Abstract
Aim
Recently, nuclear cardiology has dramatically advanced by a new technology development such as the device, short-term acquisition system, image reconstruction algorithm and image analysis. Although these innovations have been gradually employed in routine examinations, we did not investigate the current use of image acquisition, image reconstruction, and image analysis with myocardial perfusion single-photon emission computed tomography (MPS). We investigated the current status of MPS imaging technology in Japan.
Methods
We carried out a survey using a Web-based questionnaire system, the opening of which was announced via e-mail, and it was available on a website for 3 months. We collected data on the current use of MPS with 201Tl and/or 99mTc agents with respect to routine protocols, image acquisition, image reconstruction, and image analysis.
Results
We received responses to the Web-based questionnaire from 178 and 174 people for 99mTc and 201Tl MPS, respectively. The routine protocols of MPS of stress-rest and rest-stress MPS on 1-day protocols with 99mTc were 41.2% and 14.5%, respectively, and the rest-only scan response rate was 23.7%, whereas that of 201Tl MPS was 65.9% with stress-rest MPS, 19.0% with rest-only MPS, and 10.9% with stress-rest MPS adding a rest scan 24 h after injection. The filtered back projection (FBP) method is most commonly used image reconstruction method, yielding 70.5% for 99mTc MPS and 76.8% for 201Tl MPS, including combined FBP and ordered subset expectation maximization method. The results for no-correction (NC) images were 49.2% with 99mTc MPS and 55.2% with 201Tl MPS including the response of NC and combined attenuation correction (AC) and scatter correction (SC) (i.e., ACSC) images. The AC or ACSC images of 99mTc and 201Tl were provided by 30–40% of the institutions surveyed.
Conclusions
We investigated the current status of MPS imaging technology in Japan, and found that although the use of various technical developments has been reported, some of these technologies have not been utilized effectively. Hence, we expect that nuclear medicine technology will be used more effectively to improve diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Nuclear cardiologists have performed disease severity assessment, decisions regarding treatment strategies, evaluation of treatment effects, and prognosis of cardiac diseases (e.g., ischemic heart disease and myocardial infarction) using qualitative images and quantitative indexes created from myocardial perfusion single-photon emission computed tomography (MPS). Recommendations on the use of image acquisition, image reconstruction, and image analysis have been published by expert nuclear cardiologists in several academic conferences [1,2,3,4,5,6]. Dramatic advances have been made in the field of nuclear cardiology thanks to recent technological developments, such as the use of short-term image acquisition, image reconstruction algorithms, and image analysis [7,8,9,10,11,12]. Although these innovations have been gradually employed in routine examinations, the current use of image acquisition, image reconstruction and image analysis with MPS has not been investigated so far.
The device of MPS is becoming more multifaceted; dedicated cardiac cadmium zinc telluride camera and single-photon emission computed tomography (SPECT)–computed tomography (CT) scanner is gradually beginning to spread across Japan. Therefore, it is now much easier to provide an attenuation correction (AC) with CT or an absolute quantitative index of myocardial blood flow and myocardial flow reserve [13]. In addition, the ordered subset expectation maximization (OSEM) method incorporating scatter correction (SC), AC and resolution correction (RC) can be rapidly processed because of the improvements made in the processing power of personal computers, which contributes to improvements in the diagnostic accuracy [14,15,16]. Hence, these technologies can now be used more easily than before. Unlike other countries, the acquisition and image reconstruction parameters of MPS in Japan are mainly determined by nuclear medicine technologists who are also licensed radiological technologists, not by nuclear cardiologists or medical physicists. Therefore, a nationwide survey on MPS is also important in raising awareness regarding the role of nuclear medicine technologists, which will lead to an improvement in the diagnostic accuracy. The aim of this study was to investigate the current status of MPS imaging technology in Japan.
Materials and methods
Study design
A research survey was performed using a Web-based questionnaire system of the Japanese Society of Radiological Technology (JSRT). The opening of the questionnaire survey was announced to the members of the JSRT (approximately 9000 people) via e-mail, and it was conducted online for 3 months (from October to December 2017). The survey was approved by the Human Research Ethics Committee of the hospital to which the research leader and coauthor belong.
