Abstract
Background
The adverse effect of low-dose CT on image quality may be mitigated using iterative reconstructions. The purpose of this study was to evaluate the performance of the full model-based iterative reconstruction (MBIR) and adaptive statistical reconstruction (ASIR) algorithms in low radiation dose and low contrast dose abdominal contrast-enhanced CT (CECT) in children.
Methods
A total of 59 children (32 males and 27 females) undergoing low radiation dose (100kVp) and low contrast dose (270 mgI/ml) abdominal CECT were enrolled. The median age was 4.0 years (ranging from 0.3 to 13 years). The raw data were reconstructed with MBIR, ASIR and filtered back-projection (FBP) algorithms into 6 groups (MBIR, 100%ASIR, 80%ASIR, 60%ASIR, 40%ASIR and FBP). The CT numbers, standard deviations, signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) of liver, pancreas, kidney and abdominal aorta were measured. Two radiologists independently evaluated the subjective image quality including the overall image noise and structure display ability on a 4-point scale with 3 being clinically acceptable. The measurements among the reconstruction groups were compared using one-way ANOVA.
Results
The overall image noise score and display ability were 4.00 ± 0.00 and 4.00 ± 0.00 with MBIR and 3.27 ± 0.33 and 3.25 ± 0.43 with ASIR100%, respectively, which met the diagnostic requirement; other reconstructions couldn’t meet the diagnostic requirements. Compared with FBP images, the noise of MBIR images was reduced by 62.86–65.73% for the respective organs (F = 48.15–80.47, P < 0.05), and CNR increased by 151.38–170.69% (F = 22.94–38.02, P < 0.05).
Conclusions
MBIR or ASIR100% improves the image quality of low radiation dose and contrast dose abdominal CT in children to meet the diagnostic requirements, and MBIR has the best performance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Low-dose CT has been used more often to reduce the potential risks of radiation-induced damage to patients, especially pediatric patients [1]. To further reduce the potential risks of contrast-induced nephropathy, CT scans with both low radiation dose and low contrast dose (“double low”) are often combined in contrast-enhanced CT (CECT) scanning [2, 3]. As low-kV imaging can increase the absorption of iodide ions to improve the enhancement effect of iodine contrast agents [4], it is often used in the “double-low” CT scans. Iterative reconstruction (IR) has been used in the "double-low" CT to reduce image noise and to meet the diagnostic requirements and has been applied to CT applications in chest, abdomen, blood vessel and other areas [5,6,7,8,9,10,11]. In addition, relevant studies have shown that the more sophisticated full model-based iterative reconstruction (MBIR) algorithm is more powerful than the adaptive statistical iterative reconstruction (ASIR) in image noise reduction [12,13,14,15,16,17]. So far, most of the "double-low" CT studies have been focused on blood vessel(s) [3, 4, 6, 8], or in adults, and there are only few reports on CECT in children's abdomen, which often requires higher x-ray doses than other body regions [18]. For this reason, the purpose of this study was to evaluate the performance of MBIR and ASIR algorithms in improving the image quality of "double-low" abdominal CECT in children.
Methods
General data
This retrospective study was approved by the ethics committee of our hospital. The requirement for informed consent was waived. Consecutive pediatric patients in our hospital from August 2015 to October 2015 were included; all patients underwent abdominal CT scans with low radiation dose and low contrast dose scan protocol. The exclusion criteria were adolescent children over 14 years old and/or children weighing more than 35 kg.
Instruments and equipment
All scan data were collected on a 64-row CT scanner with gemstone detector (Discovery, HDCT 750, GE, USA). All patients followed same scan and contrast injection protocol: tube voltage of 100 kV, helical pitch value of 1.375 and rotation speed of 0.4 s. The tube current was set by automatic tube current modulation (ATCM) in the range of 10–700 mA during the scan to obtain age-based image noise index (NI) settings: NI = 11HU for children with age of 0–12 months; NI = 13HU for 1–2 years old; and NI = 15HU for 3–14 years old. Iodixanol (270 mgI/ml, GE Healthcare, America) was used as contrast agent, and contrast dose was adjusted according to the body weight of children (1.8 ml/kg for 3–5 kg, 1.6 ml/kg for 5–10 kg, 1.4 ml/kg for 10–15 kg, 1.2 ml/kg for 15–35 kg). The contrast agent was injected using a single-head power injector at injection rates of 0.4–3.0 ml/s adjusted to a fixed injection time of 15 s. Enhanced scans started at 55 s after the start of injection for children under 3 years of age and 60 s for children over 3 years of age. During CT scans, the children were lying on their back with arms raised over their head without holding breath. Oral sedative medicine (10% chloral hydrate, 0.5 ml/Kg) was given to children who could not cooperate, and scan was performed after subjects fall asleep. The raw data were reconstructed with MBIR, ASIR and filtered back-projection (FBP) reconstruction algorithms into 6 groups (MBIR, ASIR100%, ASIR80%, ASIR60%, ASIR40% and FBP) at image slice thickness of 0.625 mm. Different weights (100%, 80%, 60% and 40%) were applied for the ASIR algorithm.
