Abstract
Purpose
To perform a survey among all members of the Italian Society of Medical and Interventional Radiology (SIRM) to assess how whole-body MRI (WB-MRI) is performed in oncologic patients in Italy.
Methods
On March 2019, we administered an online poll to all SIRM members about their use of WB-MRI in 2018 asking 15 questions regarding oncologic indications, imaging protocol, use of contrast media, experience in WB-MRI, duration of scan time and reporting time.
Results
Forty-eight members participated to the survey. WB-MRIs/total MRIs ratio was 1%. Lymphoma was the most common indication (17/48, 35%), followed by myeloma and prostate cancer, with these three tumors representing the most common indication in 39/48 of cases (81%). WB-MRI acquisition time and reporting time were 46–60 min in 22/48 centers (46%) and 20–30 min in 19/48 (40%), respectively. WB-MRIs were mostly performed in 1.5T scanners (43/48, 90%), with surface coils (22/48, 46%) being preferred to Q-body (15/48, 31%) and integrated coils (11/48, 23%). Contrast media were injected in 22/48 of the centers (46%), mainly used for breast cancer (13/22, 59%). DWI was the most used sequence (45/48, 94%), mostly with b800 (27/48, 56%), b0 (24/48, 50%) and b1000 (20/48, 42%) values. In about half of cases, radiologists started evaluating WB-MRI non-contrast morphologic sequences, then checking DWI and post-contrast images.
Conclusion
WB-MRI was mainly performed at 1.5T unit, with lymphoma, myeloma and prostate cancer having been the most common indications. The extreme variability in the choice of imaging protocols and use of contrast agents demonstrates the need of a standardization of WB-MRI application in clinical practice.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the last years, concerns have been raised on the association of radiation exposure due to imaging examinations—mainly related to computed tomography (CT) and positron emission tomography (PET)/CT—with the increased secondary cancer risk in oncologic patients [1, 2]. This has led to the increased interest for the use of whole-body magnetic resonance imaging (WB-MRI) as a radiation-free alternative to currently used imaging modalities [3, 4]. The advancements in MRI technology have allowed a widespread introduction of WB-MRI in clinical practice, especially to evaluate patients with cancer [5, 6]. Indeed, this technique provides images of the entire body as other whole-body imaging modalities but with the strengths of MRI, including its high contrast resolution and the possibility to take advantage of “functional” information deriving from diffusion-weighted imaging (DWI) [7, 8]. Several papers have been published reporting the reliability, diagnostic accuracy and potential applications of WB-MRI in several clinical settings [9, 10]. Nevertheless, different imaging protocols have been proposed and few guidelines have been developed, mostly for patients with myeloma and prostate cancer [11, 12]. Indeed, WB-MRI is already recommended by the International Myeloma Working Group to stage and monitor patients with myeloma [11]. Thus, the actual role of WB-MRI in diagnostic work-up of most cancers is still unclear. Furthermore, to the best of our knowledge, no papers have been published on the current clinical application of WB-MRI.
Hence, the purpose of this study was to perform an online survey among all members of the Italian Society of Medical and Interventional Radiology (SIRM) to understand how WB-MRI is performed in daily clinical practice in Italy.
Materials and methods
Institutional review board approval was not needed because this study did not involve patients. This survey was approved by the SIRM on March 26, 2019. We administered an online survey to all SIRM members about the use of WB-MRI in oncologic patients in their institutions asking 15 questions, including 12 closed and 3 open questions. We included an additional question (16th) asking the participant to provide his/her name in order to be acknowledged in the final paper. An online questionnaire was built up using the online tool Google Documents (Mountain View, CA) [13], as already done in previous surveys [14, 15]. The survey was aimed to collect data about the number of MRI and WB-MRI scans performed in 2018, oncologic indications of WB-MRI, imaging protocol, use of contrast media, experience in WB-MRI imaging, duration of WB-MRI scan time and reporting time.
On March 27, 2019, an email was sent to all SIRM members who were invited to take part in this project by answering to the online poll. All participants were invited to retrieve the total number of WB-MRI scans performed at their institution in 2018 and were reassured that only 5 min were required to complete the online poll, the questionnaire was anonymous, and data would have been managed in aggregated form. Each member could answer only once. They were also asked to provide their name and email address, which were not associated with the data, in order to acknowledge them in the article. As a reminder, one more email was sent to all SIRM members 3 weeks later. The link to answer to the online questionnaire remained available for 32 days up to April 28, 2019.
