Abstract
Purpose
To evaluate the changes in splenic volume during hypovolemic shock and after recovery by use of multidetector computed tomography (MDCT).
Materials and methods
We investigated 22 cases who underwent MDCT during hypovolemic shock up to 3 h after presentation, compared the splenic volume with that after recovery, and evaluated the volume difference. We compared the volume ratio (recovery/shock) for two age groups: under 60 years (n = 10) and 60 years and over (n = 12). For cases (n = 10) undergoing CT examination twice after treatment, we compared the volume ratios by using the initial recovery CT and the second CT images.
Results
The average spleen volume in shock was 63 cm3; under normal conditions it was 132 cm3 (P < 0.001). The average volume ratio for groups under 60 years old was 2.34; for groups 60 years and over it was 2.05 (P = 0.051). The average volume ratio obtained by use of the initial post-recovery CT was 2.11; the ratio obtained by use of the second post-recovery CT was 2.16 (P = 0.386).
Conclusions
Our results revealed that splenic volume was reduced during hypovolemic shock and rapidly increased after recovery. Splenic contraction is an important CT finding in shock.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The spleen has many functions; these include storing iron and viable blood cells, although these two functions of the human spleen are not well developed [1]. The human spleen can contract in size, and splenic volume reduction is associated with elevation of sympathetic nervous system activity [1–9]. Although it is not known from computed tomography (CT) whether splenic volume is reduced among shock patients, a small number of papers have addressed splenic volume change in CT in general [2, 3]. We hypothesized that the volume reduction in shock is a result of sympathicotonia, and that the volume recovers rapidly after shock recovery. If this hypothesis is true, we can suspect shock in cases with a small spleen. The main purpose of this study was to evaluate the change in spleen volume during hypovolemic shock by using multidetector computed tomography (MDCT).
Materials and methods
Case selection
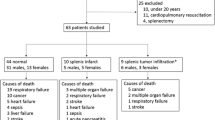
The institutional review board of our hospital approved this retrospective study, and the need for informed consent was waived. Our diagnostic criteria for shock included obtundation, heart rate >100 bpm, respiratory rate >22, hypotension (systolic blood pressure <90 mmHg) or a 30 mmHg fall from baseline blood pressure, and urine output <0.5 mL/kg/h [10]. We reviewed the electronic medical records of all patients who were clinically diagnosed with shock (n = 112) at our hospital during the 3-year period between January 2009 and December 2011. We selected 27 patients presenting with hypovolemic shock who matched our diagnostic criteria of shock up to 3 h before CT scan, who also underwent repeat CT after recovery. Patients who had splenic injury on CT (n = 5) were excluded. A final total of 22 patients (11 men and 11 women; age range, 16–88 years, mean, 62 years) were included in the study. Also, for cases (n = 10) undergoing CT examination twice after treatment, we compared the volume ratios using both the initial recovery CT and the second CT. We did not distinguish between cases examined with or without contrast. The number of cases imaged with and without contrast media was 21 and 1 in shock, 19 and 3 at initial post-recovery CT, and 8 and 2 at second post-recovery CT, respectively. Etiology of hypovolemic shock included 7 pelvic fractures, 3 liver injuries, 3 retroperitoneal hematomas, 2 hemothoraces, 2 femoral fractures, 1 facial bone fracture, 1 ruptured hepatocellular carcinoma, 1 multiple abdominal organ injury, 1 bleeding duodenal ulcer, and 1 case of multiple bone fractures. With regard to treatment for the hypovolemic shock, all patients were first treated with: infusion solutions then with blood transfusion only (n = 2); blood transfusion and transcatheter arterial embolization (TAE) (n = 11); blood transfusion and surgery (n = 4); blood transfusion, TAE, and surgery (n = 4); or blood transfusion and endoscopic hemostasis (n = 1). Shock recovery was defined as patients no longer meeting the shock criteria for 12 h after treatment.
CT technique
All CT examinations were performed with a 64-slice MDCT system (Somatom Definition or Somatom Sensation, Siemens Medical Solutions, Forchheim, Germany) during end-inspiration with or without contrast medium, with 2 mm-thick axial images reconstructed using an optimum clinical reconstruction field of view, 120 kVp and 140–260 mAs. Abdominal CT images, including unenhanced or contrast-enhanced images, were obtained for all cases. Post-contrast CT examinations were obtained between 90 and 120 s after administration of 100 mL non-ionic contrast medium (300 mg/mL) at a rate of 1–2 mL/s by use of a power injector.
