Abstract
Background
Which patients with pancreatic intraductal papillary mucinous neoplasms (IPMNs) should undergo surgical intervention remains a controversial issue. The aim of this retrospective study was to validate the new European evidence-based guidelines on pancreatic cystic neoplasms (EEBGPCN) for the management of IPMNs.
Methods
One hundred fifty-eight patients with resected IPMNs at National Taiwan University Hospital between January 1994 and December 2016 were enrolled. Clinical information, including new-onset diabetes mellitus (DM) and preoperative CA 19-9 levels, were collected. All patients were stratified into three groups—absolute, relative indications, and conservative approach—according to EEBGPCN. The performance characteristics of EEBGPCN for high-grade dysplasia (HGD)/invasive carcinoma (IC) of IPMNs were calculated.
Results
One hundred seven (67.7%) patients with low-grade dysplasia and 51 patients with HGD/IC, including 10 HGD and 41 IC, were analyzed. The missed rate for HGD/IC by EEBGPCN was 1.9% (3/158). The sensitivity, specificity, positive and negative predictive values, and accuracy of the absolute or relative indications for resecting IPMN according to EEBGPCN were 94.1%, 28.0%, 38.4%, 90.9%, and 49.4%. Jaundice, enhancing mural nodule < 5 mm, cyst diameter > 40 mm, increased levels of serum CA 19-9, new-onset DM, and main pancreatic duct dilation were associated with HGD/IC.
Conclusions
The missed rate for HGD/IC is low by EEBGPCN. Increased serum CA 19-9 and new-onset DM in EEBGPCN were verified as the indications for the surgical resection of IPMNs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intraductal papillary mucinous neoplasms (IPMNs) of the pancreas represent a group of pancreatic mucinous cystic neoplasms that are considered to have malignant potential1. The estimated malignant transformation rates of IPMNs range from 6 to 40%2,3. Surgically fit patients should consider to be treated by tumor resection, but surgical resection for IPMNs is associated with significant rates of morbidity and mortality and not all IPMNs are malignant. Therefore, which patients with IPMNs should undergo surgical intervention remains controversial4. In recent decades, different practice guidelines have been published to provide recommendations for the clinical management of pancreatic IPMNs, but their application has reported the presence of unnecessary surgery for low-risk lesions and missing lesions of high-grade dysplasia (HGD) or invasive carcinoma (IC)5,6,7,8,9. Sighinolfi et al. reported that the 2015 American Gastroenterological Association (AGA) criteria have lower sensitivity than the 2012 International Consensus/Fukuoka Guidelines for the detection of advanced pancreatic cystic neoplasms but higher specificity than the Fukuoka criteria6. European evidence-based guidelines on pancreatic cystic neoplasms (EEBGPCN) were published to improve the diagnosis and management of PCN in 201810. The summary of European evidence-based guidelines, AGA Institute guidelines, and the Fukuoka consensus guidelines on management of pancreatic cystic neoplasms are shown in Table 1. The EEBGPCN recommend that patients with the absolute and relative indications to receive surgical resection of IPMN. A conservative approach is recommended for asymptomatic IPMNs measuring less than 40 mm10. The main differences between EEBGPCN and the other international guidelines are the adoption of laboratory data, including the serum levels of carbohydrate antigen (CA) 19-9 and new-onset diabetes mellitus (DM), and an increased cyst diameter to 40 mm as indications for resection10. To evaluate the performance characteristics of the new EEBGPCN, we conducted this retrospective study to enroll a series of patients with surgically resected and pathologically proven IPMNs at our institution and prove the effectiveness of EEBGPCN.
Methods
Study Population
We retrospectively analyzed and reviewed the medical records of 158 consecutive patients diagnosed with IPMNs by surgical pathology at the National Taiwan University Hospital between January 1994 and December 2016. Clinical information, including age at the time of surgery, gender, presence of symptoms (jaundice and history of acute pancreatitis), presence of DM, new-onset DM, and preoperative CA 19-9 serum levels, imaging studies, and pathologic reports, was collected. The preoperative imaging diagnosis was made by computed tomography (CT), magnetic resonance imaging (MRI)/magnetic resonance cholangiopancreatography (MRCP), and/or endoscopic ultrasonography (EUS). The sizes of the cyst, mural nodule, and diameter of the main pancreatic duct were evaluated by imaging studies, and the maximum measurements were recorded. All the patients with IPMNs were stratified into three groups (absolute indications, relative indications, and conservative approach) after retrospectively reviewing the absolute and relative indications for resection according to EEBGPCN. The IPMNs that did not meet any criteria of absolute or relative indications for resection were classified as the conservative approach group. The surgical pathology specimens were reviewed by a single experienced pathologist (Y. M. Jeng) using a two-tiered classification system: low grade versus high grade to replace the WHO three-tiered classification for IPMN according to the revised classification system from the Baltimore consensus meeting for neoplastic precursor lesions in the pancreas11. Because EEBGPCN guidelines recommend that all the patients with MD (main ductal)-IPMN or MT (mixed type)-IPMN who are fit for surgery should undergo resection, we analyzed all the patients with IPMN and patients with BD-IPMN separately. The study protocol was approved by the Institutional Review Board of National Taiwan University Hospital. Informed consent from the patients was waived because this study was a retrospective medical record review.
