Abstract
Purpose
Few finite element studies have investigated changes in cervical biomechanics with various prosthesis design parameters using hybrid surgery (HS), and none have investigated those combined different HS strategies. The aim of our study was to investigate the effect of ball-and-socket prosthesis geometry on the biomechanical performance of the cervical spine combined with two HS constructs.
Methods
Two HS strategies were conducted: (1) ACDF at C4–C5 and anterior cervical disc replacement (ACDR) at C5–C6 (ACDF/ACDR), and (2) ACDR/ACDF. Three different prostheses were used for each HS strategy: prosthesis with the core located at the center of the inferior endplate with a radius of 5 mm (BS-5) or 6 mm (BS-6), or with a 5 mm radius core located 1 mm posterior to the center of the inferior endplate (PBS-5). Flexion and extension motions were simulated under displacement control.
Results
The flexion motions in supra- and infra-adjacent levels increased in all cases. The corresponding extension motions increased with all prostheses in ACDR/ACDF group. The stiffness in flexion and extension increased with all HS models, except for the extension stiffness with ACDF/ACDR. The facet stresses between the index and infra-adjacent level in ACDR/ACDF were significantly greater than those in the intact model . The stresses on the BS-5 UHMWPE core were greater than the yield stress.
Conclusion
The core radii and position did not significantly affect the moments, ROM, and facet stress in extension. However, the moments and ROM in flexion were easily affected by the position. The results implied that the large core radii and posterior core position in ACDR designs may reduce the risk of subsidence and wear in the long term as they showed relative low stress . The ACDF/ACDR surgery at C4–C6 level may be an optimal treatment for avoiding accelerating the degeneration of adjacent segments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cervical discectomy and fusion (ACDF) procedures have been widely used for cervical diseases including arthritis, tumor, and trauma [1]. However, ACDF carries a potential risk of adjacent segment degeneration, which may be related to the increases in the motion and intradiscal pressure adjacent to the fused level [1,2,3,4]. In particular, the increased adjacent-level intradiscal pressure may increase the rates of early disc degeneration [5, 6]. Previous studies have reported that anterior cervical disc replacement (ACDR) is superior to spinal fusion in reproducing normal kinematics at the index level [7, 8] and has a better clinical effect in the short term [8]. The hybrid surgery (HS) of ACDF plus ACDR has emerged as an alternative treatment for multi-level cervical diseases [9, 10].
One-level ACDR does not eliminate index-level motion and avoids hypermobility and greater force at adjacent levels compared with ACDF. The stiffness of the cervical spine decreases after two-level ACDR and significantly increases after two-level fusion [11]. HS could provide a tradeoff in the stiffness and motion preservation; biomechanical studies have reported that HS is beneficial in maintaining the motion of operative levels [12, 13] and does not decrease the stiffness of cervical segments [11].
The cervical biomechanics after two-level HS are related to the chosen hybrid strategy and the prosthesis design parameters (DPs). Previous finite element (FE) studies have explored the effect of hybrid strategies (ACDR/ACDF vs. ACDF/ACDR) on the kinematic and mechanics of the cervical segments [14]. However, regarding the DPs of prostheses (such as the location of rotation center and height), most FE studies have focused on how the change in DP affected biomechanical performance after one-level ACDR [15,16,17]. As there are some discrepancies in terms of the biomechanical mechanisms in one-level replacement constructs and hybrid constructs, this suggests conclusions related to the optimization of DPs of artificial discs in one-level ACDR may not be applicable to HS. Thus, it is necessary to explore the relationships between the DPs and cervical biomechanics in the HS model. To our knowledge, no FE studies have investigated the effect of different geometry DPs combined with hybrid constructs on cervical biomechanics.
The aim of this study was to systematically explore the effect of varying geometry of a ball-and-socket prosthesis (prototype: Prodisc-C) using two hybrid strategies on the range of motion (ROM) and stresses of cervical segments.
Materials and methods
The model employed herein was developed and validated in our previous study [18]. In order to build an FE model, the computed tomography (CT) images of a healthy subject (male 170 cm, aged 35 year 65 kg) in terms of C3–C7 cervical segments were obtained with 1-mm intervals. The scanned object did not have any history of cervical disc diseases and abnormal physiological curvature in vertebral body. The ball-and-socket (BS) type artificial discs were designed into 3 different radii of curvature with their center of rotation (COR) located on the inferior endplate.