Once received, the database was analyzed. Data were expressed as median and 25th–75th percentiles. Proportions were calculated and expressed as percentages.
Results
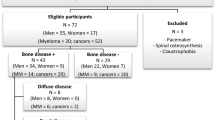
A total of 48 SIRM members from 14 Italian regions (Table 1) participated to the survey providing answers to all questions included in the online poll.
We used #1 and #2 answers to calculate WB-MRIs/total MRIs ratio resulting in a median of 1% (interquartile range 1–3: 0–5%). Lymphoma was the most common indication for WB-MRI in 17/48 centers (35%), followed by myeloma and prostate cancer, with these three tumors representing the most frequent indications in 39/48 of cases (81%) (Fig. 1). WB-MRI was performed from less than 2 years in 18/48 (37%) of centers, whereas it has been introduced from more than 5 years in 13/48 (27%). The main answers to question #5 (WB-MRI acquisition time) and #11 (WB-MRI reporting time) were 46–60 min (22/48, 46%) and 20–30 min (19/48, 40%), respectively (Figs. 2 and 3). WB-MRI examinations were mostly performed in 1.5T scanners (43/48, 90%), with surface coils (22/48, 46%) being preferred to Q-body (15/48, 31%) and integrated coils (11/48, 23%). Gadolinium-based contrast agents were injected during WB-MRI in almost half of centers (22/48, 46%) (Fig. 4), being mainly used for breast cancer (13/22, 59%). DWI was the most used sequence for WB-MRI protocol (45/48, 94%), mostly with b800 (27/48, 56%), b0 (24/48, 50%) and b1000 (20/48, 42%) values. After checking #10 answers, it resulted that 2 b values were used in 22/48 (46%) of centers, 1 in 12/48 (25%), 3 in 10/48 (21%) and 4 in 4/48 (8%). Regarding question #12, in about half of cases, radiologists started evaluating non-contrast morphologic sequences, then checking DWI and post-contrast images. Regarding the range of experience in MRI of radiologists reporting WB-MRI (question #13), the most frequent answer was 0–1 year (18/48, 37%).
Table 2 summarizes the list of questions of the online poll including all answers provided by SIRM members who participated to the survey.
Discussion
To date, no data have been published regarding the real diffusion and application of WB-MRI in daily clinical practice. According to the results of this survey, it seems that there is still no a widespread diffusion of WB-MRI. Indeed, WB-MRI examinations are 1% of the total number of MRI scans performed in Italian institutions where WB-MRI is used for oncological purposes. Then, no answers have been received from one-third of Italian regions, although a balanced geographical distribution has been observed throughout the whole country. Further, as shown by #4 answers, more than one-third (37%) of institutions use WB-MRI in clinical practice from less than one year, making this imaging modality a relatively novel tool for diagnostic work-up of oncologic patients.
Regarding question #3, the most common indication for WB-MRI was lymphoma, followed by myeloma and prostate cancer. This is indirectly demonstrated by the huge amount of papers published on these tumors. On the one hand, several studies have proven the accuracy and potential clinical application of WB-MRI for lymphoma staging [16,17,18], response assessment after treatment [19,20,21] and follow-up [22,23,24,25]. This is especially due to the robust functional evaluation of lymph nodes through DWI [26] and the high contrast resolution of WB-MRI to evaluate bone marrow [6, 27,28,29,30]. Nevertheless, the place of WB-MRI in diagnostic imaging pathway of patients with lymphoma is still unclear since no guidelines have been established in this setting. On the other hand, the role of WB-MRI is much better defined for diagnostic work-up of patients with myeloma and prostate cancer. The International Myeloma Working Group and the British Society for Haematology recommend to stage all forms of myeloma and solitary bone plasmacytoma with WB-MRI [11, 31, 32]. Regarding prostate cancer, WB-MRI is considered the first choice imaging modality to monitor the response of bone metastases [33]. Further, recommendations about acquisition, interpretation and reporting of WB-MRI performed in patients with prostate cancer have already been promoted [12].
