Abstract
Background
Physical exercise prehabilitation has been proposed to improve postoperative outcomes in patients undergoing major abdominal surgery. The aim of this systematic review was to investigate the effect of preoperative exercise training compared with standard care on postoperative outcomes in major abdominal surgery.
Methods
Randomized controlled trials (RCT) comparing prehabilitation with standard care were identified by a systematic literature search of MEDLINE and CENTRAL. Qualitative and quantitative analyses of perioperative outcome data were conducted. Meta-analyses were performed wherever possible and meaningful.
Results
A total of eight trials including 442 patients met the inclusion criteria. These trials investigated the effect of prehabilitation in patient cohorts undergoing major liver, colorectal, gastroesophageal, and general abdominal surgery. Quantitative analyses of all included trials showed a significant reduction in postoperative pulmonary complications (OR 0.37; 0.20 to 0.67; p = 0.001) as well as in postoperative overall morbidity (OR 0.52; 0.30 to 0.88; p = 0.01) in the prehabilitation group compared with standard care. The length of hospital stay showed no significant differences between the groups (MD − 0.58; − 1.28 to 0.13; p = 0.11). Risk of bias and methodological quality varied substantially among the trials, most of which were small single-center studies.
Conclusion
Prehabilitation including a physical exercise intervention may lead to a reduction of postoperative pulmonary complications as well as less overall morbidity compared with standard care in patients undergoing major abdominal surgery. Further, well-designed RCT are needed to evaluate these potential positive effects in more detail and to identify suitable target populations.
Protocol Registration
PROSPERO 2017 CRD42017080366
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morbidity after major abdominal surgery is substantial. More than 20% of patients suffer from postoperative complications that require invasive treatment and substantially increase the risk of further morbidity and mortality.1 Apart from surgical morbidity, nonsurgical complications represent a significant proportion of postoperative complications. Cardiopulmonary adverse events account for up to 50% of postoperative complications in upper abdominal operations.2,3,4 Pulmonary complications lead to significantly increased morbidity, mortality, and length of hospital stay (LOS), especially after major upper abdominal surgery.5 Multiple perioperative interventions have been proposed in the past to reduce the risk of postoperative complications, including “enhanced recovery after surgery” protocols, which can lead to a reduction in postoperative complications and shorter LOS.6 However, the focus of these interventions is largely on in-hospital care in the immediate postoperative period.
Other approaches have been suggested to improve perioperative outcomes in surgical patients. One promising concept is “prehabilitation,” i.e., the reduction of postoperative complications by improving the preoperative physical fitness of patients by means of preoperative exercise training programs.7 Prehabilitation represents a shift not only away from the postoperative to the preoperative period, but also away from a passive model of care “towards a proactive approach that enables patients to become active participants in their care” by improving their physical health before surgery.8
A beneficial effect of prehabilitation has been proposed for several surgical specialties, including pulmonary9 and orthopedic surgery.10 In abdominal surgery, the evidence for preoperative prehabilitation is sparse, although a few randomized controlled trials (RCT) have investigated the effect of preoperative exercise in patients undergoing abdominal surgery.11,12,13 While some RCT have shown promising results, with the reduction of postoperative complications14 and improvement of pulmonary function,12,15 others have reported conflicting outcomes.16 Previous systematic reviews have attempted to summarize these results17,18,19,20; however, the lack of standardized inclusion criteria, quantitative analyses, or a clear focus on abdominal surgery in these reports hampers interpretation of the results. In addition, some of these reviews included interventions that differ from aerobic exercise training, such as inspiratory muscle training (IMT) or nutritional approaches, thus leading to bias in further analyses.17 Finally, new studies have been published in the meantime.
Thus, the aim of our systematic review and meta-analysis is to assess the findings of RCT with regard to the effect of exercise-based prehabilitation in major abdominal surgery, focusing on important parameters of postoperative outcome.
Methods
This systematic review was performed according to the recommendations of the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA).21 The study was registered in the “International Prospective Register of Systematic Reviews” (PROSPERO) in 2017 (CRD42017080366), and the detailed prespecified protocol is available upon request.
Literature Search
In accordance with recently published recommendations for surgical systematic reviews of RCT,22 we conducted a systematic literature search of MEDLINE (via PubMed) and the Cochrane Central Register of Controlled Trials (CENTRAL) from the respective database initiation until 30 October 2017. To construct the search, the patient–intervention–comparison–outcome (PICO) scheme was used, combining patient (abdominal surgery), intervention (prehabilitation), control (standard care), and outcome (postoperative outcome measures) characteristics. To improve accuracy, the MEDLINE search was combined with the “Cochrane Highly Sensitive Search Strategy for identifying RCT in MEDLINE,” sensitivity-maximizing version, PubMed format (2008 revision). The exemplary search strategy for MEDLINE (via PubMed) is provided in supplement 1. For CENTRAL, the search strategy was adapted to the specific vocabulary of the database. Additionally, retrieved articles were hand searched for relevant studies. There were no restrictions regarding language or publication date.
