Abstract
Purpose
Over the last 3 decades, laparoscopic procedures have emerged as the standard treatment for many elective and emergency surgical conditions. Despite the increased use of laparoscopic surgery, the role of laparoscopic repair for perforated peptic ulcer remains controversial among general surgeons. The aim of this study was to compare the outcomes of laparoscopic versus open repair for perforated peptic ulcer.
Methods
A systemic literature review was conducted using Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. A search was conducted using MEDLINE, EMBASE, PubMed and Cochrane Database of all randomised controlled trials (RCT) that compared laparoscopic (LR) with open repair (OR) for perforated peptic ulcer (PPU). Data was extracted using a standardised form and subsequently analysed.
Results
The meta-analysis using data from 7 RCT showed that LR for PPU has decreased overall post-operative morbidity (LR = 8.9% vs. OR = 17.0%) (OR = 0.54, 95% CI 0.37 to 0.79, p < 0.01), wound infections, (LR = 2.2% vs. OR = 6.3%) (OR = 0.3, 95% CI 0.16 to 0.5, p < 0.01) and shorter duration of hospital stay (6.6 days vs. 8.2 days, p = 0.01). There were no significant differences in length of operation, leakage rate, incidence of intra-abdominal abscess, post-operative sepsis, respiratory complications, re-operation rate or mortality. There was no publication bias and the quality of the studies ranged from poor to good.
Conclusion
These results demonstrate that laparoscopic repair for perforated peptic ulcer has a reduced morbidity and total hospital stay compared with open approach. There are no significant differences in mortality, post-operative sepsis, abscess and re-operation rates. LR should be the preferred treatment option for patients with perforated peptic ulcer disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prior to the twentieth century, perforated peptic ulcer (PPU) was a rare but invariably fatal disease.1,2 The incidence of PPU has steadily increased over the past few decades, predominantly among the elderly population.1,2 Surgical repair at laparotomy using a variety of surgical techniques is the usual treatment for PPU3,4,5,6 with laparoscopic repair (LR) first reported in 1990.3
The proposed advantages of LR compared with open repair (OR) are a reduction in overall mortality and morbidity including post-operative wound infection, post-operative pain and length of stay (LOS).4,5 There have been multiple studies, including randomised controlled trials (RCT), cohort studies and case-controlled studies, published in recent years which have compared the two techniques with no clear benefit demonstrated for either operative technique.1,2 Four previous meta-analyses found that LR had superior short-term benefits of reduced post-operative pain and reduced wound morbidity.4,5,6,7 They were unable to demonstrate any effect on overall morbidity, mortality or LOS, and concluded more RCT were needed.4,5,6,7,8 The lack of conclusive studies and concerns related to longer operative time and leakage rate4,5 has resulted in a low uptake of LR as the preferred method of repair. The aim of this study was to compare LR and OR for the surgical treatment of PPU and provide evidence-based guidance to the selection of the most appropriate operative technique.
Methods
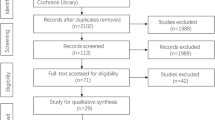
A systematic search was conducted following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines.9 The following databases were searched for relevant studies: PubMed (from 1946), EMBASE (from 1949), Google Scholar and Google. The search terms used were “laparoscopic”, “laparoscopy”, “peptic ulcer perforation”, “gastric ulcer perforation”, “duodenal ulcer perforation” and “open” were used in combinations. The reference lists of selected articles were searched for relevant studies. There were no language restrictions. All RCT that compared LR with OR for peptic ulcer perforation from 1990 to 2017 were included in this meta-analysis for further data analysis. All other non-randomised studies such as cohort studies, case control studies, case reports and case series were excluded.
The data were extracted and critically appraised by two independent authors (GS and GE). The following data were extracted using a standardised data extraction form. Patient characteristics included age, gender, ASA classification, history of previous peptic ulcer, history of NSAID use, location of perforation and size of perforation. Primary outcomes included conversions from LR to OR and various types of morbidity and mortality. Secondary outcomes included post-operative pain, LOS, solid food resumption, insertion of nasogastric tube (NGT) and return to daily activities.
