Abstract
Objective
The aim of our study was to measure the rate of radiologists’ additional recommended imaging examinations (RAI) at a hospital-based inpatient setting and to estimate the influence on RAI of clinical variables.
Materials and methods
This retrospective study was approved by the institutional review board. Inpatients CT and US examinations interpreted by fifteen radiologists between October and December 2016 were studied. Information about RAI from radiology report texts was extracted manually. The analytic data set included the interpreting radiologists’ years of experience, patient age, patient gender, radiologist gender, ordering service and “clinical question to be answered” as collected from the radiology request forms.
Results
Of the 1996 US and CT examinations performed between October and December 2016 in the inpatient setting, 34% (683 examinations) had a radiologists’ RAI. The largest proportion of RAI was for chest CT, followed by PET-CT, abdominal CT and abdominal MRI. Patient age and gender had no impact on RAI. Radiologists’ years of experience were inversely correlated to RAI. “Pneumonia” showed the highest rate of RAI due to follow-up of lung nodules.
Conclusion
A high percentage of RAI resulted from CT and US radiologists’ reports. The largest proportion of RAI was for chest CT, followed by PET-CT, abdominal CT, and abdominal MRI. Radiologists’ years of experience play an important role in the number of the requested RAI. Further studies with a larger cohort of radiologists are needed to confirm the role of radiologists’ experience in RAI. Also, follow-up studies are warranted to assess the number of RAI that are actually acted upon by the referring physicians.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Medical imaging utilization has grown dramatically in recent years. Indeed, the growth rate of imaging reflects expanded applications that have occurred over the years in high-tech imaging services such as computed tomography (CT), magnetic resonance (MR) imaging and CT-positron emission tomography (PET-CT). Overutilization can be defined as applications of imaging procedures where circumstances indicate that they are unlikely to improve patient outcome [1, 2]. Some publications have suggested that as many as 20–50% of high-tech imaging procedures may fail to provide information that improves patient welfare and therefore may represent, at least in part, unnecessary imaging services [3]. Aside from referring physicians, it has been reported that radiologists too make recommendations for further imaging tests in their interpretative reports [4]. Often the purpose of additional imaging is to reduce uncertainty about equivocal findings at the current examination [4]. Since it may contribute to increased utilization and cost, this tendency has been characterized as being problematic. The aim of our study was to measure the proportion of radiologists’ additional recommended imaging examinations (RAI) at a hospital-based inpatient setting and to estimate the influence on RAI of radiologist gender and radiologist’s years of experience, of patient gender, patient age, ordering service and clinical question to be answered as collected from the radiology request forms.
Methods
Inpatient CT and US examinations interpreted by fifteen radiologists between October and December 2016 at the Fondazione PTV Policlinico Tor Vergata were evaluated by two radiologists. Information about imaging recommendations from radiology report texts was extracted manually. Additional imaging recommendations (RAI) that were for follow-up examinations (by using the same modalities) were included in the study. Reports that recommended “correlate with clinical information” or other suggestions to glean missing clinical information were excluded.
The influence on RAI of radiologist gender and radiologist’s years of experience and of patient gender, patient age and ordering service were evaluated. Also the clinical question to be answered was collected from the radiology request form. For each of the “clinical question to be answered” collected, the number and percentage of examinations with at least one RAI were enumerated. Then the effect size (odds ratios) and significance (confidence intervals) of “each clinical question to be answered” on the likelihood of RAI was calculated.
This retrospective study was approved and waived for patients’ consents by the institutional review board (IRB).
Statistical analysis
Data were analyzed with the nonparametric Mann–Whitney U test. Correlations for the univariate analysis were evaluated with Spearman’s nonparametric test. To assess the independent value of each parameter related to RAI, a principal component analysis (PCA) was performed. A value of p < 0.05 was considered significant. Analyses were performed using Graph Pad Prism software (GraphPad Software, Inc.) and NCSS software (NCSS statistical Software). Odds ratio with the respective confidence intervals was calculated using MedCalc Software.
