Abstract
We report the case of a 74-year-old man who developed type IA endoleak after endovascular thoracic aortic repair. The patient was admitted with expansion of the aneurysm after TEVAR, for additional therapy. Fluoroscopy and cone-beam computed tomography-guided direct transthoracic sac puncture and complete embolization of the endoleak channels with metal coils and glue were performed, and resulted in complete exclusion of the endoleak. One month after the coil embolization, the type IA endoleak was completely excluded, and the thoracic aneurysm had decreased in size.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Thoracic endovascular aortic repair (TEVAR) has become established as a useful alternative to open surgery for treatment of thoracic aortic aneurysm [1, 2]. However, late complications have been reported, in particular, endoleaks, which may contribute to sac enlargement or rupture [3–7]. In this paper we report a case in which we performed direct transthoracic puncture embolization of a type IA endoleak after TEVAR, guided by fluoroscopy and cone-beam computed tomography (CBCT).
Case report
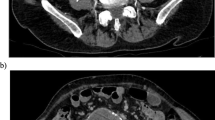
The patient was a 74-year-old man, who had undergone a TEVAR (TAG stentgraft; W.L. Gore and Associates, Flagstaff, AZ, USA) for a 5.5-cm diameter thoracic aortic aneurysm (TAA). Although the TEVAR was completed without any evidence of endoleak, the patient subsequently developed an endoleak and the thoracic aneurysm sac expanded, detected on follow-up CT (Fig. 1a–c), and additional treatment had to be considered.
The patient was placed in the prone position, and the procedure was performed under local anesthesia. A 23-G, 70-mm needle was inserted along the planned route under CBCT guidance as a marker and for local anesthesia. A 19-G coaxial needle (MCXS2015L; Sheen-man, Osaka, Japan) was inserted near the endoleak sac by use of the tandem technique [8], then a 20-G, 20-cm Chiba-type biopsy needle (MCN2008US; Sheen-man) was advanced through 19-G coaxial needle into the endoleak sac, and sacography was performed. The type IA endoleak channel was clearly visualized (Fig. 2a). Thereafter, the 19-G coaxial needle was advanced through the 20-G biopsy needle into the endoleak sac, and a 2.0-Fr microcatheter (Excelsior1018; Stryker, Kalamazoo, Michigan, USA) was advanced through the 19-G coaxial needle into the aortic arch via the endoleak channel, followed by embolization of the endoleak channel and the efferent bronchial artery (Fig. 2b, c) by use of interlocking metal coils (Interlock; Boston Scientific; Natick, MA, USA); thereafter 1.0 mL of a 50 % N-butyl 2-cyanoacrylate (NBCA) (Histacryl; B. Braun, Tuttlingen, Germany)–lipiodol (Lipiodol Ultrafluid, Laboratoire Guerbet, Aulnay-Sous-Bois, France) mixture was injected for the purpose of complete embolization of the orifice of the bronchial artery. After embolization, sacography was repeated; this confirmed the absence of the endoleak channel after the procedure. Intra-sac pressure measurement confirmed disappearance of the pulsatile wave form. CBCT was performed again after the coaxial needle was removed, and no pneumothorax or hematoma was identified. On follow-up CT obtained after 1 month, the type IA endoleak had completely disappeared, and the aneurysm had decreased 0.5 cm in size (Fig. 3a–c). The patient died 3 months after procedure because of pneumonia; there were no aneurysmal or procedure-related complications.
a Sacography showing the endoleak sac and channels continuous with the aortic arch. The left subclavian artery (small arrow) and common carotid artery (large arrow) are clearly visualized. b, c Sacography after embolization of the endoleak channel showing the bronchial artery continuous with the endoleak sac
Discussion
Endoleaks after TEVAR occur among 5–20 % of patients, similar to the incidence of endoleaks after endovascular aneurysm repair (EVAR) [3–6]. Endoeaks are diagnosed by contrast-enhanced computed tomography (CT); they may, however, be difficult to differentiate from type II endoleaks, and, often, reliable diagnosis can be made only by sacography during treatment of the endoleak [7]. It is possible to interrupt the treatment of endoleaks when using a transarterial approach; in the direct puncture approach, however, it is necessary to complete the treatment after puncture of the aorta, because aneurysm sac pressure is similar to systemic pressure, irrespective of type [9]. Type IA endoleaks after TEVAR or EVAR are usually treated by additional endovascular repair, for example cuff deployment or open repair, and several case reports of transarterial embolization of type IA endoleaks via the endoleak channels after EVAR have been published.
CT and CBCT-guided direct puncture embolization of type II endoleaks after TEVAR or EVAR using metal coils and/or NBCA–lipiodol have been described elsewhere. There are only six published reports of direct transthoracic endoleak embolization of type II endoleaks after TEVAR [10–15]; however, to the best of our knowledge, direct transthoracic puncture embolization for type IA major endoleak after TEVAR has not been reported previously. In our method, a metal needle was used, and it was possible to finely adjust the re-positioning of the needle securely, even if the needle position shifted during the procedure. However, it is necessary to be careful not to cause a microcatheter transection with the edge of the metal needle. In this regard, use of non-metal needle, for example Elaster needle (Hakko, Japan), is recommended.
