Abstract
Background
The relationship between RAS mutation status and outcome for patients undergoing repeat hepatectomy (RH) for recurrent colorectal liver metastases (CLM) has not been defined.
Objective
The objective of this study was to evaluate the relationship between RAS mutation status and outcome in patients undergoing RH for CLM.
Methods
All patients who underwent RH for CLM with known RAS mutation status between January 2005 and November 2014 were identified, and the outcomes of patients with and without RAS mutations were compared.
Results
Ninety-eight patients underwent RH, of whom 34 (35 %) harbored a RAS mutation. Wild-type (WT) and mutant RAS groups had similar clinicopathologic characteristics. Median recurrence-free survival (RFS) for patients with WT and mutant RAS was 12.2 and 6.1 months, respectively (p = 0.03). Median overall survival (OS) for the WT and mutant RAS patients were 42.5 and 26.6 months, respectively (p < 0.01). On multivariate analysis, RAS mutations [hazard ratio (HR) = 1.69, p = 0.04] were associated with worse RFS, while multiple tumors (HR = 1.92, p = 0.045) and RAS mutations (HR = 2.11, p = 0.02) predicted worse OS.
Conclusion
Patients with recurrent CLM that harbor RAS mutations have worse RFS and OS than patients with WT RAS, and RAS mutations are independently associated with worse RFS and OS. RAS mutation status should be determined prior to RH, as it may impact treatment decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The RAS family of proteins is involved in cell signaling and regulation of cell division and proliferation.1 , 2 KRAS mutations occur frequently in colorectal cancer and other types of cancer and have long been implicated in carcinogenesis.1 , 2 More recently, there has been a resurgence of interest in RAS mutations with the advent of targeted therapies.3 Van Cutsem et al. published a randomized trial in patients with metastatic epidermal growth factor receptor (EGFR)-positive colorectal cancer in which patients received FOLFIRI alone or in combination with cetuximab.3 The addition of cetuximab reduced the risk of disease progression, but this risk reduction was limited to patients with wild-type (WT) KRAS tumors. Over the next several years, it became apparent that RAS mutations were a marker of tumor biology and had potential prognostic value.4 – 8 Several series have evaluated patients with colorectal liver metastases (CLM) and have found that RAS mutations are associated with worse survival,4 , 9 higher rates of lung recurrence,4 , 10 poor radiologic and pathologic responses to chemotherapy,5 and higher rates of margin positive resections.6 A recent meta-analysis found that KRAS mutations were negatively associated with recurrence-free survival (RFS) and overall survival (OS).11 The preponderance of evidence suggests that RAS mutation status in CLM has prognostic significance and may help guide therapy.
Hepatectomy is well accepted as the best treatment for CLM and effectively prolongs survival.12 , 13 Despite good long-term survival,12 , 13 most patients develop recurrence after hepatectomy for CLM.14 , 15 Several studies have demonstrated the safety and efficacy of repeat hepatectomy (RH) in selected patients.15 – 18 Despite 5-year survival rates up to 73 % following RH,16 recurrence rates remain high with median RFS of 7 months.16 Andreou et al. reported that a positive surgical margin at RH was associated with worse RFS.16 In summary, although long-term survival can be achieved following RH, recurrence following RH develops early and often. Hepatobiliary surgeons and their multidisciplinary partners are in need of molecular and other biomarkers that will aid in treatment decision making for patients with recurrent metastatic disease.
To date, the relationship between RAS mutation status and RH for CLM has not been defined. The present study sought to evaluate the relationship of RAS mutation status in patients undergoing RH for recurrent CLM and hypothesized that RAS mutation status may help predict which patients would derive the most benefit from RH.
Materials and Methods
Study Population
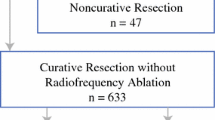
The Institutional Review Board of the University of Texas MD Anderson Cancer Center approved this study of patients undergoing repeat hepatectomy for CLM. The institutional liver surgery database was used to identify all patients who underwent hepatectomy for CLM with known RAS mutation status between January 2005 and November 2014. Next, we identified patients who underwent repeat hepatectomy following recurrence of CLM. Two-stage hepatectomies were considered as one procedure.