Eligibility Criteria and Study Selection
All RCT that included patients undergoing abdominal surgery for different indications and compared the outcomes after a preoperative physical training program with that after standard care without a physical training program were eligible for inclusion in this systematic review. Studies comparing different types of physical training and lacking a control group without preoperative physical training were excluded. The study selection process was performed by two reviewers (PH and ALM) who independently inspected the title and abstract of all articles retrieved by the systematic literature search and the full texts of all articles assessed for eligibility. In the event of a disagreement about inclusion or exclusion of a study, a third reviewer (MKD) was consulted and a decision was made after discussion of the article.
Data Extraction and Outcomes
The extraction of the data from the included trials was carried out independently by two authors (PH and ALM) using prespecified forms. The data extracted included publication and study data, title of publication, authors, year of publication, journal, language, funding sources, trial duration, number of treatment groups, total number of patients, evaluable patients, withdrawals, and patients lost to follow-up. The clinical and outcome data that were extracted included the patient’s baseline characteristics such as age, gender, body mass index, tumor entity, neoadjuvant therapy, smoking history, and pulmonary baseline function together with perioperative data such as functional pulmonary parameters after prehabilitation, postoperative overall complications, pulmonary complications, overall mortality, quality of life, and length of hospital stay (LOS).
Risk of Bias Assessment
As this systematic review included only RCT, the risk of bias for each study was evaluated using the Cochrane tool for risk of bias.23 The tool includes the following six domains, each rated as high, unclear, or low risk of bias: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, and selective reporting. Furthermore, a funnel plot was created to evaluate publication bias for each outcome.
Statistical Analyses
A qualitative analysis was performed for all studies fulfilling the inclusion criteria. Studies not offering perioperative outcome data were not suitable for meta-analyses and were therefore excluded from further quantitative analyses. For all trials that included postoperative outcome parameters, quantitative analyses and meta-analyses were additionally performed. For continuous outcomes, the mean differences (MD) and 95% confidence intervals (CI) were measured by the inverse-variance method. For dichotomous outcomes, the odds ratios (OR) and 95% CI were calculated using a Mantel–Haenszel model. Where data were reported by median and range, the method described by Hozo et al.24 was used to provide mean and standard deviation. Statistical analyses were conducted using Review Manager (version 5.3; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). As the level of significance, an alpha of 0.05 was determined. A random effects model was used as there was clinical heterogeneity among the included trials. Heterogeneity was evaluated using the I2 statistic. The results were classified as follows: below 25%, low heterogeneity; between 25% and 75%, possibly moderate heterogeneity; over 75%, considerable heterogeneity.
Results
Study Selection
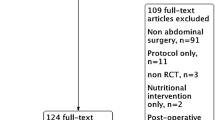
A total number of 5548 articles were identified after the initial search of MEDLINE and CENTRAL, of which 5527 were excluded as they were nonrandomized studies, not relevant, or duplicates (see Fig. 1 for PRISMA flow chart). Thus, the full texts of 21 articles were retrieved and assessed for eligibility. An additional three articles were found by hand-searching the reference lists of retrieved articles. After the assessment, eight of these 24 articles met the inclusion criteria and were included in the qualitative analysis of this systematic review, and data extraction was performed.12,14,25,26,27,28,29,30 Further assessment showed that one of the included trials30 offered no perioperative outcome data, so it was excluded from additional analyses and meta-analyses. The remaining seven trials were included in the quantitative analyses and meta-analyses.
Study Characteristics
Two of the eight trials evaluated prehabilitation in patients undergoing liver resection, three trials in patients undergoing colorectal surgery (one of which investigated the effect in elder patients with an age > 60 years), one study included patients with esophageal resection for esophageal cancer, and two trials evaluated prehabilitation in a patient cohort undergoing various kinds of major abdominal surgery (see Table 1 for study characteristics).
The eight included studies evaluated a total number of 442 patients, of whom 226 underwent preoperative prehabilitation. The various training protocols all included aerobic training sessions. The duration of prehabilitation in the intervention group ranged from 7 days to 6 weeks before surgery, and the number of sessions per week from one to five. The prehabilitation sessions included aerobic training in various modes (ergometer or walking) in all studies, together with a variety of additional types of training such as IMT, resistance training, coughing training, or stretching (Table 1).