Statistical Analysis
To assess the difference in the demographic data and clinical characteristics between the low-grade dysplasia (LGD) and HGD/IC groups diagnosed by surgical pathology, categorical variables were analyzed using chi-squared tests and continuous variables using t tests. Fisher’s exact test was used when the cell counts were fewer than 5. Univariate analysis was performed to identify risk factors that were correlated with HGD/IC. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated to evaluate the performance of EEBGPCN in identifying HGD/IC. Statistical analysis was performed using SAS 9.4 Statistical Software (SAS Institute, Cary, NC, USA). All tests were two-tailed, differences were considered significant when p < 0.05, and confidence intervals were set at 95%.
Results
Patient Characteristics
One hundred fifty-eight patients were included in our study. The clinical characteristics of the study population stratified by final surgical pathology results are shown in Table 2. Among these 158 patients, 107 (67.7%) had a LGD diagnosis by surgical pathology; the remaining 51 patients were classified as HGD/IC, which included 10 HGD and 41 IC based on surgical pathology. The mean age of these 158 patients was 63.4 years (20–84.8 years) with a male: female ratio of 1.19:1. Most of the lesions were located at the pancreatic head (71.5%, 113/158) and were branch duct (BD)-IPMNs (64.6%, 102/158) (Table 2). The mean size of the cystic lesion measured on imaging study was 34.3 mm (5–120 mm). The mean size of the main pancreatic duct (MPD) measured was 9.6 mm (0.8–75 mm). The mean of the CA 19-9 serum level was 437.2 U/mL (1–24,000 U/mL). Among these 158 patients, age, gender, tumor location, IPMN type, mean MPD size, and DM history were not significantly different between the LGD and HGD/IC groups (Table 2).
Among 102 patients with BD-IPMN, 69 (67.6%) had a LGD diagnosis by surgical pathology. The remaining 33 patients were classified as HGD/IC, which included 6 HGD and 27 IC based on surgical pathology (Table 2). The mean age of these 102 patients was 62.0 years (20–84.4 years) with a male:female ratio of 1.04:1. Most of the lesions were located at the pancreatic head (67.6%, 69/102) (Table 2). The mean size of the cystic lesion measured on imaging study was 34.7 mm (7–120 mm). The mean size of the main pancreatic duct (MPD) measured was 6.4 mm (2.1–16 mm). The mean of the CA 19-9 serum level was 519.2 U/mL (1–24,000 U/mL). Among these 102 patients, age, gender, tumor location, mean MPD size, and DM history were not significantly different between the LGD and HGD/IC groups (Table 2).
Diagnostic Performance of the 2018 EEBGPCN for Resected IPMNs
When EEBGPCN was applied to the study population, 60 (38.0%, 60/158) patients met the criteria with at least one absolute indication for resection, and 29 (48.3%, 29/60) were verified with HGD/IC (Table 2). In the patients with at least one relative indication for resection, 47 of 116 (40.5%) patients were verified with HGD/IC. The indications including positive cytology for malignancy/HGD (p = 0.001), solid mass (p = 0.0003), jaundice (p < 0.0001), MPD dilation more than 10 mm (p = 0.046), a growth rate more than 5 mm per year (p = 0.040), increased levels of serum CA 19-9 (p = 0.004), a cyst diameter more than 40 mm (p = 0.0005), new-onset DM (p = 0.004), and enhancing mural nodule less than 5 mm (p < 0.0001) were significantly associated with HGD/IC (Table 2).