Construction of C3–C7 finite element model and instruments
CT images were imported into Mimics 10.0 (Materialise Inc., Leuven, Belgium) with a DICOM format to construct the geometric structure of the cervical spine and were then embedded into the FE model pre-processing software Hypermesh 13.0 (Altair Technologies, Inc., Fremont, CA, USA) to develop high-quality FE mesh. After all the meshing work was done, the C3–C7 model was imported into Abaqus 6.13 (Simulia Inc., Providence, RI, USA) to set boundary conditions and to solve.
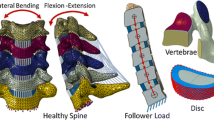
In the present model (Fig. 1), the vertebral bodies were composed of cancellous bone with solid elements and 0.4-mm-thick cortical bone, and endplates with shell elements [19]. The cervical disc was divided into three parts: ground substance, nucleus pulposus, and one layer of net-structure annulus fibrosus attached to the outmost layer of ground substance. Collagen fibers were assigned with an inclination range from \(15{^{\circ }}\) to \(45{^{\circ }}\) [20], and were set up to occupy 20% of the ground substance volume [21]. In addition, five groups of ligaments employed tension-only rod elements attached to the corresponding vertebral bodies, which were also inserted into vertebral bodies: anterior longitudinal ligament, posterior longitudinal ligament, capsular ligament, flaval ligament, and interspinous ligament. Two adjacent cartilages with a thickness of 0.5 mm were assigned with nonlinear surface-to-surface contact [22]. The numbers of nodes and elements in the whole FE model were 52,663 and 202,544 respectively, and the convergence was with 1% which guaranteed the accuracy of calculations related to the mesh itself.
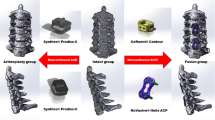
To compare the effect of varying core radii on ROM and stresses, BS models with two different sized cores located on the center of the inferior endplate (5 mm: BS-5; 6 mm: BS-6) were designed. A third BS model had a 5 mm core located 1 mm posterior to the center of the inferior endplate (PBS-5). The prostheses were 15 mm wide \(\times \) 12 mm long \(\times \) 6 mm high, and the plate was 12 mm wide \(\times \) 25 mm high [23]. The thickness of the two endplates (CoCrMo) and plate (Ti6Al4V) was 2 mm. The material properties and element types were assigned with corresponding components according to previous studies (Table 1) [19, 22].
Biomechanical testing and boundary conditions
According to the hybrid strategy, HS models were divided into two groups (A and B), each with the three aforementioned prostheses combined with the same plate inserted into the cervical spine (Fig. 2).
In group A, an ACDF was conducted at C4–C5 and the Prodisc-C was inserted at C5–C6 (ACDF/ACDR), under the following three conditions:
-
ACDF/ACDR with BS-5 prosthesis (A-BS-5)
-
ACDF/ACDR with BS-6 prosthesis (A-BS-6)
-
ACDF/ACDR with PBS-5 prosthesis (A-PBS-5)
In group B, the Prodisc-C was inserted at C4–C5 and an ACDF was conducted at C5–C6 (ACDR/ACDF), under the following three conditions:
-
ACDR/ACDF with BS-5 prosthesis (B-BS-5)
-
ACDR/ACDF with BS-6 prosthesis (B-BS-6)
-
ACDR/ACDF with P BS-5 prosthesis (B-PBS-5)
In the whole model, each cervical disc was tied between its adjacent endplates, and each two contiguous superior and inferior facets were set to sliding contact without friction [24]. The superior endplate and core of the prosthesis were defined as frictionless contact, and the bone-implant interface was applied with tied constraint [19]. At the ACDR level in each HS model, the anterior longitudinal ligament, nucleus pulposus, and about 60% of annulus were excised and the prosthesis was inserted at the corresponding locations recommended by an experienced surgeon.
A moment of 1 Nm combined with a 50 N follower load [25] was applied at the center of the superior endplate in the C3 vertebra to simulate flexion–extension with the inferior endplate in C7 fixed. The follower load was employed a set of connector elements to simulate and pass through the flexion–extension center of rotation [19]. The corresponding overall movement angles of flexion and extension in the intact model were then both, respectively, imposed on each HS model (Fig. 3).
Results
Model validation
The ROM of the normal model subjected to 1 Nm is shown in Fig. 5, which is consistent with existing experimental results [26, 27]. The ROM of flexion and extension was \(18.62{^{\circ }}\) and \(15.63{^{\circ }}\), respectively, under 1 Nm and 50 N follower load. These two rotation displacements were, respectively, applied at the center of the endplate of the C3 segment in all FE models.