Pooled odds ratios and 95% confidence intervals were calculated for patient outcomes for PPU using a random effects model.10 Weighted mean difference was calculated for continuous variables such as mean operating time and total length of hospital stay.11 Relative risk ratio was calculated for dichotomous variables such as post-operative complications and mortality.11 Intention to treat analysis was performed where patients were converted from LR to OR or when there were missing data. Yates’s half correction was used in studies that reported no events for outcomes.11,12 Heterogeneity was tested with Cochran’s Q statistic, with p < 0.10 indicating heterogeneity, and the degree of heterogeneity was quantified using the I2 statistic, which represents the percentage of the total variability across studies which is due to heterogeneity.12,13 I2 values of 25, 50 and 75% corresponded to low, moderate and high degrees of heterogeneity respectively.12,13 A funnel plot analysis was performed to assess publication bias. The overall quality of each trial was assessed with the Jadad score.14 One of the authors (GE) who is an experienced biostatistician performed all statistical analyses.
Results
The literature search generated a total of 321 articles. Out of this, articles were excluded based on titles, abstracts, full texts or a combination of these. Finally, seven RCT were included in this meta-analysis (Fig. 1).15,16,17,18,19,20,21
The total number of patients were 631 with 319 patients in the LR group and 312 patients in the OR group (Table 1). There was no publication bias noted. The quality of the studies ranged from 1 to 3 based on Jadad scores with four studies having a score of three and two studies considered poor with a score of one (Table 1). The average age of patients was 53 years in both groups. Approximately two-thirds of the patients were male. There were no significant differences between the two groups for ASA classification, history of previous peptic ulcer or history of NSAID usage (Table 2). The most frequent site of perforation was duodenal (312 patients, 49.4%), followed by gastric (97 patients, 15.4%) and juxtapylorus (79 patients, 12.5%). The site of the perforation was not defined in 143 (22.7%) patients. There was no significant difference in perforation site between the two groups (Table 2). There was no difference in the mean size of the perforation between the LR (6.6 mm) and OR (5.2 mm) (p = 0.23).
Primary Outcomes
All studies reported the incidence of conversions from LR to OR. A total of 28 patients (9.4%) in the LR group needed a conversion to OR. The most common reason for conversion to open repair was failure to repair the perforation either due to technical difficulties or size of the perforation (n = 16, 57.1%). This is followed by conversion due to extensive peritoneal adhesions (n = 6, 21.4%), the patient being unstable during the operation (n = 5, 17.9%), failure to find the perforation (n = 4, 14.3%) and indication not defined (n = 2, 7.1%). These patients were included in the analysis on an intention-to-treat analysis.
Six studies reported the incidence of post-operative morbidity.15,17,18,19,20,21 The overall morbidity was significantly lower in the LR group (8.9%) compared to the OR group (17.0%), (RR = 0.54, 95% CI = 0.37–0.79, p < 0.01) (Fig. 2, Table 3). The reported complications in most studies were wound, respiratory, cardiac, incisional hernia, sepsis, leakage, intra-abdominal abscess, ileus, urinary tract infection and cerebral vascular accident (Table 3).
Six studies reported the incidence of wound complications.15,17,18,19,20,21 The wound infection rate was significantly lower in the LR arm (n = 14, 2.2%) compared to the OR arm (n = 40, 6.3%) (Table 3, Fig. 3). In the random effects model, the overall incidence of wound complications was significantly lower in the LR group (OR = 0.3, 95% CI = 0.17–0.55, p < 0.01). There was no evidence of statistical heterogeneity (I2 = 0%, p = 0.87).
Four studies reported the incidence of post-operative leakage.15,17,19,21 There were 7 (1.1%) patients in the LR group and 2 (0.3%) patients in the OR group that developed leakage post-operatively. In the random effects model, the incidence of leakage was higher in the LR group, but it was not statistically significant (Table 3). There was no evidence of statistical heterogeneity (I2 = 0%, p = 0.64).