Among the patients with BD-IPMN, 15 (14.7%) patients met the criteria with at least one absolute indication for resection and 11 (73.3%) were verified with HGD/IC (Table 2). In the patients with at least one relative indication for resection, 30 of 70 (42.8%) patients were verified with HGD/IC. Positive cytology for malignancy/HGD (p = 0.01), solid mass (p = 0.011), jaundice (p < 0.0001), increased levels of serum CA 19-9 (p = 0.001), MPN dilation between 5 and 9 mm (p = 0.004), a cyst diameter more than 40 mm (p = 0.0006), new-onset DM (p = 0.011), and enhancing mural nodule less than 5 mm (p = 0.002) were significantly associated with HGD/IC (Table 2).
Based on the final surgical pathology, Table 3 shows the diagnostic performance of indications for resection according to the EEBGPCN stratified by the all patients with IPMN and patients with BD-IPMN. Among the 102 patients with BD-IPMN, 11 (33.3%) and 30 (90.9%) of 33 patients with HGD/IC met the criteria of at least one absolute and at least one relative indication for resection, respectively (Table 3). The sensitivity, specificity, PPV, NPV, and accuracy for at least one absolute indication for resection according to EEBGPCN to identify HGD/IC in patients with BD-IPMN were 33.3%, 94.2%, 73.3%, 74.7%, and 74.5%, respectively, The diagnostic performance for at least one relative indication for resection in identified HGD/IC among the BD-IPMN group were 90.9%, 42.0%, 42.8%, 90.6%, and 57.8%, respectively (Table 3). Table 3 also shows the diagnostic performance of at least one absolute or one relative indication and at least one absolute and one relative indications for resection according to EEBGPCN.
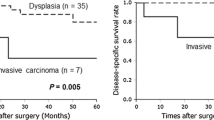
According to EEBGPCN, 33 patients were presumed to be in the conservative approach group but received surgical resection. Thirty of them were the patients with BD-IPMN and three of them were proven to have HGD/IC (Table 2). Hence, the missed rate for EEBGPCN was 1.9% (3/158) among all the patients with IPMN and 2.9% (3/102) among the patients with BD-IPMN in this study. One of these three patients who received pylorus-preserving pancreatectomy had a 3.7-cm-sized cyst that turned out to be IPMN with HGD by surgical pathology. Another two patients had 2.6- and 2.1-cm-sized cysts, respectively. Distal pancreatectomy was performed, and both final pathologic reports were IC.
Discussion
The selection of patients with IPMN for surgical resection remains a clinical challenge because the biological behavior of IPMN ranges from benign to malignant. The EEBGPCN introduced by a joint initiative of the European experts in 2018 replaced the 2013 European expert consensus statement on cystic tumors of the pancreas7,10. It recommended that patients with MD-/MT-IPMN should undergo surgical resection because of the high prevalence of malignancy, and patients with BD-IPMN should be followed unless they have absolute or relative indications for resection10. In addition to the European guidelines, other international guidelines for the management of patients with PCN have been published for years8,9,12. The reported ranges of the sensitivity, specificity, PPV, NPV, and accuracy for the other guidelines were 7.3–97.7%, 28.2–95.8%, 10.0–78.6%, 73.2–98.9%, and 44.7–80.2%, respectively2,6,13,14,15. The diagnostic performance of 2018 EEBGPCN is comparable to those reported by previous studies using the other guidelines 2,6,13,14,15. This study investigated the clinical usefulness of the 2018 EEBGPCN using a case series with pathologically proven IPMNs. We found that the frequency of HGD/IC of IPMNs was 32.3% in our study, a value within the range of previously reported surgical series13,14. When EEBGPCN was applied, three of 33 patients presumed to be in the conservative approach group were verified with HGD/IC by surgical pathology. Therefore, the missed rate for EEBGPCN was 1.9% (3/158) in this study. Thus, the false-negative rate was 5.9% (3/51), which was correlated with the high sensitivity (94.1%) of the at least one absolute or one relative indication for resection according to EEBGPCN (Table 3). These three missed cases were all young (53, 51, and 52 years old, respectively) and had BD-IPMN with a cyst size more than 2 cm in diameter. They received surgical resection according to the recommendation of the Fukuoka guidelines. The first one had a 3.7-cm-sized cyst, and the second and third patients had a 2.6- and 2.1-cm-sized cyst with worrisome features on EUS, respectively. The last two patients both had a cyst more than 2 cm but less than 3 cm in diameter, indicating that even small cysts can harbor IC in this study. The Sendai and Fukuoka guidelines have emphasized a cyst size more than 3 cm as an indication for resection, but there are several studies with demonstrated HGD/IC in cysts with a size less than 3 cm16,17. Therefore, size alone is not an accurate indication for resection. In this study, the sensitivity, specificity, PPV, NPV, and accuracy of a cyst diameter more than 40 mm as a resection indication were 45.1% (23/51), 81.3% (87/107), 53.5% (23/43), 75.6% (87/115), and 69.6% (110/158), respectively. Applying the criteria of a cyst diameter more than 30 mm as a resection indication in our case series, the sensitivity (52.9%, 27/51) was higher than 45.1%, but the specificity (71.0%, 76/107) was lower than 81.3%. The accuracy (69.6%) of the cyst diameter more than 40 mm was higher than that more than 30 mm (65.2%, 103/158), indicating that EEBGPCN provided a significant paradigm by classifying the cyst size more than 40 mm as a relative indication for resection without sacrificing the diagnostic accuracy in this study.
