Abstract
Purpose
To determine the incidence and clinical relevance of extra-intestinal incidental findings (IF) in a cohort of patients with proven or suspected Crohn disease (CD) examined with magnetic resonance enterography (MR-E) in a single University Centre.
Methods
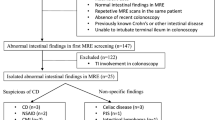
Between January 2018 and June 2019, 182 patients with proven or suspected CD with a planned first MR-E examination, were retrospectively included in this study. Incidental findings were considered as any abnormality identified in the absence of previous clinically suspected or known disease. IF were categorized as unremarkable, benign or potentially relevant findings requiring further imaging or specific treatment.
Results
Of the 182 revised MR-E, extra-intestinal IF were recorded in 70 cases (38.5%); 35 (50%) incidental lesions were recognized as non-significant, 24 (34%) as benign and 11 (16%) as clinically relevant. Moreover, there was a positive correlation between IF and patients’ age (p < 0.0001).
Conclusions
In our experience, a high number of IF (38.5%) was found, with a prevalence that increases with patients’ age. Clinically relevant findings were found in 16% of MR-E. This means that MR-E is a useful tool to detect IF, therefore, the presence of a radiologist during the image acquisition is crucial in adding sequences to the examination.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Small bowel examination represents a challenge for the diagnosis of its diseases by both clinicians and radiologists, because of its relative inaccessibility through conventional endoscopy [1]. Since its introduction in the clinical practice, magnetic resonance enterography (MR-E) has become increasingly important in the diagnosis and staging of small bowel diseases in adult and paediatric patients [2,3,4]. Recently, a huge number of scientific studies have demonstrated its high sensitivity in assessing both activity and severity of Crohn disease (CD) [5,6,7]. Unlike conventional small bowel barium enterography, cross-sectional techniques allow a rapid evaluation of the bowel surface and bowel wall, as well as the detection of abdominal abscesses and perianal lesions, without projection overlapping [1, 8]. In addition to this, MR-E is a radiation-free and panoramic technique: its use as first choice imaging method in children and young patients has raised enormously in last years, together with the number of examination performed in referring centres [9]. Thanks to its wide field of view and to the use of multiple pulse sequences, MR-E consistently visualize extra-intestinal structures and may reveal incidental findings (IF) [10], as some authors have pointed out, encountering clinically relevant IF in 2–30% of the cases [10, 11].
On the one hand, there is concern that IF may lead to further unnecessary investigations resulting in inappropriate resource utilization, augmentation of health care costs, and increased patient anxiety [12, 13]. On the other hand, the discovery of clinically relevant unexpected findings such as small malignancies may lead to early diagnosis with potential reduction of patients’ morbidity [10]. For these reasons, the management of IF is not a simple issue and specific recommendation are available from a number of scientific societies [14,15,16,17,18].
The aim of our study is to retrospectively evaluate the prevalence and clinical relevance of extra-intestinal IF in a cohort of patients with proven or suspected CD examined with MR-E in a single University Centre.
Methods
This is a retrospective study based on the revision of MR-E examinations performed in the Department of Diagnostic imaging of our University hospital in the period from January 2018 to June 2019. Namely, all MR-E reports were identified using our Radiology Information System (RIS) and all the small bowel examinations of patients with known or suspected “Inflammatory Bowel Disease (IBD)” or CD were included. MR-E with indication other than IBD or CD were excluded. In cases of patients undergoing multiple follow-up studies within the considered period, only the first MR-E was considered.
Two hundred and forty MR-E were retrieved from our RIS. 21/240 MR scans performed for indications other than IBD/CD and 37/240 representing repeated scans were excluded. Finally, this study included 182 MR-E (101 males and 81 females, aged 18–83, mean 50, SD 15), which were downloaded from our PACS system and reviewed in consensus by two experienced radiologists. Moreover, the medical history of the patients was examined to record any additional tests or specific treatment within 6 months.
MR-E technique
All MR-E were performed with a 1.5-Tesla MR machine (Philips Achieva 1.5T A-series, Koninklijke Philips Electronics N.V., Eindhoven, The Netherlands) with a 16-channel phased-array torso coil in prone position. The patients were asked to take oral laxatives at different times and personalized doses to cleanse the bowel an overnight before the exam. On the day of the examination, 45–55 min before, each patient received an oral solution of biphasic contrast medium, previously prepared by dissolving 250–300 ml of 18% mannitol in 1500 ml of water in order to achieve a 3.5–4% solution. Inhibition of bowel peristalsis was achieved by injecting 10 ml/mg N-butyl scopolamine (Buscopan, Boringher Ingelheim, Florence, Italy) intramuscularly before starting the MR examination. The MRI protocol consisted of the following breath-hold sequences:
-
1.
