Abstract
Ectopic pancreas is an uncommon and benign finding. However, these lesions can cause symptoms including abdominal pain and often require removal. We present the case of a 27-year-old patient with long-standing vague abdominal symptoms eventually found to have ectopic pancreas tissue in the proximal jejunum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A 27-year-old female presented with epigastric abdominal pain and worsening diarrhea. Her medical history included gastroesophageal reflux disease, endometriosis, and chronic diarrhea with a surgical history of diagnostic laparoscopy 8 years prior with ablation of endometrial implants. Physical examination was notable for tenderness in the epigastric area with slight voluntary guarding. No abdominal wall hernias were noted and laboratory tests were within normal values.
The patient was evaluated by colonoscopy which showed nonspecific crypt inflammation by pathology. The patient was diagnosed with likely Clostridium difficile infection and treated with vancomycin. Despite treatment, she remained symptomatic. Upper endoscopy with biopsies revealed no abnormalities. She underwent a computed tomography (CT) enterography with finding of a 1.6 cm enhancing, smoothly marginated mass in the small bowel wall at the juncture of the duodenum and jejunum (Fig. 1).
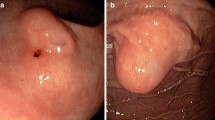
The patient was taken to surgery for an exploratory laparoscopy. A lobular mass in the proximal jejunum 5 cm from the ligament of Treitz was identified, measuring 1.8 × 1.5 × 1.2 cm and corresponding to the preoperative CT (Fig. 2). A laparoscopic wedge resection of the tumor with primary closure of the jejunal defect was performed. Subsequent pathology demonstrated heterotopic pancreas, within the bowel wall, with focal overlying mucosal erosion, negative for dysplasia or malignancy.
Discussion
Heterotopic or ectopic pancreas is defined as pancreatic tissues lacking vascular or anatomic communication with the normal body of the pancreas, yet possessing histological features of pancreatic acinar formation, duct development, and islets of Langerhans.1 The prevalence of ectopic pancreatic tissue is reported to be around 0.25 % in the general population, and 14 % in autopsy material,2 being more common at 30–50 years of age with male predominance.3
Approximately 90 % of ectopic pancreatic tissue is found in the upper gastrointestinal tract, the most common site is the stomach with 27.5 % of cases. Ectopic pancreas has also been reported in the esophagus, ileum, colon, mesentery, and omentum.2
Most patients are asymptomatic; however, when symptoms are present, pain is the most common. Other symptoms may depend upon the location of the pancreatic tissue and size greater than 1.5 cm. Complications seen in normal pancreatic tissue, such as chronic pancreatitis, can also be present in ectopic pancreas. Malignant transformation may rarely occur.3
The diagnosis can be challenging and can include barium swallow study with sensitivity and specificity of 87.5 and 71.4 %, respectively; endoscopic ultrasonography with fine needle aspiration has a reported sensitivity ranging 80–100 %.3 CT is the most commonly used noninvasive modality for the preoperative evaluation of gastric tumors. There are morphologic CT findings that can lead us to the diagnosis of ectopic pancreatic tissue, such as the location (antrum, pylorus, duodenum), prominent enhancement of overlying mucosa, ill-defined border, endoluminal growth pattern, and long diameter/short diameter ratio >1.4, with a sensitivity and specificity of 100 and 82.5 % when at least two of the five criteria were used in combination.
The treatment consists of surgical excision. It provides symptomatic relief and is recommended, especially if diagnostic uncertainty remains.
References
Sathyanarayana SA, Deutsch GB, Bajaj J, Friedman B, Bansal R, Molmenti E, Nicastro JM, Coppa GF. Ectopic pancreas: a diagnostic dilemma. Int J Angiol 2012;21:177-180.
Straatman J, Meester RJ, Grieken NC, Jacobs MJ, Graaf PD, Kazemier G, Cuesta MA. Clinical picture: multiple sites of ectopic pancreatic tissue. Springerplus 2015;4:293.
Christodoulidis G, Zacharoulis D, Barbanis S, Katsogridakis E, Hatzitheofilou K. Heterotopic pancreas in the stomach: a case report and literature review. World J Gastroenterol 2007;13:6098-6100.
Disclosure Information
Dr. Serrano reported no biomedical financial interests or potential conflicts of interest. Dr. Stauffer reported no biomedical financial interests or potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Serrano, J.S., Stauffer, J.A. Ectopic Pancreas in the Wall of the Small Intestine. J Gastrointest Surg 20, 1407–1408 (2016). https://doi.org/10.1007/s11605-016-3104-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3104-4