Six studies reported the incidence of intra-abdominal abscess (IAA).15,17,18,19,20,21 Six (1%) patients in the LR group and 11 (1.7%) patients in the OR group developed an intra-abdominal abscess which was not statistically significant (Table 3). There was evidence of statistical heterogeneity (I2 = 35.59%, p = 0.17). Only two studies reported the incidence of post-operative sepsis.20,21 Five (0.8%) patients in the LR group and 3 (0.5%) patients in the OR group developed sepsis post-operatively. In the random effects model, there was no significant difference in the incidence of post-operative sepsis (Table 3). There was no evidence of statistical heterogeneity (I2 = 0%, p = 0.51).
Four studies reported the incidence of post-operative ileus.15,17,20,21 Four (0.6%) patients in the LR group and 9 (1.4%) patients in the OR group developed a post-operative ileus which was not statistically significant (Table 3). There was no evidence of statistical heterogeneity (I2 = 0%, p = 0.9).
Four studies reported the incidence of incisional hernia.15,18,19,21 No patients in the LR group developed an incisional hernia compared to 4 (0. 6%) patients in the OR group. This difference was not statistically significant (Table 3) and there was no evidence of statistical heterogeneity (I2 = 0%, p = 1).
Five studies reported the incidence of respiratory complications.15,17,18,20,21 A total of 1.4% (n = 9) of patients in the LR group and 2.7% (n = 17) of patients in the OR group developed post-operative respiratory complications. This included eight cases of pneumonia in the LR arm and 13 cases of pneumonia in the OR arm (Table 3). In the random effects model, the incidence of respiratory complications was not significantly different (Table 3). Although there was evidence of statistical heterogeneity, it was not significant (I2 = 14.39%, p = 0.32).
Three studies reported the incidence of re-operation.15,17,20 Seven (1.1%) patients in the LR group required re-operation compared to 3 (0.5%) patients in the OR group with no significant difference between the groups (Table 3). There was no evidence of statistical heterogeneity (I2 = 16.490%, p = 0.49).
Four studies reported the mortality rate15,17,20,21 with 6 (1%) patients in the LR group and 9 (1.4%) patients in the OR group. There was no significant difference between groups (Table 3, Fig. 4). There was no evidence of statistical heterogeneity (I2 = 0%, p = 0.98). The reported causes of mortality were multi-organ failure, respiratory failure, sepsis, leakage and cerebral vascular accident.
Secondary Outcomes
The secondary outcomes including operative duration, LOS, post-operative pain, solid food resumption, NGT duration, return to daily activities, mean operative time and mean size of perforation are summarised in Table 4. Seven studies reported the operative duration.15,16,17,18,19,20,21 There was no significant difference between the LR group (mean 72.9 min) and the OR group (mean 59.6 min) (p = 0.73). Six studies reported the LOS15,17,18,19,20,21 with the average LOS was significantly lower for the LR group (5.3 ± 1.5 days) compared to the OR group (6.9 ± 1.3 days) (p = 0.01). Four studies reported on post-operative pain.15,17,20,21 Three studies used visual analogue scale (VAS) on day 1 post-operative.15,17,21 The average VAS in the LR group is 3.8 compared with 5.2 in the OR group (p < 0.001). There was no significant difference between LR and OR for solid food resumption, nasogastric tube use and return to normal activities (Table 4).
Discussion
Laparoscopic surgery is being used increasingly in many aspects of emergency gastrointestinal surgery, including appendectomy and cholecystectomy.22,23,24 The advantages of laparoscopic surgery include decreased overall morbidity, mortality, cost, LOS and post-operative pain with an earlier return to work and resumption of normal daily activity.22,23,24,25,26 The results of this meta-analysis show a significant benefit in performing LR in PPU with a significant reduction in the overall post-operative morbidity, post-operative wound infection and a shorter LOS in the LR group compared to the OR group. There was no difference in the mortality rate or in the incidence of respiratory complications, IAA, ileus, incisional hernia, cardiac complications and urinary tract infection. Similarly, there was no significant difference in the length of NGT insertion, solid food resumption and return to daily activities. These results support the premise that LR should be the routine surgical treatment for PPU.