Questionnaire contents
We collected data on the management style of the participating institutions, the levels of experience of their nuclear medicine technologists and the presence of professional licensees of the Japan Board of Nuclear Medicine Technology (JBNMT) to figure out the profiles of the questionnaire respondents. We also collected the current status of MPS with 201Tl and/or 99mTc agents with respect to routine protocols, image acquisition, image reconstruction, and image analysis methods, as shown in Table 1. The options of the routine protocol with 99mTc were set as follows: stress-rest (1 day), rest-stress (1 day), stress-rest (2 days), rest-stress (2 days), stress only, and others. Stress-rest (1 day) means the stress-first MPS protocol, whereas rest-stress (1 day) is the rest-first MPS protocol. Stress-rest (2 days) and rest-stress (2 days) mean performing stress and rest MPS, respectively, on different days. We allowed multiple responses for the routine pattern of image acquisition, reconstruction, correction, and analysis to respond to various examination situations.
Results
We received responses to the Web-based questionnaire from 226 people. Questionnaires related to 99mTc and 201Tl MPS were answered by 178 and 174 people, respectively (response ratio: 2% for both 99mTc and 201Tl), including 126 people who answered both questionnaires for 99mTc and 201Tl MPS. Among all institutions, respondents from a public hospital were the most: 66 (37.1%) people for 99mTc and 62 (35.6%) people for 201Tl. Furthermore, many of the respondents were nuclear medicine technologists who had more than 10 years of experience, whereas respondents of a professional license for JBNMT were less than 50% each for both 99mTc and 201Tl MPS (Table 2).
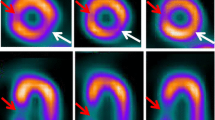
The routine protocols for 99mTc and 201Tl MPS are shown in Fig. 1. The response rate of routine protocol for 99mTc MPS was 41.2% and 14.5% with stress-rest and rest-stress MPS on 1-day protocols, and the rest-only scan was 23.7%, respectively. Stress-only MPS or stress-rest MPS on 2 days’ protocol was categorized as “Others” in Fig. 1. The response rate of 201Tl MPS was 65.9% for stress-rest MPS, 19.0% for rest-only MPS, and 10.9% for stress-rest MPS adding rest scan with 24 h after injection. Stress-rest with reinjection MPS and stress-only MPS are categorized as “Others” in Fig. 1. The response rate of routine image acquisition pattern for SPECT only and SPECT–CT only was approximately 40% and 15% for both 99mTc and 201Tl MPS, respectively. Furthermore, planar scans of 99mTc and 201Tl were performed 41% and 43.8%, respectively (Fig. 2). The response rate of supine MPS with 99mTc and 201Tl was approximately 90%, and prone or upright positions were acquired as the routine examination in the part of the hospital (5.6% and 2.0% with 99mTc and 201Tl MPS).
The filtered back projection (FBP) method was the most commonly used image reconstruction method, with results of 70.5% with 99mTc MPS and 76.8% with 201Tl MPS, including the combined FBP and OSEM methods (Fig. 3). The OSEM with RC was 66.7% for 99mTc and 63.6% for 201Tl in all OSEM methods. The no-correction (NC) images were 49.2% with 99mTc MPS and 55.2% with 201Tl MPS including the response of NC and combined AC and SC (ACSC) images (Fig. 4). The AC or ACSC images of 99mTc and 201Tl were provided by 30–40% of the institutions, and many hospitals (approximately 75% using both 99mTc and 201Tl) with a SPECT–CT scanner created those images using CT-based AC (CTAC).
More than 50% of the respondents reported that their preferred image analysis method was processed by an electrocardiogram (ECG) gating process, scoring both 99mTc and 201Tl MPS, and washout rate of 201Tl MPS (Table 3). In particular, the gating process of 99mTc MPS was performed in most of the respondent hospitals. Various validation techniques were adopted, such as phase analysis, computer-aided diagnosis, fusion image combined coronary CT angiography (CCTA) and MPS image, and absolute quantitative analysis.
In most of the institutions, decisions to use additional images or to omit routine images were performed by nuclear cardiologists. The hospitals that acted upon the judgment of nuclear medicine technologists achieved results of 18.0% with 99mTc and 13.8% with 201Tl. For example, when some of the respondents generated artifacts by a high accumulation of liver, gallbladder or bowels, there were underestimation of the LV volume for small hearts and detection of an abnormal physiological uptake pattern. Therefore, they provided nuclear cardiologists with additional images. Furthermore, if we performed the MPS with an arrhythmia, implantation of a pacemaker or small heart patients, some respondents omitted the gating process.