Regarding question #5, in 41/48 centers (85%), WB-MRI scan time has resulted lower than one hour, that can be considered feasible for most patients. Clearly, this finding depends on MRI Unit and imaging protocol applied. In this respect, regarding question #6, most centers used to perform WB-MRI at 1.5T MRI Unit, which is probably related to the wider diffusion of these scanners in Italy in comparison with 3T. Of note, previous studies have shown similar diagnostic performance of 1.5 and 3T scanners, with the latter allowing for a decreased scan time [34,35,36,37]. Conversely, a wide variability has been observed in the choice of MRI coils (question #7), that is another feature highly dependent on MRI technology, since, for instance, some scanners do not enable to use integrated coils.
The question #8 highlights another crucial point that concerns the use of gadolinium-based contrast agents in WB-MRI. It is well-known that post-contrast images increase the accuracy of the examination in case of locations of disease in the central nervous system and focal lesions in the hypochondriac organs [5, 38, 39]. This justifies the higher tendency to inject contrast media in patients with breast cancer (59%), who are at higher risk of these types of metastatic locations. Furthermore, over the last years, the greater attention to this point is probably also due to the increasing awareness of gadolinium accumulation in human tissues, although any clinical impact has not been demonstrated yet [40, 41].
Regarding questions #9 and #10, we have received variable answers about imaging protocol. DWI is the most commonly used sequence, and its robustness and feasibility for whole-body imaging have been proven by several papers, since when in 2004 Takahara introduced WB-DWI with free breathing acquisition and homogeneous fat saturation ensured by STIR suppression [42]. Most centers used only two b values, which are considered sufficient by several authors, with b800 (27/48, 56%) and b1000 (20/48, 42%) as the highest b values. The slight preference of b800 as highest b value can be justified by the attitude and predilection of the single radiologist and by the will to avoid to lose the background signal with too high b value DWI images [43]. Gradient-echo Dixon is increasingly being used for bone marrow imaging, due to its homogeneous water/fat suppression [44], although only 14/28 centers (19%) included this sequence in their WB-MRI protocol, which can be explained by a still low diffusion of the sequence itself. As shown by the answers to question #12, non-contrast morphologic (T1- and T2-weighed, Dixon) and DWI sequences are evaluated at first by 92% of centers for WB-MRI interpretation, with post-contrast images just checked later. The minor role of post-contrast images additionally validates the advantages of WB-MRI that, besides being a radiation-free imaging modality, allows to avoid contrast media injection [45].
It should be noted that, as proven by answers to questions #11 and #13, WB-MRI reporting can be burdensome. Thirty-two out of 48 (67%) radiologists need more than 20 min to report a WB-MRI scan and 29/48 (60%) of radiologists who report WB-MRI have more than 6 years of experience in MRI (27% more than 10 years). WB-MRI interpretation requires the evaluation of a huge number of images with the possibility to use only a small number of sequences. This could be another explanation of the relatively limited diffusion of this imaging modality and especially could justify the low diffusion in private practice (21%), as shown by answers to question #13. Indeed, 38/48 (79%) of centers using WB-MRI were public or academic hospitals, in which improved technology and higher radiologists’ experience could explain this result.
Some limitations of this study should be pointed out: first, the relatively low number of participants to the survey. This could be related by the low diffusion of this imaging modality all over Italy, and we can postulate that WB-MRI is probably mostly performed in referral oncologic centers. Then, we did not perform a subgroup analysis between the different hospitals (public, academic and private) since the small sample size did not allow us to do it, so we were not able to investigate possible differences in the approach to WB-MRI in the different institutions.
In conclusion, 1% of MRIs were WB-MRI scans, which were mainly performed at 1.5T. Lymphoma, myeloma and prostate cancer were the most common indications. We observed an extreme variability in the choice of imaging protocols and use of contrast agents. This survey is an instant picture of the actual use of WB-MRI for oncologic purposes and demonstrates the need of a better standardization of WB-MRI application in clinical practice. It should be a starting point to promote future multicenter studies and expert consensus statements to establish further recommendations and guidelines.