Predicted moment
Figure 4 depicts the displacement–moment curves in flexion–extension. In flexion, the moments required to reach the same displacement increased with all HS models in group A and group B when compared with that required in the intact model. In extension, the aforementioned moments increased by approximately 12% with all ACDR/ACDF models in group B, whereas they were decreased by approximately 20% with the ACDF/ACDR models in group A. In addition, with the same prosthesis design, the flexion moment in each HS model in group A was greater than it in group B by approximately 17%.
Range of motion
Figure 5 depicts the ROM of segmental angulation during flexion. As expected, the ROM of the fusion level in both groups was nearly zero. The flexion motions at the implanted level and adjacent levels (C3–C4 and C6–C7) increased in all cases when compared with the intact model. The maximum increase in flexion motion at the adjacent levels in the A-BS-5 and A-BS-6 models was 51%, whereas it was 38% in the A-PBS-5 model. The corresponding maximum increase, however, in the B-BS-5 and B-BS-6 model was 36%, whereas it was 23% in the B-PBS-5 model.
Figure 6 depicts the ROM of segmental angulation in extension. Compared with the intact model, the extension motions at ACDR levels (C5–C6) increased in all cases. The extension ROM of the adjacent levels decreased in all hybrid models in group A, whereas it increased in group B. There was no significant difference in terms of extension motion among three models with the same hybrid strategy. Compared with the intact value of the extension ROM, the maximum decrease in group A was 16% and the maximum increase in group B was 10%.
Facet joint force and stresses
Figure 7 depicts the maximum contact force and facet stress on cartilage between the adjacent and operative levels in extension. There were four cartilages involved: inferior cartilage of (ICO) C3 segment, superior cartilage of (SCO) C4 segment, ICO-C6, and SCO-C7. Compared with the intact model, the contact force at cartilages between the adjacent and index level in group A decreased, whereas they increased in group B. The maximum facet stress was 1.77 MPa at the SCO-C7 in the ACDR/ACDF group. There was no significant change in facet stress among all hybrid models with the same hybrid strategy. Compared with those in the intact model, the facet stress in group A decreased, with the maximum decrease of 24% being observed at the ICO-C6. The facet stress in group B at the ICO-C6 and SCO-C7 was obviously greater than those in the intact model, with the maximum increase 41% at the ICO-C6.
Stresses on artificial core
The stress distribution on the artificial cores in flexion is shown in Fig. 8. The maximum stresses with the A-BS-5, A-BS-6 and A-PBS-5 were 39.05, 16.62 and 22.32 MPa, respectively, whereas with the B-BS-5, B-BS-6 and B-PBS-5 they were 39.29, 19.88 and 24.29 MPa, respectively.
Discussion
HS as an alternative approach for treating multi-level cervical degenerative disc diseases is still controversial. However, clinical follow-up studies have reported that HS for the cervical spine has feasibility and recovery comparable with both ACDR and ACDF [9, 10]. There have also been several in vitro biomechanical analysis studies on the ROM at cervical levels in ACDF and ACDR [28,29,30,31]. One cadaveric study reported that hybrid operations (ACDF at C5–C6 and Prodisc-C inserted at C6–C7) did not change the ROM of the whole C4–T1 segments, whereas two-level ACDF decreased ROM and two-level ACDR increased ROM compared with the intact model [28].
Theoretically, in two-level cervical disease treatment, the clinical effects are related to both the hybrid strategy and the DPs of the prosthesis. Thus, exploring how these various combinations affect cervical biomechanics after HS is helpful for clinical practice. Regarding the hybrid strategy, initial in-vitro biomechanical studies [28, 30, 32] and FE studies [14] have investigated the kinematic responses to different hybrid methods through varying levels of fusion and replacement. Regarding the DPs of the artificial disc, most FE studies only used one-level ACDR to investigate the influence of various DPs on cervical spine biomechanics [15,16,17, 19, 25]. As the mechanism of the hybrid model is different from one-level ACDR, conclusions related to the optimization of design variations of prostheses based on one-level ACDR may not be applicable to the hybrid model. To our knowledge, no FE studies have explored the effect of geometry variation of the ball-and-socket prosthesis on cervical biomechanics based on HS, and none have investigated those combining hybrid strategies.