Discussion
Even though MPS with 201Tl produces more radiation exposure compared to that with 99mTc, it is still widely used in Japan [17]. MPS with 201Tl in Japan has a greater level of diagnostic evidence than that with 99mTc, having been in use for a longer time [4]. Furthermore, 201Tl MPS has several advantages: obtaining stress and rest images by a single injection of the radiopharmaceutical and calculating the washout rate. The washout rate is an additional index which is useful for risk stratification of ischemia [18]. In particular, diffuse slow washout of 201Tl is important as an indicator of multi-vessel coronary artery disease [19]. Therefore, many respondents performing the stress-rest 201Tl MPS provided the washout rate as the routine protocol. However, if re-distribution image from 3 to 4 h after injection is insufficient, the detection of a viable myocardium is underestimated. Twenty-four-hour delayed scan or fill-in scan after reinjection has been reported to improve the underestimation for detection of a viable myocardium [20, 21]. Only a small number of respondent institutions undertook those scans routinely. 99mTc MPS has various advantages, such as a high quantitative accuracy and image quality, as well as improved inferior attenuation compared with 201Tl MPS [22,23,24]. Therefore, the ratio of 99mTc to 201Tl in MPS has been gradually increasing in Japan [17].
Recently, stress-only MPS with 99mTc has been attracting attention related to radiation exposure and patient burden [25], but it has not been commonly performed. Many hospitals suffer from a shortage of nuclear cardiologists and so do not consistently have the facilities to interpret images of stress MPS. Nuclear cardiologists cannot, therefore, judge immediately after an examination using stress MPS whether rest MPS is necessary. To expand the use of stress-only MPS in the future, it will be necessary to determine criteria for quantitative indices and image interpretation that can judge stress MPS images in the absence of nuclear cardiologists.
A planar image is often acquired in addition to MPS. Planar image with 201Tl can help analyze the lung-to-heart ratio as a quantitative index, which is useful in the detection of multi-vessel disease [26, 27], wall thickening, evaluation of the left ventricular chamber, and detection of diseases like tumors other than cardiac disease [28, 29]. Multi-vessel diseases are particularly difficult to diagnose from nuclear medicine images, due to display of relative value normalized by the maximum value. Therefore, the lung-to-heart ratio will offer good diagnostic support. Similarly, a planar image with 99mTc is useful for the detection of incidental tumors and in assisting with the long-term prognosis of multi-vessel disease [30, 31]. Therefore, a planar image should be acquired regardless of whether 99mTc or 201Tl is used.
CTAC reduces the likelihood for a false positive of the inferior wall [12]. However, 25% of hospitals with SPECT–CT scanners do not perform a CTAC. Furthermore, an additional scan in a prone or an upright positions is also very useful in improving the attenuation artifacts of the inferior wall [32,33,34,35]. However, the MPS images of these positions were less than 5% of the routine examination. There are disadvantages associated with myocardial imaging with CTAC, such as the insufficient maintenance of the normal database (NDB) and the increase in radiation exposure. In particular, the NDBs created by the Japanese Society of Nuclear Medicine (JSNM) consist only of myocardial images without AC [36, 37]. Thus, NDBs data that provide the quantitative index of myocardial image with AC are insufficient. It is also noted that the criteria to perform additional scans of prone or upright positions have not been clarified. If there is no nuclear cardiologist at an institution, the use of an additional scan must be determined by a nuclear medicine technologist. Consequently, it is very important to set the criteria for additional scans and to expand NDBs to include images with AC.
The MPS images reconstructed using OSEM with AC, SC, and RC have been reported to be useful for improving the diagnostic accuracy [14, 15, 38]. Furthermore, OSEM can improve streak-artifact caused by the strong accumulation of liver, gallbladder and/or bowels. However, MPS images were reconstructed by FBP without AC, SC, and RC in many hospitals. One of several reasons may be that the maintenance of NDBs is inadequate, and so a JSNM working group created the Japanese NDB from the MPS image reconstructed by FBP [36, 37]. The NDB for scanner-specific systems has also gradually been added in recent years [8, 39, 40], but the NDBs of OSEM with and without SC, AC, and RC have not been reported yet. Differences in image reconstruction and correction patterns affect the normal values of %uptake. In particular, the RC algorithm is different for each vendor [41,42,43] and it is difficult to create the NDB of OSEM with RC. Efforts to add to the NDB will be very important in the future expansion of OSEM incorporating AC, SC, and RC. OSEM with RC is useful for patients with small hearts to improve the partial volume effect [16], and this effect depends on the RC algorithm. However, OSEM with RC has been reported to overestimate the quantitative index owing to the presence of a Gibbs artifact [44]. Some venders always include the RC when SPECT data are reconstructed with the OSEM method. Therefore, OSEM with RC images must be checked for Gibbs artifacts. To improve the problem of NDBs and artifacts, images from some hospitals were reconstructed using both the FBP and the OSEM methods. Therefore, it is important that nuclear cardiologists understand the image interpretation arising from different image reconstructions.