Subjective image quality evaluation
All images of were transmitted to GE AW4.6 CT workstation for analysis and measurement; the relevant information of children, scanning parameters and reconstruction algorithms was shielded. Image quality evaluation and scoring were carried out by 2 experienced radiologists with 13-year (3-year imaging experience for adult, 10-year imaging experience for children) and 15-year experience in imaging and radiology for children. All images were randomly sorted. During the evaluation process, doctors can adjust window width and level according to their personal habits; multiplanar reconstruction (MPR) and volume rendering (VR) were also available for viewing.
Qualitative evaluation of image quality was performed in refer to relevant studies [6, 19]; the 4-point system was adopted to qualitatively evaluate image quality. The scoring content was divided into two parts: the overall image noise and the display ability of tissues and structures. Standard for overall image noise was as follows: 4 points: image was excellent, only contained very little noise; 3 points: image was fine, contained certain noise and could meet the diagnostic requirements; 2 points: more image noise, could not meet the diagnostic requirements, but could determine lesion location and rough range; 1 point: too much noise, image quality was not acceptable, and there were difficulties in distinguishing between and/or within organizational structures. Criteria for evaluating the display ability of abdominal tissues were as follows: 4 points: obvious enhancement in soft tissue, clear margins of organs and lesions, full diagnostic; 3 points: adequate enhancement in soft tissue, clear margin of organs, abnormal density structures could be identified and measured, still meeting the diagnostic requirement; 2 points: poor contrast enhancement degree in tissue or lesions, unclear margin of organs and the internal structure was not clearly demarcated, for qualitative diagnosis only; 1 point: poor structural enhancement with marginal boundary unclear, could not meet the diagnostic requirement.
Objective image quality measurement
After the subjective image quality evaluation was completed, the two doctors jointly measured the objective image quality: CT number and standard deviation (SD) value (image noise); the porta hepatis section was selected as the measuring cross section, and a region of interesting (ROI) was used for CT number and SD measurement. The ROI was generally about half of the cross-sectional area of the abdominal aorta at the same image layer. The CT and SD values of liver, pancreas, kidney, abdominal aorta and back muscle were measured. Measurement areas were selected on both the left lobe and right lobe for liver, the head and body for pancreas, and the front and back cortex for kidney. Measurements were averaged for the respective organs; the abdominal aorta was only measured once; and the mean value of erector spinae muscles of both sides was calculated. Moreover, signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) of each organ were calculated:
ROIs were placed avoiding pathological changes, and ROI sizes could change based on the organ size. Because of the thinner renal cortex, ROI shape was changed, and ROI area was reduced to 1/4 of the abdominal aorta area.
Radiation and contrast agent dose
The radiation dose and contrast agent dose were recorded. The radiation dose included volumetric CT dose index (CTDIvol) and dose length product (DLP), and the contrast dose included the total volume of contrast agent used. The amount of iodine used was then calculated according to the concentration of the contrast agent.
Statistical analysis
The recorded data of the objective noise and subjective scoring were represented as X ± SD. The analysis of variance (one-way ANOVA) was used to compare the differences in the subjective score and objective measurement among the 6 groups of different reconstruction methods. Tukey’s test was used to compare the statistical differences among reconstruction methods. Kappa test was used to test the consistency of subjective scores of the two physicians; the strength was recommended by Landis and Koch: κ < 0: worst; 0 < κ < 0.20: worse; 0.21 < κ < 0.4: poor; 0.41 < κ < 0.6: moderate; 0.61 < κ < 0.8: good; 0.81 < κ < 1.0: perfect. Statistical analysis was carried out with SPSS 17.0 (IBM, USA) statistical software. P < 0.05 was considered as having significant difference.
