stage III disease (all P < 0.05). (Table 2).
Patients who underwent MIS were more likely to have had ≥ 8 LNs examined when compared to patients in the open surgery cohort (OR 1.34, 95% CI 1.22–1.48). Patients treated at facilities of higher case volume ≥ 50th percentile were more likely to have ≥ 8 lymph nodes examined when compared to patients in the open surgery cohort (OR 1.30, 95% CI 1.13–1.49). Finally, patients with Stage III SBNETs were also more likely to have had ≥ 8 lymph nodes examined when compared to patients with Stage II disease (OR 3.86, 95% CI 3.42–4.31) (Table 3).
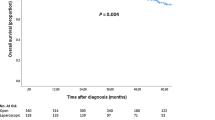
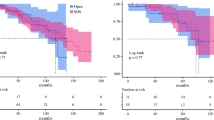
Kaplan–Meier Analysis of Overall Survival
In both the open surgery cohort and MIS cohort, overall survival was noted to be significantly better for patients with LN yield ≥ 8 LNs compare to patients with < 8 LNs (all p < 0.001) (Fig. 3A, Fig. 3B). In the open surgery cohort, five-year OS rates for LN yield ≥ 8 and LN yield < 8 in the open surgery cohort were 81.0% and 74.0%, respectively. In the MIS cohort, five-year OS rates were 89.7% with LN yield ≥ 8 and 82.2% with LN yield < 8.
Kaplan–Meier Analysis of overall survival (OS) for Stage I-III small bowel neuroendocrine tumors. A In the open surgery cohort, five-year OS for LN yield ≥ 8 and LN yield < 8 (81.0% and 74.0%, respectively). B In the minimally invasive surgery cohort, five-year OS for LN yield ≥ 8 and LN yield < 8 (89.7% and 82.2%, respectively)
Multivariable Cox Proportion Hazards Model Analysis
Patients with Stage I-III SBNETs who had LN yield ≥ 8 were associated with better overall survival than patients with LN yield < 8 (HR 0.77, 95% CI 0.68–0.87). Additional factors associated with better overall survival in patients undergoing surgery for SBNETs included younger age (< 56 years old), female gender, white non-Hispanic race, private insurance, metropolitan setting, existence of ≤ 1 comorbidity, and negative surgical margin status (all P < 0.05). (Table 4).
An additional surgical outcomes analysis demonstrated that patients who underwent MIS were less likely to have an unplanned readmission within 30 days of surgical discharge than patients who underwent an open procedure (OR 0.48, 95% CI 0.34–0.68, P < 0.001). In addition, cases that reported positive surgical margin status after the initial procedure were less likely associated with the MIS approach than cases that involved open approach (OR 0.65, 95% CI 0.57–0.74, P < 0.001).
Sensitivity Analysis
A sensitivity analysis was conducted that excluded patients who had unplanned 30-day readmission and died within 90 days of discharge (N = 683 in open cohorts excluded, N = 245 in MIS cohort excluded) as a proxy for non-elective, acute care surgery cases. This analysis demonstrated that the MIS cohort was still more likely to obtain at least 8 LNs for examination when compared to the open surgery cohort (OR 1.45, 95% CI 1.30–1.60, P < 0.001).
Discussion
This study provides the first large database analysis on the utilization of minimally invasive surgery (MIS) in the management of Stage I-III SBNETs. Our study identified a rising utilization of a minimally invasive approach for SBNET resection with regional lymphadenectomy. In addition, our study demonstrated that a MIS approach is associated with greater LN harvest compared to an open approach. The results of our study demonstrate that the preference of a surgical approach is multifactorial, with differences in patient characteristics, socioeconomic status, and hospital characteristics, which may highlight targets in quality improvement for patients with resectable SBNETs, especially as a MIS approach is associated with improved short-term outcomes without compromising lymph node harvest.