The remaining 216 of 442 patients served as controls without a preoperative training program. In five trials,12,14,26,29,30 the control group underwent standard care only; in two studies,13,28 the control group received the same additional advice (dietary measures, coping strategies) as the intervention group but without preoperative training; and in one trial,25 the control group was advised to do training at home, but in contrast to the intervention group there was no standardization or further assistance.
The baseline parameters of the included patients were comparable and showed no significant differences between the intervention and control groups in any individual trial. The overall mean age of the patients was 64.9 years in the prehabilitation group and 65.6 years in the control group. A meta-analysis of baseline individual patient data (IPD) was impossible, as no IPD were reported in any trial.
Liver Surgery
Two of the included trials26,28 investigated the effect of a prehabilitation program on patients being treated by liver resection. Kaibori et al. included 51 patients undergoing liver resection due to hepatocellular carcinoma and performed a training program of three 60-min sessions per week over at least a month preoperatively and for another 6 months postoperatively. This was an exploratory trial without a predefined primary endpoint. The prehabilitation program led to significant decreases in whole body mass, fat mass, and fasting serum insulin as well as an increase in the anaerobic threshold and improvement in insulin resistance. Furthermore, the authors reported a postoperative morbidity rate of 8.7% and a mean length of hospital stay (LOS) of 13.7 days in the prehabilitation group compared with 13.0% and 17.5 days, respectively, in the control group (p = 0.67 for morbidity and p = 0.12 for LOS). No definition of or classification for postoperative complications was applied.
The second trial, by Dunne et al., included 38 patients, of whom 20 underwent a preoperative training program of 12 interval-exercise sessions on a cycle ergometer over 4 weeks. The indications for liver surgery were colorectal liver metastases in all patients. The primary outcome of the study, the preoperative oxygen uptake at the anaerobic threshold after completion of the prehabilitation program, was found to significantly improved in the intervention group. Furthermore, the oxygen pulse and the quality of life as evaluated by the SF-36 score were both higher after the training period. Of the 38 patients included, 34 (19 in the prehabilitation group, 15 in the control group) were available for intention-to-treat analysis of the clinical outcomes. The authors reported a 42.1% overall postoperative complication rate, defined as any complication according to the Clavien–Dindo classification,31 in the prehabilitation group compared with 46.7% in the control group (not statistically significant). Similarly, pulmonary complications were 10.5% in the prehabilitation group vs. 20.0% in the control group (not statistically significant). The mean LOS was 5.0 days in the intervention group and 5.4 days after standard care.
Colorectal Surgery
Three trials included patients undergoing colorectal resections and compared a prehabilitation intervention with a control group.13,25,30 The study by Gillis et al. included a total of 77 patients. The indication for surgery in this trial was nonmetastatic colorectal cancer. Sixty-three percent of patients had colonic resections, while the remaining 37% rectal resections. The 38 patients in the experimental group completed a program of at least three individually balanced 50-min exercise sessions per week over a period of 4 weeks and were compared with 39 patients who had no exercise intervention and served as the control group. The primary outcome of this study was the functional walking capacity as measured by the 6-min walk test (6MWT) at 8 weeks after surgery. The mean walking distance increased by 23.4 m in the patients with prehabilitation, whereas in the control group the 6MWT was 21.8 m lower than before surgery. This difference between the two groups was statistically significant (p = 0.02). The study also analyzed perioperative outcomes but found no significant differences. The authors reported a 31.8% overall complication rate according to the Dindo–Clavien classification, a 2.6% rate of pulmonary complications, and a mean LOS of 4.0 days in the prehabilitation group, compared with 43.6%, 2.6%, and 4.0 days, respectively, in the control group (p = 0.28 for overall complications, p = n.a. for pulmonary complications, and p = 0.45 for LOS).
Dronkers et al. performed an exploratory trial without a prespecified primary endpoint to investigate the effect of preoperative training in patients undergoing elective colon resection for various benign and malignant indications. The intervention group consisted of 22 patients who underwent two 60-min training sessions per week for 2 to 4 weeks preoperatively. This group was compared with a control group consisting of 20 patients who were only advised to do unspecified physical exercise. Respiratory muscle endurance increased significantly in the intervention group. However, no difference was found for the timed-up-and-go test or quality of life questionnaires. The authors evaluated clinical outcomes including overall postoperative complications (not clearly defined: prehabilitation 40.1% vs. control 40.0%; p = 0.65), pulmonary complications (prehabilitation 22.7% vs. control 25.0%; p = 0.93), and mean LOS (prehabilitation 16.2 days vs. control 21.6 days; p = 0.31).
