Abstract
Introduction
As the SOFIA (Soft torqueable catheter Optimized For Intracranial Access) 6F catheter has a large luminal diameter, it can be used as an aspiration catheter. Furthermore, it may function as an intermediate catheter when a stent retriever is required.
Purpose
We aimed to evaluate the usefulness of the SOFIA 6F catheter in mechanical thrombectomy with the direct aspiration first pass technique.
Method
Patients who had undergone mechanical thrombectomy (September 2017–January 2019) using the SOFIA 6F catheter in two centers were retrospectively analyzed. We used the thrombolysis in cerebral infarction (TICI) scale to evaluate the success of recanalization. National Institutes of Health Stroke Scale scores on admission and discharge were used together with the modified Rankin Scale (mRS) scores at 90 days.
Results
In 132 (89.1%) of the 148 cases, the thrombus was in the anterior system. The SOFIA 6F catheter reached the thrombus site in 130 (87.8%) cases. The rate of successful recanalization (TICI ≥ 2b) was 89.1%. The targeted clinical outcome (mRS score ≤ 2 at 90th days) was achieved in 49.3% of cases. Symptomatic intracranial hemorrhage occurred in 5.4%. The rate of emboli to new vascular territories was 5.4%. Mortality was 14.1%.
Conclusion
In the majority of our cases, the SOFIA 6F catheter provided effective and rapid recanalization with aspiration thrombectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is the second leading cause of death and the third leading cause of disability in the world [1]. Endovascular strategies and intravenous thrombolytic therapy are the two main treatment options in acute ischemic stroke. However, in acute ischemic strokes resulting from proximal large vessel occlusions, mechanical thrombectomy offers significantly higher successful recanalization rates compared to intravenous thrombolytics [2].
With the recent advances in technology and the development of different revascularization devices, new methods have emerged in mechanical thrombectomy, such as a direct aspiration first pass technique (ADAPT). The production of large-bore catheters with improved trackability has allowed the ADAPT to gain widespread recognition among neurointerventionalists. In ADAPT, first, aspiration thrombectomy with new-generation catheters is attempted. If recanalization could not be achieved, then the same catheter functions as an intermediate catheter and provides support for stent retrievers.
SOFIA (Soft torqueable catheter Optimized For Intracranial Access, Microvention Terumo, CA, USA) is one of the most commonly employed catheters in modern aspiration thrombectomy [3,4,5,6,7,8,9,10]. The SOFIA catheter provides atraumatic access to the thrombus site by its soft structure. Furthermore, SOFIA’s soft design allows the operator to reach the clot level even in the presence of increased vascular tortuosity.
Since larger luminal diameter offers a higher aspiration force [11], today, many neurointerventionalists utilize the SOFIA Flow Plus 6F (SOFIA Flow Plus in Japan and North America, and SOFIA Plus in Europe) in their aspiration thrombectomy practice. Currently, the feasibility of SOFIA Flow Plus in aspiration thrombectomy has been very well established in the literature [6,7,8,9]. However, there are countries where SOFIA Flow Plus is not commercially available or not reimbursed by the insurances. Due to similar problems, in our country, endovascular surgeons utilize the non-flow plus version of the SOFIA 6F catheter.
Both SOFIA Flow Plus 6F and SOFIA 6F have the SOFIA’s unique soft structure, and therefore, have a high trackability. Furthermore, both catheters have a luminal diameter of 0.070 inches and a distal length of 19 cm. The main differences between SOFIA Flow Plus 6F and SOFIA 6F are in total length and price. While SOFIA 6F has a total length of 115 cm, SOFIA Flow Plus 6F has two versions with the total lengths of 125 and 131 cm. Nevertheless, SOFIA 6F has a significantly lower market price.
Although the effectiveness and safety of the SOFIA Flow Plus 6F have been investigated previously [6,7,8,9], the utility of SOFIA 6F as a primary aspiration catheter remains unclear due to scant evidence. In this study, we aimed to evaluate the performance of SOFIA 6F in direct aspiration thrombectomy. To our knowledge, this is the first study focusing on SOFIA 6F’s performance with ADAPT.
