Abstract
A 69-year-old male with a history of hepatitis B-induced cirrhosis underwent segmental liver resection for hepatocellular carcinoma. At his 12-month follow-up, local recurrence in segment VII was diagnosed, measuring 7.8 by 6.2 cm, with irregular margins and the presence of a tumor thrombus in the portal vein. After evaluation by the multidisciplinary liver team, the patient underwent transcatheter arterial chemoembolization with drug-eluting beads. Forty-eight hours after his discharge, the patient presented with gangrenous cholecystitis and he underwent an uneventful cholecystectomy. Cholecystitis is a well-documented complication of transcatheter arterial chemoembolization due to inadvertent reflux of the embolic material into the cystic artery. However, super selective embolization significantly reduces the risk of cholecystitis. In most cases, management is conservative and only severe cases require further intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Case Presentation
A 69-year old male with a history of hepatitis B-induced cirrhosis was referred to the surgical ward in July, 2013 with a newly diagnosed liver tumor on ultrasound screening. His serum alpha-fetoprotein (AFP) levels were within normal range (4.3 ng/ml). The multiphase-multidetector CT showed a typical hypervascularized hepatocellular carcinoma (HCC) lesion in segment VI. Upon completion of the preoperative evaluation, the patient underwent an uneventful elective segmental liver resection.
At his 12-month follow-up, contrast-enhanced CT showed a large HCC lesion in segment VII, measuring 7.8 by 6.2 cm, with irregular margins and the presence of a tumor thrombus in the portal vein. The imaging findings were evaluated by the multidisciplinary liver team, and the patient was admitted for transcatheter arterial chemoembolization (TACE) with drug-eluting beads (DEB).
Under local analgesia, DC Bead microspheres (Biocompatibles UK, Farnham, Surrey, UK) loaded with doxorubicin were super selectively injected into the feeding vessels of the tumor through the right hepatic artery. His postinterventional recovery was uneventful, and the patient was discharged from the hospital 48 h after TACE.
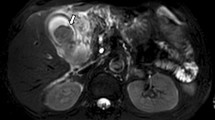
Forty-eight hours after his discharge, the patient presented with high fever, tachycardia, tachypnea, abdominal pain, and vomiting. On examination, he had right subcostal pain with guarding. He had marginal leukocytosis of 13 × 109/L with 86 % polymorphs and elevated C-reactive protein. Liver function, blood, and urine amylase were normal. Imaging work-up with abdominal ultrasound and contrast-enhanced CT showed an over-distended gallbladder, with thick, irregular wall, intraluminal membranes and stranding in the fat surrounding the fundus (Fig. 1a, b). Pericholecystic fluid and gas in the gallbladder wall were also present. The patient underwent cholecystectomy and was discharged from the hospital 48 h later. Pathology examination confirmed the diagnosis of acute acalculous gangrenous cholecystitis with extensive ischemic changes and focal transmural necrosis and identified the TACE microspheres in the gallbladder wall vessels (Fig. 2a, b). At last follow-up in June 2015, he remains well and is treated with sorafenib.
a Gallbladder resection specimen showing the TACE microspheres in the gallbladder wall vasculature and transmural necrosis of the gall bladder wall, hematoxylin and eosin staining (arrows). b Magnified view of the TACE microspheres in the gallbladder wall vessels and coagulative type necrosis of the gallbladder wall, hematoxylin and eosin staining
Discussion
TACE is widely used in the treatment of HCC, offering significant survival benefits.1 It is indicated for the treatment of patients with unresectable HCC or for patients awaiting liver transplantation.2 Common complications related to TACE are hepatic failure, liver abscess and intrahepatic bilomas, iatrogenic abdominal aortic dissection related to the manipulation of the catheter or the guide wire, cholecystitis, and pancreatitis.3
Cholecystitis is a well documented complication of TACE due to inadvertent reflux of the embolic material into the cystic artery.4 However, super selective embolization significantly reduces the risk of cholecystitis. In most cases, management can be conservative, and no surgical or radiological intervention is necessary.4 In cases of severe cholecystitis, the placement of a cholecystostomy tube is mandatory and cholecystectomy may also be required.
References
Llovet J M, Real M I, Montaña X, et al. Barcelona Liver Cancer Group arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet 2002;359:1734-1739.
Sangro B, Salem R, Kennedy A, Coldwell D, Wasan H. Radioembolization for hepatocellular carcinoma: a review of the evidence and treatment recommendations. Am J Clin Oncol 2011;34:422-31.
Poggi G, Pozzi E, Riccardi A, Tonini S, Montagna B, Quaretti P, Tagliaferri B, Sottotetti F, Baiardi P, Pagella C, Minoia C, Bernardo G. Complications of image-guided transcatheter hepatic chemoembolization of primary and secondary tumours of the liver. Anticancer Res 2010;;;30:5159-64.
Wagnetz U, Jaskolka J, Yang P, Jhaveri KS. Acute ischemic cholecystitis after transarterial chemoembolization of hepatocellular carcinoma: incidence and clinical outcome. J Comput Assist Tomogr 2010;34:348-53.
Authors’ Contributions
All authors contributed equally to obtaining of the images and writing of the report, and all authors approved the final version.
Conflict of Interest
The authors declare that they have no competing interests.
Funding Source
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karavias, D., Kourea, H., Sotiriadi, A. et al. Gangrenous Cholecystitis Related to Transcatheter Arterial Chemoembolization (TACE) Treatment for Hepatocellular Carcinoma. J Gastrointest Surg 19, 2093–2095 (2015). https://doi.org/10.1007/s11605-015-2896-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2896-y





