Abstract
Acquired bronchoesophageal fistula can have their origin in a benign or malign cause. Benign bronchoesophageal fistula is rare and often associated with nonspecific symptoms that may delay the correct diagnosis. The authors present a case of a bronchoesophageal fistula in a 57-year-old woman caused by tuberculosis infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bronchoesophageal fistula (BEF) in adults can arise from mediastinal malignancies as well as from a variety of benign conditions.1 Malignant causes such as esophageal carcinoma or lymphoma are the most common causes. Most benign BEF have a traumatic origin, either from iatrogenic lesions (complication during intubation), blunt and penetrating trauma, radiation, or caustic ingestion. Rarely, infectious diseases can be BEF cause, and among them, tuberculosis is one of the rarest.
Case Report
A 57-year-old woman was referred to our hospital with complaints of dysphagia and recurrent episodes of cough with sputum and fever (39 °C) in the past year, which improves with antibiotics but resorts again after stopping antimicrobial treatment. She denies dyspnea, vomiting, or heartburn. She mentions a weight loss of 5 kg and had a slim and weak appearance. There is no history of recent surgery or trauma.
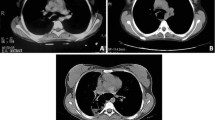
The patient was hospitalized and underwent several diagnostic tests including blood samples, sputum culture, and imaging examines. The X-ray was normal and the thoracic computerized tomography scan showed nonspecific changes. She then performed a gastrografin swallow esophagram that revealed the presence of a high-throughput bronchoesophageal fistula just below the carina with the opacification of the right bronchial tree to the right lung (Fig. 1). The upper gastrointestinal endoscopy (UGE) showed the presence of a fistula in the esophagus with a 2-mm-diameter hole, about 29 cm from de dental arch (Fig. 2). A bronchoscopy was performed but failed to identify the fistula. Viral infection was ruled out and there was no bacterial growth on the cultures plates. The Mantoux test was performed but was not conclusive, so the interferon gamma release assay (IGRA) was used with a positive value consistent with a tuberculosis infection that was then confirmed by the polymerase chain reaction (PCR) test which detected Mycobacterium tuberculosis DNA. The patient was then treated with tuberculostatic antibiotics and performed a UGE to close the fistula with the placement of an endoscopic clip (Fig. 3). The patient improved and was then discharged.
Five months later, the patient returned to our hospital with reappearance of symptoms. She performed another gastrografin swallow esophagram that was consistent with a fistula recurrence (Fig. 4). She was then submitted to surgery with excision of the fistulous path and closure of the esophageal end bronchial openings.
Tuberculosis infection is an extremely rare cause of acquired BEF and the diagnosis requires a high index of suspicion in patients with recurrent respiratory infections of poorly defined etiology.2 The treatment involves a multidisciplinary approach, at an early stage with interruption of oral feeding, antibiotic therapy, and parenteral nutritional support, later supplemented by a more interventional approach such as endoscopic treatment or surgery in refractory cases. There were no post-operative intercurrences and the patient is currently without any symptoms.
References
William A. Ross, and Jeffrey H. Lee. Endoscopic Approach to Tracheoesophageal Fistulas in Adults. Techniques in Gastrointestinal Endoscopy. 2008; 10:155–163
Salvatore Griffo, Paolo Stassano, Gavriele Lannelli, Luigi Di Tommaso, Marcellino Cicalese, Mario Monaco, and Giovanni Ferrante. Benign bronchoesophageal fistula: Report of four cases. The journal of Thoracic and Cardiovascular Surgery 2007; 133: 1378–9
Author information
Authors and Affiliations
Contributions
Aires Martins: Design of manuscript, research, manuscript revision, and approval.
Álvaro Gonçalves: Analysis, revision, and approval.
Teresa Almeida: Analysis, revision, and approval.
Francisco Fazeres: Analysis, revision, and approval.
Alberto Midões: Director of General Surgery department, revision and approval.
Corresponding author
Rights and permissions
About this article
Cite this article
Martins, A., Gonçalves, Á., Almeida, T. et al. Bronchoesophageal Fistula in the Setting of Tuberculosis Infection. J Gastrointest Surg 21, 2119–2121 (2017). https://doi.org/10.1007/s11605-017-3484-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3484-0