Results
Analysis of CT and US imaging reports
Of the 1996 US and CT examinations performed between October and December 2016 in the inpatient setting at the Fondazione PTV Policlinico Tor Vergata, 34% (683 examinations) had a radiologist’s recommendation for additional CT, PET-CT or MRI. The largest proportion of imaging examinations prompted by a radiologist’s recommendation was for chest CT (N = 260, 38%), followed by PET-CT (N = 198, 29%), abdominal CT (N = 164, 24%) and abdominal MRI (N = 61, 9%). Chest CT was most often prompted by a recommendation in chest CT (58%) and whole body CT reports (42%); PET-CT, in chest CT (52%) and in whole body CT (48%); abdominal CT, in abdominal US (93%) and in whole body CT (7%) reports; abdominal MRI, in abdominal CT (56%) and in abdominal US (44%) reports. Also, inconclusive radiology examinations were another relatively common reason for additional imaging recommendation (11%).
Pulmonary solid or subsolid nodules < 6 mm were the most common findings that prompted a RAI (31%), followed by adenopathy (23%). The other findings leading to additional imaging were renal lesions (14%), liver lesions (12%) and pulmonary parenchyma abnormalities other than nodules (9%).
Correlation with clinical variables
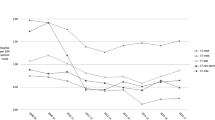
In our cohort, there were 438 patients (172 males and 266 females, mean age 52 ± 14 years), 203 were hospitalized in the clinical medicine department, 132 in the surgery department and 103 in the neuroscience department. As shown in Figs. 1 and 2, respectively, there was no statistically significant correlation between patient age and RAI (r = 0.02, p = 0.066) and patient gender and RAI (male 52 ± 17 years, 95% CI 41–72 vs female 49 ± 23 years, 95% CI 35–63, p = 0.067). As shown in Fig. 3, RAI rates were significantly higher when the ordering service was the clinical medicine department (60 ± 10%, 95% CI 55–66) with respect to surgery (46 ± 13%, 95% CI 36–56 p = 0.042) and to neurosciences (40 ± 10%, 95% CI 34–49 p = 0.032).
Among the radiologists, both sexes were almost equally represented (7 females, 8 males, mean years of experience 15 ± 11). There was a significant negative correlation between the years of experience of the radiologists and RAI (r = − 0.61, p = 0.022), meaning that there was a tendency for experienced radiologists to recommend less RAI (Fig. 4). As shown in Fig. 5, male radiologists (56 ± 15%, 95% CI 45–67) were more prone to recommend RAI with respect to female radiologists (37 ± 12%, 95% CI 27–45, p = 0.024). We performed principal component analysis (PCA) to assess the contribution to RAI of radiologist gender and radiologist’s years of experience. The analysis demonstrated that 62% of RAI were explained by radiologist’s years of experience and 32% by radiologist gender (Fig. 6).
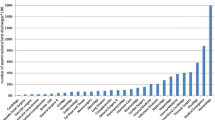
Table 1 gives results stratified according to clinical question to be answered as collected from the radiology request forms. The lowest rate of RAI was found in nephrolithiasis (7%), and this was set as the reference for odds ratios. Pneumonia was notable in being responsible for relatively few examinations overall (5% of total), yet having the highest rate of RAI (odds ratio = 4.24). On the contrary, oncological evaluation was notable in being responsible for the majority of the examination (30% of total), yet having the lowest rate of RAI (odds ratio = 2.83).
Discussion
In our study, we evaluated the rates of additional imaging recommendations (RAI) from US and CT reports in the inpatient setting and estimated the influence on RAI of radiologist gender and radiologist’s years of experience, of patient gender, patient age, ordering service and clinical question to be answered as collected from the radiology request forms. Few studies analyzed the rates of radiologists’ recommendation for additional imaging. Blaivas and Lyon [5] and Baumgarten and Nelson [6] found that in abdominal computed tomographic scans the rate of radiologists’ recommendations for additional imaging in the outpatients setting was, respectively, 31% and 19%, which is comparable to what we found in our inpatient setting (34%). Margolis et al. [7] evaluated the effect of the radiologist on the frequency of recommendations for additional imaging during sonographic (US) interpretation. Examinations were performed at an outpatient radiology facility and at an inpatient emergency department. The authors found that the individual radiologist influenced the frequency of recommendations for additional imaging, the percentages of recommendations for additional imaging ranged from 12% to 45%.