Kim et al. performed an exploratory trial in patients undergoing colorectal surgery and included 21 patients, of whom 14 underwent a preoperative training program over 4 weeks, including aerobic exercise on an ergometer, supervised by physical therapists. The intervention group showed a significant increase of 26% in peak power output on exercise, while the control group showed no change (p < 0.05). This trial did not report any further clinical outcomes of the included patients, so it was excluded from further quantitative analyses due to the lack of clinical data.
Gastroesophageal Surgery
Only one of the studies identified evaluated preoperative training in patients with esophageal cancer.29 It included 63 patients who underwent esophagectomy with gastric tube reconstruction for esophageal cancer. Of these, three patients were excluded from the final analysis because of withdrawal of consent (one patient) and major complications (bilateral recurrent nerve palsy and esophagopulmonary fistula; one patient in each group). Hence, 30 patients in each group were analyzed. The intervention group received prehabilitation for more than 7 days consisting of five 60-min sessions per week of multimodal training therapy including respiratory muscle training, breathing and coughing training, muscle strengthening, and ergometer training. The primary outcome of this study was the rate of postoperative pulmonary complications, defined by the Dindo–Clavien classification. Postoperative pulmonary complications were found to be significantly lower in the prehabilitation group (26.7% grade II–IV complications vs. 60.0% in the control group; p = 0.014). Furthermore, on multivariate analysis, the absence of preoperative training was identified as an independent risk factor for postoperative pulmonary complications. Non-pulmonary complications were not reported in this study.
Major Abdominal Surgery
The remaining two studies evaluated the effect of prehabilitation in major abdominal surgery for various indications.12,14 Major abdominal surgery was defined as operations including at least one gastrointestinal anastomosis or involving parenchymal resection of the pancreas or liver. The study by Soares et al. included 32 patients receiving gastric, esophageal, or biliary surgery. Sixteen patients in the interventional group underwent prehabilitation over a period of 2 to 3 weeks with two 50-min sessions per week, while 16 patients served as controls and were given standard care only. The prehabilitation group showed better pulmonary and physical function parameters after the surgical intervention than the control group (respiratory muscle endurance 7 days after surgery, 22 cmH2O vs. 13 cmH2O, p = 0.01; 6MWT distance 7 days after surgery, 368.5 m vs. 223.0 m, p = 0.025). Furthermore, the preoperative exercise intervention led to a significant reduction in pulmonary complications (prehabilitation 31.3%, control 68.8%; p = 0.034). The median LOS was the same (8.5 days) in each group, but interquartile ranges showed a tendency towards shorter LOS in the prehabilitation group.
The second study, by Barberan-Garcia et al., included a total of 125 patients who underwent elective major abdominal surgery for various indications. Sixty-three patients had preoperative training over a period of 6 weeks comprising one to three 50-min sessions per week, while 62 were randomized to standard care without prehabilitation. The study was a confirmatory trial with a predefined primary outcome and sample size calculation. The primary outcome was the overall postoperative complication rate according to the classification of the European Society of Anaesthesiology and the European Society of Intensive Care Medicine. Prehabilitation significantly reduced postoperative complications (prehabilitation 31.0%, control 62.0%; p = 0.001). Pulmonary complications did not differ significantly between the groups but were lower in the prehabilitation group (prehabilitation 6.5%, control 15.9%; p = 0.155). Furthermore, mean LOS was shorter in the exercise group than in the control group, albeit without reaching statistical significance (prehabilitation 8 days vs. control 13 days; p = 0.078).
Risk of Bias Assessment
The risk of bias among the studies was assessed using the Cochrane tool for risk of bias,23 as only RCT were included in this systematic review. The process of random sequence generation and allocation concealment was adequately described and performed in five of the seven included studies (Fig. 2). The other two trials lacked information, resulting in an unclear risk of bias. Due to the nature of an exercise intervention, it was not possible to blind the patients included in the studies. One of the studies blinded the surgery and anesthesia personnel during the operation,14 while two studies mentioned a lack of blinding of performance personnel.12,25 The other four studies offered no information on blinding. The outcome assessors were blinded in three of the trials,13,14,25 while one trial used unblinded outcome assessment,12 resulting in a high risk of bias. However, it is still unclear how a lack of blinding affects outcomes in surgical trials.32 The risk of incomplete outcome data was low in four of the included trials.13,14,25,26 Two of the studies exhibited a high risk of selective reporting.28,29 Overall, four of the included trials showed low to minimal risk of bias,13,14,25,26 whereas three studies exhibited a moderate to high overall risk of bias.12,28,29 Funnel plots of the analyzed outcomes showed no asymmetry, resulting in a low risk of publication bias across all included studies.