EEBGPCN shows less stringent resection criteria than the European expert consensus statement and the Fukuoka guidelines, allowing more patients to be observed, but the false-positive rate for surgical resection according to the at least one absolute or at least one relative indications for resection was 58.3% (42/72) in patients with resected BD-IPMN. Thus, 42 patients received unnecessary surgery for a low-grade lesion. These low-specificity (39.1%) and accuracy (55.9%) values were comparable to the study by Zhou W et al in China15. Furthermore, when another guideline was applied to our case series, surgical resection was also recommended to the patients with low-grade lesions in this study. The EEBGPCN, like other guidelines for the management of IPMN, still cannot avoid overtreating patients or treating patients too early with PCNs.
We found that the presence of jaundice, an enhancing mural nodule less than 5 mm, a cyst diameter more than 40 mm, increased levels of serum CA 19-9, new-onset DM, MPD dilation between 5 and 9.9 mm, and an MPD dilation more than 10 mm are associated with malignancy. Most of the 12 absolute and relative indications for resection according to EEBGPCN are the predictors of IPMN with HGD/IC in another studies7,8,9,10,12,18. Increased levels of serum CA 19-9 and new-onset DM are the relative indications for resection according to EEBGPCN and are the relatively new criteria formally applied in the guidelines for the management of PCNs. Using 2018 EEBGPCN criteria, we confirmed that increased levels of serum CA 19-9 were associated with HGD/IC in this study. Increased levels of serum CA 19-9, at least one absolute indication, and at least one absolute and one relative indications in identified HGD/IC among resected IPMN group have the same accuracy (71.6–76.5%). In a systematic review conducted by Heckler et al. for the predictive performance of factors associated with IPMN with HGD/IC, it was reported that CA 19-9 might be a valuable adjunct for the management of IPMN18. Our study provides evidence that increased levels of serum CA 19-9 could be a relative indication of resection for IPMNs as an EEBGPCN recommendation.
In this study, we found that new-onset DM was statistically significantly associated with IPMNs with HGD/IC. Although the sensitivity of new-onset DM (27.3%) in identified HGD/IC was not as high, the specificity was 92.8% and accuracy was 71.6% in identified HGD/IC among resected BD-IPMN group. The association between DM and pancreatic cancer (PC) has been known for years19,20. Long-standing DM is a risk factor for PC, and new-onset DM can be an early manifestation of PC. An evidence-based review conducted by Raghavan et al. reported that patients with non-insulin-dependent (NID) DM have a 1.5- to 2-fold increased relative risk of developing PC. One-fourth of patients with PC have NIDDM compared with one-tenth of age-matched control subjects (p < 0.0001). New-onset DM is identified in 14.7% of patients with PC compared with 2.7% of age-matched controls21. Khadka et al. reported a review article that revealed a bidirectional relationship between DM and PC. New-onset DM could be an early sign of PC22. Our study validated that new-onset DM is a risk factor for IPMN and should be a relative indication for the resection of IPMN as an EEBGPCN recommendation.
There are several differences between the EEBGPCN and the Fukuoka guidelines. First, EEBGPCN classifies cyst size more than 40 mm as a relative indication for resection. Second, increased levels of serum CA 19-9 and new-onset DM are formally the indications for resection of IPMNs in the guidelines. Third, EEBGPCN defined a growth rate of more than 5 mm per year as a relative indication for resection. Fourth, the cutoff value of an enhancing mural nodule was set at 5 mm as the criterion for absolute and relative indication. According to this study, we validated the clinical usefulness of a cyst size more than 40 mm, increased levels of serum CA 19-9, and new-onset DM as indications for the resection of IPMN.