Results
Cases information
A total of 59 children (32 males and 27 females) underwent abdominal CECT examination. The median age was 4.0 years (ranging from 0.3 to 13 years). The mean body weight was 16.20 ± 5.28 kg (ranging from 7.0 to 34.0 kg). There were 18 cases of neurogenic tumors, 9 cases of renal space-occupying lesions, 4 cases of liver space-occupying lesions, 1 case of teratoma, 2 cases of pancreatic space-occupying lesions, 13 cases of postoperative reexamination, 3 cases of trauma; moreover, there were 7 cases of abdominal pain to be examined and 2 cases of hematemesis. The radiation dose for the group was 1.67 ± 0.83 mGy in CTDIvol and 41.54 ± 22.78 mGy·cm in DLP. The contrast dose was 21.42 ± 7.42 ml; the amount of iodine used was 5.78 ± 1.95 gI.
Subjective image quality
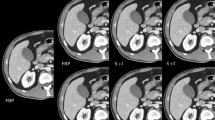
Compared with other images, MBIR images reduced the granular noise artifacts significantly and provided clearer internal structures of organs, which was helpful to detect lesions with smaller density difference and to better display the range and structure of lesions (Figs. 1,
6-year-old boy, abdominal CECT examination; all images were 0.625 mm in slice thickness. a FBP reconstructed image; b 40%ASIR image; c 60%ASIR image; d 80%ASIR image; e 100%ASIR image; f MBIR image. All images had a low contrast object; the contrast of aorta and kidney was better than other tissues. Image noise decreased in IR images, especially in 100%ASIR and MBIR images, and these two groups of images had higher contrast-to-noise ratio (CNR) values. MBIR could display more fine structures, such as gastric mucosa (white arrow), and observe lesions more clearly, such as bile cyst and necrotic lesion (black arrow). The tissues display ability score of the ASIR100% image could meet the diagnostic requirements. The rest of the images could not meet the diagnostic requirements, these images could still be used to identify different density objects, but the structure borders were not clear enough because of the high noise level and low CNR
5-year-old girl, abdominal CECT examination; all images were 0.625 mm in slice thickness. a FBP reconstructed image; b 40%ASIR image; c 60%ASIR image; d 80%ASIR image; e 100%ASIR image; f MBIR image. All images had high contrast objects, such as the hepatic and hepatic vessels (black arrow); all images could display the vessels clearly, but it was difficulty to show some tiny vessels (white arrow) in a–c because of the high image noise, which reduced the contrast-to-noise ratio (CNR). MBIR images had the best image quality. The 80%ASIR and 100%ASIR images provided the diagnostic quality
3-year-old boy suffered from neuroblastoma with necrotic lesion (black arrow) overlapping with small vessels (white arrows). All images were reconstructed using multi-planner reconstruction and were 0.625 mm in slice thickness. a FBP reconstructed image; b 40%ASIR image; c 60%ASIR image; d 80%ASIR image; e 100%ASIR image; f MBIR image. The necrotic lesion could be seen on all images. a–d has difficulty to show tiny vessels because of the high image noise, which reduced the contrast-to-noise ratio (CNR). d–f shows clear margins with MBIR images having the best image quality and 100%ASIR images providing diagnostic quality
The specific scoring results are shown in Table 1. For the overall image noise score, MBIR was the best, followed by ASIR100%, both of which provided diagnostic quality images, while images of the other 4 reconstruction methods did not fully meet the diagnostic quality requirements. With the decrease in ASIR weight, the image quality gradually decreased, FBP image was the worst, and FBP images and ASIR40% images could no longer show clearly the boundaries of organs and lesions; the ASIR60% and ASIR80% images could be used to identify lesions of various low contrast densities, but their edges were not clear enough for accurate size measurements. ASIR100% images could meet the diagnostic requirements, while MBIR images got the full scores for displaying organs and lesions. The inter-observer Kappa value for the subjective image quality score between the two observers was 0.81, indicating a good consistency.