Materials and methods
Patients
Patients who had undergone direct aspiration thrombectomy due to acute ischemic stroke (September 2017–January 2019) in two stroke centers were retrospectively screened, and the data of 148 cases using the SOFIA 6F catheter were evaluated. The SOFIA 6F catheter was specifically used because it was reimbursed fully by the Social Insurance Institution.
In all patients, intracranial hemorrhage was excluded by CT, and proximal large vessel occlusions were confirmed by CT angiography or MR angiography.
The clinical criterion for the decision of mechanical thrombectomy was the baseline NIHSS (National Institutes of Health Stroke Scale) score. Mechanical thrombectomy was performed for the patients with a baseline NIHSS score of ≥ 5 or aphasia if NIHSS was < 5 at admission.
Infarcts involving more than 1/3 of MCA (middle cerebral artery) territory were categorized as advanced ischemic damage, and these patients were not considered eligible for mechanical thrombectomy. Intravenous thrombolytic treatment was performed at the neurology department on patients who fulfilled the appropriate criteria.
Endovascular treatment
Three endovascular surgeons performed mechanical thrombectomies in two flagship hospitals. Endovascular surgeons utilized ADAPT as a thrombectomy method, and patients were under general anesthesia or sedation during the procedures. In all thrombectomies, initially, the SOFIA 6F was used as a primary aspiration catheter. However, in patients where aspiration attempts failed to achieve recanalization, SOFIA 6F was used as an intermediate catheter to support stent retriever devices.
First, the 6F Neuron MAX 088 (Penumbra, CA, USA) guiding catheter was placed in the most distal segment of the ICA (internal carotid artery) to which it could safely be advanced for the anterior circulation cases. During the posterior occlusions, the 6F guiding catheter was placed in the V2 segment or the subclavian artery. Subsequently, with the help of a microcatheter and microwire, the SOFIA 6F catheter was advanced to the thrombus site without passing through the clot. In decreasing order of frequency, the Rebar (Medtronic, MN, USA), Prowler (Codman, MA, USA), Vasco (Balt, Montmorency, France), and Headway (Microvention Terumo, CA, USA) were used as microcatheters; while, in decreasing order of frequency, different microwires such as Traxcess (Microvention Terumo, CA, USA), Hybrid (Balt, Montmorency, France), Synchro (Stryker Neurovascular, CA, USA), and Choice (Boston Scientific, MA, USA) were used. After inserting the distal end of the SOFIA 6F catheter into the proximal part of the clot, the microcatheter and microwire were removed, and aspiration was begun using a vacuum pump or a 20–60 ml syringe. After cessation of blood flow in the aspiration catheter, aspiration was continued for a further 2 min. The SOFIA 6F catheter was removed while aspiration was continuing. If the angiographic images obtained after aspiration revealed inadequate recanalization, the same procedure was repeated, or stent retriever thrombectomy was performed according to the decision of the operator.
In case of the operator’s decision to use a stent retriever, the microcatheter was passed through the thrombus, and a contrast agent was given via microcatheter to confirm its position. Following the insertion of the stent retriever into the microcatheter, the microcatheter was drawn back slowly to open the stent retriever. After removal of the microcatheter and stent retriever, control angiography images were obtained. The Solitaire (Medtronic, MN, USA), Trevo (Stryker Neurovascular, CA, USA), and Catch (Balt, Montmorency, France) were used as stent retrievers in decreasing order of frequency. In cases where adequate recanalization could not be achieved, the operator repeated or terminated the process.