The standard surgical approach for SBNET resection and lymphadenectomy is an open surgical approach. Current North American and European SBNET guidelines acknowledge the controversial role of MIS for SBNETs and question whether MIS can adhere to the universal principles of surgical oncology including complete resection of the primary tumor, mesenteric masses, and nodal disease to complete staging as well as an adequate evaluation of abdominal organs and peritoneum.4,5 This is particularly essential for a disease that typically presents with a high rate (> 80%) of regional lymph node metastasis4 and a high 5-year recurrence rate (33%)17 after open surgery. In addition, with high rates of multifocal disease and sub-centimeter tumor sizes, it is recommended to conduct an exploratory laparotomy and digital palpation of the entire jejunum and ileum.4
The primary concern of a MIS approach is a reliance on visualization of occult lesions without accurate tactile feedback, as well as the technical difficulties of safely removing masses near the mesenteric root. One solution is to use a hand-assisted laparoscopic device or enlarge an incision to exteriorize the small bowel for digital palpation of bowel.7,9,11,12 It is possible that variations of the hand-assisted technique were included in this study’s MIS only cohort. Another adjunct involves careful patient selection prior to consideration of a MIS approach to resection and lymphadenectomy. Kasai et al. developed an objective system for predicting cases when an MIS only approach is likely to fail based on the proximal location and size of mesenteric masses identified on preoperative imaging.9 Although there is inconclusive evidence to define the role of MIS for SBNETs, its short-term clinical benefits (i.e., shorter length of hospital stay, less postoperative pain, and decrease surgical morbidity) make the option of MIS worth considering, which seems to be the case based on the significantly increased use of MIS observed in this study.
The ability for clinicians to detect SBNETs, especially at early stages, is important in deciding on the clinical management and surgical approach for patients. Diagnostic imaging with injection of a somatostatin analogue labeled with positron emitting gallium 68 (68 Ga) dota peptides is highly accurate for guiding preoperative and intraoperative surgical management of patients.18 Lakis et al. conducted a clinical trial illustrating the benefit of radioguided surgery for a curative resection of NETs.19 However, the majority of patients in this clinical trial underwent open laparotomy. If a minimally invasive approach is being considered, one study did suggest using 68 Ga DOTATATE as an adjunct imaging study when all other studies are negative.20 Future prospective studies are needed to assess appropriate oncologic resection with radioguided minimally invasive surgery. Within the current years of our study sample, the imaging modality is not routinely covered by some insurance companies,18 which may also be a reason why patients with no insurance or government issued insurance were less likely associated with a MIS approach in this study.
Besides the observed short-term clinical benefits in the MIS only cohort, our study demonstrated a significantly greater (but clinically similar) number of LN harvested in the MIS cohort (13.3 in the MIS cohort vs 11.8 in the open cohort). This is also greater than the optimal cutoff of 8–9 LN needed to accurately identify nodal positivity in patients with SBNET as demonstrated by Motz et al. and Tran et al.16,21. Our study is the first to show that patients who underwent the MIS approach were more likely to obtain at least 8 lymph nodes than patients who underwent the open approach. Although the average number of nodes obtained (12 LNs) was similar, results from recent literature showed no statistical difference in LN yield between the two surgical groups, which is likely due to their small sample sizes (N = 61 and N = 93, respectively).10,13 Obtaining a larger LN harvest from a MIS approach (including hand-assisted techniques) has been demonstrated in the surgical management of other cancer types such as colorectal cancer because of better visualization and better access to more proximal areas of mesentery with laparoscopy for more complete mesenteric resection.22,23
Greater LN harvest is associated with improved prognosis regardless of nodal positivity in SBNETs, which is consistent with previous literature.16,24 This may be due to the high prevalence of occult nodal metastases with SBNETs regardless of pathologic stage. The results of our study confirm that examination of at least 8 LNs is associated with an improved overall survival, and, therefore, we agree with previous literature that harvesting at least 8 LNs is a desirable target goal for surgeons when performing regional lymphadenectomy for locoregional SBNETs.16,24
The MIS cohort’s likelihood to obtain at least 8 LN for both staging and removal of nodal micro-metastases may be due to the appropriate perioperative care at higher case volume centers received. Because of the greater learning curve to complete complex surgical oncology cases laparoscopically, higher case volume centers and academic centers have higher rates of laparoscopy experience in surgical oncology.8,16,25,26,27 This association is consistent with our findings for SBNETs, as we observed that patients treated at higher volume facilities were more likely to undergo minimally invasive surgery.