In the present FE study, we employed three ball-and-socket designs (prototype: Prodisc-C) with varying positions of the geometry center and the size of radius of the artificial core, and constructed two hybrid strategies (ACDF/ACDR vs. ACDR/ACDF) to systematically explore how they affect the cervical biomechanics. Our results indicated that the DPs of prostheses did not significantly affect the extension motions. The effect of the location of rotation center of the prosthesis on flexion motions, however, is more sensitive than the artificial core radii. The flexion ROM of the adjacent levels with PBS-5 was relative close to that in the intact model in both groups. In our study, the flexion and extension motions showed a significant difference between the ACDR/ACDF and ACDF/ACDR groups by using the same prosthesis. Each ACDF/ACDR model decreased the extension motion of the adjacent levels compared with the intact value, whereas the ACDR/ACDF model increased the aforementioned motions. The increase in ROM at adjacent levels with the ACDR/ACDF construct may accelerate the adjacent-segment degeneration in the long term. Thus, the hybrid strategy for treating 2-level disc degeneration should be considered in a clinical environment as it has a significant effect on the kinematics distribution of the cervical segments.
As for the stiffness of the cervical spine, the models with the same hybrid construct, regardless of the prosthesis DPs, demonstrated a similar performance in extension. However, the predicted moment with the PBS-5 was relative close to the intact value in flexion. With the same design, a change in the hybrid strategy has a greater influence on the extension stiffness than the flexion stiffness.
Facet stresses following ACDF/ACDR in extension between the index and adjacent level were less than the intact facet stress values (Fig. 7). However, in the ACDR/ACDF group, these facet stresses were greater than the corresponding intact values at the ICO-C6 and SCO-C7, and the maximal increase was approximately 41% at the ICO-C6. Similarly, a previous FE study reported that the facet loads at adjacent levels using the ACDR/ACDF construct were greater than using ACDF/ACDR [14]. Also, the ACDR/ACDF resulted in greater contact force at adjacent levels than that of the intact model, which may accelerate degeneration of adjacent segments. The facet stresses in flexion at the aforementioned cartilages were almost zero. In both hybrid strategies, the change in geometry parameters of prostheses did not significantly change the extension contact force and facet stresses. In addition, in both hybrid strategies, the large artificial core radii and the posterior position of the artificial core showed a relative low core stress. In the present investigation, the maximum stress on the core of the BS-5 design in both groups was above the tensile strength (28 MPa) of the UHMWPE [25], which may affect the long-term follow-up of hybrid surgery.
Although a FE model may be a useful tool to predict spinal treatment efficiency [33], there are limitations to this study that must be considered. A limitation of the present study is that various factors, such as the position of the implant, the frictionless contact between the artificial core and endplate, may affect the results. The prediction of the facet contact force and facet stress based on an appropriately validated model could provide comparative results to guide clinical surgery. However, similar with most previous FE studies [19, 20, 25], the lack of validation for the contact force and facet stress is another limitation, which needs to be further studied. The prosthesis (prototype: Prodisc-C) inserted at the replacement level is widely accepted clinically, but has a fixed core. Various types of prostheses with different design concepts are commercially available, such as the Mobi-C, PCM and Bryan. Further study should analyze the relationships between the DPs of those prostheses combined with a hybrid construct and cervical mechanical properties. In addition, the predicted results were attained under the hybrid constructs with index levels of C4–C5 and C5–C6. A surgical procedure involving another hybrid intervention, such as choosing C5–C6 and C6–C7 as index levels [31], should be considered in future study. The graft bone and plate/screw were employed to simulate completely fusion [23] and, to some extent, may not fully represent the ACDF operation. However, the motion at the ACDF level was almost completely limited, which indicated that the influence of ACDF types in the present study could be neglected. The present study analyzed the motions in flexion and extension, as they are the main movements of the cervical spine in daily life [19]; investigation of the corresponding cervical biomechanical performance in lateral bending and axial rotation is planned in a subsequent study.
In conclusion, the ACDR design did not affect the extension ROM and facet stress in one hybrid strategy. The flexion ROM and stiffness were affected more sensitively by the location of the core rather than the radius of the core. A large core radius and relative posterior position of the core, however, exhibited a low stress. Even using the same ACDR design, different HS strategies had various effects on cervical biomechanics of the adjacent levels. The ACDR/ACDF models resulted in a significant increase in the facet stress at the index and inferior adjacent levels. Prosthesis selection should consider both the hybrid strategy and the DPs of various artificial discs.