There are several limitations in this study. First, it was a retrospective study involving a small number of patients. The outcomes of our patients presumed to receive a conservative approach by EEBGPCN were not known because all the patients underwent surgical resection, so our study might not be applied to the population of patients being evaluated prior to surgical resection. A large population-based prospective cohort study is needed to further validate the performance of EEBGPCN. Second, only 13 patients had received endoscopic-ultrasound-guided fine needle aspiration of the pancreas before surgical intervention. The absolute indication of positive cytology for malignancy/HGD cannot be well evaluated. Third, six of 158 patients had a solid mass and none had a final surgical pathology of LGD. We could not calculate the robust OR using statistical methods. Finally, our institution is an academic tertiary care referral center. We could not obtain the detailed follow-up history and imaging data of the patients from other hospitals. Therefore, we could not evaluate whether the growth rate was more than 5 mm per year.
Conclusion
The diagnostic performance of the 2018 EEBGPCN was comparable to other established guidelines. Both absolute and relative indications for the resection of IPMNs show statistically significant differences between the LGD and HGD/IC groups. Adhering to the guidelines, the missed rate for HGD/IC is low using the EEBGPCN criteria. In addition to most indications for resection that had been well established by the other guidelines, increased levels of serum CA 19-9 and new-onset DM were verified as the relative indications for surgical resection of IPMNs in this study. We recommend EEBGPCN as the current guideline for the management of patients with IPMN, but more well-designed prospective studies are needed to answer the uncertain questions about the clinical management of IPMNs in the future.
References
Bassi C, Sarr MG, Lillemoe KD, Reber HA. Natural History of Intraductal Papillary Mucinous Neoplasms (IPMN): Current Evidence and Implications for Management. J Gastrointest Surg. 2008;12(4):645-50. https://doi.org/10.1007/s11605-007-0447-x.
Xu MM, Yin S, Siddiqui AA, Salem RR, Schrope B, Sethi A et al. Comparison of the diagnostic accuracy of three current guidelines for the evaluation of asymptomatic pancreatic cystic neoplasms. Medicine (Baltimore). 2017;96(35):e7900. https://doi.org/10.1097/md.0000000000007900.
Hsiao CY, Yang CY, Wu JM, Kuo TC, Tien YW. Utility of the 2006 Sendai and 2012 Fukuoka guidelines for the management of intraductal papillary mucinous neoplasm of the pancreas: A single-center experience with 138 surgically treated patients. Medicine (Baltimore). 2016;95(38):e4922. https://doi.org/10.1097/md.0000000000004922.
LaFemina J, Katabi N, Klimstra D, Correa-Gallego C, Gaujoux S, Kingham TP et al. Malignant Progression in IPMN: A Cohort Analysis of Patients Initially Selected for Resection or Observation. Ann Surg Oncol. 2013;20(2):440-7. https://doi.org/10.1245/s10434-012-2702-y.
Falconi M, Crippa S, Chari S, Conlon K, Kim SW, Levy P et al. Quality assessment of the guidelines on cystic neoplasms of the pancreas. Pancreatology. 2015;15(5):463-9. https://doi.org/10.1016/j.pan.2015.05.478.
Sighinolfi M, Quan SY, Lee Y, Ibaseta A, Pham K, Dua MM et al. Fukuoka and AGA Criteria Have Superior Diagnostic Accuracy for Advanced Cystic Neoplasms than Sendai Criteria. Dig Dis Sci. 2017;62(3):626-32. https://doi.org/10.1007/s10620-017-4460-y.
Del Chiaro M, Verbeke C, Salvia R, Kloppel G, Werner J, McKay C et al. European experts consensus statement on cystic tumours of the pancreas. Dig Liver Dis. 2013;45(9):703-11. https://doi.org/10.1016/j.dld.2013.01.010.
Tanaka M, Fernandez-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12(3):183-97. https://doi.org/10.1016/j.pan.2012.04.004.
Vege SS, Ziring B, Jain R, Moayyedi P. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015;148(4):819-22; quize12-3. https://doi.org/10.1053/j.gastro.2015.01.015.
M. H, L. B, U. H, T. P, C. T, J. K et al. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018;67(5):789-804. https://doi.org/10.1136/gutjnl-2018-316027.