References
Chien SH, Liu CJ, Hu YW et al (2015) Frequency of surveillance computed tomography in non-Hodgkin lymphoma and the risk of secondary primary malignancies: a nationwide population-based study. Int J Cancer 137:658–665. https://doi.org/10.1002/ijc.29433
Huang B, Law MW, Khong PL (2009) Whole-body PET/CT scanning: estimation of radiation dose and cancer risk. Radiology 251:166–174. https://doi.org/10.1148/radiol.2511081300
Lauenstein TC, Semelka RC (2006) Emerging techniques: whole-body screening and staging with MRI. J Magn Reson Imaging 24:489–498. https://doi.org/10.1002/jmri.20666
Galia M, Albano D, Narese D et al (2016) Whole-body MRI in patients with lymphoma: collateral findings. Radiol Med 121:793–800. https://doi.org/10.1007/s11547-016-0658-x
Petralia G, Padhani AR, Pricolo P et al (2019) Whole-body magnetic resonance imaging (WB-MRI) in oncology: recommendations and key uses. Radiol Med 124:218–233. https://doi.org/10.1007/s11547-018-0955-7
Albano D, Patti C, Lagalla R, Midiri M, Galia M (2017) Whole-body MRI, FDG-PET/CT, and bone marrow biopsy, for the assessment of bone marrow involvement in patients with newly diagnosed lymphoma. J Magn Reson Imaging 45:1082–1089. https://doi.org/10.1002/jmri.25439
Kwee TC, Takahara T, Ochiai R et al (2009) Whole-body diffusion-weighted magnetic resonance imaging. Eur J Radiol 70:409–417. https://doi.org/10.1016/j.ejrad.2009.03.054
Albano D, La Grutta L, Grassedonio E et al (2016) Pitfalls in whole body MRI with diffusion weighted imaging performed on patients with lymphoma: what radiologists should know. Magn Reson Imaging 34:922–931. https://doi.org/10.1016/j.mri.2016.04.023
Xu GZ, Li CY, Zhao L, He ZY (2013) Comparison of FDG whole-body PET/CT and gadolinium-enhanced whole-body MRI for distant malignancies in patients with malignant tumors: a meta-analysis. Ann Oncol 24:96–101. https://doi.org/10.1093/annonc/mds234
Li B, Li Q, Nie W, Liu S (2014) Diagnostic value of whole-body diffusion-weighted magnetic resonance imaging for detection of primary and metastatic malignancies: a meta-analysis. Eur J Radiol 83:338–344. https://doi.org/10.1016/j.ejrad.2013.11.017
Dimopoulos MA, Hillengass J, Usmani S et al (2015) Role of magnetic resonance imaging in the management of patients with multiple myeloma: a consensus statement. J Clin Oncol 20(33):657–664. https://doi.org/10.1200/JCO.2014.57.9961
Padhani AR, Lecouvet FE, Tunariu N et al (2017) METastasis Reporting and Data System for Prostate Cancer: practical Guidelines for Acquisition, Interpretation, and Reporting of Whole-body Magnetic Resonance Imaging-based Evaluations of Multiorgan Involvement in Advanced Prostate Cancer. Eur Urol 71:81–92. https://doi.org/10.1016/j.eururo.2016.05.033
https://docs.google.com/forms/. Accessed 28 April 2019
Silvestri E, Barile A, Albano D et al (2018) Interventional therapeutic procedures in the musculoskeletal system: an Italian Survey by the Italian College of Musculoskeletal Radiology. Radiol Med 123:314–321. https://doi.org/10.1007/s11547-017-0842-7
Sconfienza LM, Albano D, Messina C, Silvestri E, Tagliafico AS (2018) How, When, Why in Magnetic Resonance Arthrography: an International Survey by the European Society of Musculoskeletal Radiology (ESSR). Eur Radiol 28:2356–2368. https://doi.org/10.1007/s00330-017-5208-y
Albano D, Patti C, La Grutta L et al (2016) Comparison between whole-body MRI with diffusion-weighted imaging and PET/CT in staging newly diagnosed FDG-avid lymphomas. Eur J Radiol 85:313–318. https://doi.org/10.1016/j.ejrad.2015.12.006
Stecco A, Buemi F, Quagliozzi M et al (2015) Staging of primary abdominal lymphomas: comparison of whole-Body MRI with diffusion-weighted imaging and (18)F-FDG-PET/CT. Gastroenterol Res Pract 2015:104794. https://doi.org/10.1155/2015/104794
