Abstract
Purpose
We conducted a multi-institutional prospective study on accelerated partial breast irradiation (APBI) using interstitial brachytherapy. The clinical results over a minimum follow-up period of 30 months are presented here.
Materials and methods
Forty-six patients with breast cancer were treated with breast-conserving surgery and postoperative APBI. After confirmation of negative surgical margins and negative lymph nodes, a high-dose-rate brachytherapy protocol of 36 Gy/6 fractions was carried out. All clinical data were prospectively collected using the Common Terminology Criteria for Adverse Events ver. 3.0.
Results
No recurrence was observed. Cumulative rates of grade 2 or higher late sequelae were 25% for fibrosis, 2% for fractures, 9% for pain, and 9% for soft tissue necrosis. Rates of excellent or good cosmetic results as assessed by the physician and patient were 93 and 89% at the 12-month follow-up and 76 and 74% at the 30-month follow-up, respectively. Large volumes of resected tissue in small breasts were associated with fibrosis of grade 2 or higher.
Conclusion
APBI in Japanese women provides satisfactory clinical results except for cosmetic outcomes. There is some difficulty with the assessment of fibrosis and cosmetic outcomes, especially in patients with small breasts.
Clinical Trial Registration Number
UMIN000001677.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast-conserving therapy, which consists of breast-conserving surgery and postoperative radiation therapy, is the standard of care for early breast cancer. The most common postoperative radiation therapy is whole-breast irradiation (WBI), which has been proven to reduce the rate of local recurrence by one-third [1, 2]. However, several studies have reported that WBI only prevents recurrence near the tumor bed [3, 4]. Furthermore, the majority of local recurrences occur in the area neighboring the tumor bed [5, 6]. It should also be noted that WBI generally has a treatment period of several weeks and is reported to increase the risk of adverse cardiovascular events [2]. These factors drove us to reconsider the necessity of WBI in all patients.
Accelerated partial breast irradiation (APBI) using interstitial multicatheter brachytherapy may present a solution to the issues associated with WBI. In APBI, high-dose radiation is delivered to the tumor bed with minimal exposure of adjacent normal tissues. This method requires a much shorter treatment period (e.g., several days) than WBI. Recently, the results of a phase III clinical trial in Europe were published and demonstrated the noninferiority of APBI when compared to WBI [7]. On the other hand, APBI is not widely used in Japan. It is an attractive treatment option for Japanese patients who have limited time for treatment or for candidates who can avoid WBI [8].
As the first step in popularizing APBI in Japan, we conducted a trial to evaluate the applicability of APBI. This is the first multi-institutional prospective study on APBI in Japan. Early clinical results, including detailed treatment methods, have been published elsewhere [9, 10]. The results showed that the treatment methods were technically reproducible between institutions, and also showed excellent disease control with acceptable sequelae rates at a median follow-up of 26 months. However, during periodic follow-up meetings to assess the acquired data, several issues emerged. One great concern was the cosmetic results, and another was the fibrosis after radiotherapy, which had deteriorated over time. Together with some discussion of these issues, clinical results over the course of a minimum follow-up period of 30 months are reported here.
Materials and methods
The protocol was registered at the University Hospital Medical Information Network Clinical Trials Registry and was approved by the participating institutional review boards. As the details of the patient selection and the treatment methods have been previously described [9, 10], a summary is given below.
Patients
Patient eligibility criteria are summarized in Table 1. Forty-six patients from six institutions underwent the treatment regimen from October 2009 to December 2011. Written informed consent was obtained from all patients.
Treatment
All patients underwent breast-conserving surgery, wherein surgical clips were implanted at the resection margins. Brachytherapy applicators were implanted postoperatively in 45 patients after confirmation of negative surgical margins and negative lymph nodes. Postoperative implantation was carried out under imaging guidance, which consisted of ultrasonography in 44 patients and computed tomography (CT) in one patient. In one patient, the applicators were implanted during surgery. In that patient, negative surgical margins and negative lymph nodes were confirmed before the start of radiation therapy. Applicators were generally implanted in two or more planes. Single-plane implantation, which could lead to a nonhomogeneous dose distribution, was not allowed.