Our study highlights that insurance status and race are independent predictors of the utilization of MIS and survival. Insured and white non-Hispanic patients were more likely to be treated under MIS over uninsured and black patients. Private insurance and white non-Hispanic patients were associated with better survival than patients on Medicare and black patients. This racial and socioeconomic disparity is well established in laparoscopic surgeries including appendectomies, colectomies, and hysterectomies.28,29,30 Minority and lower socioeconomic groups may present with more advanced disease or present within hospital systems that provide lower quality of care for managing SBNETs.28 Therefore, further investigation is warranted to identify solutions to more equitable surgical access across race and insurance status.
This study should be interpreted with the following limitations. Utilizing a large registry such as the NCDB for a retrospective study may lead to selection bias. However, potential bias is mitigated by using a large sample size and using propensity score weighting to control for patient, socioeconomic, facility, and pathologic factors in our logistic regression and Cox proportional hazards models. Molecular biomarkers, such as Ki-67 index, which can be important for prognostication, are not collected in the NCDB to ensure it is equally distributed or controlled between the two surgical groups.31 In addition, the NCDB does not collect data on whether each case involved multifocal disease, on disease-free survival, and on recurrence of disease, which are common in SBNETs.17,32 Ethun et al.10 found that MIS cases for SBNETs were less likely to report multiple tumors resected, and recurrence rates were similar between both surgical approaches.
Another limitation especially for assessing overall survival between the MIS and open surgical approach is that the NCDB does not collect data on the urgency of the operation as patients may have been more likely to undergo open surgery and less likely to perform adequate regional lymphadenectomy if the initial presentation (such as complete intestinal obstruction or ischemic bowel) required emergent or urgent surgery. This may also explain the difference in survival between the two approaches in our Cox proportional hazards model. There may still be other unobserved factors (such as type of diagnostic imaging used) driving the decision to choose MIS or an open approach. To mitigate the limitation of identifying the urgency of surgery, patients who were readmitted within 30 days from initial operation and who died within 90 days of initial operation were excluded as a proxy for emergent surgeries in our sensitivity analysis. Significant results of MIS utilization and LN harvest were unchanged.
It is also important to note that cases identified as MIS only could have included a variation of hand-assisted techniques,7,9,11,12 which are not mentioned in the NCDB. However, cases that required a conversion to open surgery were captured as a separate variable and incorporated into the MIS cohort for this study’s trend analysis similar to an intention to treat analyses. The significant uptrend of MIS cases with the unchanged proportion of converted cases over the study period highlights the potential of attempting MIS initially for oncologic resection of SBNETs. It was assumed that postoperative outcomes such as LN harvest in converted cases would be similar to that of open surgery only. Therefore, the multivariable regression models as well as the weighted Cox proportional hazard models included the converted cases into the Open surgery subgroup.
Conclusion
To date, this is the only multicenter study highlighting the increasing prevalence of MIS for surgical resection of Stage I-III SBNETs and regional lymphadenectomy in the USA. We established that the utility of MIS should be recognized, considering its short-term clinical benefits such as shorter length of stay and lower unplanned readmissions. After careful preoperative planning with select patients, obtaining oncological outcomes including optimal LN harvest (≥ 8 LN) for adequate staging and treatment may be possible. Future randomized prospective studies will be needed to confirm non-inferiority with overall survival with a MIS approach when compared to an open surgery. As new advancements in minimally invasive techniques, new diagnostic modalities for detecting occult disease, and new systematic therapies arise, we predict that the role of MIS will be more clearly defined and may be the preferred initial approach to surgically managing SBNETs.
Abbreviations
- SBNETs:
-
Small bowel neuroendocrine tumors
- MIS:
-
Minimally invasive surgery
- LN:
-
Lymph node
- AJCC:
-
American Joint Committee on Cancer
- NCDB:
-
National Cancer Database
- ICD:
-
International Classification of Diseases
References
Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, et al. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA oncology. 2017;3(10):1335-42.