In tandem occlusions, the stenotic segment was passed with a guidewire, and SpiderFX embolic protection device (Covidien, MA, USA) was deployed in the terminal segment of the cervical ICA. Subsequently, emergency percutaneous transluminal balloon angioplasty with Aviator Plus (Cordis Cardinal Health, OH, USA) was performed for the stenotic segment. If balloon angioplasty failed to achieve luminal patency, then additional carotid stenting with Protege RX (Medtronic, MN, USA) was performed to allow mechanical thrombectomy. After achieving adequate luminal patency, SOFIA 6F was navigated to the thrombus site, and direct aspiration thrombectomy was performed as described above.
After the thrombectomies, all patients were followed up in an inpatient setting and evaluated by a multidisciplinary team on a regular basis.
Data collection
The demographic data of 148 patients who were treated with the SOFIA 6F catheter were recorded. Acute thromboembolic intracranial occlusions with concomitant extracranial steno-occlusive lesions in the carotid artery were defined as tandem occlusions. National Institutes of Health Stroke Scale (NIHSS) scores on admission and discharge were used together with the modified Rankin Scale (mRS) scores at 90 days. The targeted clinical result after treatment was determined as an mRS score of ≤ 2. The clinical and angiographic data were analyzed, and the procedure-related time variables were calculated. The recanalization data were evaluated by the Thrombolysis in Cerebral Infarction (TICI) scale. Achieving a blood flow of TICI ≥ 2b was considered as a successful recanalization. The successful advancement rate of the SOFIA 6F catheter to the occlusion site and thrombectomy-related complications were recorded. Ethics approval was obtained from the local ethics committee.
Statistical analysis
For the quantitative data, the descriptive statistics were given as mean and standard deviation, whereas for the qualitative data, frequency and percentage were used. The statistical analysis of the data was carried out using the SPSS 23.0 statistical package (IBM, Armonk, New York, USA).
Results
Table 1 summarizes the baseline characteristics of the patients. The mean age of the 148 patients (81 men and 67 women) who had undergone direct aspiration thrombectomy using a SOFIA 6F catheter was 63.8 years (range 22–89 years). Of these 148 patients, 62 (41.8%) were referred to our institutions for mechanical thrombectomy. The thrombus was in the ICA in 47 (31.8%) patients; in the MCA, in 85 (57.4%) patients; and in the posterior system, in 16 (10.8%) patients (Table 1). The median duration from the onset of symptoms to vascular access in the groin was 205 min (IQR 163–260 min). In 17 cases, the exact time of the onset of symptoms was not clear. Intravenous thrombolytic therapy was administered to 32.4% of the cases. The median NIHSS score on admission was 14 (IQR 11–18). In 130 (87.8%) cases, the SOFIA 6F catheter was able to reach the occlusion site. However, initial aspiration thrombectomy could not be performed in the remaining 18 cases. The main reasons for failed advancement were extreme tortuosity, insufficient catheter length, and severe intracranial stenosis. For 19 tandem occlusions, a balloon angioplasty alone restored luminal patency in 17 cases, and additional stenting was required in the remaining 2. In all these 19 cases, steno-occlusive lesions were successfully passed, and SOFIA 6F reached the thrombus site.
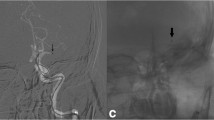
Table 2 summarizes revascularization results and complications. After direct thrombus aspiration, successful recanalization was achieved in 90 (69.2%) of the 130 patients. An additional stent retriever was used in 55/130 (42.3%) patients. In 18 patients, SOFIA 6F could not reach the clot level; therefore, stent retriever therapy was used as a first-line treatment. The mean time between vascular access and successful recanalization was 38 ± 33.2 min. Overall, successful recanalization could be achieved in 132/148 patients (89.1%), and the rate of successful recanalization was 16/19 (84.2%) for the tandem occlusions. In 28/75 (37.3%) cases, the SOFIA 6F catheter was able to reach the thrombus site without the help of a microcatheter and microwire (Fig. 1). The rate of complete recanalization (TICI 3) was 36.9% with direct aspiration and 52.7% in all cases. The median NIHSS score on discharge was 4 (IQR 2–10.5). The rate of patients with an mRS score of 0–2 at 90 days was 49.3%. Thromboembolic complications in new territories occurred in 8 cases. After treatment, a symptomatic intracranial hemorrhage (sICH) that increased the NIHSS score by 4 points or more within 24 h was observed in 8 patients. In three cases, intracranial dissection was detected after the use of the stent retriever. There was no complication directly related to the SOFIA 6F catheter. The mortality rate after the procedure was 14.1%.