Coronal, axial and sagittal 2D balanced turbo-field echo (BTFE): matrix 256 × 256, slice number 40, thickness 8 mm, with 4 mm overlap, TE/TR shortest, flip angle 90°, FOV 350–450, acquisition time 21 s/sequence.
-
2.
Coronal and axial T2w single-shot turbo spin echo (SSh-TSE): thickness 4–5 mm; TE 100 ms; shortest TR; flip angle 90°; matrix 320 × 320; FOV 350–450 mm; breath-hold acquisition.
-
3.
Axial T2w single-shot turbo spin echo SPAIR (SSh-TSE-SPAIR): thickness 4–5 mm; TE 100 ms; shortest TR; flip angle 90°; matrix 320 × 320; FOV 350–450 mm; breath-hold acquisition.
-
4.
Coronal and axial T1w high-resolution isotropic volume (THRIVE): matrix 256 × 256, slice number 100, thickness 2 mm, SENSE factor 4, TE/TR: shortest, flip angle: 10, FOV 350–450, acquisition time 19 s/sequence. These sequences were acquired also after intravenous administration of 0.15 ml/Kg of gadolinium diethylene-triamine penta acetic acid (Gd-DTPA) 0.5 M followed by 20 ml of saline solution with a scan delay of 35, 70 and 120 s.
-
5.
THRIVE acquisitions in the axial and sagittal planes: matrix 256 × 256, slice number 100, thickness 2 mm, SENSE factor 4, TE/TR: shortest, flip angle: 10, FOV 350–450, acquisition time 19 s/sequence.
-
6.
Diffusion weighted images in the axial and coronal planes (b = 0/400/800). Matrix 256 × 256, slice number 35–40, thickness 8 mm, TE/TR: shortest, flip angle: 90.
Image analysis
All MR exams were reviewed in consensus by two senior radiologists (with 10 and 4 years of experience, respectively) in order to recognize extra-intestinal IF defined as unexpected lesions not related to IBD or CD; consequently, extramural complications of CD such as fistulas or abscesses as well as enlarged abdominal lymph nodes were not recorded. IF were classified into three categories: (1) non-significant extra intestinal findings, (2) Benign extra-intestinal findings, (3) Potentially relevant findings requiring further imaging or specific treatment. Finally, the original radiological reports were also checked in order to verify whether IF had already been mentioned.
Statistical analysis
All data were analysed using the Chi-square test, the T-student test and multivariate analysis (ANOVA) with Bonferroni post hoc test. The statistical analysis was performed with STATA/IC software version 14.2. In all tests, significant threshold was set at 5%.
Results
All recorded IF and their clinical significance are detailed in Tables 1, 2 and 3. Extra-intestinal IF were found in 70/182 (38.5%) patients: 33/81 (41%) in females and 37/101 (37%) in males with no statistical differences between these two groups (p = 0.69). Student’s T test showed that the mean age of the 70 patients with extra-intestinal IF was higher than patients without IF (61.4 ± 12.4 vs. 45.2 ± 13.1—p value < 0.0001). After MR-E revision, 35/70 (50%) incidental lesions were deemed as non-significant, 24/70 (34%) as benign, while 11/70 (16%) were classified as clinically relevant. The ANOVA test did not show any statistically significant difference in patient’s age according to the clinical relevance of IF (p = 0.079). Non-significant and benign findings could always be characterized on the images obtained with MR-E (Fig. 1) and no further was needed within 6 months. In case of relevant incidental findings, three patients with adrenal adenoma and abdominal aortic aneurism and two subjects with intraductal papillary mucinous neoplasm (IPMN) of pancreas were scheduled for appropriate follow-up. In one case, MR-E showed a hyperintense linear image in the left lower lobe of the lung requiring a CT scan which displayed the presence of bronchiectasis with mucoid impaction (Fig. 2). In last two cases, MR-E demonstrated a small renal solid lesion requiring surgical consultation (Fig. 3). In both patients, a renal wedge resection was performed and histopathology demonstrated a chromophobe renal cell carcinoma in one case and a low fat angiomyolipoma in the second one.