Bilimoria KY, Bentrem DJ, Wayne JD, Ko CY, Bennett CL, Talamonti MS. Small Bowel Cancer in the United States: Changes in Epidemiology, Treatment, and Survival Over the Last 20 Years. Annals of Surgery. 2009;249(1):63-71.
Shah M, Goldner W, Al B, al. e. Neuroendocrine and Adrenal Tumors National Comprehensive Cancer Network. 2020;Version 2. 2020.
Howe JR, Cardona K, Fraker DL, Kebebew E, Untch BR, Wang YZ, et al. The Surgical Management of Small Bowel Neuroendocrine Tumors: Consensus Guidelines of the North American Neuroendocrine Tumor Society. Pancreas. 2017;46(6):715-31.
Niederle B, Pape UF, Costa F, Gross D, Kelestimur F, Knigge U, et al. ENETS Consensus Guidelines Update for Neuroendocrine Neoplasms of the Jejunum and Ileum. Neuroendocrinology. 2016;103(2):125-38.
Choi AB, Maxwell JE, Keck KJ, Bellizzi AJ, Dillon JS, O’Dorisio TM, et al. Is multifocality an indicator of aggressive behavior in small bowel neuroendocrine tumors? Pancreas. 2017;46(9):1115.
Reissman P, Shmailov S, Grozinsky-Glasberg S, Gross DJ. Laparoscopic resection of primary midgut carcinoid tumors. Surgical Endoscopy. 2013;27(10):3678-82.
Tran CG, Sherman SK, Howe JR. The Landmark Series: Management of Small Bowel Neuroendocrine Tumors. Ann Surg Oncol. 2021;28(5):2741-51.
Kasai Y, Mahuron K, Hirose K, Corvera CU, Kim GE, Hope TA, et al. A novel stratification of mesenteric mass involvement as a predictor of challenging mesenteric lymph node dissection by minimally invasive approach for ileal neuroendocrine tumors. Journal of Surgical Oncology. 2020;122(2):204-11.
Ethun CG, Postlewait LM, Baptiste GG, McInnis MR, Cardona K, Russell MC, et al. Small bowel neuroendocrine tumors: A critical analysis of diagnostic work-up and operative approach. Journal of Surgical Oncology. 2016;114(6):671-6.
Wang SC, Parekh JR, Zuraek MB, Venook AP, Bergsland EK, Warren RS, et al. Identification of Unknown Primary Tumors in Patients With Neuroendocrine Liver Metastases. Archives of Surgery. 2010;145(3):276-80.
Massimino KP, Han E, Pommier SJ, Pommier RF. Laparoscopic surgical exploration is an effective strategy for locating occult primary neuroendocrine tumors. The American Journal of Surgery. 2012;203(5):628-31.
Figueiredo MN, Maggiori L, Gaujoux S, Couvelard A, Guedj N, Ruszniewski P, et al. Surgery for small-bowel neuroendocrine tumors: Is there any benefit of the laparoscopic approach? Surgical Endoscopy. 2014;28(5):1720-6.
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B, et al. Using the National Cancer Database for Outcomes Research: A Review. JAMA Oncol. 2017;3(12):1722-8.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-9.
Motz BM, Lorimer PD, Boselli D, Hill JS, Salo JC. Optimal Lymphadenectomy in Small Bowel Neuroendocrine Tumors: Analysis of the NCDB. J Gastrointest Surg. 2018;22(1):117-23.
Singh S, Chan DL, Moody L, Liu N, Fischer HD, Austin PC, et al. Recurrence in Resected Gastroenteropancreatic Neuroendocrine Tumors. JAMA Oncology. 2018;4(4):583-5.
Shell J, Keutgen XM, Millo C, Nilubol N, Patel D, Sadowski S, et al. 68-Gallium DOTATATE scanning in symptomatic patients with negative anatomic imaging but suspected neuroendocrine tumor. Int J Endocr Oncol. 2018;5(1):IJE04-IJE.
El Lakis M, Gianakou A, Nockel P, Wiseman D, Tirosh A, Quezado MA, et al. Radioguided Surgery With Gallium 68 Dotatate for Patients With Neuroendocrine Tumors. JAMA Surgery. 2019;154(1):40-5.