We believe that complete exclusion of type IA endoleaks after TEVAR requires not only embolization of the proximal afferent endoleak channels but also of the efferent vessels, for example a bronchial artery and/or intercostal artery. From this perspective, addition of entire sac embolization by use of NBCA–lipiodol was considered; use of NBCA–lipiodol in the aortic arch area is, however, associated with a very high risk of migration of the NBCA into the aortic arch branches, and complete endoleak channel embolization by use of metal coils should be the objective. Although direct transthoracic puncture embolization might be a viable option for thoracic type IA endoleaks, especially under fluoroscopy and CBCT guidance, it is not without risks, many of which are entirely different from those associated with direct transthoracic embolization for type II endoleaks.
Conclusion
Fluoroscopy and CBCT-guided direct transthoracic puncture embolization is feasible for selected patients with type IA endoleaks developing after TEVAR. More experience with this technique and longer follow-up of such patients are needed, and further research is mandatory.
References
Conrad MF, Ergul EA, Patel VI, Paruchuri V, Kwolek CJ, Cambria RP. Management of diseases of the descending thoracic aorta in the endovascular era: a medicare population study. Ann Surg. 2010;252:603–10.
Orandi BJ, Dimick JB, Deeb GM, Patel HJ, Upchrch GR Jr. A population-based analysis of endovascular versus open thoracic aneurysm repair. J Vasc Surg. 2009;49:1112–6.
Stavropoulos SW, Carpenter JP. Postoperative imaging surveillance and endoleak management after endovascular repair of thoracic aortic aneurysms. J Vasc Surg. 2006;43:89A–93A.
Morales JP, Greenberg RK, Lu Q, Cury M, Hernandez AV, Mohabbat W, et al. Endoleaks following endovascular repair of thoracic aortic aneurysm: etiology and outcomes. J Endovasc Ther. 2008;15:631–8.
Parmer SS, Carpenter JP, Stavropoulos SW, Fairman RM, Pochettino A, Woo EY, et al. Endoleaks after endovascular repair of thoracic aortic aneurysms. J Vasc Surg. 2006;44:447–52.
Alsac JM, Khantalin I, Julia P, Achouh P, Farahmand P, Capdevila C, Isselmou KO, et al. The significance of endoleaks in thoracic endovascular aneurysm repair. Ann Vasc Surg. 2011;25:345–51.
Adams JD, Tracci MC, Sabri S, Cherry KJ, Angle JF, Matsumoto AH, et al. Real-world experience with type I endoleaks after endovascular repair of the thoracic aorta. Am Surg. 2010;76:599–605.
Desai S, Nemcek AA. Percutaneous biopsy. In: Mauro MA, Murphy KP, Thomson KR, et al., editors. Image-guided interventions. 1st ed. Philadelphia: Saunders Elsevier; 2008. p. 1339–44.
Baum RA, Carpenter JP, Cope C, Golden MA, Velazquez OC, Neschis DG, et al. Aneurysm sac pressure measurements after endovascular repair of abdominal aortic aneurysms. J Vasc Surg. 2001;33:32–41.
Stavropoulos SW, Tucker J, Carpenter JP. Thoracic endoleak embolization using a direct percutaneous puncture of the endoleak through lung parenchyma. J Vasc Interv Radiol. 2009;20:1248–51.
Riesenman PJ, Farber MA, Mauro MA, Selzman CH, Feins RH. Aortoesophageal fistula after thoracic endovascular aortic repair and transthoracic embolization. J Vasc Surg. 2007;46:789–91.
Katada Y, Kondo S, Takahashi S, Okita Y, Kagoshima A, Rokkaku K, et al. Direct percutaneous puncture embolization of type II endoleaks using coaxial technique. J Endovasc Ther. 2013;20:34–8.
Klein S, Picus D. Thoracic type II endoleak embolization using direct percutaneous puncture. Cardiovasc Intervent Radiol. 2012;35:1249–52.
Mussa FF, Maldonado TS, Schwartz CF. Percutaneous embolization of patient intercostal artery causing persistent type II endoleak and sac enlargement of thoracoabdominal aneurysm 2 years after hybrid repair. J Thorac Cardiovasc Surg. 2012;144:e102–6.
Kreusch AS, Samuels S, Benenati JF, Schernthaner M, Uthoff H. Direct percutaneous sac injection for treatment of a thoracic type II endoleak. J Vasc Interv Radiol. 2013;24:1071–3.
Conflict of interest
The authors declare that they have no conflict of interest. The authors have no commercial, proprietary, or financial interest in any products or companies described in this article.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Katada, Y., Kondo, S., Tsuboi, E. et al. Type IA endoleak embolization after TEVAR via direct transthoracic puncture. Jpn J Radiol 33, 169–172 (2015). https://doi.org/10.1007/s11604-015-0392-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-015-0392-7