Three recent meta-analyses have reported a reduced wound infection rate but did not demonstrate a reduced overall morbidity and LOS for LA.4,7,8 These studies only used three,8 four4 or five7 RCT in their analysis with each study concluding that more RCT were required to clarify any benefit for LA. The addition of two recent RCT19,20 in our analysis has provided the additional data required to demonstrate the significantly reduced overall morbidity and LOS.
The use of laparoscopic surgical techniques in emergency surgery was controversial in the early 1990s due to concerns of risk of bacteraemia and endotoxaemia in the presence of abdominal sepsis.25 It was thought that establishing carbon dioxide pneumoperitoneum increased the risk of bacteraemia due to the increased in abdominal pressure.25 This was a particular concern in PPU where patients generally present with abdominal sepsis and generalised peritonitis. However, this theory was disproved in studies assessing the laparoscopic treatment of generalised peritonitis.27,28 The current study demonstrates no significant difference in the incidence of sepsis or intra-abdominal collections between LR and OR. Based on the current study results, an RCT to demonstrate a 30% reduction in sepsis or intra-abdominal abscess in LR would require 722 patients in each group.
Elective laparoscopic gastrointestinal surgery is invariably associated with a reduction in post-operative respiratory complications credited to reduced post-operative pain.29,30,31 However, the present study did not reveal the expected reduction in respiratory complications despite being associated with significantly less post-operative pain. This may be due to insufficient case numbers. A more likely explanation is the established peritonitis pre-operatively is a major contributor to post-operative respiratory complications, a contributing factor that is the same for LR and OR.
Another concern for LR in PPU was the higher leakage rate and subsequent formation of IAA persistent post-operative sepsis requiring further interventions reported in early studies.1,2 Our study found no significant difference in the rate of leakage, sepsis and reoperation between the LR and OR groups. The rate of leakage (1.1%) in our study was much lower than that reported in earlier studies (3.8 to 6.9%).32,33 An explanation for the reduction in reported leak rates includes improved laparoscopic techniques, improved equipment and increased laparoscopic surgical expertise. Prior to 2000, the incidence and reports of complex laparoscopic procedures such as pancreatic resection, gastrectomy and complex colonic surgery was low. Twenty years later, these elective laparoscopic resections are considered commonplace and routine.34,35,36 A recent meta-analysis demonstrated a steady, ongoing reduction in post-operative morbidity over time for emergency laparoscopic surgery.37 Similarly, laparoscopic surgery for complicated (gangrenous or perforated) appendicitis was initially associated with a higher morbidity, particularly for IAA,38,39 whereas recent studies have shown laparoscopic surgery has a reduced morbidity and no difference in IAA rate.40,41
An early criticism of LR for PPU was the longer average operating time (OT) associated with LR. Although in this study, the average OT was 13 min longer in the LR group, this was not statistically significant (p = 0.73). When the average OT was further subcategorised to before and after 2000, there was a reduction in average OT after 2000 in the LR group (61.4 min) compared with the OR group (74.3 min). This reflects the increasing use of laparoscopic techniques in gastrointestinal surgery and the improved laparoscopic expertise of surgeons. It is reasonable to expect the average OT of LR to be comparable with OR in coming years as occurred in appendectomy and cholecystectomy,23,24,37 and therefore, a prolonged operating time is no longer a valid argument against LR.