Nockel P, Babic B, Millo C, Herscovitch P, Patel D, Nilubol N, et al. Localization of Insulinoma Using 68Ga-DOTATATE PET/CT Scan. The Journal of Clinical Endocrinology & Metabolism. 2016;102(1):195-9.
Tran TB, Qadan M, Dua MM, Norton JA, Poultsides GA, Visser BC. Prognostic relevance of lymph node ratio and total lymph node count for small bowel adenocarcinoma. Surgery. 2015;158(2):486-93.
Boutros M, Hippalgaonkar N, Silva E, Allende D, Wexner SD, Berho M. Laparoscopic resection of rectal cancer results in higher lymph node yield and better short-term outcomes than open surgery: a large single-center comparative study. Dis Colon Rectum. 2013;56(6):679-88.
Douaiher J, Hussain T, Langenfeld SJ. Predictors of adequate lymph node harvest during colectomy for colon cancer. The American Journal of Surgery. 2019;218(1):113-8.
Landry CS, Lin HY, Phan A, Charnsangavej C, Abdalla EK, Aloia T, et al. Resection of at-risk mesenteric lymph nodes is associated with improved survival in patients with small bowel neuroendocrine tumors. World J Surg. 2013;37(7):1695-700.
Damle RN, Macomber CW, Flahive JM, Davids JS, Sweeney WB, Sturrock PR, et al. Surgeon Volume and Elective Resection for Colon Cancer: An Analysis of Outcomes and Use of Laparoscopy. Journal of the American College of Surgeons. 2014;218(6):1223-30.
Keller DS, Qiu J, Senagore AJ. Predicting opportunities to increase utilization of laparoscopy for rectal cancer. Surgical Endoscopy. 2018;32(3):1556-63.
Yeo HL, Isaacs AJ, Abelson JS, Milsom JW, Sedrakyan A. Comparison of Open, Laparoscopic, and Robotic Colectomies Using a Large National Database: Outcomes and Trends Related to Surgery Center Volume. Dis Colon Rectum. 2016;59(6):535-42.
Robinson CN, Balentine CJ, Sansgiry S, Berger DH. Disparities in the use of minimally invasive surgery for colorectal disease. Journal of Gastrointestinal Surgery. 2012;16(5):897-904.
Abenhaim HA, Azziz R, Hu J, Bartolucci A, Tulandi T. Socioeconomic and Racial Predictors of Undergoing Laparoscopic Hysterectomy for Selected Benign Diseases: Analysis of 341487 Hysterectomies. Journal of Minimally Invasive Gynecology. 2008;15(1):11-5.
Guller U, Jain N, Curtis LH, Oertli D, Heberer M, Pietrobon R. Insurance status and race represent independent predictors of undergoing laparoscopic surgery for appendicitis: Secondary data analysis of 145,546 patients. Journal of the American College of Surgeons. 2004;199(4):567-75.
Modlin IM, Gustafsson BI, Pavel M, Svejda B, Lawrence B, Kidd M. A Nomogram to Assess Small-Intestinal Neuroendocrine Tumor (‘Carcinoid’) Survival. Neuroendocrinology. 2010;92(3):143-57.
In H, Bilimoria KY, Stewart AK, Wroblewski KE, Posner MC, Talamonti MS, et al. Cancer recurrence: an important but missing variable in national cancer registries. Ann Surg Oncol. 2014;21(5):1520-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Disclosures
The authors have no relevant financial disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meeting Presentations
• Clinical Congress 2021 – American College of Surgeons, Virtual Quick Shot Oral Presentation, October 2021.
• North American Neuroendocrine Tumor Society 2021 Medical Symposium, Virtual Poster Presentation, November 2021.
Rights and permissions
About this article
Cite this article
Wong, W., Perez Holguin, R.A., Olecki, E.J. et al. Predictors and Outcomes of Minimally Invasive Surgery for Small Bowel Neuroendocrine Tumors. J Gastrointest Surg 26, 1252–1265 (2022). https://doi.org/10.1007/s11605-022-05264-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05264-6