Anterior–posterior angiogram of a patient with pretreatment NIHSS score of 16 revealing left M1 occlusion (a). SOFIA 6F’s tip (arrow) was positioned proximal to the thrombus without the help of microcatheter and microwire (b). Clot aspirated for 2 min with a 60 cc syringe (not shown). Anterior–posterior (c) and lateral (d) angiograms confirming TICI 3 revascularization. Post-treatment NIHSS score of the patient was 4. Modified Rankin Scale score at 90 days was 0. TICI thrombolysis in cerebral infarction, NIHSS National Institutes of Health Stroke Scale
Discussion
Mortality and hemorrhagic complication rates increase as the time to recanalization is prolonged in the treatment of acute ischemic stroke, and the clinical outcome becomes distanced from the intended results [12,13,14]. Thanks to the production of new-generation catheters, the time to successful recanalization with aspiration thrombectomy has shortened, and the clinical outcome after endovascular treatment has improved considerably [15,16,17,18].
Early recanalization directly affects the short-term and long-term clinical outcomes [13, 19, 20]. For quick and successful recanalization, the time passed until reaching the clot site should be as short as possible. Therefore, an effective aspiration catheter should contribute to shortening the time to recanalization by providing easy access to the thrombus site with minimum effort, even in the presence of tortuosity.
In our study, the rate of successful recanalization (TICI ≥ 2b) was 90/130 (69.2%) with direct aspiration and 132/148 (89.1%) after rescue therapy with stent retrievers. In thrombectomies performed with the SOFIA 6F Flow Plus, the rate of successful recanalization ranged from 70% to 73.3% with direct aspiration; while when used together with a stent retriever, this rate ranged between 90.2% and 96.5% [7, 8]. In the studies in which the SOFIA 5F and 6F Flow Plus catheters were used together, successful recanalization ranged from achieved in 77.8% and 91.8% with aspiration only; while in overall cases, this rate ranged between 82.1% and 86.1% [6, 9]. In a meta-analysis study including different aspiration catheters, the rate of successful recanalization was reported as 66% with direct aspiration and 89% with additional methods [21]. The rate of successful recanalization in our patients was similar to that in the literature. The difference between the rates of successful recanalization achieved with direct aspiration may be due to the fact that operators make different decisions between repeated aspiration trials and transition to additional treatment methods.
In our study, the intended clinical outcome (mRS score: 0–2) was achieved in 49.3% of cases. Kabbasch et al. achieved an mRS (0–2) rate of 43.2% in their patients with the SOFIA 5F catheter [5]. This rate was 49.4% in thrombectomy procedures performed using the SOFIA 6F Flow Plus catheter [8]. In thrombectomies performed with SOFIA 5F and 6F Flow Plus, the rate of intended clinical outcome ranged between 34.3% and 43% [6, 9]. In a meta-analysis evaluating the ADAPT technique, this rate was reported as 52% with different catheters [21].
The rate of sICH was reported as 10% with the SOFIA 5F [5] catheter and as 4.7% with the SOFIA 6F Flow Plus [8] catheter. In thrombectomies performed with SOFIA 5F and 6F Flow Plus, sICH observed in 6.2% and 7.1% [6, 9]. In a meta-analysis, sICH was observed in 5% of cases in whom different catheters were used [21]. In our study, this rate was 5.4%.