Each quantitative index of gated MPS improves the diagnostic accuracy by the adding of a non-gated MPS image [45, 46], and there are important considerations arising from these indexes. The end-diastolic volume and end-systolic volume (ESV) by partial volume effect in Japanese women and pediatric patients have been underestimated, and this has been particularly remarkable with the ESV, with some improvements reported [16, 47]. As these methods can be easily used, they should be positively encouraged. Another point is that in arrhythmic patients, it is possible that a false impression of wall thickening would reduce the benefits of incorporating visual assessments of thickening and motion into perfusion observations and inhibit the recognition of artifacts [48]. Some of the respondents omitted acquiring a gated MPS of arrhythmic patients, only having acquired a non-gate MPS. If a gated MPS is performed on arrhythmic patients, attention should be paid to the interpretation of quantitative indexes.
The number of CCTAs dramatically increases every year in Japan. However, the fusion imaging of MPS and CCTA was less than 16%. This may be because the software needed for creating fusion images of MPS and CCTA is not part of standard packages, but must be purchased separately from venders. Additionally, if workstations are set up outside nuclear medicine rooms, the workflow of nuclear medicine technologists becomes more complicated. We have also found that the number of fusion images of CCTA and MPS increases with the increase in CCTA, but CCTAs cannot be performed routinely because of the lack of manpower. Fusion images improve the sensitivity and specificity in the diagnosis of coronary artery disease [49]. Moreover, it helps distinguish whether the affected coronary artery is RCA or LCX if there is an ischemic finding in the inferolateral wall in MPS [50]. We, therefore, strongly recommend creating fusion images where a CCTA is carried out before or after MPS.
MPS is rarely carried out beyond acquisition protocols, image reconstruction, and image processing other than in routine examinations, and the guidelines for its use are based on a considerable body of evidence [1,2,3,4,5,6]. Certain guidelines for the image acquisition and image processing protocols needed for performing routine examinations are determined by each hospital, and we found minor differences between hospitals. Thus, MPS diagnosis should be possible with only image acquisition protocols and image processing for routine examinations in most cases.
The questionnaire could not obtain a high response rate, because it contained the members of JSRT who had not worked in nuclear medicine, and there are approximately 450 JSRT members working in nuclear medicine. Therefore, we assumed a response rate of approximately 40% (174 or 178 out of 450 people). Every respondent to our questionnaire was the only member of JSRT in his/her hospital department of nuclear medicine. Thus, we believe that our results reflect the current state of nuclear medicine technology in Japan, but there is little other survey on the state of nuclear medicine [51, 52]. Therefore, the results of our research will provide important data for the improvement of MPS technology.
Conclusion
We have investigated the current status of MPS imaging technology in Japan, and found that, despite the use of various technological developments that have been reported, some of these technologies have not been effectively utilized. Hence, we expect that nuclear medicine technology will be used more effectively to improve diagnosis.
References
Verberne HJ, Acampa W, Anagnostopoulos C, Ballinger J, Bengel F, De Bondt P, et al. EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur J Nucl Med Mol Imaging. 2015;42:1929–40.
Strauss HW, Miller DD, Wittry MD, Cerqueira MD, Garcia EV, Iskandrian AS, et al. Procedure guideline for myocardial perfusion imaging 3.3. J Nucl Med Technol. 2008;36:155–61.
Society of nuclear medicine. The SNM procedure guideline for general imaging 6.0. https://snmmi.files.cms-plus.com/docs/General_Imaging_Version_6.0.pdf (Reference 2019.7.18)
JCS, Joint Working Group. Guidelines for clinical use of cardiac nuclear medicine (JCS 2010) – digest version –. Circ J. 2012;76:761–7.