MR-E of a 45 years old woman. a Coronal Balanced-FFE, b Coronal Contrast enhanced THRIVE, c Coronal T2w SSH, d Unenhanced Coronal THRIVE, e Axial contrast enhanced THRIVE, f coronal b 800 DWI. A round-shaped hypervascular lesion is seen in left hepatic lobe (arrowhead). This lesion is mostly hysointense if compared with surrounding liver and is consistent with FNH
MR-E of a 30 years old man. a Coronal Balanced-FFE, b Coronal T2w SSH, c Axial T2w SSH, d–e Axial unenhanced CT, f Coronal unenhanced CT reformation. MR images show a linear hyperintense image in pulmonary left lower lobe (arrow), but no significant intestinal changes. CT scan demonstrated the presence of bronchiectasis with mucoid impaction (arrow)
MR-E of a 49 years old man. a Coronal balanced-FFE, b Contrast enhanced coronal THRIVE, c Coronal b 800 DWI, d Axial T2w SSH, e Axial contrast enhanced THRIVE, f axial b 800 DWI. MR-E shows a mild thickening of terminal ileum with clear hyperintensity in DWI image (arrowhead). Endoscopy demonstrated Crohn disease in chronic phase. Axial MR images from the same exam depict a 2.5 cm solid renal mass (arrow). After surgical resection, a chromophobe renal cell carcinoma was diagnosed
In 14/70 (20%) cases (1 diaphragmatic hernia, 2 hepatic cysts, 4 renal cysts, 1 uterine fibroid, 1 inguinal hernia, 4 spondylosis and 1 aortic aneurism), the IF described by the reviewing radiologists has not been mentioned in the original report.
Discussion
MR-E, like other diagnostic investigations such as Pulmonary CT-Angiography, Cardiac CT-angiography and Cardiac MRI, is a kind of examination whose aim is to respond to specific clinical questions. However, this examination, even with specific technical requirements, thanks to its inherent characteristics, may incidentally reveal serious and unexpected lesions. According to some authors, although such findings are incidental with respect to the primary purpose, imaging techniques are so prone to discover incidental findings that it is inappropriate to term them ‘unanticipated’ or unexpected [19].
Our study shows that a specific revision of MR-E images looking for extra-intestinal lesions may reveal a very high number of IF (38.5% in our experience). In agreement with previous experiences, the prevalence of IF increases with patients’ age, being unremarkable or benign lesions predominantly represented by renal and hepatic cysts, the most common findings (63%). Contrary to our results, recently Jensen et al. [10] recorded extra-intestinal lesions in a lower number of cases (25%) with a very small percentage of clinical relevant IF (1.5%). In our opinion, the reason for these discrepancies is due to the fact that authors have based their results on the original MR reports, without reviewing MR-E scans. In our experience, 20% of IF had not been described in the original reports: most of unreported IF (13/14—93%) were unremarkable or benign, but in one case, an important condition, such as an aortic aneurism, was missed. In this case, a structured report could be adopted in order to give a clear and standardized description and recommendation for any relevant finding [20].
On the other hand, Herfarth et al. [11] found extra-intestinal lesion in 57% of their MR-E; nevertheless, in this study, the majority of clinically relevant lesions were represented by extra-intestinal complication of CD, such as abdominal abscess, which were excluded from the review by our team. In order to address this kind of discrepancy, essentially linked to a different definition of IF, the American College of Radiology has recently published a white paper with specific recommendations for abdominal and pelvic imaging [18].
In our series, the number of potentially relevant IF was 16%, a higher percentage if compared with the previous literature [21,22,23,24]. This result may be due to our decision to consider as relevant all IF requiring further investigation or follow-up study; for this reason, benign lesions such as adrenal adenoma dropped in this category. Only in one case of the reported series, an indeterminate thoracic IF required further imaging and a Thoracic CT was included in patient’s clinical record, demonstrating left lower lobe bronchiectasis. In our opinion, this is a very interesting data as the use of standard MR examination with a wide surface coil (16 channel torso coil) allowed a good image quality for the entire abdomen, with a significant reduction of indeterminate findings. However, as MR-E usually requires a protocol tailored to the study of small bowel, the careful presence of a Radiologist during image acquisition can be crucial to recognize any IF requiring additional sequences.
IPMN of the pancreatic gland was recognized in two patients, as the presence of cystic lesions are increasingly recognized by imaging studies, namely with the extensive use of MRI [25]. Although a cystic carcinoma is uncommon in patients with asymptomatic pancreatic cysts, a recent consensus of radiologists suggested the need of dedicated MR follow-up, even for cysts < 10 mm in size, as the procedure of choice for evaluating a pancreatic IPMT over the time [26].