Objective image quality
The objective measurement results are shown in Fig. 4
Objective measurements of MBIR, ASIR and FBP images. There was no statistically significant difference in CT number among different reconstructions; the noise value of FBP image was the highest, with the decrease in ASIR weight, the noise value increased, and that of MBIR image was the lowest; the trends of SNR and CNR were opposite to noise value, those of MBIR image were the highest, and those of FBP image were the lowest
and supplementary file. There was no statistically significant difference in CT numbers among the 6 reconstructed image sets; the noise value of MBIR image was the lowest, followed by ASIR100%; with the decrease in ASIR weight, the noise value increased, and that of FBP image was the highest; compared with FBP image, the noise value of MBIR image was reduced by 64.03%; the trends of SNR and CNR were opposite to noise value, those of MBIR image were the highest, and those of FBP image were the lowest, of which the CNR of MBIR image increased by 165.68% in comparison with that of FBP.
Discussion
With the optimization of scanning protocol, reduction in tube voltage, automatic adjustment of tube current and other ways being studied and utilized, the radiation dose of CT scanning has been greatly reduced. On this basis, some scholars have proposed a "double-low" CT scanning protocol, that is, low radiation dose combined with low contrast dose CT, which can reduce ionization damage and kidney damage caused by contrast agent simultaneously. Yu et al. [4] reported that low-voltage scanning can increase the CT number of contrast agent, so it is possible to maintain CT number by reducing the dose of contrast agent in low-voltage scanning protocol. However, low-voltage scanning may increase image noise and adversely affect image quality.
Iterative reconstructions (IR) can reduce image noise, such as ASIR, and use information obtained from the FBP algorithm, combined with matrix algebra, to transform the measured value of each pixel in the image to a new estimate of pixel value and then compared against the value that the noise model predicts, and over successive cycling an ideal pixel value is created. MBIR algorithm based on ASIR adds physics model and X-ray optical model in addition to the original noise mode to not only consider the noise character, but also the geometric characters of the CT detection system. It can accurately describe each volume pixel and restore the real X-ray detection mechanism.
MBIR has been applied in clinical practice; through the analysis of the existing literature, MBIR can greatly reduce noise and dramatically improve image quality [11,12,13,14,15,16,17,18], so we evaluated 0.625-mm-thin slice image quality instead of routine 5-mm images (with ASIR40%) to obtain more details. In addition, it has been reported that MBIR can improve the recognition of necrotic lesions in children and is suitable for displaying the density difference of soft tissue [20]. Therefore, this study was designed to apply ASIR and MBIR to evaluate the recognition ability of soft tissue lesions in children's abdominal thin slice "double-low" CT and the feasibility of their clinical application.
The subjective evaluation results of this study showed that in terms of overall image noise score, the MBIR image quality was significantly superior to ASIR and FBP image qualities to reach a full mark (4.00 ± 0.00 points); it had significantly less granular image noise, and the image quality was excellent. ASIR image quality was improved in comparison with FBP image quality, and with the increase in ASIR weight, the granular image noise was significantly reduced, the image was better, the image density was more uniform, and the ASIR100% image score reached 3.27 ± 0.33 points, which met the diagnostic requirements; the average overall image noise score was higher than 2 points with ASIR80% and equal to 2 points with ASIR60%, indicating that in some clinical cases, for example, in the images with high contrast and high CNR, these images were acceptable for diagnosis, but for some lesions, the size measurement might not be accurate due to the rough edges caused by image noise. Images with ASIR40% and FBP had overall image noise scores less than 2, indicating that these images could not meet the diagnostic requirements. In terms of the display ability of organs and lesions in abdomen, the MBIR images had the best ability; due to the dramatic reduction in image noise, the contrast noise ratio of MBIR images was significantly improved, which was more conducive to display small structures and low contrast objects. Therefore, MBIR could display more fine structures, such as gastric mucosa (Fig. 1) and small intrahepatic venous vessels (Fig. 2) even in a low contrast situation. MBIR improved the lesion diagnosis both qualitatively