References
Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y (2010) Adjacent segment disease and degeneration after anterior cervical decompression and fusion. Neurosurg Q 20:15–22. doi:10.1097/WNQ.0b013e3181ce0d13
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? The spine J 4:190S–194S. doi:10.1016/j.spinee.2004.07.007
Park DK, Lin EL, Phillips FM (2011) Index and adjacent level kinematics after cervical disc replacement and anterior fusion in vivo quantitative radiographic analysis. Spine 36:721–730. doi:10.1097/BRS.0b013e3181df10fc
McDonald CP, Chang V, McDonald M, Ramo N, Bey MJ, Bartol S (2014) Three-dimensional motion analysis of the cervical spine for comparison of anterior cervical decompression and fusion versus artificial disc replacement in 17 patients. J Neurosurg Spine 20:245–255. doi:10.3171/2013.11.SPINE13392
Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, An HS (2002) Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 27:2431–2434. doi:10.1097/01.BRS.0000031261.66972.B1
Dmitriev AE, Cunningham BW, Hu NB, Sell G, Vigna F, McAfee PC (2005) Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty — an in vitro human cadaveric model. Spine 30:1165–1172. doi:10.1097/01.brs.0000162441.23824.95
Rabin D, Pickett GE, Bisnaire L, Duggal N (2007) The kinematics of anterior cervical discectomy and fusion versus artificial cervical disc: a pilot study. Neurosurgery 61S:100–104. doi:10.1227/01.NEU.0000279997.11201.B4
Sasso RC, Smucker JD, Hacker RJ, Heller JG (2007) Artificial disc versus fusion a prospective, randomized study with 2-year follow-up on 99 patients. Spine 32:2933–2940
Shi J, Lin B, Xue C, Zhang H, Chen Z, Zhao Z (2015) Clinical and radiological outcomes following hybrid surgery in the treatment of multi-level cervical spondylosis: over a 2-year follow-up. J Orthop Surg Res 10(1):185. doi:10.1186/s13018-015-0330-5
Grasso G (2015) Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J 247:S842–S848. doi:10.1007/s00586-015-4281-7
Gandhi AA, Kode S, DeVries NA, Grosland NM, Smucker JD, Fredericks DC (2015) Biomechanical analysis of cervical disc replacement and fusion using single level, two level, and hybrid constructs. Spine 40:1578–1585. doi:10.1097/BRS.0000000000001044
Liu B, Zeng Z, Van Hoof T, Kalala JP, Liu Z, Wu B (2015) Comparison of hybrid constructs with 2-level artificial disc replacement and 2-level anterior cervical discectomy and fusion for surgical reconstruction of the cervical spine: a kinematic study in whole cadavers. Med Sci Monit 21:1031–1037
Jia Z, Mo Z, Ding F, He Q, Fan Y, Ruan D (2014) Hybrid surgery for multilevel cervical degenerative disc diseases: a systematic review of biomechanical and clinical evidence. Eur Spine J 23:1619–1632. doi:10.1007/s00586-014-3389-5
Chung T, Hueng D, Lin S (2015) Hybrid strategy of two-level cervical artificial disc and intervertebral cage biomechanical effects on tissues and implants. Medicine doi:10.1097/MD.0000000000002048
Rousseau M, Bonnet X, Skalli W (2008) Influence of the geometry of a ball-and-socket intervertebral prosthesis at the cervical spine–a finite element study. Spine 33:E10–E14
Faizan A, Goel VK, Garfin SR, Bono CM, Serhan H, Biyani A, Elgafy H, Krishna M, Friesem T (2012) Do design variations in the artificial disc influence cervical spine biomechanics? A finite element investigation. Eur Spine J 21(Suppl 5):S653–S662. doi:10.1007/s00586-009-1211-6
Womack W, Leahy PD, Patel VV, Puttlitz CM (2011) Finite element modeling of kinematic and load transmission alterations due to cervical intervertebral disc replacement. Spine 36:E1126–E1133. doi:10.1097/BRS.0b013e31820e3dd1
Li Y, Fogel GR, Liao Z, Tyagi R, Zhang G, Liu W (2017) Biomechanical analysis of two-level cervical disc replacement with a stand-alone U-shaped disc implant. Spine. doi:10.1097/BRS.0000000000002128
Mo Z, Zhao Y, Du C, Sun Y, Zhang M, Fan Y (2015) Does location of rotation center in artificial disc affect cervical biomechanics? Spine 40:E469–E475