Overall Postoperative Morbidity
Five of the included trials provided data on overall postoperative complication rates, and two of them used the predefined Clavien–Dindo classification.13,26 Only one of the trials reported the period in which postoperative morbidity was assessed, namely 30-day morbidity.13 The mean complication rates across all studies were 30.1% in the prehabilitation group and 45.4% in the control group. A meta-analysis (Fig. 3) showed a significant reduction in overall postoperative complications in the prehabilitation group compared with the controls (OR 0.52; 95% CI 0.30 to 0.88; p = 0.01; I2 = 15%).
Pulmonary Complications
Of the seven included trials, six reported data on postoperative pulmonary complications. There were clear definitions of pulmonary complications in most studies. The only study to categorize this subgroup of complications was the one by Yamana et al. using the Clavien–Dindo classification.29 The overall pulmonary complication rates were 13.4% in the prehabilitation group and 26.2% in the control group. The meta-analysis of postoperative pulmonary complications (Fig. 4) showed a significantly lower complication rate after prehabilitation than in the control group (OR 0.37; 95% CI 0.20 to 0.67; p = 0.001; I2 = 0%).
Length of Hospital Stay
The LOS was reported in six of the seven included studies and ranged from a mean of 4 days in both groups in the study by Gillis et al. to a mean of 21.6 days in the control group of the study by Dronkers et al. The mean LOS across all studies was 8.7 days in the prehabilitation group and 11.8 days in the control group. A meta-analysis of the LOS (Fig. 5) showed no significant differences between the two groups (MD − 0.58; 95% CI − 1.28 to 0.13; p = 0.11; I2 = 56%).
Discussion
Prehabilitation including exercise training prior to major abdominal surgery seems a promising preoperative intervention to positively influence the postoperative course of the patients. Recent studies have shown that the incidence of postoperative pulmonary complications is substantial after major abdominal surgery.15,33 Preoperative physical exercise is known to exert a positive influence on pulmonary function parameters,34,35 and consequently exercise and training methods to improve pulmonary or aerobic endurance have been the focus of prehabilitation programs.12 Our systematic review and meta-analysis not only confirmed the high rate of pulmonary complications reported previously15,33 but confirmed a significant reduction in postoperative pulmonary complications that was not evident in some of the individual trials.
Similarly, with regard to overall postoperative complications, most individual trials failed to show a significant reduction13,25,26,28 after prehabilitation. A meta-analysis, however, revealed a significant improvement in postoperative morbidity for prehabilitation (Fig. 3). Interestingly, RCT including patients undergoing more complication-prone surgeries such as esophageal resections showed greater reductions in overall complications than the RCT including patients undergoing colorectal or liver resections. Therefore, aerobic exercise prehabilitation may be effective in abdominal surgery in general, but even more so in particular subgroups. However, the number of patients was too low for further subgroup analyses. Therefore, further studies are needed to identify the patients that benefit most from prehabilitation.
Given the positive effect on pulmonary complications and overall morbidity, it was surprising that, according to our meta-analyses, the mean LOS after surgery was not significantly influenced by prehabilitation. This may be explained by the multiple factors, including nonmedical aspects, that influence the LOS. LOS has come under scrutiny as a quality indicator,36 and new, more valid and reliable measures such as time to readiness for discharge have been developed for use in clinical trials.37
Unfortunately, all other postoperative outcomes, such as rate of reoperation, rate of postoperative ileus, mortality, and quality of life, were reported so sparsely that quantitative synthesis was not possible. Thus, more evidence is needed to elucidate these aspects. Another important factor in modern multimodal cancer therapy, namely the presence of neoadjuvant chemotherapy, was reported too inaccurately, if at all, among the included studies to permit further evaluation of the effect of prehabilitation under these circumstances. Delaying surgery in cancer patients in order to perform prehabilitation is controversial, as it may have detrimental effects on oncologic outcome and tumor progression.38 Therefore, given the increasing number of indications for neoadjuvant therapy, prehabilitation warrants further investigation in this setting, as the period of neoadjuvant treatment would offer a unique opportunity for preoperative physical improvement.