and quantitatively. The tissues display ability score of ASIR100% image which was 3.25 ± 0.43 points, which met the diagnostic requirements. The ASIR80%, ASIR60%, ASIR40% and FBP images could show the structure and density of lesions, but because of excessive noise, the edges of lesions with different densities and structures were blurred, and some small structures could not be observed clearly. At the same time, we also noticed that blurring effect could be seen on the edges of MBIR images with different densities, but with low enough image noise, it could still meet the diagnostic requirements and increase the diagnostic confidence of observers. With the increase in ASIR weight, the gradually increased edge blurring effect could be seen at the edges of different densities, but we believed that this blurring effect was not enough to affect the confidence of diagnosis, and was deemed acceptable, which was similar to a previous study [21]. In the abdominal CECT examination of children, we believe that the reason why ASIR100% images could be accepted was that there were obvious density differences among different tissues in images, and these obvious density differences were due to the application of 100 kV low voltage. Under the same conditions, the CT value of contrast agent in low-tube-voltage images was significantly increased in comparison with that in high-tube-voltage images [19, 22], which is conducive to distinguish different structures in CECT images. Even though low-concentration contrast agent (270 mgI/ml) was used in this group of cases, which was 15.63% lower than that of the 320mgI/ml contrast agent commonly used before, it could still maintain a high contrast ratio under 100 kV low-voltage condition. The potential image noise increase in low-tube-voltage scanning was compensated with the use of IR algorithms to ensure adequate contrast noise ratio. The objective noise evaluation results showed that different reconstruction algorithms had no effect on CT number value (F = 0.01–0.04, P > 0.05), but with the increase in ASIR weight, the objective noise of different tissues decreased in various degrees. Compared with FBP image, the noise of MBIR image decreased by 62.86–65.73% (F = 48.15–80.47, P < 0.05) for the respective organs, both SNR and CNR were improved, and the CNR of MBIR image was increased by 151.38–170.69% (F = 22.94—38.02, P < 0.05).
Low-voltage scanning can improve the CT value of contrast agent, which made it possible to reduce the dose of contrast agent. However, the application of low-voltage scanning to patients with large body size will significantly increase image noise and affect image quality. Combining with our practical work experience and referring to the recommendation of ICRP121 [23], 100-kV CT scanning mode was adopted in our clinical work, which took into account the image enhancement degree and the overall noise of images; moreover, it was easy to operate and can be applied in most children's examinations. In order to avoid insufficient penetrating force of X-ray caused by the oversize of children and too much noise which may affect image quality, 120-kV scanning scheme was still adopted for children over 14 years old or weighing more than 35 kg, and they were not included in the study group.
There were some limitations in this study. Firstly, the sample size was small, and differences among different diseases, ages and genders were not considered. The main reason was that the MBIR reconstruction time was too long to meet the speed requirements of our center's daily work, while ASIR provides real-time images. Considering the long reconstruction time for MBIR, we are proposing a two-tiered reconstruction approach: 5-mm 100%ASIR images for routine diagnosis and 0.625-mm MBIR images to provide higher spatial resolution and better image quality for detailed lesion analysis. Secondly, due to the large age span of this group of children, the image quality obtained by other low tube voltages was not compared with. In future research, we will study the application of 80 kV or 70 kV combined with IR algorithms, especially with very young population. Thirdly, our study limited the patient population to children younger than 14 years and less than 35 kg in weight. In the future, this “double-low” research needs to be extended to older and heavier children and also include the use of lower tube voltages. Lastly, this study only had two observers to evaluate image quality and we did not carry out research and evaluation on abdominal CTA.
Conclusion
The “double-low” CT can reduce the potential risks of ionization damage and contrast agent damage, MBIR or ASIR100% can be used to increase image CNR and provide diagnostic quality images in the abdominal CECT scans in children with low radiation dose and contrast dose, and MBIR algorithm provides the best performance.