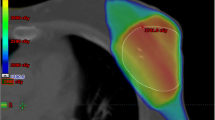
During the three-dimensional brachytherapy planning using CT images, 15-mm-radius balloons were drawn around the surgical clips. The spaces between the balloons were interpolated clinically and the reproduced volume was defined as the clinical target volume (CTV). The skin (5 mm thickness from the surface) and chest wall were excluded from the target volume. The radiation dose was prescribed using the Paris dosimetry system with manual modifications. A total dose of 36 Gy/6 fractions/3 days (with an interval of 6 h between the two fractions on the same day) was delivered to the surface of the CTV using a high-dose-rate Ir-192 brachytherapy system. To control the quality of brachytherapy, dose constraints were set as follows. The reference volume (Vref), which was the irradiated volume receiving ≥100% of the prescribed dose, was principally limited to the range 40–150 cm3. The dose nonuniformity ratio (DNR), which was defined as V1.5ref/Vref, was less than 0.35. V1.5ref is the irradiated volume receiving ≥150% of the prescribed dose. The clip dose had to be ≥6 Gy/fraction.
Systemic therapy was performed at the discretion of the treating physician. Chemotherapy was not allowed during the protocol treatment period and for 2 weeks thereafter.
Follow-up
All clinical data were prospectively collected every 2 weeks for 1 month, every 3 months until 24 months after treatment, and every 6 months thereafter until 60 months. Case report forms included 12 items (dermatitis, ulceration, infection, hypopigmentation, hyperpigmentation, telangiectasia, fibrosis, fracture, pain, pneumonitis, pneumothorax, and soft tissue necrosis) that had been reported in the previous APBI literature. The item of soft tissue necrosis was used for assessing fat necrosis. These items were scored by the physician according to the Common Terminology Criteria for Adverse Events ver. 3.0 (CTCAE). Cosmetic outcomes were assessed independently by the physician and by the patient, and recorded every 6 months, using the 4-point Harvard scale [11]. The cosmetic outcomes were graded as follows: excellent—the treated breast looked essentially the same as the opposite breast; good—minimal but identifiable effects of radiation on the treated breast; fair—significant effects of radiation on the treated breast were noted; poor—severe normal tissue sequelae.
Analysis
The primary endpoint of this study was the verification of the reproducibility of APBI using interstitial brachytherapy. This finding was published elsewhere [9]. The secondary endpoints were the probabilities of sequelae, the local control rate, and cosmetic results, which are presented in this article.
Additional analyses were performed to clarify the relationships between cosmetic results and several factors: bra cup size, resected tissue weight, number of applicators, implant plane, Vref, V1.5ref, V2.0ref (irradiated volume receiving ≥200% of the prescribed dose), DNR, CTV mean dose, CTV volume, V100 (volume of CTV subjected to the prescribed dose), D100 (the minimum dose delivered to the CTV), maximum skin dose, conformity index, and degree of fibrosis. The relationships between fibrosis and the other factors were also evaluated.
Follow-up time was calculated from the day of implantation. Statistical analysis was performed using JMP ver. 10 software (SAS Institute Inc.). The Kaplan–Meier method was used to evaluate radiation sequelae rates. Factors associated with cosmetic results and fibrosis were analyzed using Fisher’s exact test or the Wilcoxon rank-sum test. p values were calculated using two-sided tests.
Results
Collected data were provided for analysis in November 2014. All patients were treated and followed up according to the protocol with no dropouts. The follow-up period ranged from 30 months to 54 months (median of 42 months). As early clinical results have been published elsewhere [9, 10], we mainly describe late toxicity and cosmetic outcomes here.
Disease control
Neither locoregional nor distant recurrences have been observed to date.
Late toxicities
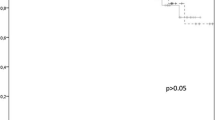
Hypopigmentation, hyperpigmentation, telangiectasia, fibrosis, fracture, pain, and soft tissue necrosis were observed as late toxicities. Ulceration, infection, and pneumonitis were not observed throughout the follow-up period. Toxicities of grade 2 or higher were observed for fibrosis, fracture, pain, and soft tissue necrosis. The cumulative rates of these toxicities at 42 months after treatment were 24.6, 2.2, 8.7, and 8.7%, respectively (Fig. 1). Fibrosis tended to increase in number over time, while other adverse events did not.
Cosmetic results
Cosmetic results are illustrated in Fig. 2. The rates of excellent or good results as assessed by the physician and the patient at the 12-month follow-up were 93 and 89%, respectively. They decreased to 76 and 74% at the 30-month follow-up, and over time to 70 and 67% at the 42-month follow-up.