Our study has several limitations. First, all of the studies lacked blinding of participants and very few of them blinded the outcome assessors. While the first is notoriously difficult to achieve in exercise interventions, the latter is a concern, as it may well have biased outcome assessment. Second, although the standardization of the physical intervention was well defined within each trial, the variability between studies was immense. For example, the trial by Barberan-Garcia et al.14 offered a very low exercise intensity with a range of only one to three sessions per week and the distribution of training sessions between the patients was not reported, while the study by Yamana et al.29 employed more intensive training with five sessions per week lasting 60 min each. Third, all studies adapted physical interventions to the patient-specific baseline level, i.e., they put patients on a personalized exercise program. Although this is a clinical routine, the intensity of physical exercise varied considerably within the intervention groups. Similarly, given the nonblinded study design, it cannot be excluded that patients in the control group performed considerable physical exercise of their own accord. Future studies will need to accurately document physical activity in both groups, e.g., with the help of pedometers or activity trackers, which have become widely available in recent years. Another important factor in exercise training studies is patient adherence to the intervention. Three of the included trials12,14,28 included no data on training adherence. In other studies, the rate of completed exercise sessions was remarkably high, confirming the feasibility of prehabilitation in abdominal surgery. Finally, the quantitative analysis and its results are based on a heterogeneous patient cohort including various indications and surgical interventions. Subgroup analyses would be desirable but unfortunately could not be performed due to a lack of data and studies for single indications. In any case, the results regarding the postoperative overall and pulmonary complications seem to be consistent over the included RCT, so it may be that the number of patients in the individual studies was too low for a relevant effect. Furthermore, as mentioned before, the subgroups that may benefit most from prehabilitation still have to be defined.
One of the strengths of our study is the application of clear inclusion and exclusion criteria and the focus on RCT. Furthermore, we defined a standardized physical training as an inclusion criterion in the intervention group and absence of physical training as an inclusion criterion in the control group to clearly assess the efficacy of physical exercise. Therefore, then RCT had to be excluded after the screening process as they either performed no physical exercise intervention in the experimental group,16,34,39,40,41,42,43 or they compared different types of training in the two groups.11,44,45 The fact that this systematic review shows significant reductions not only in postoperative pulmonary complications but also in the overall morbidity in well-defined intervention and control groups substantiates the hypothesis that physical exercise prehabilitation may have a beneficial effect in patients undergoing major abdominal surgery.
This systematic review and meta-analysis provide the latest evidence on perioperative optimization via physical exercise in abdominal surgery. There have been previous systematic reviews on this topic, but with a markedly different focus. Bruns et al.18 analyzed the effect of physical prehabilitation in patients older than 60 years undergoing colorectal surgery and found no differences between their groups. Hijazi et al.46 investigated prehabilitation before abdominal surgery in a descriptive systematic review, but also included observational studies and did not perform quantitative analyses of the data. Most recently, Bolshinsky et al.47 and Luther et al.19 both reviewed different kinds of prehabilitation programs, but also included nutritional supplementation and smoking cessation. Again, neither study performed quantitative analyses. Finally, Moran et al. analyzed a very heterogeneous pool of studies, including trials with only IMT prehabilitation and no physical exercise at all in the intervention group as well as RCT comparing different types of physical exercise interventions in the intervention and control groups. They concluded that prehabilitation can decrease overall and pulmonary postoperative complications.17
Our analyses show that prehabilitation schemes are heterogeneous and trials exhibit meaningful risks of bias as well as lack of detailed patient outcome data. Future trials should target these flaws by offering detailed perioperative data on well-designed physical exercise intervention groups compared with standard care control groups.
Another important factor in evaluating postoperative morbidity is the use of well-defined and standardized definitions and a system to classify the severity of morbidity. Only the trials by Gillis and Dunne13,26 used the internationally accepted Clavien–Dindo classification system for assessment of the overall postoperative morbidity. Furthermore, for the subgroup of pulmonary morbidity, only Yamana et al.29 applied a clear definition of pulmonary complications. This is important, as different outcome definitions may lead to marked differences in complication rates. Thus, standardization of outcome parameters should be one of the main considerations in future studies.
Conclusion
Prehabilitation including a physical exercise intervention can lead to a reduction of postoperative pulmonary complications as well as overall morbidity compared with standard care in patients undergoing major abdominal surgery. The heterogeneity of physical exercise interventions is quite high, and the reporting quality of recently published trials is low. Therefore, further well-designed RCT including a standardized prehabilitation strategy and offering detailed perioperative outcome data, especially in high-risk patient collectives undergoing major abdominal surgery, are needed for further evaluation of the positive effects of physical exercise prehabilitation.
References
Straatman, J., et al., Predictive Value of C-Reactive Protein for Major Complications after Major Abdominal Surgery: A Systematic Review and Pooled-Analysis. PLoS One, 2015. 10(7): p. e0132995.
Cunningham, D., et al., Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med, 2006. 355(1): p. 11-20.
Ychou, M., et al., Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol, 2011. 29(13): p. 1715-21.