During the endovascular treatment, the rate of emboli to a new territory was reported to be 3% with the SOFIA 5F catheter [5]. With SOFIA 6F Flow Plus, this rate ranged from 4.7% to 4.8% [7, 8]. In thrombectomies performed with SOFIA 5F and 6F Flow Plus, this rate ranged between 1.4% and 4.3% [6, 9]. In our study, the rate of embolism to new territory was 5.4%. In a meta-analysis about the ADAPT, this rate was reported as 2% [21]. The frequency of thromboembolic events in our cases undergoing the thrombectomy procedure using the SOFIA 6F catheter was similar to that in recent studies on the ADAPT technique.
The mortality rate of cases undergoing the thrombectomy procedure with the SOFIA 6F catheter was 14.1%. The reported mortality rate in the procedures performed with the SOFIA 6F Flow Plus and 5F catheters varies between 13.9% and 25% [4,5,6, 8, 9]. In a meta-analysis, this rate was reported to be 15% [21].
Navigability and large luminal diameter are the essential components of an ideal aspiration catheter. Enhanced navigability is imperative to reach the thrombus, and a large lumen provides high aspiration force [11]. Since SOFIA catheters offer these features, SOFIA is commonly preferred in aspiration thrombectomy. In the current literature, researchers primarily focused on the performance of SOFIA Flow Plus with modern aspiration thrombectomy [6,7,8,9]. However, unfortunately, SOFIA Flow Plus is not available in some countries due to reimbursement issues. Therefore, in such countries, neurointerventionalists usually employ SOFIA 6F as a cost-effective alternative.
Despite the fact that SOFIA 6F is widely used in countries where SOFIA Flow Plus 6F is not available, the performance of SOFIA 6F as a primary aspiration catheter was unknown. In this study, we have reached the thrombus site at a rate of 87.8%, and our overall successful recanalization rate was 89.1% with ADAPT. Furthermore, our results were comparable to those of the SOFIA Flow Plus studies.
Limitations
First, our study was performed retrospectively. The TICI and mRS scores were evaluated by the authors, and this may have led to bias in data analysis.
Conclusion
In our study, we have evaluated various safety and efficacy parameters. Our recanalization and morbidity rates were encouraging and similar to those of studies conducted with other aspiration catheters. Therefore, our study indicates that aspiration thrombectomy with SOFIA 6F is feasible. Moreover, our results confirm that aspiration thrombectomy with SOFIA 6F is a highly effective option for neurointerventionalists who prefer SOFIA catheters in their practice but do not have access to SOFIA Flow Plus.
References
Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res. 2017;120(3):439–48.
Bhatia R, Hill MD, Shobha N, Menon B, Bal S, Kochar P, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real-world experience and a call for action. Stroke. 2010;41(10):2254–8.
Heit JJ, Wong JH, Mofaff AM, Telischak NA, Dodd RL, Marks MP, et al. Sofia intermediate catheter and the SNAKE technique: safety and efficacy of the Sofia catheter without guidewire or microcatheter construct. J NeurointervSurg. 2018;10(4):401–6.
Stampfl S, Kabbasch C, Muller M, Mpotsaris A, Brockmann M, Liebig T, et al. Initial experience with a new distal intermediate and aspiration catheter in the treatment of acute ischemic stroke: clinical safety and efficacy. J NeurointervSurg. 2016;8(7):714–8.
Kabbasch C, Möhlenbruch M, Stampfl S, Mpotsaris A, Behme D, Liebig T. First-line lesional aspiration in acute stroke thrombectomy using a novel intermediate catheter: initial experiences with the SOFIA. IntervNeuroradiol. 2016;22(3):333–9.
Nouri N, Ferrigno M, Personnic T, Bala F, Bretzner M, Estrade L, et al. Real-world thrombectomy using the Sofia catheter. World Neurosurg. 2019;122:e1247–51.
Shallwani H, Shakir HJ, Rangel-Castilla L, Davies JM, Sonig A, Sattur MG, et al. Safety and efficacy of the sofia (6F) plus distal access reperfusion catheter in the endovascular treatment of acute ischemic stroke. Neurosurgery. 2018;82(3):312–21.