Disease Treatment
Computed tomography (CT) of the chest, abdomen, and pelvis with a triphasic liver protocol was used in all patients to assess resectability and extrahepatic disease. After diagnosis of recurrent disease, preoperative oxaliplatin or irinotecan-based chemotherapy was administered to the majority of patients. Parenchymal transection was performed using a two-surgeon technique with the cavitron ultrasonic surgical aspirator (Valleylab, Boulder, CO, USA) and saline-linked cautery (Dissecting Sealer DS 3.0; TissueLink Medical, Inc., Dover, NH, USA) under hepatic inflow and/or outflow occlusion.19 Following repeat hepatectomy, patients received postoperative chemotherapy and returned every 3–4 months for follow-up, which included surveillance CT scans to assess for recurrence. When recurrence was identified, therapy was at the discretion of the treatment team.
Histological Evaluation and RAS Mutation Analysis
All surgical specimens underwent histologic evaluation by the pathology department, and the presence of CLM was confirmed, the surgical margins were assessed, and the percentage of viable tumor cells was recorded. A positive margin was defined as viable tumor cells <1 mm from the margin.20 A major pathologic response to preoperative chemotherapy was defined as ≤49 % viable tumor cells.21 DNA from the primary tumor or CLM was used to determine RAS mutation status as previously described.4 , 6 We screened for mutations in KRAS codons 12 and 13 in all patients and for mutations in KRAS codons 61 and 146 and NRAS codons 12, 13, and 61 in the majority of patients treated since 2012.6 , 22 The lower limit of detection of the assay was approximately one mutant allele in the background of nine wild-type alleles.6 Mutations in KRAS and NRAS codons were collectively reported as RAS mutations.
Statistics
Clinicopathologic variables for patients undergoing first repeat hepatectomy for CLM with WT and mutant RAS tumors were compared. Quantitative and qualitative variables were expressed as frequency and median (range). Comparisons between groups were analyzed with chi-square or Fischer’s exact test for categorical data and the Mann-Whitney test for continuous data. RFS and OS were calculated using the Kaplan-Meier method from the date of repeat hepatectomy until the date or recurrence and last follow-up, respectively, and compared using the log-rank test. Univariate analysis was performed to evaluate potential variables associated with RFS and OS. Potential variables included gender, age, primary tumor location (colon vs. rectum), primary tumor lymph node status, number of CLM, size of largest CLM, carcinoembryonic antigen (CEA) level, preoperative chemotherapy (cycles, lines, and agents), types of hepatectomy [major (≥3 Couinaud’s segments) vs. minor], estimated blood loss (EBL), radiofrequency ablation (RFA), margin status of repeat hepatectomy (R0 vs. R1), and RAS mutational status (mutant vs. wild-type). All variables associated with RFS or OS on univariate analysis with p value <0.10 were included in a multivariate cox proportional hazard model. p Value <0.05 was considered statistically significant. All statistical analysis was performed using SPSS version 17.2 (SPSS Inc., Chicago, IL, USA).
Results
Patient Characteristics
During the study period, 922 patients with known RAS mutation status underwent curative-intent hepatectomy. Ninety-eight of these were first repeat hepatectomies—64 patients had wild-type RAS tumors and 34 (35 %) had tumors with a mutant RAS. For the majority of patients, RAS mutational analysis was performed on a metastatic tumor (Table 1). Of note, 14 patients had RAS mutational analysis performed on a primary tumor and a metastatic site. The mutational status from the primary and metastatic site was concordant in all 14 of these cases. KRAS mutations (n = 32) predominated and two patients were found to have NRAS mutations. KRAS mutations were identified in exon 12 (n = 22), exon 13 (n = 8), and exon 61 (n = 2).