References
Brenner DJ, Hall EJ (2007) Computed tomography–an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Takahashi Y, Ota H, Omura K et al (2018) Image quality and radiation dose of low-tube-voltage CT with reduced contrast media for right adrenal vein imaging. Eur J Radiol 98:150–157
Cheng B, Xing H, Lei D et al (2018) Impact of iterative model reconstruction combined with dose reduction on the image quality of head and neck CTA in children. Sci Rep 8:12613
Yu L, Bruesewitz MR, Thomas KB et al (2011) Optimal tube potential for radiation dose reduction in pediatric CT: principles, clinical implementations, and pitfalls. Radiographics 31:835–848
Iyama Y, Nakaura T, Iyama A et al (2017) Feasibility of iterative model reconstruction for unenhanced lumbar CT. Radiology 284:153–160
Zhao Y, Zuo Z, Cheng S et al (2018) CT pulmonary angiography using organ dose modulation with an iterative reconstruction algorithm and 3D Smart mA in different body mass indices: image quality and radiation dose. Radiol Med 123:676–685
Yan C, Xu J, Liang C et al (2018) Radiation dose reduction by using CT with Iterative model reconstruction in patients with pulmonary invasive fungal infection. Radiology 288:285–292
Nakagawa M, Ozawa Y, Sakurai K et al (2015) Image quality at low tube voltage (70 kV) and sinogram-affirmed iterative reconstruction for computed tomography in infants with congenital heart disease. Pediatr Radiol 45:1472–1479
Pontana F, Billard AS, Duhamel A et al (2016) Effect of iterative reconstruction on the detection of systemic sclerosis-related interstitial lung disease: clinical experience in 55 patients. Radiology 279:297–305
Fletcher JG, Fidler JL, Venkatesh SK et al (2018) Observer performance with varying radiation dose and reconstruction methods for detection of hepatic metastases. Radiology 289:455–464
Miéville FA, Berteloot L, Grandjean A et al (2013) Model-based iterative reconstruction in pediatric chest CT: assessment of image quality in a prospective study of children with cystic fibrosis. Pediatr Radiol 43:558–567
Lee SH, Yun SJ, Jo HH et al (2018) Diagnosis of lumbar spinal fractures in emergency department: low-dose versus standard-dose CT using model-based iterative reconstruction. Clin Imaging 14:216–222
Sun J, Peng Y, Duan X et al (2014) Image quality in children with low-radiation chest CT using adaptive statistical iterative reconstruction and model-based iterative reconstruction. PLoS ONE 9:e96045
Kataria B, Althén JN, Smedby Ö et al (2018) Assessment of image quality in abdominal CT: potential dose reduction with model-based iterative reconstruction. Eur Radiol 28:2464–2473
Moloney F, Twomey M, Fama D et al (2018) Determination of a suitable low-dose abdominopelvic CT protocol using model-based iterative reconstruction through cadaveric study. J Med Imaging Radiat Oncol 62:625–633
Fontarensky M, Alfidja A, Perignon R et al (2015) Reduced radiation dose with model-based iterative reconstruction versus standard dose with adaptive statistical iterative reconstruction in abdominal CT for diagnosis of acute renal colic. Radiology 276:156–166
Volders D, Bols A, Haspeslagh M et al (2013) Model-based iterative reconstruction and adaptive statistical iterative reconstruction techniques in abdominal CT: comparison of image quality in the detection of colorectal liver metastases. Radiology 269:469–474
Patino M, Fuentes JM, Singh S et al (2015) Iterative reconstruction techniques in abdominopelvic CT: Technical concepts and clinical implementation. AJR Am J Roentgenol 205:W19–31
Sun J, Zhang Q, Hu D et al (2015) Improving pulmonary vessel image quality with a full model-based iterative reconstruction algorithm in 80kVp low-dose chest CT for pediatric patients aged 0–6 years. Acta Radiol 56:761–768
Sun J, Yu T, Liu J et al (2017) Image quality improvement using model based iterative reconstruction in low dose chest CT for children with necrotizing pneumonia. BMC Med Imaging 17:24
Singh S, Kalra MK, Gilman MD et al (2011) Adaptive statistical iterative reconstruction technique for radiation dose reduction in chest CT: a pilot study. Radiology 259:565–573
Matsuoka S, Hunsaker AR, Gill RR et al (2009) Vascular enhancement and image quality of MDCT pulmonary angiography in 400 cases: comparison of standard and low kilovoltage settings. AJR Am J Roentgenol 192:1651–1656
Khong PL, Ringertz H et al (2013) ICRP publication 121: radiological protection in paediatric diagnostic and interventional radiology. Ann ICRP. 42:1–63
Acknowledgements
The authors would like to express our sincere thanks to Dr. Jianying Li for his technical support in understanding the model-based iterative reconstruction algorithm.
Funding
This study was supported by the Beijing Children’s Hospital Young Investigator Program (Grant Numbers BCH-YIPB-2016–06) and Clinical Technology Innovation Project of Beijing Municipal Commission (Grant Numbers xmlx201407).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The present study was approved by the Ethics Committee of Beijing Children’s Hospital. The legal guardian of all the children signed written informed consents.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sun, J., Yang, L., Zhou, Z. et al. Performance evaluation of two iterative reconstruction algorithms, MBIR and ASIR, in low radiation dose and low contrast dose abdominal CT in children. Radiol med 125, 918–925 (2020). https://doi.org/10.1007/s11547-020-01191-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-020-01191-1