Factors affecting cosmetic results
The relationships between cosmetic results and several factors are shown in Table 2. Only grade 2 or higher fibrosis was significantly correlated with unfavorable cosmetic results (p = 0.003). When fibrosis of grade 2 or higher was set as an endpoint, the correlated factors were large resected tissue weight (p = 0.005), large CTV volume (p = 0.004), large V100 (p = 0.020), small D100 (p = 0.004), and small maximum skin dose (p = 0.014). Vref, V1.5ref, V2.0ref, DNR, and conformity index had no impact (Table 3).
In additional subgroup analyses, the impact of the resected tissue weight was investigated separately in two subgroups of patients: patients with small bra cup sizes (A–B), and those with large bra cup sizes (C or larger). As a result, large resected tissue weight had a significant impact on grade 2 or higher fibrosis (p = 0.049) in patients with bra cup sizes of A–B. However, no significant impact was observed in patients with bra cup sizes of C or larger (p = 0.206).
Discussion
This is the first multi-institutional prospective study of APBI in Japan. Early clinical results, including detailed treatment methods, have been published elsewhere [9, 10]. No recurrences of the disease have been observed to date, which appears to indicate that the patient selection and treatment regimen were appropriate. However, when focusing on late toxicities and cosmetic outcomes, several issues emerge. We discuss those issues in this report.
Late toxicities of grade 2 or higher were observed for fibrosis, fracture, pain, and soft tissue necrosis. Reported incidences of these toxicities are summarized in Table 4 [7, 12,13,14,15,16,17,18]. The incidence of rib fracture after brachytherapy was described to be 4.5% in one report [19]. Our results are consistent with that value. However, in most previous reports, the incidence of grade 2 or higher fibrosis ranged from 10 to 20%, so the rate of 24.6% observed in our study was a little higher. Furthermore, because fibrosis tends to increase over time, the result may become worse with the length of follow-up. It is premature to discuss the late toxicity, but one possibility is that our treatment parameters were affected the higher rate of fibrosis. That is, the biologically effective dose and Vref in the current study seemed to be a little larger than those in previous studies (Table 4), which may have caused higher-grade fibrosis. On the other hand, Vref and DNR had no impact on grade 2 or higher fibrosis (Table 3), though these parameters may predict the harmful effects of a large volume of high-dose irradiation. This fact suggests that Vref and DNR, with the dose constraints we used, may not have been significantly related to the grade ≥2 fibrosis. Reassessment after a longer follow-up is necessary.
From another point of view, further consideration should be given to fibrosis. Fibrosis is defined by the CTCAE as follows: grade 1—visible only on close examination; grade 2—readily apparent but not disfiguring; grade 3—significant disfigurement. Items to be measured are not specified. Clinicians make a judgment after taking into consideration deformity, edema, contraction, firmness, change of color, and so on when evaluating fibrosis. These symptoms may be caused by the surgery as well as by irradiation. Thus, observers cannot strictly distinguish the primary cause. Although we can easily identify radiation-induced changes in WBI by studying a different part of the breast than the postoperative site, the affected area of APBI is the same as the postoperative site of the breast. This could make it quite difficult to make the appropriate judgment. We may have overjudged the fibrosis owing to confusion between radiation-induced and surgery-induced influences. In other words, when the fibrosis is defined as combined changes after surgery and irradiation, the incidence rate will be higher as a matter of course. A Japanese study reported a rate of 31.5% for “soft tissue fibrosis affecting cosmetic change” after conventional fractionated whole-breast irradiation [20]. Compared with that report, the rate of fibrosis in our series was not high.
Cosmetic results seemed to be unsatisfactory during the period of this interim analysis as compared to the cosmetic results reported in previous papers (reported rates of excellent or good cosmetic results: 78–99%) [16, 17, 21]. Our analysis indicated that grade 2 or higher fibrosis was strongly correlated with unfavorable cosmetic results. We then investigated factors that may have correlated with grade 2 or higher fibrosis (Table 3). Large resected tissue weight, large CTV volume, and large V100 were significantly correlated with grade 2 or higher fibrosis. These factors are all thought to have a strong correlation with the volume deficit caused by surgery. Small D100 was also correlated with grade 2 or higher fibrosis, which may be explained by an assumption that a large CTV is often hard to cover with the prescription dose.