Mariette, C., et al., Hybrid Minimally Invasive Esophagectomy for Esophageal Cancer. N Engl J Med, 2019. 380(2): p. 152-162.
Smith, P.R., et al., Postoperative pulmonary complications after laparotomy. Respiration, 2010. 80(4): p. 269-74.
Visioni, A., et al., Enhanced Recovery After Surgery for Noncolorectal Surgery?: A Systematic Review and Meta-analysis of Major Abdominal Surgery. Ann Surg, 2018. 267(1): p. 57-65.
Carli, F. and C. Scheede-Bergdahl, Prehabilitation to enhance perioperative care. Anesthesiol Clin, 2015. 33(1): p. 17-33.
Wynter-Blyth, V. and K. Moorthy, Prehabilitation: preparing patients for surgery. BMJ, 2017. 358: p. j3702.
Singh, F., et al., A systematic review of pre-surgical exercise intervention studies with cancer patients. Surg Oncol, 2013. 22(2): p. 92-104.
Moyer, R., et al., The Value of Preoperative Exercise and Education for Patients Undergoing Total Hip and Knee Arthroplasty: A Systematic Review and Meta-Analysis. JBJS Rev, 2017. 5(12): p. e2.
Carli, F., et al., Randomized clinical trial of prehabilitation in colorectal surgery. Br J Surg, 2010. 97(8): p. 1187-97.
Soares, S.M., et al., Pulmonary function and physical performance outcomes with preoperative physical therapy in upper abdominal surgery: a randomized controlled trial. Clin Rehabil, 2013. 27(7): p. 616-27.
Gillis, C., et al., Prehabilitation versus rehabilitation: a randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology, 2014. 121(5): p. 937-47.
Barberan-Garcia, A., et al., Personalised Prehabilitation in High-risk Patients Undergoing Elective Major Abdominal Surgery: A Randomized Blinded Controlled Trial. Ann Surg, 2018. 267(1): p. 50-56.
Boden, I., et al., Preoperative physiotherapy for the prevention of respiratory complications after upper abdominal surgery: pragmatic, double blinded, multicentre randomised controlled trial. BMJ, 2018. 360: p. j5916.
Parikh, M., et al., Does a preoperative medically supervised weight loss program improve bariatric surgery outcomes? A pilot randomized study. Surg Endosc, 2012. 26(3): p. 853-61.
Moran, J., et al., The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: A systematic review and meta-analysis. Surgery, 2016. 160(5): p. 1189-1201.
Bruns, E.R., et al., The effects of physical prehabilitation in elderly patients undergoing colorectal surgery: a systematic review. Colorectal Dis, 2016. 18(8): p. O267-77.
Luther, A., et al., The Impact of Total Body Prehabilitation on Post-Operative Outcomes After Major Abdominal Surgery: A Systematic Review. World J Surg, 2018. 42(9): p. 2781-2791.
Treanor, C., T. Kyaw, and M. Donnelly, An international review and meta-analysis of prehabilitation compared to usual care for cancer patients. J Cancer Surviv, 2018. 12(1): p. 64-73.
Panic, N., et al., Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLoS One, 2013. 8(12): p. e83138.
Goossen, K., et al., Optimal literature search for systematic reviews in surgery. Langenbecks Arch Surg, 2018. 403(1): p. 119-129.
Higgins, J.P., et al., The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ, 2011. 343: p. d5928.
Hozo, S.P., B. Djulbegovic, and I. Hozo, Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol, 2005. 5: p. 13.
Dronkers, J.J., et al., Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: a randomized controlled pilot study. Clin Rehabil, 2010. 24(7): p. 614-22.
Dunne, D.F., et al., Randomized clinical trial of prehabilitation before planned liver resection. Br J Surg, 2016. 103(5): p. 504-12.
Gillis, C., et al., Prehabilitation with Whey Protein Supplementation on Perioperative Functional Exercise Capacity in Patients Undergoing Colorectal Resection for Cancer: A Pilot Double-Blinded Randomized Placebo-Controlled Trial. J Acad Nutr Diet, 2016. 116(5): p. 802-12.
Kaibori, M., et al., Perioperative exercise for chronic liver injury patients with hepatocellular carcinoma undergoing hepatectomy. Am J Surg, 2013. 206(2): p. 202-9.
Yamana, I., et al., Randomized Controlled Study to Evaluate the Efficacy of a Preoperative Respiratory Rehabilitation Program to Prevent Postoperative Pulmonary Complications after Esophagectomy. Dig Surg, 2015. 32(5): p. 331-7.
Kim, D.J., et al., Responsive measures to prehabilitation in patients undergoing bowel resection surgery. Tohoku J Exp Med, 2009. 217(2): p. 109-15.