A potentially malignant renal lesion was found in two male patients. After surgical consultation, both of them underwent surgery, and a chromophobe cell carcinoma was diagnosed in one case. The possibility of incidental renal masses is well known in the literature. In general, the suggested management of a renal mass begins with ensuring that the lesion is not the result of a disease that can mimic a neoplasm (such as hypertrophied tissue adjacent to scars, vascular anomalies, infarcts and infections). In addition to this, a mass that contains fat can be diagnosed as an angiomyolipoma with confidence in almost 100% of cases. For cystic and solid “non-fatty” renal masses, the management strategy is basically determined by their size, the macroscopic structure and the vascularity [21].
Our study suffers for some limitations. Firstly, it is a retrospective MR revision which cannot replicate the clinical practice. Our evaluation, in fact, was made in consensus by two radiologists who were expressly asked to look for extra-intestinal IF: this kind of study may have led to an over estimation of IF, as well as the high number of well-characterized IF may be linked to the consultation between the two readers rather than to the quality of MRI images. Moreover, we have not verified whether the patients were aware of these findings, which would exclude them from the definition of IF.
In conclusion, MR-E returns a significant number of mostly benign IF. Thanks to its high contrast resolution and to the possibility of a detailed study of the entire abdominal cavity the majority of these IF may be characterized by the same MR examination. IFs should always be mentioned in the final report and the systematic use of a structured reporting system can be useful to have a consistent evaluation of extra-intestinal findings. Well-characterized non-significant and benign findings don’t need any other investigation, while further imaging should be reserved to a restricted number of patients for a precise follow-up schedule (like in the case of IPMN and aortic aneurysm) or to findings requiring a timely treatment.
References
Kim SH (2015) Computed tomography enterography and magnetic resonance enterography in the diagnosis of Crohn’s disease. Intest Res 13(1):27–38. https://doi.org/10.5217/ir.2015.13.1.27
Masselli G, Casciani E, Polettini E, Gualdi G (2008) Comparison of MR enteroclysis with MR enterography and conventional enteroclysis in patients with Crohn’s disease. Eur Radiol 18(3):438–447. https://doi.org/10.1007/s00330-007-0763-2
Laghi A, Borrelli O, Paolantonio P, Dito L, Buena de Mesquita M, Falconieri P, Passariello R, Cucchiara S (2003) Contrast enhanced magnetic resonance imaging of the terminal ileum in children with Crohn’s disease. Gut 52(3):393–397
Ognibene NM, Basile M, Di Maurizio M, Petrillo G, De Filippi C (2016) Features and perspectives of MR enterography for pediatric Crohn disease assessment. Radiol Med 121(5):362–377. https://doi.org/10.1007/s11547-015-0613-2
Macarini L, Stoppino LP, Centola A, Muscarella S, Fortunato F, Coppolino F, Della Valle N, Ierardi V, Milillo P, Vinci R (2013) Assessment of activity of Crohn’s disease of the ileum and large bowel: proposal for a new multiparameter MR enterography score. Radiol Med 118(2):181–195. https://doi.org/10.1007/s11547-012-0841-7
Tolan DJ, Greenhalgh R, Zealley IA, Halligan S, Taylor SA (2010) MR enterographic manifestations of small bowel Crohn disease. Radiographics 30(2):367–384
Scardapane A, Ambrosi A, Salinaro E, Mancini ME, Principi M, Di Leo A, Lorusso F, Stabile Ianora AA, Angelelli G (2015) Assessment of disease activity in small Bowel Crohn’s disease: comparison between endoscopy and magnetic resonance enterography using MRIA and modified MRIA score. Gastroenterol Res Pract 2015:1–7. https://doi.org/10.1155/2015/159641
Fujii T, Naganuma M, Kitazume Y, Saito E, Nagahori M, Ohtsuka K, Watanabe M (2014) Advancing magnetic resonance imaging in Crohn’s disease. Digestion 89(1):24–30. https://doi.org/10.1159/000356210
Athanasakos A, Mazioti A, Economopoulos N, Kontopoulou C, Stathis G, Filippiadis D, Spyridopoulos T, Alexopoulou E (2015) Inflammatory bowel disease-the role of cross-sectional imaging techniques in the investigation of the small bowel. Insights Imaging 6(1):73–83. https://doi.org/10.1007/s13244-014-0377-6
Jensen MD, Nathan T, Kjeldsen J, Rafaelsen SR (2010) Incidental findings at MRI-enterography in patients with suspected or known Crohn’s disease. World J Gastroenterol 16(1):76–82