Image evaluation and statistical analysis
We measured the volume of the spleen during shock and on the initial post-recovery CT for all 22 cases. One radiologist (TK, with 7 years of clinical experience in diagnostic radiology) measured and compared the splenic volumes. Volume measurement was performed by drawing the outline of the spleen manually in three dimensions by use of a workstation (Centricity AW Suite, GE Healthcare, Piscataway NJ, USA), which enabled manual adjustment of window level and window width. We compared the volume ratio (recovery/shock) for age groups under 60 years old (n = 10) and 60 years and over (n = 12). For cases (n = 10) undergoing CT examination twice after treatment we also compared the volume ratios using both the initial recovery CT (1–9 days after shock) and the second CT (7 days–2 years after shock). We also investigated the correlation between the volume ratio (recovery/shock) and vital signs including systolic blood pressure (sBP), diastolic blood pressure (dBP), and heart rate (HR). We used the SPSS (Statistics for Windows version 18.0; IBM, Chicago IL, USA) for statistical tests. The Wilcoxon signed-rank test was used for the two statistical tests targeting the same patients because results did not follow the normal distribution with the Shapiro–Wilk test. The Mann–Whitney U test was used to assess differences between splenic size in the two age groups. Spearman’s rank correlation test was used to investigate the correlation between the volume ratio (recovery/shock) and each vital sign (sBP, dBP, HR) because these also did not follow a normal distribution with the Shapiro–Wilk test.
Results
CT findings during hypovolemic shock and post-recovery are shown in Fig. 1. The average volume of the spleen was 63 cm3 (range 19–223 cm3) and 132 cm3 (range 23–401 cm3) in shock and post-recovery, respectively (P < 0.001) (Fig. 2). The average volume ratio (non-shock/shock) was 2.07 (range 1.13–3.12). The average volume ratio for patients under 60 years old was 2.34 (range 1.78–3.02); for patients 60 years and over it was 2.05 (range 1.13–2.98) (P = 0.051) (Fig. 3). The average volume ratio using initial post-recovery CT was 2.11 (range 1.13–2.98); the ratio using second post-recovery CT was 2.16 (range 1.34–2.95) (P = 0.386) (Fig. 4). There was no significant correlation between the volume ratio and sBP (r = 0.369, P = 0.091), the volume ratio and dBP (r = 0.208, P = 0.352), and the volume ratio and HR (r = 0.023, P = 0.918) (Fig. 5). No patients in our study did not recover.
Discussion
In this study, splenic volumes after recovery were significantly larger than those measured during shock. The volume ratio ranged from more than three to slightly greater than 1.0; however, the ratio was never less than 1.0. This indicates that during hypovolemic shock, the spleen has the ability to contract and the amount of contraction varies widely. The spleen contracted to one-third its normal size at most. We hypothesized that splenic volume would rapidly increase after recovery from shock, and then would remain stable. There was no significant difference between age groups, nor was there a significant correlation between the degree of contraction and each vital sign.
The size and weight of the spleen varies with age and sex. In the adult it is usually 12 cm long, 7 cm broad, and 3–4 cm wide [11]. The spleen is composed of a supporting connective tissue framework and a parenchyma made up of red and white pulp. The red pulp contains terminal branches of the central arteries, splenic sinuses, splenic cords separating the sinuses, and pulp veins, all supported by a meshwork of reticular cells and fibers.
The spleen has many functions including formation of antibodies, lymphocytes, and monocytes, filtration, phagocytosis and destruction of red blood cells, and storage of iron and viable blood cells. In general, the storage function is not well developed in the human spleen because it contains only 200–250 ml of blood on average [1].
The first reported case of splenic emptying occurred in 1852, when Henle electrically stimulated the splenic nerve of a decapitated human, both in situ and after removal. He observed that the spleen which was originally pale and wrinkled became darker and smoother after removal from the body. This, he suggested, showed the spleen had contracted [2]. Observations of human splenic volume reduction have been recorded more recently [3–7]. A comprehensive series of in-vitro studies found that stimulation of the postganglionic sympathetic nerves to the human spleen evoked reductions in spleen volume [2]. All research on splenic volume reduction has been associated with sympathetic nervous system activity [1]. In these studies, the volume changes of the spleen were demonstrated by use of ultrasound [5], magnetic resonance imaging [6], or nuclear medicine [1]. Other studies used spleens obtained by surgery [2] or autopsy [4].
Low attenuation values for the spleen in hypovolemic shock are related to severe hypoperfusion on CT [12]. Splenic arterial flow has no autoregulatory mechanism and is very sensitive to sympathetic stimulation, and thus vasoconstriction [12, 13]. However, splenic volume change associated with shock was observed in our study. The volume of the spleen decreases because blood in the spleen flows out in response to sympathetic stimulation in the shock state. Although a small number of papers addressed the splenic volume change on CT [2, 3], none has followed the course of the splenic volume after recovery. As far as we are aware, ours is the first report using MDCT and thin slice reconstruction to examine splenic volume change.