Arumugam P, Harbinson M, Reyes E, Sabharwal N, Tonge C, Underwood R, et al. Procedure guidelines for radionuclide myocardial perfusion imaging with single-photon emission computed tomography. Nucl Med Commun. 2013;34:813–26.
Fathala A. Myocardial perfusion scintigraphy: techniques, interpretation, indications and reporting. Ann Saudi Med. 2011;31:625–34.
Sun XX, Tian YQ, Wang DY, He ZX. Shortened acquisition time or reduced-activity dose for gated myocardial perfusion SPECT with new reconstruction algorithm. Int J Cardiovasc Imaging. 2013;29:1287–93.
Nakajima K, Okuda K, Momose M, Matsuo S, Kondo C, Sarai M, et al. IQ·SPECT technology and its clinical applications using multicenter normal databases. Ann Nucl Med. 2017;31:649–59.
Onoguchi M, Konishi T, Shibutani T, Matsuo S, Nakajima K. Technical Aspects Image Reconstruction. Ann Nucl Cardiol. 2016;2:68–72.
Shibutani T, Nakajima K, Wakabayashi H, Mori H, Matsuo S, Yoneyama H, et al. Accuracy of an artificial neural network for detecting a regional abnormality in myocardial perfusion SPECT. Ann Nucl Med. 2019;33:86–92.
Fiechter M, Ghadri JR, Kuest SM, Pazhenkottil AP, Wolfrum M, Nkoulou RN, et al. Nuclear myocardial perfusion imaging with a novel cadmium–zinc–telluride detector SPECT/CT device: first validation versus invasive coronary angiography. Eur J Nucl Med Mol Imaging. 2011;38:2025–30.
Sharma P, Patel CD, Karunanithi S, Maharjan S, Malhotra A. Comparative accuracy of CT attenuation-corrected and non-attenuation-corrected SPECT myocardial perfusion imaging. Clin Nucl Med. 2012;37:332–8.
Nkoulou R, Fuchs TA, Pazhenkottil AP, Kuest SM, Ghadri JR, Stehli J, et al. Absolute Myocardial Blood Flow and Flow Reserve Assessed by Gated SPECT with Cadmium–Zinc–Telluride Detectors Using 99mTc-Tetrofosmin: Head-to-Head Comparison with 13N-Ammonia PET. J Nucl Med. 2016;57:1887–922.
Harel F, Génin R, Daou D, Lebtahi R, Delahaye N, Helal BO, et al. Clinical impact of combination of scatter, attenuation correction, and depth-dependent resolution recovery for (201)Tl studies. J Nucl Med. 2001;42:1451–6.
Velidaki A, Perisinakis K, Koukouraki S, Koutsikos J, Vardas P, Karkavitsas N. Clinical usefulness of attenuation and scatter correction in Tl-201 SPECT studies using coronary angiography as a reference. Hellenic J Cardiol. 2007;48:211–7.
Yoneyama H, Nakajima K, Okuda K, Matsuo S, Onoguchi M, Kinuya S, et al. Reducing the small-heart effect in pediatric gated myocardial perfusion single-photon emission computed tomography. J Nucl Cardiol. 2017;24:1378–88.
Subcommittee on Survey of Nuclear Medicine Practice in Japan. The Present State of Nuclear Medicine Practice in Japan—a Report of the 8th Nationwide Survey in 2017. Radioisotopes. 2018;67:339–87.
Koskinen M, Pöyhönen L, Seppänen S. Thallium-201 washout in coronary artery disease using SPECT—a comparison with coronary angiography. Eur J Nucl Med. 1987;12:609–12.
Bateman TM, Maddahi J, Gray RJ, Murphy FL, Garcia EV, Conklin CM, et al. Diffuse slow washout of myocardial thallium-201: a new scintigraphic indicator of extensive coronary artery disease. J Am Coll Cardiol. 1984;4:55–64.
He YM, Yang XJ, Wu YW, Zhang B. Twenty-four-hour thallium-201 imaging enhances the detection of myocardial ischemia and viability after myocardial infarction: a comparison study with echocardiography follow-up. Clin Nucl Med. 2009;34:65–9.
Tamaki N, Ohtani H, Yonekura Y, Nohara R, Kambara H, Kawai C, et al. Significance of fill-in after thallium-201 reinjection following delayed imaging: comparison with regional wall motion and angiographic findings. J Nucl Med. 1990;31:1617–23.