Basturk O, Hong SM, Wood LD, Adsay NV, Albores-Saavedra J, Biankin AV et al. A Revised Classification System and Recommendations From the Baltimore Consensus Meeting for Neoplastic Precursor Lesions in the Pancreas. Am J Surg Pathol. 2015;39(12):1730-41. https://doi.org/10.1097/pas.0000000000000533.
Tanaka M, Fernandez-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017;17(5):738-53. https://doi.org/10.1016/j.pan.2017.07.007.
Yu S, Takasu N, Watanabe T, Fukumoto T, Okazaki S, Tezuka K et al. Validation of the 2012 Fukuoka Consensus Guideline for Intraductal Papillary Mucinous Neoplasm of the Pancreas From a Single Institution Experience. Pancreas. 2017;46(7):936-42. https://doi.org/10.1097/mpa.0000000000000874.
Srinivasan N, Teo J-Y, Chin Y-K, Hennedige T, Tan DM, Low AS et al. Systematic review of the clinical utility and validity of the Sendai and Fukuoka Consensus Guidelines for the management of intraductal papillary mucinous neoplasms of the pancreas. HPB (Oxford). 2018;20(6):497-504. https://doi.org/10.1016/j.hpb.2018.01.009.
Zhou W, Xu Y, Rong Y, Wu W, Kuang T, Xin B et al. Validation of Sendai and Fukuoka consensus guidelines in predicting malignancy in patients with preoperatively diagnosed mucinous pancreatic cystic neoplasms. J Surg Oncol. 2017;117(3):409-16. https://doi.org/10.1002/jso.24882.
Wong J, Weber JA Centeno B, Vignesh S, Harris CL, Klapman JB et al. High-Grade Dysplasia and Adenocarcinoma Are Frequent in Side-Branch Intraductal Papillary Mucinous Neoplasm Measuring Less than 3 cm on Endoscopic Ultrasound. J Gastrointest Surg. 2013;17(1):78-85. https://doi.org/10.1007/s11605-012-2017-0.
Fritz S, Klauss M, Bergmann F, Hackert T, Hartwig W, Strobel O et al. Small (Sendai Negative) Branch-Duct IPMNs: Not Harmless. Ann Surg. 2012;256(2):313-20. https://doi.org/10.1097/SLA.0b013e31825d355f.
Heckler M, Brieger L, Heger U, Pausch T, Tjaden C, Kaiser J et al. Predictive performance of factors associated with malignancy in intraductal papillary mucinous neoplasia of the pancreas. BJS Open. 2018;2(1):13-24. https://doi.org/10.1002/bjs5.38.
Aggarwal G, Rabe KG, Petersen GM, Chari ST. New-onset diabetes in pancreatic cancer: a study in the primary care setting. Pancreatology. 2012;12(2):156-61. https://doi.org/10.1016/j.pan.2012.02.003.
Pannala R, Leibson CL, Rabe KG, Timmons LJ, Ransom J, de Andrade M et al. Temporal association of changes in fasting blood glucose and body mass index with diagnosis of pancreatic cancer. Am J Gastroenterol. 2009;104(9):2318-25. https://doi.org/10.1038/ajg.2009.253.
Raghavan SR, Ballehaninna UK, Chamberlain RS. The impact of perioperative blood glucose levels on pancreatic cancer prognosis and surgical outcomes: an evidence-based review. Pancreas. 2013;42(8):1210-7. https://doi.org/10.1097/MPA.0b013e3182a6db8e.
Khadka R, Tian W, Hao X, Koirala R. Risk factor, early diagnosis and overall survival on outcome of association between pancreatic cancer and diabetes mellitus: Changes and advances, a review. Int J Surg. 2018;52:342-6. https://doi.org/10.1016/j.ijsu.2018.02.058.
Author information
Authors and Affiliations
Contributions
I-Shiow Jan: contributions to the design of study, interpretation of data, and drafting the manuscript. Ming-Chu Chang, Ching-Yao Yang, Yu-Wen Tien, Yung-Ming Jeng, Chih-Horng Wu, and Bang-Bin Chen: contributions to acquisition, analysis, and interpretation of data and assisting in drafting the manuscript. Yu-Ting Chang: contributions to the design of the study, acquisition, analysis, and interpretation of data, drafting the manuscript, and final approval of the version to be published.
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jan, IS., Chang, MC., Yang, CY. et al. Validation of Indications for Surgery of European Evidence-Based Guidelines for Patients with Pancreatic Intraductal Papillary Mucinous Neoplasms. J Gastrointest Surg 24, 2536–2543 (2020). https://doi.org/10.1007/s11605-019-04420-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04420-9