With regard to the clinical benefit of this study, first, we can suspect shock in cases with a small spleen. To diagnose a small spleen, it is most important and reliable to compare splenic volume on CT with previous CT images, if available. Splenic volume differs with age and sex, and there are also individual differences; therefore, without previous CT data, it is difficult to confirm small splenic volume. Second, we can avoid misdiagnosing splenomegaly in cases with a larger spleen than in previous CT images by recognizing that splenic volume can change.
This study has some limitations. First, our study involved only patients in hypovolemic shock. If our hypothesis is correct, the spleen may also contract in other shock states, for example cardiogenic or distributive shock. Other shock etiology also cause sympathicotonia, and further investigation is needed. Second, when the patients underwent their first CT, the shock may have improved to some extent as a result of emergency treatment. In general, during shock, emergency treatment takes precedence over CT imaging. Spleen volumes may have been increasing from a nadir if fluid resuscitation was initiated before CT imaging; this has been verified in animal studies [14]. Third, this study presented no pathological evidence, although pathology may not be absolutely necessary when following the radiological change. Finally, the timing of the examinations in shock and in recovery varied. This may be a reason for the range in volume measurements and no significant correlation between the degree of contraction and each vital sign.
In conclusion, our MDCT results revealed that splenic volume was reduced in hypovolemic shock and rapidly increased after recovery from shock. We believe that contraction of the spleen is an important CT finding in shock.
References
Stewart IB. Splenic contraction, catecholamine release, and blood volume redistribution during exercise in man. The University of British Columbia, Ph.D. thesis, Vancouver, 2002. Available from: http://circle.ubc.ca/handle/2429/13234. Accessed 12 Feb 2015.
Corradi F, Brusasco C, Garlaschi A, Santori G, Vezzani A, Moscatelli P, et al. Splenic doppler resistive index for early detection of occult hemorrhagic shock after polytrauma in adult patients. Shock. 2012;38:46–73.
Goodman R. Changes in splenic size after abdominal trauma. Radiology. 1990;176:629–32.
Ayers AB, Davies BN, Withrington PG. Responses of the isolated, perfused human spleen to sympathetic nerve stimulation, catecholamines and polypeptides. Br J Pharmacol. 1972;44:17–30.
Silagy C, Sage M, Wallage A. Patient-detected diurnal changes in spleen volume. Lancet. 1998;352:710.
Haffner HT, Graw M, Erdelkamp J. Spleen findings in drowning. Forensic Sci Int. 1994;66:95–104.
Fisher BM, Gillen G, Hepburn DA, Dargie HJ, Barnett EFB. Splenic responses to acute insulin-induced hypoglycaemia in humans. Clin Sci. 1990;78:469–74.
Kaufman MJ, Siegel AJ, Mendelson JH, Rose SL, Kukes J, Sholar MB, et al. Cocaine administration induces human splenic constriction and altered hematologic parameters. J Appl Physiol. 1998;85:1877–83.
Knecht H, Jost R, Gmür J, Burger J, Fehr J. Functional hyposplenia after allogeneic bone marrow transplantation is detected by epinephrine stimulation test and splenic ultrasonography. Eur J Haematol. 1988;41:382–7.
de Moya MA. Shock. Merck Manuals. 2013. Available from: https://www.merckmanuals.com/professional/critical-care-medicine/shock-and-fluid-resuscitation/shock. Accessed 26 June 2015.
Borley NR. Spleen. In: Standring S, editor. Gray’s Anatomy. Fortieth ed. Amsterdam: Elsevier; 2008. p. 1191–5.
Tarrant AM, Ryan MF, Hamilton PA, Benjaminov O. A pictorial review of hypovolaemic shock in adults. Br J Radiol. 2008;81:252–7.
Kanki A, Ito K, Tamada T, Higashi H, Sato T, Tanimoto D, et al. Dynamic contrast-enhanced CT of the abdomen to predict clinical prognosis in patients with hypovolemic shock. AJR. 2011;197:W980–4.
Guntheroth WG, Mullins GL. Liver and spleen as venous reservoirs. Am J Physiol Legacy Content. 1963;204:35–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This article does not contain any studies with human participants or animals performed by any of the authors.
About this article
Cite this article
Kiguchi, T., Higuchi, T., Takahashi, N. et al. CT measurement of splenic volume changes as a result of hypovolemic shock. Jpn J Radiol 33, 645–649 (2015). https://doi.org/10.1007/s11604-015-0470-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-015-0470-x