The conversion rate in this study is 9.4% which was much lower than conversion rates reported in earlier studies (12.4–19.1%).32,33 The most common cause of conversion was an inability to repair the ulcer due to either technical difficulties or size of perforation. As with post-operative morbidity rates, the conversion rates have reduced with better laparoscopic skills and experience. This has been demonstrated in other emergency gastrointestinal surgeries such as laparoscopic cholecystectomy for acute cholecystitis where conversion rates in the 1990s were over 20%42 and now range between 2.6 to 7.7%.43,44
Potential confounding factors are the patients’ co-morbidities and the nature of disease resulting in a bias that may favour either LR or OR. As expected for an RCT, all patients’ characteristics in both groups were similar including gender, age, ASA scores and APACHE II scores. There were no significant differences in the history of non-steroidal anti-inflammatory drug (NSAID) usage or history of previous peptic ulcer. The most common place of perforation was duodenal, followed by gastric and juxtapyloric, with the same distribution between the 2 procedures. The average size of perforation was the same for LR and OR.
The average mortality in both LA (1%) and OA (1.4%) is much lower than that reported in population-based studies where the mortality ranges from 25 to 30%.45,46,47 This may indicate that all seven RCT had an inherent bias of selecting patients with a lower risk of morbidity and mortality for randomisation. The number of cases with perforated ulcer disease not selected or randomised was not provided in any of the RCT. Neither were the reasons or outcomes of patients not randomised reported. The overall morbidity (LA = 8.9% and OA = 17%) is lower than that reported in recent studies48,49 adding further evidence to a selection bias. The lower average age of around 53 years compared to the population-based studies ranging 60 to 80 years is further evidence of a selection bias in the RCT. Older age groups have been noted to be an independent predictor of morbidity and mortality in PUD.50,51 Although there may be a selection bias for entry into the RCT that explains the variance in outcomes compared to various case series, it is most unlikely to change the conclusions from this meta-analysis. The improved outcomes for laparoscopic surgery in the current results are most likely to prevail in older patients with more co-morbidities.
Our meta-analysis provides clear evidence that LR is a safe method in treating PU perforation compared with the traditional OR. There is no increased incidence of post-operative leak, sepsis or abscess formation. Furthermore, LA has reduced morbidity, wound infection and LOS. LR should be considered the routine approach for patients presenting with PPUD.
Conclusion
LR is a safe option for treating PPU. It is better than OR with a lower incidence of post-operative morbidity, wound infection and shorter LOS. The laparoscopic approach should be considered the treatment of choice for PPU.
References
Svanes C. Trends in perforated peptic ulcer: incidence, etiology, treatment, and prognosis. World J Surg. 2000;24(3):277–83.
Bertleff MJ, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg. 2010;27(3):161–9.
Mouret P, Francois Y, Vignal J, Barth X, Lombard-Platet R. Laparoscopic treatment of perforated peptic ulcer. Br J Surg. 1990;77(9):1006.
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Meta-analysis of laparoscopic versus open repair of perforated peptic ulcer. JSLS. 2013;17(1):15–22.
Zhou C, Wang W, Wang J, Zhang X, Zhang Q, Li B, et al. An Updated Meta-Analysis of Laparoscopic Versus Open Repair for Perforated Peptic Ulcer. Sci Rep. 2015;5:13976.
Lau H. Laparoscopic repair of perforated peptic ulcer: a meta-analysis. Surg Endosc. 2004;18(7):1013–21.
Tan S, Wu G, Zhuang Q, Xi Q, Meng Q, Jiang Y, et al. Laparoscopic versus open repair for perforated peptic ulcer: A meta analysis of randomized controlled trials. Int J Surg. 2016;33 Pt A:124–32.
Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev. 2013(2):CD004778.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
F Y. Contingency tables involving small numbers and the x2 test. J R Stat Soc. 1934;1(2):217–235
Haviland MG. Yates’s correction for continuity and the analysis of 2 x 2 contingency tables. Stat Med. 1990;9(4):363–7; discussion 9–83.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, Dawson JJ, et al. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. 1996;224(2):131–8.
Lau JY, Lo SY, Ng EK, Lee DW, Lam YH, Chung SC. A randomized comparison of acute phase response and endotoxemia in patients with perforated peptic ulcers receiving laparoscopic or open patch repair. Am J Surg. 1998;175(4):325–7.
Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, et al. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. 2002;235(3):313–9.
Schietroma M, Piccione F, Carlei F, Sista F, Cecilia EM, Amicucci G. Peritonitis from perforated peptic ulcer and immune response. J Invest Surg. 2013;26(5):294–304.
Shah FH, Mehta SG, Gandhi MD, Saraj. Laparoscopic Peptic Ulcer Perforation Closure: the Preferred Choice. Indian J Surg. 2015;77(Suppl 2):403–6.
Ge B, Wu M, Chen Q, Chen Q, Lin R, Liu L, et al. A prospective randomized controlled trial of laparoscopic repair versus open repair for perforated peptic ulcers. Surgery. 2016;159(2):451–8.
Bertleff MJ, Halm JA, Bemelman WA, van der Ham AC, van der Harst E, Oei HI, et al. Randomized clinical trial of laparoscopic versus open repair of the perforated peptic ulcer: the LAMA Trial. World J Surg. 2009;33(7):1368–73.
Jimenez Rodriguez RM, Segura-Sampedro JJ, Flores-Cortes M, Lopez-Bernal F, Martin C, Diaz VP, et al. Laparoscopic approach in gastrointestinal emergencies. World J Gastroenterol. 2016;22(9):2701–10.
Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg. 2012;16(10):1929–39.
Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Di Saverio S, et al. Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg. 2015;18:196–204.
Navez B, Navez J. Laparoscopy in the acute abdomen. Best Pract Res Clin Gastroenterol. 2014;28(1):3–17.
Mandrioli M, Inaba K, Piccinini A, Biscardi A, Sartelli M, Agresta F, et al. Advances in laparoscopy for acute care surgery and trauma. World J Gastroenterol. 2016;22(2):668–80.
Navez B, Tassetti V, Scohy JJ, Mutter D, Guiot P, Evrard S, et al. Laparoscopic management of acute peritonitis. Br J Surg. 1998;85(1):32–6.
Navez B, Delgadillo X, Cambier E, Richir C, Guiot P. Laparoscopic approach for acute appendicular peritonitis: efficacy and safety: a report of 96 consecutive cases. Surg Laparosc Endosc Percutan Tech. 2001;11(5):313–6.
Cox MR, Gunn IF, Eastman MC, Hunt RF, Heinz AW. Open cholecystectomy: a control group for comparison with laparoscopic cholecystectomy. Aust N Z J Surg. 1992;62(10):795–801.
Ephgrave KS, Kleiman-Wexler R, Pfaller M, Booth B, Werkmeister L, Young S. Postoperative pneumonia: a prospective study of risk factors and morbidity. Surgery. 1993;114(4):815–9; discussion 9–21.
Lee C-Z, Kao L-T, Lin H-C, Wei P-L. Comparison of clinical outcome between laparoscopic and open right hemicolectomy: a nationwide study. World J Surg Oncol. 2015;13(250).
Lunevicius R, Morkevicius M. Systematic review comparing laparoscopic and open repair for perforated peptic ulcer. Br J Surg. 2005;92(10):1195–207.
Bertleff MJ, Lange JF. Laparoscopic correction of perforated peptic ulcer: first choice? A review of literature. Surg Endosc. 2010;24(6):1231–9.
Riviere D, Gurusamy KS, Kooby DA, Vollmer CM, Besselink MG, Davidson BR, et al. Laparoscopic versus open distal pancreatectomy for pancreatic cancer. Cochrane Database Syst Rev. 2016;4:CD011391.
Xiong H, Wang J, Jia Y, Ye C, Lu Y, Chen C, et al. Laparoscopic surgery versus open resection in patients with gastrointestinal stromal tumors: An updated systematic review and meta-analysis. Am J Surg. 2017;214(3):538–46.
Celentano V, Giglio MC, Bucci L. Laparoscopic versus open Hartmann’s reversal: a systematic review and meta-analysis. Int J Colorectal Dis. 2015;30(12):1603–15.