Germano G, Erel J, Kiat H, Kavanagh PB, Berman DS. Quantitative LVEF and qualitative regional function from gated thallium-201 perfusion SPECT. J Nucl Med. 1997;38:749–54.
Wang SJ, Chen YT, Hwang CL, Lin MS, Kao CH, Yeh SH. 99mTc-sestamibi can improve the inferior attenuation of TL-201 myocardial spect imaging. Int J Card Imaging. 1993;9:87–92.
DePuey EG, Parmett S, Ghesani M, Rozanski A, Nichols K, Salensky H. Comparison of Tc-99m sestamibi and Tl-201 gated perfusion SPECT. J Nucl Cardiol. 1999;6:278–85.
Chang SM, Nabi F, Xu J, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: similar patient mortality with reduced radiation exposure. J Am Coll Cardiol. 2010;55:221–30.
Hitzel A, Manrique A, Cribier A, Véra P. Diagnostic value of Tl-201 lung uptake is dependent on measurement method. J Nucl Cardiol. 2001;8:332–8.
Boucher CA, Zir LM, Beller GA, Okada RD, McKusick KA, Strauss HW, et al. Increased lung uptake of thallium-201 during exercise myocardial imaging: clinical, hemodynamic and angiographic implications in patients with coronary artery disease. Am J Cardiol. 1980;46:189–96.
-Talavera P, Olmos R, -Esteban A, Ruiz MÁ, González ML, Gamazo C. Evaluation by SPECT-CT of an incidental finding of a thymoma and breast cancer in a myocardial perfusion SPECT with 99mTc-MIBI. Rev Esp Med Nucl Imagen Mol. 2013;32:260–2.
Tseng JC, Hua CC, Tsai MF, Chang LC. Incidental detection of an invasive thymoma during thallium-201 imaging for coronary artery disease. Chang Gung Med J. 2004;27:138–42.
Markopoulos C, Sampalis F, Zerva C, Kiriaki D, Kitsou E, Alevizou-Terzaki V, Gogas J. 99mTc Tetrofosmin imaging in breast tumours. Eur J Gynaecol Oncol. 1998;19:163–6.
Georgoulias P, Tsougos I, Valotassiou V, Tzavara C, Xaplanteris P, Demakopoulos N. Long-term prognostic value of early poststress (99m)Tc-tetrofosmin lung uptake during exercise (SPECT) myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2010;37(4):789–98.
Arsanjani R, Hayes SW, Fish M, Shalev A, Nakanishi R, Thomson LE, et al. Two-position supine/prone myocardial perfusion SPECT (MPS) imaging improves visual inter-observer correlation and agreement. J Nucl Cardiol. 2014;21:703–11.
Nakaya K, Onoguchi M, Nishimura Y, Kiso K, Otsuka H, Nouno Y, et al. Criteria for the addition of prone imaging to myocardial perfusion single-photon emission computed tomography for inferior wall. Nucl Med Commun. 2017;38:748–55.
Nakazato R, Tamarappoo BK, Kang X, Wolak A, Kite F, Hayes SW, et al. Quantitative upright-supine high-speed SPECT myocardial perfusion imaging for detection of coronary artery disease: correlation with invasive coronary angiography. J Nucl Med. 2010;51:1724–31.
Nakaya K, Onoguchi M, Nishimura Y, Kiso K, Otsuka H, Nouno Y, et al. Comparison Between Prone and Upright Imaging of the Inferior Wall Using 201TlCl Myocardial Perfusion SPECT. J Nucl Med Technol. 2017;45(4):304–8.
Nakajima K, Kumita S, Ishida Y, Momose M, Hashimoto J, Morita K, et al. Creation and characterization of Japanese standards for myocardial perfusion SPECT: database from the Japanese Society of Nuclear Medicine Working Group. Ann Nucl Med. 2007;21:505–11.
Nakajima K, Matsumoto N, Kasai T, Matsuo S, Kiso K, Okuda K. Normal values and standardization of parameters in nuclear cardiology: Japanese Society of Nuclear Medicine working group database. Ann Nucl Med. 2016;30:188–99.