In our study, chest CT was the most represented RAI. The most common reason for this recommendation was 6 months CT follow-up of pulmonary nodules < 6 mm discovered at prior chest CT. The Fleischner Society guidelines for the management of pulmonary nodules exclude from 6 months CT follow-up all nodules < mm 6. We hypothesize that the higher proportion of recommendations for follow-up chest CT of small nodules < mm 6 resulted from our radiologists’ not adherence to these recognized guidelines [8].
PET-CT was the second most frequently RAI. The most common reason for this recommendation was the evaluation of adenopathy discovered at chest CT. Enlarged mediastinal lymph nodes are commonly encountered by radiologists. Lymph nodes may be enlarged due to inflammatory, infectious or malignant reasons. Most of the published studies have shown high PET-CT sensitivity and specificity when maximum standardized uptake value of 2.5 was used as the cutoff to differentiate benign from malignant conditions [9]. However, no clear guidelines have been established for the employment of PET-CT in the evaluation of enlarged lymph nodes [9].
Liver and renal lesions were the other findings that often generated radiologist-recommended MRI or CT evaluation in our cohort. These were incidental findings in US examinations, or in whole body CT. For these lesions, there is currently no criterion aside from follow-up and CT or MRI evaluation by which they can be characterized as benign versus malignant. Although it is known that most incidental findings often have little or no clinical significance, the drive to evaluate them is often prompt by radiologist and patient unwillingness to accept uncertainty, even given the rare possibility of an important diagnosis. Mills et al. evaluated the diagnostic yield of 1000 total abdominal and pelvic ultrasound examinations in patients referred for primary diagnostic ultrasound. The authors found that 9.1% of the patients who underwent abdominal ultrasonography had an incidental finding [10]. However, there is to date little to no literature concerning management of incidental abdominal US findings [11]. On the contrary, the American College of Radiology published a white paper which provides evidence-based guidelines for approaching incidental CT abdominal lesions [12]. Whether this approach will influence radiologists’ behavior will remain subject of speculation.
Negative examinations also resulted in a high number of radiologist-recommended supplement examinations. We hypothesized that this could be explained either a. by practicing defensive medicine or b. by the inappropriate or suboptimal selection of the initial imaging modality.
Indeed, the excessive ordering of diagnostic tests is one of the most frequently encountered forms of defensive medicine (a), which is defined as a deviation from sound medical practice induced mainly by the fear of liability [13]. A review of 16 surveys indicated that 20–81% of physicians had increased their use of diagnostic tests because of liability concerns [14]. Radiologists aware that malpractice liability can make clinical errors more costly, resort to diagnostic tests that, they hope, will reduce the probability of diagnostic error.
However, defensive medicine typically operates together with several other variables to motivate clinical practice decisions [14]. Some of these variables may be clinical such as patient symptoms, seriousness of the suspected disease, degree of certainty about diagnosis and accuracy of the available diagnostic tests. Others are nonclinical, such as availability of technology, years of training and communication skills.
With respect to the radiologist gender, we found that male radiologists were more prone to recommend a supplement examination. A recent study by Tsugawa et al. published in JAMA [15] suggests that female doctors may outperform men due to better communication skills. Thus, it maybe not surprising that in our cohort female radiologists recommend for less supplement imaging than male radiologists.
On the other side, a communication gap between the radiologist and the referring clinician could result in (b.) inappropriate or suboptimal selection of the initial imaging modality [16]. A radiologist–clinician consultation would be advisable for a better and more complete understanding of the clinical scenario, especially for complicated patients with multi-morbidities such as those hospitalized in the clinical medicine department. Notably, in our study the percentage of RAIs were higher when the ordering service was the clinical medicine department. Radiologists and clinicians should be encouraged to routinely dialogue with one another over matters regarding imaging examination selection. Systems with decision support for physician order entry that hold promise for more appropriate selection of imaging studies are now being offered [17]. However, whether or not these systems will lead to changes in radiologists’ recommended clinical imaging also remains to be seen.
Notably, in our cohort of radiologists there was a negative correlation between the radiologists’ years of experience and RAI meaning that there is a tendency in younger participants to recommend supplement imaging. We hypothesize that radiologists improve their accuracy and confidence as they build their experience base and gain more knowledge through continuing education.