Clinicopathologic variables were similar between WT and mutant RAS groups (Table 2). Two thirds of patients had a solitary CLM prior to repeat hepatectomy. One third of patients received >6 cycles of chemotherapy prior to repeat hepatectomy. A major hepatectomy was performed in 22 % of patients, and 11 % of patients had an RFA. On pathologic evaluation, 12 patients were found to have a positive margin. There were no major differences between the WT and mutant RAS groups with regards to demographics, tumor characteristics, treatments, or pathologic features.
Recurrence
At a median follow-up of 35 months, 75 (77 %) patients had developed a recurrence. The two most common sites of disease recurrence were the liver and lungs. Liver recurrence was seen in 62 and 50 % of WT and mutant RAS patients, respectively, while lung recurrence was seen in 21 and 39 %, respectively (Fig. 1a). Recurrent disease was treated with local therapy in 31 (41 %) patients—47 % of WT and 32 % of mutant RAS patients (Fig. 1b). The differences in recurrence patterns and treatment of recurrent disease were not significantly different between the two groups.
a Recurrence patterns following repeat hepatectomy for recurrent CLM. Percentage of wild-type and mutant RAS recurrences in the liver (62 vs. 50 %, p = 0.32), lung (21 vs. 39 %, p = 0.09), lymph nodes (17 vs. 14 %, p = 0.76), and peritoneum (9 vs. 11 %, p = 0.75). b Treatment of recurrent disease following repeat hepatectomy for recurrent CLM. Percentage of wild-type and mutant RAS patients who received an additional resection (30 vs. 21 %, p = 0.43), ablation (17 vs. 11 %, p = 0.46), or chemotherapy (53 vs. 68 %, p = 0.21)
Survival
The median RFS and OS for the entire cohort were 7.8 and 34.6 months, respectively. Patients with mutant RAS had a median RFS of 6.1 months, compared to 12.2 months for those with WT RAS (p = 0.03) (Fig. 2a). The median overall survival was 26.6 versus 42.5 months for mutant and wild-type RAS, respectively (p = 0.005) (Fig. 2b).
a Recurrence-free survival following repeat hepatectomy for recurrent CLM. Median recurrence-free survival for wild-type and mutant RAS patients was 12.2 and 6.1 months, respectively. b Overall survival following repeat hepatectomy for recurrent CLM. Median overall survival for wild-type and mutant RAS patients was 42.5 and 26.6 months, respectively
Univariate and Multivariate Analyses
Patient, tumor, treatment, and pathologic variables were incorporated into a multivariate analysis to determine which factors impacted RFS and OS. On univariate analysis, multiple tumors, tumor size >3 cm, EBL >750 ml, and RAS mutation status were associated with RFS, but only RAS mutation status [HR = 1.69 (1.03–2.72), p = 0.04] was associated with RFS on multivariate analysis (Table 3). Gender, multiple tumors, major hepatectomy, and RAS mutation status were associated with OS on univariate analysis, but only multiple tumors [HR = 1.92 (1.02–3.54), p = 0.045] and RAS mutation status [HR = 2.11 (1.11–3.98), p = 0.02] were associated with OS (Table 4).
Discussion
The present study is the first to investigate the relationship of RAS mutation status and outcomes following repeat hepatectomy for recurrent CLM. Thirty-four (35 %) of 98 patients undergoing RH were found to have mutant RAS tumors—32 KRAS mutations and 2 NRAS mutations. Brudvik et al. reported a RAS mutation rate of 36 % in patients undergoing hepatectomy for CLM.6 Another recent study reported a KRAS mutation rate of 39.5 % in CLM.23 In CLM, the most commonly identified RAS mutation is KRAS, which compromises about 80 % of identified mutations with the remaining being mutations in NRAS.4 , 5 In this cohort, KRAS mutations were most frequently identified exons 12 and 13 (69 and 25 %, respectively). The incidence and specific type of RAS mutations found in the present RH study is similar to the larger population of patients who undergo hepatectomy for CLM.