Dindo, D., N. Demartines, and P.A. Clavien, Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg, 2004. 240(2): p. 205-13.
Probst, P., et al., Blinding in randomized controlled trials in general and abdominal surgery: protocol for a systematic review and empirical study. Syst Rev, 2016. 5: p. 48.
Zingg, U., et al., Factors associated with postoperative pulmonary morbidity after esophagectomy for cancer. Ann Surg Oncol, 2011. 18(5): p. 1460-8.
Barbalho-Moulim, M.C., et al., Effects of preoperative inspiratory muscle training in obese women undergoing open bariatric surgery: respiratory muscle strength, lung volumes, and diaphragmatic excursion. Clinics (Sao Paulo), 2011. 66(10): p. 1721-7.
Limongi, V., et al., Effects of a respiratory physiotherapeutic program in liver transplantation candidates. Transplant Proc, 2014. 46(6): p. 1775-7.
Lingsma, H.F., et al., Evaluation of hospital outcomes: the relation between length-of-stay, readmission, and mortality in a large international administrative database. BMC Health Serv Res, 2018. 18(1): p. 116.
Fiore, J.F., Jr., et al., Time to readiness for discharge is a valid and reliable measure of short-term recovery after colorectal surgery. World J Surg, 2013. 37(12): p. 2927-34.
Curtis, N.J., et al., Time from colorectal cancer diagnosis to laparoscopic curative surgery-is there a safe window for prehabilitation? Int J Colorectal Dis, 2018. 33(7): p. 979-983.
Kulkarni, S.R., et al., Pre-operative inspiratory muscle training preserves postoperative inspiratory muscle strength following major abdominal surgery - a randomised pilot study. Ann R Coll Surg Engl, 2010. 92(8): p. 700-7.
Bond, D.S., et al., Bari-Active: a randomized controlled trial of a preoperative intervention to increase physical activity in bariatric surgery patients. Surg Obes Relat Dis, 2015. 11(1): p. 169-77.
Baillot, A., et al., Impacts of Supervised Exercise Training in Addition to Interdisciplinary Lifestyle Management in Subjects Awaiting Bariatric Surgery: a Randomized Controlled Study. Obes Surg, 2016. 26(11): p. 2602-2610.
Llorens, J., et al., Preoperative inspiratory muscular training to prevent postoperative hypoxemia in morbidly obese patients undergoing laparoscopic bariatric surgery. A randomized clinical trial. Obes Surg, 2015. 25(6): p. 1003-9.
Haasenritter, J., et al., [Impact of a pre-operative mobilisation program using the Viv-Arte training model based on kinesthetic mobilisation on mobility, pain, and post-operation length of stay of patients receiving an elective medial laparotomy: a prospective, randomised, controlled pilot study]. Pflege, 2009. 22(1): p. 19-28.
Mayo, N.E., et al., Impact of preoperative change in physical function on postoperative recovery: argument supporting prehabilitation for colorectal surgery. Surgery, 2011. 150(3): p. 505-14.
van Adrichem, E.J., et al., Comparison of two preoperative inspiratory muscle training programs to prevent pulmonary complications in patients undergoing esophagectomy: a randomized controlled pilot study. Ann Surg Oncol, 2014. 21(7): p. 2353-60.
Hijazi, Y., U. Gondal, and O. Aziz, A systematic review of prehabilitation programs in abdominal cancer surgery. Int J Surg, 2017. 39: p. 156-162.
Bolshinsky, V., et al., Multimodal Prehabilitation Programs as a Bundle of Care in Gastrointestinal Cancer Surgery: A Systematic Review. Dis Colon Rectum, 2018. 61(1): p. 124-138.
Funding
The resources and facilities of the University of Heidelberg were used in conducting this study. No additional funding was applied for or received.
Author information
Authors and Affiliations
Contributions
PH and ALM developed the study concept. MKD, PP, JW, and KS helped to develop the study concept and gave methodological advice. PH and ALM carried out the literature search and data extraction. PH and ALM conducted statistical analyses. PH and ALM wrote the first draft of the manuscript. MKD, PP, JW, and KS provided scientific input for the study’s background and rationale and contributed to interpretation of the data. All authors read, critically revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
: Example of a search strategy for MEDLINE (via PubMed). (DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Heger, P., Probst, P., Wiskemann, J. et al. A Systematic Review and Meta-analysis of Physical Exercise Prehabilitation in Major Abdominal Surgery (PROSPERO 2017 CRD42017080366). J Gastrointest Surg 24, 1375–1385 (2020). https://doi.org/10.1007/s11605-019-04287-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04287-w