We thus focused on the volume of resected tissue as a predictor of cosmetic outcomes. The median resected weight in this study was 73 g (23–234 g) (data not shown in the “Results” section). This weight was similar to that reported in a study in which the cosmetic outcomes were better than they are in our study [21]. Based on the hypothesis that the ratio of the volume of resected tissue to the whole breast may be more influential than the absolute resected volume, we performed further analyses. As expected, resected tissue weight had a significant impact on fibrosis (which probably represents deformity) only in patients with small bra cup sizes. We could not show a direct significant relationship between the relative resected volume and the cosmetic results. This will be elucidated through further investigation.
The current study was initially planned to verify the applicability of APBI for Japanese women. Our results confirmed that the technical aspects of APBI, which were established in Europe and North America, were reproducible in Japanese women. At the same time, our study demonstrated that cosmetic results were not satisfactory at this time. We believe that these results should not necessarily be interpreted to mean that APBI is unsuitable for Japanese women in terms of cosmetic outcomes. We found difficulties in assessing fibrosis separately from surgery-induced influences, especially in patients with small breasts. The sequelae of radiation therapy should be discussed separately from the adverse effects of surgery. One solution is to implement an objective measurement of fibrosis using a method such as elastography. A central review process might also help to achieve uniform judgments of cosmetic results. Furthermore, we should discuss cosmetic outcomes according to other factors such as the breast volume and resected tissue volume. The usefulness of preoperative volumetric analysis is widely recognized in the field of oncoplastic surgery. In fact, three-dimensional imaging techniques have recently been developed for this purpose [22]. These approaches may aid the adequate evaluation and assessment of cosmetic outcomes. That is, preoperative prediction of cosmetic results, which solely depend on surgery, may facilitate the separate evaluation of the cosmetic impact of radiation.
In conclusion, APBI in Japanese women has been demonstrated to achieve comparable outcomes to those seen in previous studies in Europe and North America, with the exception of cosmetic outcomes. Cosmetic outcomes were not satisfactory according to this interim analysis. Assessment of fibrosis is difficult and uncertain, especially in patients with small breasts. Improvements in the evaluation methods for fibrosis or cosmetic outcomes should be applied in future clinical trials. We need some more time to draw firm conclusions about late sequelae and cosmetic results. A longer follow-up is necessary to validate the applicability of APBI in Japanese women with breast cancer.
References
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41.
Early Breast Cancer Trialists’ Collaborative Group. Favourable and unfavourable effects on long-term survival of radiotherapy for early breast cancer: an overview of the randomised trials. Lancet. 2000;355:1757–70.
Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227–32.
Morrow M. Rational local therapy for breast cancer. N Engl J Med. 2002;347:1270–1.
Van Limbergen E, van den Bogaert W, van der Schueren E, Rijnders A. Tumor excision and radiotherapy as primary treatment of breast cancer. Analysis of patient and treatment parameters and local control. Radiother Oncol. 1987;8:1–9.
Clarke DH, Le MG, Sarrazin D, Lacombe MJ, Fontaine F, Travagli JP, et al. Analysis of local-regional relapses in patients with early breast cancers treated by excision and radiotherapy: experience of the Institut Gustave-Roussy. Int J Radiat Oncol Biol Phys. 1985;11:137–45.
Strnad V, Ott OJ, Hildebrandt G, Kauer-Dorner D, Knauerhase H, Major T, et al. 5-Year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in situ carcinoma of the female breast: a randomised, phase 3, non-inferiority trial. Lancet. 2016;387:229–38.
Polgár C, Limbergen EV, Pötter R, Kovács G, Polo A, Lyczek J, et al. Patient selection for accelerated partial-breast irradiation (APBI) after breast-conserving surgery: Recommendations of the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) breast cancer working group based on clinical evidence (2009). Radiother Oncol. 2010;94:264–73.
Otani Y, Nose T, Dokiya T, Saeki T, Kumazaki Y, Asahi S, et al. A Japanese prospective multi-institutional feasibility study on accelerated partial breast irradiation using interstitial brachytherapy: treatment planning and quality assurance. Radiation Oncology. 2015;10:126.