It is well established that recurrence after hepatectomy for CLM remains high; up to 73 % of patients will develop recurrence.14 , 15 In the current study, at a median follow-up of 35 months following RH, 75 (77 %) patients had developed recurrence. Andreou et al. reported a recurrence rate of 70 % after a median follow-up of 33 months after RH for CLM.16 In the current study, recurrence in the liver and lung were the most common at 57 and 28 %, respectively. Of note, lung recurrence was seen in 21 % of patients with WT tumors compared to 39 % in those with mutant RAS tumors (p = 0.09). Previous studies demonstrate that the lung recurrence following hepatectomy for CLM is more commonly seen in patient with RAS mutations.4 , 10 Although the current study did not find a statistically significant difference, this is likely due to sample size, and this may represent a clinically significant difference in concordance with other studies.
In the current study, about 40 % of the patients who developed recurrence following RH were able to undergo local therapy (resection 27 % and ablation 15 %). It would stand to reason that patients with mutant RAS tumors would be less likely to undergo local therapy, if they have the same rate of liver recurrence and a higher rate of lung recurrence following RH, but this was not seen in the current study; local therapy was utilized in 47 and 32 % of WT and mutant RAS patients, respectively. Recurrence following RH for CLM is common; however, patients with RAS mutant tumors may have a higher risk of lung recurrence, and when they do recur, they appear less likely to be candidates for aggressive therapy.
Recurrence-free survival following RH for CLM remains poor. Andreou et al. previously reported a median progression-free survival of 7 months in patients undergoing repeat hepatectomy for CLM, after excluding patients treated with ablation.16 Herein, we report a median RFS of 7.8 for the entire cohort of patients following RH for CLM. Fortunately, as discussed above, many of these early recurrences have treatment options. Andreou et al. reported a positive surgical margin at RH as predictor of worse PFS.16 In the current study, a positive surgical margin occurred in 12 % of the patients undergoing RH, but was not associated with RFS. RAS mutation status (HR = 1.69, p = 0.037) was the only predictor of RFS, and the median RFS for WT and mutant RAS patients were 12.2 and 6.1 months, respectively (p = 0.028). These data indicate that RAS mutations are a predictor of poor RFS.
Despite high recurrence rates, overall survivals following RH for CLM have remained comparable to first resection patients.16 , 18 This undoubtedly reflects appropriate selection of patients with favorable tumor biology for RH.24 Luo et al. conducted a systematic review and meta-analysis to determine predictors of survival following RH for CLM.24 They found six predictors of survival following RH: disease-free interval >1 year, solitary CLM, unilobar CLM, size ≤5 cm, lack of extrahepatic disease, and R0 resection.24 These reported predictors of survival are similar to the numerous scoring systems and predictive models that have been previously published for first hepatectomies.25 – 27 A comparable set of factors was evaluated in the current study following RH, but only multiple tumors (HR = 1.92, p = 0.045) and mutant RAS (HR = 2.11, p = 0.005) were found to be associated with worse OS. Furthermore, the OS for patients with wild-type and mutant RAS was 42.5 and 26.6 months, respectively (p = 0.005). These data strongly suggest that RAS mutation status needs to be incorporated into historical prognostic models as it is a powerful predictor of OS.
The retrospective design of this study is a potential limitation. Only patients with known RAS mutation status were included in the study, and the decision of whether or not to perform a RAS mutational analysis was up to the discretion of the treatment team. This having been said, the denominator cohort of patients with genetic evaluation was large, and the outcomes are well tracked with a long median follow-up interval. Another area of challenge in the study of RAS mutations is the tissue source, be it primary tumor, previous metastatic tissue, or the current metastatic tissue under treatment. Importantly, on the 14 patients with both primary and metastasis tissue assessed, there was RAS mutation concordance in 100 %. Lastly, RAS mutation testing has rapidly evolved and will continue to progress. Over the first many years of this study, only KRAS exons 12 and 13 were analyzed, so it is possible that some patients were classified as WT RAS and actually possessed a mutation in an exon that was undetectable at that time. However, correction of any potential misclassifications of this type would be likely to identify even larger difference in outcomes between WT and mutant RAS patients.
Conclusion
In general, patients with CLM that harbor RAS mutations have worse RFS and OS than patients with WT RAS. This study demonstrates that in the specific population of patients with recurrent liver CLM, RAS mutational status has prognostic value, with RAS mutations independently associated with worse RFS and OS. Thus, RAS mutation status should be determined prior to RH, as it may impact treatment decisions.