Ohyama Y, Tomiguchi S, Kira T, Kira M, Tsuji A, Koi A, et al. Diagnostic accuracy of simultaneous acquisition of transmission and emission data with technetium-99m transmission source on thallium-201 myocardial SPECT. Ann Nucl Med. 2001;15:21–6.
Okuda K, Nakajima K, Matsuo S, Kondo C, Sarai M, Horiguchi Y, et al. Creation and characterization of normal myocardial perfusion imaging databases using the IQ·SPECT system. J Nucl Cardiol. 2018;25:1328–37.
Ishihara M, Onoguchi M, Taniguchi Y, Shibutani T. Comparison of conventional and cadmium-zinc-telluride single-photon emission computed tomography for analysis of thallium-201 myocardial perfusion imaging: an exploratory study in normal databases for different ethnicities. Int J Cardiovasc Imaging. 2017;33:2057–66.
Frey EC, Gilland KL, Tsui BM. Application of task-based measures of image quality to optimization and evaluation of three-dimensional reconstruction-based compensation methods in myocardial perfusion SPECT. IEEE Trans Med Imaging. 2002;21:1040–50.
Jinghan Y, Xiyun S, Zuo Z, Da Silva. Iterative SPECT Reconstruction using matched filtering for improved image quality. In: Nuclear science symposium conference IEEE. 2006; p. 2285–2287.
Vija H, Hawman EG, Engdahl JC. Analysis of a SPECT OSEM reconstruction method with 3D beam modeling and optional attenuation correction: phantom studies. In: 2003 IEEE nuclear science symposium, Medical imaging conference. 2003, Portland, USA, p. 2662–2666.
Onishi H, Motomura N, Fujino K, Natsume T, Haramoto Y. Quantitative performance of advanced resolution recovery strategies on SPECT images: evaluation with use of digital phantom models. Radiol Phys Technol. 2013;6(1):42–53.
Taillefer R, DePuey EG, Udelson JE, Beller GA, Latour Y, Reeves F. Comparative diagnostic accuracy of Tl-201 and Tc-99m sestamibi SPECT imaging (perfusion and ECG-gated SPECT) in detecting coronary artery disease in women. J Am Coll Cardiol. 1997;29:69–77.
Links JM, DePuey EG, Taillefer R, Becker LC. Attenuation correction and gating synergistically improve the diagnostic accuracy of myocardial perfusion SPECT. J Nucl Cardiol. 2002;9:183–7.
Nakajima K, Okuda K, Nyström K, Richter J, Minarik D, Wakabayashi H, et al. Improved quantification of small hearts for gated myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2013;40:1163–70.
Nichols K, Yao SS, Kamran M, Faber TL, Cooke CD, DePuey EG. Clinical impact of arrhythmias on gated SPECT cardiac myocardial perfusion and function assessment. J Nucl Cardiol. 2001;8:19–30.
Santana CA, Garcia EV, Faber TL, Sirineni GK, Esteves FP, Sanyal R, et al. Diagnostic performance of fusion of myocardial perfusion imaging (MPI) and computed tomography coronary angiography. J Nucl Cardiol. 2009;16:201–11.
Yoneyama H, Nakajima K, Taki J, Wakabayashi H, Matsuo S, Konishi T, et al. Ability of artificial intelligence to diagnose coronary artery stenosis using hybrid images of coronary computed tomography angiography and myocardial perfusion SPECT. Eur J Hybrid Imaging. 2019;3:4.
Lindner O, Burchert W, Schäfer W, Hacker M. Myocardial perfusion SPECT 2015 in Germany. Results of the 7th survey. Nuklearmedizin. 2017;56:31–8.
Otsuka R, Kubo N, Miyazaki Y, Kawahara M, Takaesu J, Fukuchi K. Current status of stress myocardial perfusion imaging pharmaceuticals and radiation exposure in Japan: results from a nationwide survey. J Nucl Cardiol. 2017;24:1850–5.
Acknowledgements
The authors wish to thank all participating respondents for their effort in contributing to the surveys. We gratefully acknowledge the support of a JSRT research grant (2017 and 2018).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Ichikawa has received a research grant from JSRT. Other authors report no potential conflicts of interest relevant to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Shibutani, T., Okuda, K., Ichikawa, H. et al. Imaging technology for myocardial perfusion single-photon emission computed tomography 2018 in Japan. Jpn J Radiol 38, 274–282 (2020). https://doi.org/10.1007/s11604-019-00915-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-019-00915-2