Möhlenbruch MA, Kabbasch C, Kowoll A, Broussalis E, Sonnberger M, Muller M, et al. Multicenter experience with the new SOFIA Plus catheter as a primary local aspiration catheter for acute stroke thrombectomy. J NeurointervSurg. 2017;9(12):1223–7.
Marnat G, Barreau X, Detraz L, Bourcier R, Gory B, Sgreccia A, et al. First-line Sofia aspiration thrombectomy approach within the endovascular treatment of ischemic stroke multicentric registry: efficacy, safety, and predictive factors of success. AJNR Am J Neuroradiol. 2019;40(6):1006–12.
Oguz S, Dinc H, Ozturk MH. A back and forth manual aspiration technique using a SOFIA Plus catheter for acute ischemic stroke: technical note. Neuroradiology. 2019;61(1):109–11.
Hu YC, Stiefel MF. Force and aspiration analysis of the ADAPT technique in acute ischemic stroke treatment. J NeurointervSurg. 2016;8(3):244–6.
Alawieh A, Chatterjee AR, Vargas J, Chaudry MI, Lena J, Turner R, et al. Lessons learned over more than 500 stroke thrombectomies using ADAPT with increasing aspiration catheter size. Neurosurgery. 2020;86(1):61–70.
Mazighi M, Chaudhry SA, Ribo M, Khatri P, Skoloudik D, Mokin M, et al. Impact of onset-to-reperfusion time on stroke mortality: a collaborative pooled analysis. Circulation. 2013;127(19):1980–5.
Mayasi Y, Helenius J, Goddeau RP, Moonis M, Henninger N. Time to presentation is associated with clinical outcome in hemispheric stroke patients deemed ineligible for recanalization therapy. J Stroke Cerebrovasc Dis. 2016;25(10):2373–9.
Primiani CT, Vicente AC, Brannick MT, Turk AS, Mocco J, El L, et al. Direct aspiration versus stent retriever thrombectomy for acute stroke: a systematic review and meta-analysis in 9127 patients. J Stroke Cerebrovasc Dis. 2019;28(5):1329–37.
Turk AS, Siddiqui A, Fifi JT, De Leacy RA, Fiorella DJ, Gu E, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet. 2019;393(10175):998–1008.
Itabashi R, Shigehatake Y, Yazawa Y, Fukuma K, Akamatsu Y, Omodaka S, et al. The effect of the first-line devices for endovascular treatment on the recanalization efficacy and the functional outcome in acute ischemic stroke patients. J Stroke Cerebrovasc Dis. 2017;26(4):893.
Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA J Am Med Assoc. 2017;318(5):443–52.
Seker F, Pfaff J, Wolf M, Ringleb PA, Nagel S, Schönenberger S, et al. Correlation of thrombectomy maneuver count with recanalization success and clinical outcome in patients with ischemic stroke. AJNR Am J Neuroradiol. 2017;38(7):1368–71.
Yoshie T, Ueda T, Takada T, Nogoshi S, Miyashita F, Takaishi S, et al. Effects of pretreatment cerebral blood volume and time to recanalization on clinical outcomes in endovascular thrombectomy for acute ischemic stroke. J Stroke Cerebrovasc Dis. 2018;27(7):1802–9.
Gory B, Armoiry X, Sivan-Hoffmann R, Piotin M, Mazighi M, Lapergue B, et al. A direct aspiration first pass technique for acute stroke therapy: a systematic review and meta-analysis. Eur J Neurol. 2018;25(2):284–92.
Funding
Researchers did not receive any funding for this work.
Author information
Authors and Affiliations
Contributions
CB and YD contributed to the design and implementation of the research, and the writing of the manuscript. CH contributed to the data collection and analysis of the data. OFN and BH contributed to supervised the findings of this work. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Bilgin, C., Durmus, Y., Haki, C. et al. Direct aspiration thrombectomy experience with the SOFIA 6F catheter in acute ischemic stroke. Jpn J Radiol 39, 605–610 (2021). https://doi.org/10.1007/s11604-021-01090-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-021-01090-z