References
Forrester K, Almoguera C, Han K, Grizzle WE, Perucho M: Detection of high incidence of K-ras oncogenes during human colon tumorigenesis. Nature 1987, 327(6120):298-303.
Khosravi-Far R, Campbell S, Rossman KL, Der CJ: Increasing complexity of Ras signal transduction: involvement of Rho family proteins. Advances in cancer research 1998, 72:57-107.
Van Cutsem E, Kohne CH, Hitre E, Zaluski J, Chang Chien CR, Makhson A, D’Haens G, Pinter T, Lim R, Bodoky G et al: Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. The New England journal of medicine 2009, 360(14):1408-1417.
Vauthey JN, Zimmitti G, Kopetz SE, Shindoh J, Chen SS, Andreou A, Curley SA, Aloia TA, Maru DM: RAS mutation status predicts survival and patterns of recurrence in patients undergoing hepatectomy for colorectal liver metastases. Annals of surgery 2013, 258(4):619-626; discussion 626-617.
Mise Y, Zimmitti G, Shindoh J, Kopetz S, Loyer EM, Andreou A, Cooper AB, Kaur H, Aloia TA, Maru DM et al: RAS mutations predict radiologic and pathologic response in patients treated with chemotherapy before resection of colorectal liver metastases. Annals of surgical oncology 2015, 22(3):834-842.
Brudvik KW, Mise Y, Chung MH, Chun YS, Kopetz SE, Passot G, Conrad C, Maru DM, Aloia TA, Vauthey JN: RAS Mutation Predicts Positive Resection Margins and Narrower Resection Margins in Patients Undergoing Resection of Colorectal Liver Metastases. Annals of surgical oncology 2016.
Karagkounis G, Torbenson MS, Daniel HD, Azad NS, Diaz LA, Jr., Donehower RC, Hirose K, Ahuja N, Pawlik TM, Choti MA: Incidence and prognostic impact of KRAS and BRAF mutation in patients undergoing liver surgery for colorectal metastases. Cancer 2013, 119(23):4137-4144.
Nash GM, Gimbel M, Shia J, Nathanson DR, Ndubuisi MI, Zeng ZS, Kemeny N, Paty PB: KRAS mutation correlates with accelerated metastatic progression in patients with colorectal liver metastases. Annals of surgical oncology 2010, 17(2):572-578.
Schirripa M, Bergamo F, Cremolini C, Casagrande M, Lonardi S, Aprile G, Yang D, Marmorino F, Pasquini G, Sensi E et al: BRAF and RAS mutations as prognostic factors in metastatic colorectal cancer patients undergoing liver resection. British journal of cancer 2015, 112(12):1921-1928.
Pereira AA, Rego JF, Morris V, Overman MJ, Eng C, Garrett CR, Boutin AT, Ferrarotto R, Lee M, Jiang ZQ et al: Association between KRAS mutation and lung metastasis in advanced colorectal cancer. British journal of cancer 2015, 112(3):424-428.
Brudvik KW, Kopetz SE, Li L, Conrad C, Aloia TA, Vauthey JN: Meta-analysis of KRAS mutations and survival after resection of colorectal liver metastases. The British journal of surgery 2015, 102(10):1175-1183.
Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR, Hess K, Curley SA: Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Annals of surgery 2004, 239(6):818-825; discussion 825-817.
Fernandez FG, Drebin JA, Linehan DC, Dehdashti F, Siegel BA, Strasberg SM: Five-year survival after resection of hepatic metastases from colorectal cancer in patients screened by positron emission tomography with F-18 fluorodeoxyglucose (FDG-PET). Annals of surgery 2004, 240(3):438-447; discussion 447-450.
de Jong MC, Pulitano C, Ribero D, Strub J, Mentha G, Schulick RD, Choti MA, Aldrighetti L, Capussotti L, Pawlik TM: Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Annals of surgery 2009, 250(3):440-448.