Mo Z, Li Q, Jia Z, Yang J, Wong DW, Fan Y (2016) Biomechanical consideration of prosthesis selection in hybrid surgery for bi-level cervical disc degenerative diseases. Eur Spine J 26:1181–1190. doi:10.1007/s00586-016-4777-9
Kumaresan S, Yoganandan N, Pintar FA, Maimam DJ (1999) Finite element modeling of the cervical spine: role of intervertebral disc under axial and eccentric loads. Med Eng Phys 21(10):689–700. doi:10.1016/S1350-4533(00)00002-3
Ganbat D, Kim YH, Kim K, Jin YJ, Park WM (2016) Effect of mechanical loading on heterotopic ossification in cervical total disc replacement: a three-dimensional finite element analysis. Biomech Model Mechanobiol 15:1191–1199. doi:10.1007/s10237-015-0752-3
Mo ZJ, Bin Zhao Y, Wang LZ, Sun Y, Zhang M, Fan YB (2014) Biomechanical effects of cervical arthroplasty with U-shaped disc implant on segmental range of motion and loading of surrounding soft tissue. Eur Spine J 23:613–621. doi:10.1007/s00586-013-3070-4
Panzer MB, Cronin DS (2009) C4–C5 segment finite element model development, validation, and load-sharing investigation. J Biomech 42:480–490. doi:10.1016/j.jbiomech.2008.11.036
Lee S, Im Y, Kim K, Kim Y, Park W, Kim K (2011) Comparison of cervical spine biomechanics after fixed-and mobile-core artificial disc replacement: a finite element analysis. Spine 36:700–708. doi:10.1097/BRS.0b013e3181f5cb87
Panjabi MM, Crisco JJ, Vasavada A, Oda T, Cholewicki J, Nibu K, Shin E (2001) Mechanical properties of the human cervical spine as shown by three-dimensional load-displacement curves. Spine 26:2692–2700. doi:10.1097/00007632-200112150-00012
Wheeldon JA, Stemper BD, Yoganandan N, Pintar FA (2008) Validation of a finite element model of the young normal lower cervical spine. Ann Biomed Eng 36:1458–1469. doi:10.1007/s10439-008-9534-8
Cho BY, Lim J, Sim HB, Park J (2010) Biomechanical analysis of the range of motion after placement of a two-level cervical pro disc-C versus hybrid construct. Spine 35:1769–1776. doi:10.1097/BRS.0b013e3181c225fa
Barrey C, Campana S, Persohn S, Perrin G, Skalli W (2012) Cervical disc prosthesis versus arthrodesis using one-level, hybrid and two-level constructs: an in vitro investigation. Eur Spine J 21:432–442. doi:10.1007/s00586-011-1974-4
Park J, Shin JJ, Lim J (2014) Biornechanical analysis of disc pressure and facet contact force after simulated two-level cervical surgeries (fusion and arthroplasty) and hybrid surgery. World Neurosurg. doi:10.1016/j.wneu.2014.06.013
Lee MJ, Dumonski M, Phillips FM, Voronov LI, Renner SM, Carandang G, Havey RM, Patwardhan AG (2011) Disc replacement adjacent to cervical fusion a biomechanical comparison of hybrid construct versus two-level fusion. Spine 36:1932–1939. doi:10.1097/BRS.0b013e3181fc1aff
Cunningham BW, Hu N, Zorn CM, McAfee PC (2010) Biomechanical comparison of single- and two-level cervical arthroplasty versus arthrodesis: effect on adjacent-level spinal kinematics. Spine J 10:341–349. doi:10.1016/j.spinee.2010.01.006
Pan L, Yang X, Gu L, Lu W, Fang M (2011) Validation and prediction of traditional Chinese physical operation on spinal disease using multiple deformation models. Int J Comput Assist Radiol 6:201–208. doi:10.1007/s11548-010-0500-1
Acknowledgements
This work was supported by the Industry Public Technology Service Platform Capital Projects of Shenzhen [Grant Number SMJKPT20140417010001] and the Science and Technology Plan Basic Research Project of Shenzhen [Grant Number JCYJ20151030160526024]. The participant was explained on the research purpose and signed the consent form.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
This article does not contain patient data.
Rights and permissions
About this article
Cite this article
Li, Y., Fogel, G.R., Liao, Z. et al. Finite element model predicts the biomechanical performance of cervical disc replacement and fusion hybrid surgery with various geometry of ball-and-socket artificial disc. Int J CARS 12, 1399–1409 (2017). https://doi.org/10.1007/s11548-017-1616-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-017-1616-3