Herfarth HH, Grunert M, Klebl F, Strauch U, Feuerbach S, Scholmerich J, Rogler G, Schreyer AG (2009) Frequency and nature of incidental extra-enteric lesions found on magnetic resonance enterography (MR-E) in patients with inflammatory bowel diseases (IBD). PLoS ONE 4(4):e4863. https://doi.org/10.1371/journal.pone.0004863
Machaalany J, Yam Y, Ruddy TD, Abraham A, Chen L, Beanlands RS, Chow BJ (2009) Potential clinical and economic consequences of noncardiac incidental findings on cardiac computed tomography. J Am Coll Cardiol 54(16):1533–1541. https://doi.org/10.1016/j.jacc.2009.06.026
Stone JH (2006) Incidentalomas–clinical correlation and translational science required. N Engl J Med 354(26):2748–2749. https://doi.org/10.1056/NEJMp058264
Patel MD, Ascher SM, Paspulati RM, Shanbhogue AK, Siegelman ES, Stein MW, Berland LL (2013) Managing incidental findings on abdominal and pelvic CT and MRI, part 1: white paper of the ACR Incidental Findings Committee II on adnexal findings. J Am Coll Radiol 10(9):675–681. https://doi.org/10.1016/j.jacr.2013.05.023
Khosa F, Krinsky G, Macari M, Yucel EK, Berland LL (2013) Managing incidental findings on abdominal and pelvic CT and MRI, Part 2: white paper of the ACR Incidental Findings Committee II on vascular findings. J Am Coll Radiol 10(10):789–794. https://doi.org/10.1016/j.jacr.2013.05.021
Heller MT, Harisinghani M, Neitlich JD, Yeghiayan P, Berland LL (2013) Managing incidental findings on abdominal and pelvic CT and MRI, part 3: white paper of the ACR Incidental Findings Committee II on splenic and nodal findings. J Am Coll Radiol 10(11):833–839. https://doi.org/10.1016/j.jacr.2013.05.020
Sebastian S, Araujo C, Neitlich JD, Berland LL (2013) Managing incidental findings on abdominal and pelvic CT and MRI, Part 4: white paper of the ACR Incidental Findings Committee II on gallbladder and biliary findings. J Am Coll Radiol 10(12):953–956. https://doi.org/10.1016/j.jacr.2013.05.022
Berland LL (2013) Overview of white papers of the ACR incidental findings committee ii on adnexal, vascular, splenic, nodal, gallbladder, and biliary findings. J Am Coll Radiol 10(9):672–674. https://doi.org/10.1016/j.jacr.2013.05.012
Parker LS (2008) The future of incidental findings: should they be viewed as benefits. J Law Med Ethics 36(2):341–351. https://doi.org/10.1111/j.1748-720x.2008.00278.x
Reiner BI (2009) The challenges, opportunities, and imperative of structured reporting in medical imaging. J Digit Imaging 22(6):562–568. https://doi.org/10.1007/s10278-009-9239-z
Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, Brink JA, Baker ME, Federle MP, Foley WD, Francis IR, Herts BR, Israel GM, Krinsky G, Platt JF, Shuman WP, Taylor AJ (2010) Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol 7(10):754–773. https://doi.org/10.1016/j.jacr.2010.06.013
Hellstrom M, Svensson MH, Lasson A (2004) Extracolonic and incidental findings on CT colonography (virtual colonoscopy). AJR Am J Roentgenol 182(3):631–638. https://doi.org/10.2214/ajr.182.3.1820631
Hassan C, Pickhardt PJ, Laghi A, Kim DH, Zullo A, Iafrate F, Di Giulio L, Morini S (2008) Computed tomographic colonography to screen for colorectal cancer, extracolonic cancer, and aortic aneurysm: model simulation with cost-effectiveness analysis. Arch Intern Med 168(7):696–705. https://doi.org/10.1001/archinte.168.7.696
Hara AK, Johnson CD, MacCarty RL, Welch TJ (2000) Incidental extracolonic findings at CT colonography. Radiology 215(2):353–357. https://doi.org/10.1148/radiology.215.2.r00ap33353
Zhang XM, Mitchell DG, Dohke M, Holland GA, Parker L (2002) Pancreatic cysts: depiction on single-shot fast spin-echo MR images. Radiology 223(2):547–553. https://doi.org/10.1148/radiol.2232010815
Tanaka M, Fernandez-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM, Shimizu M, Wolfgang CL, Yamaguchi K, Yamao K (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 12(3):183–197. https://doi.org/10.1016/j.pan.2012.04.004
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Local ethical committee was informed and approved this retrospective study.
Informed consent
An informed consent was signed by all the patients regarding the possible use of their data for retrospective studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lorusso, F., Principi, M., Pedote, P. et al. Prevalence and clinical significance of incidental extra-intestinal findings in MR enterography: experience of a single University Centre. Radiol med 126, 181–188 (2021). https://doi.org/10.1007/s11547-020-01235-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-020-01235-6