Mayerhoefer ME, Karanikas G, Kletter K et al (2014) Evaluation of diffusion-weighted MRI for pretherapeutic assessment and staging of lymphoma: results of a prospective study in 140 patients. Clin Cancer Res 20:2984–2993. https://doi.org/10.1158/1078-0432.CCR-13-3355
Albano D, Patti C, Matranga D, Lagalla R, Midiri M, Galia M (2018) Whole-body diffusion-weighted MR and FDG-PET/CT in Hodgkin Lymphoma: predictive role before treatment and early assessment after two courses of ABVD. Eur J Radiol 103:90–98. https://doi.org/10.1016/j.ejrad.2018.04.014
Mayerhoefer ME, Karanikas G, Kletter K et al (2015) Evaluation of diffusion-weighted magnetic resonance imaging for follow-up and treatment response assessment of lymphoma: results of an 18F-FDG-PET/CT-controlled prospective study in 64 patients. Clin Cancer Res 21:2506–2513. https://doi.org/10.1158/1078-0432.CCR-14-2454
Latifoltojar A, Punwani S, Lopes A et al (2019) Whole-body MRI for staging and interim response monitoring in paediatric and adolescent Hodgkin’s lymphoma: a comparison with multi-modality reference standard including (18)F-FDG-PET-CT. Eur Radiol 29:202–212. https://doi.org/10.1007/s00330-018-5445-8
Littooij AS, Kwee TC, de Keizer B et al (2015) Whole-body MRI-DWI for assessment of residual disease after completion of therapy in lymphoma: a prospective multicenter study. J Magn Reson Imaging 42:1646–1655. https://doi.org/10.1002/jmri.24938
Galia M, Albano D, Tarella C et al (2018) Whole body magnetic resonance in indolent lymphomas under watchful waiting: the time is now. Eur Radiol 28:1187–1193. https://doi.org/10.1007/s00330-017-5071-x
Albano D, Patti C, La Grutta L et al (2017) Osteonecrosis detected by whole body magnetic resonance in patients with Hodgkin Lymphoma treated by BEACOPP. Eur Radiol 27:2129–2136. https://doi.org/10.1007/s00330-016-4535-8
Stecco A, Buemi F, Iannessi A, Carriero A, Gallamini A (2018) Current concepts in tumor imaging with whole-body MRI with diffusion imaging (WB-MRI-DWI) in multiple myeloma and lymphoma. Leuk Lymphoma 12:1–11. https://doi.org/10.1080/10428194.2018.1434881
Kwee TC, Basu S, Torigian DA, Nievelstein RA, Alavi A (2012) Evolving importance of diffusion-weighted magnetic resonance imaging in lymphoma. PET Clin 7(1):73–82. https://doi.org/10.1016/j.cpet.2011.11.001
Adams HJA, Kwee TC, Vermoolen MA et al (2013) Whole-body MRI for the detection of bone marrow involvement in lymphoma: prospective study in 116 patients and comparison with FDG-PET. Eur Radiol 23:2271–2278. https://doi.org/10.1007/s00330-013-2835-9
Albano D, Patti C, Midiri M, Galia M (2018) Osteonecrosis in Hodgkin lymphoma treated by BEACOPP. Intern Med J 48:747–748. https://doi.org/10.1111/imj.13813
Sun M, Cheng J, Zhang Y, Wang F, Meng Y, Fu X (2016) Application value of diffusion weighted whole body imaging with background body signal suppression in monitoring the response to treatment of bone marrow involvement in lymphoma. J Magn Reson Imaging 44:1522–1529. https://doi.org/10.1002/jmri.25300
Albano D, Patti C, Sconfienza LM, Galia M (2017) Whole-body MRI in the early detection of multifocal osteonecrosis. Br J Radiol 90:20170240. https://doi.org/10.1259/bjr.20170280
Chantry A, Kazmi M, Barrington S et al (2017) Guidelines for the use of imaging in the management of patients with myeloma. Br J Haematol 178:380–393. https://doi.org/10.1111/bjh.14827
Oxford Centre for Evidence-based Medicine (2009) Levels of evidence (March 2009). https://www.cebm.net/2009/06/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/. Accessed 4 Aug 2019
Lecouvet FE, Talbot JN, Messiou C et al (2014) Monitoring the response of bone metastases to treatment with Magnetic Resonance Imaging and nuclear medicine techniques: a review and position statement by the European Organisation for Research and Treatment of Cancer imaging group. Eur J Cancer 50:2519–2531. https://doi.org/10.1016/j.ejca.2014.07.002