Nose T, Otani Y, Asahi S, Tsukiyama I, Dokiya T, Saeki T, et al. A Japanese prospective multi-institutional feasibility study on accelerated partial breast irradiation using interstitial brachytherapy: clinical results with a median follow-up of 26 months. Breast Cancer. 2015 (first online: 14 October 2015).
Harris JR, Levene MB, Svensson G, Hellman S. Analysis of cosmetic results following primary radiation therapy for stages I and II carcinoma of the breast. Int J Radiat Oncol Biol Phys. 1979;5:257–61.
Kuske RR, Winter K, Arthur DW, Bolton J, Rabinovitch R, White J, et al. Phase II trial of brachytherapy alone after lumpectomy for select breast cancer: toxicity analysis of RTOG 95-17. Int J Radiat Oncol Biol Phys. 2006;65:45–51.
Strnad V, Hildebrandt G, Pötter R, Hammer J, Hindemith M, Resch A, et al. Accelerated partial breast irradiation: 5-year results of the German–Austrian multicenter phase II trial using interstitial multicatheter brachytherapy alone after breast-conserving surgery. Int J Radiat Oncol Biol Phys. 2011;80:17–24.
Ott OJ, Schulz-Wendtland R, Uter W, Pfahlberg A, Beckmann MW, Sauer R, et al. Fat necrosis after conserving surgery and interstitial brachytherapy and/or external-beam irradiation in women with breast cancer. Strahlenther Onkol. 2005;181:638–44.
Lövey K, Fodor J, Major T, Szabo E, Orosz Z, Sulyok Z, et al. Fat necrosis after partial-breast irradiation with brachytherapy or electron irradiation versus standard whole-breast radiotherapy—4-year results of a randomized trial. Int J Radiat Oncol Biol Phys. 2007;69:724–31.
Polgár C, Major T, Fodor J, Sulyok Z, Somogyi A, Lövey K, et al. Accelerated partial-breast irradiation using high-dose-rate interstitial brachytherapy: 12-year update of a prospective clinical study. Radiother Oncol. 2010;94:274–9.
Chen PY, Vicini FA, Benitez P, Kestin LL, Wallace M, Mitchell C, et al. Long-term cosmetic results and toxicity after accelerated partial-breast irradiation: a method of radiation delivery by interstitial brachytherapy for the treatment of early-stage breast carcinoma. Cancer. 2006;106:991–9.
Perera F, Chisela F, Stitt L, Engel J, Venkatesan V. TLD skin dose measurements and acute and late effects after lumpectomy and high-dose-rate brachytherapy only for early breast cancer. Int J Radiat Oncol Biol Phys. 2005;62:1283–90.
Smith GL, Xu Y, Buchholz TA, Giordano SH, Jiang J, Shih YCT, et al. Association between treatment with brachytherapy vs whole-breast irradiation and subsequent mastectomy, complications, and survival among older women with invasive breast cancer. JAMA. 2012;307:1827–37.
Nozaki M, Kagami Y, Mitsumori M, Hiraoka S. A multicenter investigation of late adverse events in Japanese women treated with breast-conserving surgery plus conventional fractionated whole-breast radiation therapy. Jpn J Clin Oncol. 2012;42:522–7.
Wazer DE, Kaufman S, Cuttino L, Dipetrillo T, Arthur DW. Accelerated partial breast irradiation: an analysis of variables associated with late toxicity and long-term cosmetic outcome after high-dose-rate interstitial brachytherapy. Int J Radiat Oncol Biol Phys. 2006;64:489–95.
O’Connell RL, Stevens RJ, Harris PA, Rusby JE. Review of three-dimensional (3D) surface imaging for oncoplastic, reconstructive and aesthetic breast surgery. Breast. 2015;24:331–42.
Acknowledgements
This work was supported in part by Grants-in-Aid for Cancer Research from the Ministry of Health, Labor and Welfare of the Government of Japan (17-10 and 21-8-2) and by the Project for Development of Innovative Research on Cancer Therapeutics from the Japan Agency for Medical Research and Development.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
About this article
Cite this article
Yoden, E., Nose, T., Otani, Y. et al. Uncertainty of cosmetic evaluation after accelerated partial breast irradiation: interim analysis of a Japanese prospective multi-institutional feasibility study. Jpn J Radiol 35, 381–388 (2017). https://doi.org/10.1007/s11604-017-0640-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-017-0640-0