Ukai T, Shikata S, Takeda H, Dawes L, Noguchi Y, Nakayama T, et al. Evidence of surgical outcomes fluctuates over time: results from a cumulative meta-analysis of laparoscopic versus open appendectomy for acute appendicitis. BMC Gastroenterol. 2016;16:37.
Krisher SL, Browne A, Dibbins A, Tkacz N, Curci M. Intra-abdominal abscess after laparoscopic appendectomy for perforated appendicitis. Arch Surg. 2001;136(4):438–41.
Paik PS, Towson JA, Anthone GJ, Ortega AE, Simons AJ, Beart RW, Jr. Intra-abdominal abscesses following laparoscopic and open appendectomies. J Gastrointest Surg. 1997;1(2):188–92; discussion 92–3.
Dai L, Shuai J. Laparoscopic versus open appendectomy in adults and children: A meta-analysis of randomized controlled trials. United European Gastroenterol J. 2017;5(4):542–53.
Quah GS EG, Cox MR. . Laparoscopic vs. Open Surgery for Complicated Appendicitis: A Meta-analysis. Aust N Z J Surg 2018;88(S1):55–6.
Cox MR, Wilson TG, Luck AJ, Jeans PL, Padbury RT, Toouli J. Laparoscopic cholecystectomy for acute inflammation of the gallbladder. Ann Surg. 1993;218(5):630–4.
Genc V, Sulaimanov M, Cipe G, Basceken SI, Erverdi N, Gurel M, et al. What necessitates the conversion to open cholecystectomy? A retrospective analysis of 5164 consecutive laparoscopic operations. Clinics (Sao Paulo). 2011;66(3):417–20.
Sakpal SV, Bindra SS, Chamberlain RS. Laparoscopic cholecystectomy conversion rates two decades later. JSLS. 2010;14(4):476–83.
Moller MH, Larsson HJ, Rosenstock S, Jorgensen H, Johnsen SP, Madsen AH, et al. Quality-of-care initiative in patients treated surgically for perforated peptic ulcer. Br J Surg. 2013;100(4):543–52.
Kujath P, Schwandner O, Bruch HP. Morbidity and mortality of perforated peptic gastroduodenal ulcer following emergency surgery. Langenbecks Arch Surg. 2002;387(7–8):298–302.
Bae S, Shim KN, Kim N, Kang JM, Kim DS, Kim KM, et al. Incidence and short-term mortality from perforated peptic ulcer in Korea: a population-based study. J Epidemiol. 2012;22(6):508–16.
Thorsen K, Glomsaker TB, von Meer A, Soreide K, Soreide JA. Trends in diagnosis and surgical management of patients with perforated peptic ulcer. J Gastrointest Surg. 2011;15(8):1329–35.
Lohsiriwat V, Prapasrivorakul S, Lohsiriwat D. Perforated peptic ulcer: clinical presentation, surgical outcomes, and the accuracy of the Boey scoring system in predicting postoperative morbidity and mortality. World J Surg. 2009;33(1):80–5.
Irvin TT. Abdominal pain: a surgical audit of 1190 emergency admissions. Br J Surg. 1989;76(11):1121–5.
Thorsen K, Soreide JA, Soreide K. What is the best predictor of mortality in perforated peptic ulcer disease? A population-based, multivariable regression analysis including three clinical scoring systems. J Gastrointest Surg. 2014;18(7):1261–8.
Author information
Authors and Affiliations
Contributions
G. S. Q.: Study design, data acquisition, analysis and interpretation and manuscript preparation. G. D. E.: Data analysis, manuscript preparation and manuscript approval. M. R. C.: Study design, data interpretation, manuscript preparation and approval.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Quah, G.S., Eslick, G.D. & Cox, M.R. Laparoscopic Repair for Perforated Peptic Ulcer Disease Has Better Outcomes Than Open Repair. J Gastrointest Surg 23, 618–625 (2019). https://doi.org/10.1007/s11605-018-4047-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-4047-8