Schmidt GP, Wintersperger B, Graser A, Baur-Melnyk A, Reiser MF, Schoenberg SO (2007) High-resolution whole-body magnetic resonance imaging applications at 1.5 and 3 Tesla: a comparative study. Invest Radiol 42:449–459. https://doi.org/10.1097/01.rli.0000262089.55618.18
Schmidt GP, Baur-Melnyk A, Haug A et al (2008) Comprehensive imaging of tumor recurrence in breast cancer patients using whole-body MRI at 1.5 and 3 T compared to FDG-PET-CT. Eur J Radiol 65:47–58. https://doi.org/10.1016/j.ejrad.2007.10.021
Schmidt GP, Baur-Melnyk A, Haug A et al (2009) Whole-body MRI at 1.5 T and 3 T compared with FDG-PET-CT for the detection of tumour recurrence in patients with colorectal cancer. Eur Radiol 19:1366–1378. https://doi.org/10.1007/s00330-008-1289-y
Azzedine B, Kahina MB, Dimitri P, Christophe P, Alain D, Claude M (2015) Whole-body diffusion-weighted MRI for staging lymphoma at 3.0T: comparative study with MR imaging at 1.5T. Clin Imaging 39:104–109. https://doi.org/10.1016/j.clinimag.2014.06.017
Chavhan GB, Babyn PS (2011) Whole-body MR imaging in children: principles, technique, current applications, and future directions. Radiographics 31:1757–1772. https://doi.org/10.1148/rg.316115523
Punwani S, Cheung KK, Skipper N et al (2013) Dynamic contrast-enhanced MRI improves accuracy for detecting focal splenic involvement in children and adolescents with Hodgkin disease. Pediatr Radiol 43:941–949. https://doi.org/10.1007/s00247-012-2616-7
Doniselli FM, Albano D, Chianca V, Cimmino MA, Sconfienza LM (2017) Gadolinium accumulation after contrast-enhanced magnetic resonance imaging: what rheumatologists should know. Clin Rheumatol 36:977–980. https://doi.org/10.1007/s10067-017-3604-y
Savarino E, Chianca V, Bodini G et al (2017) Gadolinium accumulation after contrast-enhanced magnetic resonance imaging: which implications in patients with Crohn’s disease? Dig Liver Dis 49:728–730. https://doi.org/10.1016/j.dld.2017.04.010
Takahara T, Imai Y, Yamashita T et al (2004) Diffusion weighted whole body imaging with background body signal suppression (DWIBS): technical improvement using free breathing, STIR and high resolution 3D display. Radiat Med 22:275–282
Attariwala R, Picker W (2013) Whole body MRI: improved lesion detection and characterization with diffusion weighted techniques. J Magn Reson Imaging 38:253–268. https://doi.org/10.1002/jmri.24285
Morone M, Bali MA, Tunariu N et al (2017) Whole-body MRI: current applications in oncology. AJR Am J Roentgenol 209:W336–W349. https://doi.org/10.2214/AJR.17.17984
Albano D, Bruno A, Patti C et al (2020) Whole body magnetic resonance imaging (WB-MRI) in lymphoma: state of the art. Hematol Oncol 38:12–21. https://doi.org/10.1002/hon.2676
Acknowledgements
Authors thank all SIRM members who filled the online poll and participate to the survey giving their consent to publish their names: Simi Astutillo, Carlo Biasiutti, Annalisa Balbo Mussetto, Alessia Cassarà, Stefano Cirillo, Alessandro D’Amore, Francesco Di Bartolomeo, Carmela Falcone, Kamal Faraj, Barbara Frittoli, Silvia Greco, Gianpaolo Grilli, Alessandro Guarise, Rita Loscalzo, Vittorio Macchiarella, Graziella Mangano, Simone Palma, Massimo Pedrazzini, Bortolo Perin, Giovanni Pironi, Pierpaolo Purpura, Vittoria Maria Raciti, Francesco Sani, Alessandro Semeraro, Corrado Tagliati, Lorenzo Tesè and Alberta Villanacci.
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, ethical approval was not required.
Informed consent
For this type of study, patients’ consent was not required since this study did not involve patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Albano, D., Stecco, A., Micci, G. et al. Whole-body magnetic resonance imaging (WB-MRI) in oncology: an Italian survey. Radiol med 126, 299–305 (2021). https://doi.org/10.1007/s11547-020-01242-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-020-01242-7