Saiura A, Yamamoto J, Koga R, Takahashi Y, Takahashi M, Inoue Y, Ono Y, Kokudo N: Favorable outcome after repeat resection for colorectal liver metastases. Annals of surgical oncology 2014, 21(13):4293-4299.
Andreou A, Brouquet A, Abdalla EK, Aloia TA, Curley SA, Vauthey JN: Repeat hepatectomy for recurrent colorectal liver metastases is associated with a high survival rate. HPB : the official journal of the International Hepato Pancreato Biliary Association 2011, 13(11):774-782.
Petrowsky H, Gonen M, Jarnagin W, Lorenz M, DeMatteo R, Heinrich S, Encke A, Blumgart L, Fong Y: Second liver resections are safe and effective treatment for recurrent hepatic metastases from colorectal cancer: a bi-institutional analysis Annals of surgery 2002, 235(6):863-871.
Battula N, Tsapralis D, Mayer D, Isaac J, Muiesan P, Sutcliffe RP, Bramhall S, Mirza D, Marudanayagam R: Repeat liver resection for recurrent colorectal metastases: a single-centre, 13-year experience. HPB : the official journal of the International Hepato Pancreato Biliary Association 2014, 16(2):157-163.
Aloia TA, Zorzi D, Abdalla EK, Vauthey JN: Two-surgeon technique for hepatic parenchymal transection of the noncirrhotic liver using saline-linked cautery and ultrasonic dissection. Annals of surgery 2005, 242(2):172-177.
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, Curley SA, Loyer EM, Muratore A, Mentha G et al: Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Annals of surgery 2005, 241(5):715-722, discussion 722-714.
Blazer DG, 3rd, Kishi Y, Maru DM, Kopetz S, Chun YS, Overman MJ, Fogelman D, Eng C, Chang DZ, Wang H et al: Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. Journal of clinical oncology : official journal of the American Society of Clinical Oncology 2008, 26(33):5344-5351.
Passot G, Chun YS, Kopetz SE, Zorzi D, Brudvik KW, Kim BJ, Conrad C, Aloia TA, Vauthey JN: Predictors of Safety and Efficacy of 2-Stage Hepatectomy for Bilateral Colorectal Liver Metastases. Journal of the American College of Surgeons 2016.
Kawamata H, Yamashita K, Kojo K, Ushiku H, Ooki A, Watanabe M: Discrepancies between the K-ras mutational status of primary colorectal cancers and corresponding liver metastases are found in codon 13. Genomics 2015, 106(2):71-75.
Luo LX, Yu ZY, Huang JW, Wu H: Selecting patients for a second hepatectomy for colorectal metastases: an systemic review and meta-analysis. European journal of surgical oncology : the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 2014, 40(9):1036-1048.
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH: Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Annals of surgery 1999, 230(3):309-318; discussion 318-321.
Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, Jaeck D: Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer 1996, 77(7):1254-1262.
Hill CR, Chagpar RB, Callender GG, Brown RE, Gilbert JE, Martin RC, 2nd, McMasters KM, Scoggins CR: recurrence following hepatectomy for metastatic colorectal cancer: development of a model that predicts patterns of recurrence and survival. Annals of surgical oncology 2012, 19(1):139-144.
Acknowledgments
The University of Texas MD Anderson Cancer Center is supported by the National Institutes of Health through Cancer Center Support Grant P30CA016672.
Author information
Authors and Affiliations
Corresponding author
Additional information
All authors/coauthors contributed significantly to the manuscript and fulfilled the requirements for authorship as per the guidelines of the International Committee of Medical Journal Editors (ICMJE).
This manuscript was presented in the Presidential Plenary session at the 2016 Annual Meeting of the Society for Surgery of the Alimentary Tract (SSAT) on 5/22/2106 in San Diego, CA.
Rights and permissions
About this article
Cite this article
Denbo, J.W., Yamashita, S., Passot, G. et al. RAS Mutation Is Associated with Decreased Survival in Patients Undergoing Repeat Hepatectomy for Colorectal Liver Metastases. J Gastrointest Surg 21, 68–77 (2017). https://doi.org/10.1007/s11605-016-3189-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3189-9