When RAI was stratified according to the “clinical question to be answered,” pneumonia showed the highest rate of RAI due to follow-up of lung nodules. On the contrary, oncological evaluation despite being responsible for the majority of examinations (30% of the total) had the lowest rate of RAI. We hypothesized that since oncological patients already undergo timely follow-up, the radiologists were more confident to prescribe less additional imaging.
Our study had limitations. First, we relied on manual review of report texts and had a small sample sizes. Also, our data reflect the rates of the radiologists’ recommendations and not the actual number of resulting examinations. It is possible that recommendations for further imaging are not acted upon by the referring physician [18].
In conclusion, a high percentage of RAI resulted from CT and US radiologists’ reports in our inpatient setting. Chest CT follow-up was the most frequently RAI driven by the presence of pulmonary nodule in prior CT imaging, followed by PET-CT driven by adenopathy documented in prior CT. Radiologists’ years of experience seem to play an important role in the number of the requested RAI. Further studies with a larger cohort of radiologists are needed to confirm the role of radiologists’ experience in RAI. Also, follow-up studies are warranted to assess the number of RAI that are actually acted upon by the referring physicians.
References
Iglehart JK (2006) The new era of medical imaging: progress and pitfalls. N Engl J Med 354(26):2822–2828
Levin DC, Rao VM (2008) Turf wars in radiology: updated evidence on the relationship between self-referral and the overutilization of imaging. J Am Coll Radiol. 5:806–810
Hendee WR, Becker GJ, Borgstede JP, Bosma J, Casarella WJ, Erickson BA, Maynard CD, Thrall JH, Wallner PE (2010) Addressing overutilization in medical imaging. Radiology 257(1):240–245. https://doi.org/10.1148/radiol.10100063
Sistrom CL, Dreyer KJ, Dang PP et al (2009) Recommendations for additional imaging in radiology reports: multifactorial analysis of 5.9 million examinations. Radiology 253(2):453–461
Blaivas M, Lyon M (2007) Frequency of radiology self-referral in abdominal computed tomographic scans and the implied cost. Am J Emerg Med 25(4):396–399
Baumgarten DA, Nelson RC (1997) Outcome of examinations self-referred as a result of spiral CT of the abdomen. Acad Radiol 4(12):802–805
Margolis NE, Rosenkrantz AB, Babb JS, Macari MJ (2015) Frequency of recommendations for additional imaging in diagnostic ultrasound examinations: evaluation of radiologist, technologist, and other examination-related factors. Clin Ultrasound 43(8):463–468
MacMaho H, Naidich DP, Mo Goo J, Soo Lee K, Leung ANC, Mayo JR et al (2017) Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society. Radiology 284(1):228–243
Rayamajhi SJ, Mittal BR, Maturu VN, Agarwal R, Bal A, Dey P, Shukla J, Gupta D (2016) (18)F-FDG and (18)F-FLT PET/CT imaging in the characterization of mediastinal lymph nodes. Ann Nucl Med 30(3):207–216
Mills P, Joseph AE, Adam EJ (1989) Total abdominal and pelvic ultrasound: incidental findings and a comparison between outpatient and general practice referrals in 1000 cases. Br J Radiol 62(743):974–976
West J, Fox JC, Richardson AG, Lopez S, Solley M, Lotfipour S (2011) Implications and approach to incidental findings in liver ultrasound models. Emerg Med 12(4):472–474. https://doi.org/10.5811/westjem.2011.2.2054
Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, Brink JA, Baker ME, Federle MP, Foley WD, Francis IR, Herts BR, Israel GM, Krinsky G, Platt JF, Shuman WP, Taylor AJ (2010) Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol 7(10):754–773. https://doi.org/10.1016/j.jacr.2010.06.013
Plebani M (2014) Defensive medicine and diagnostic testing. Diagnosis 1(2):151–154
U.S. Congress, Office of Technology Assessment, Defensive Medicine and Medical Malpractice (1994) OTA-H–6O2. U.S. Government Printing Office, Washington
Tsugawa I, Jena AB, Figueroa JF et al (2017) Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians: a recently study. JAMA Intern Med 177(2):206–213. https://doi.org/10.1001/jamainternmed.2016.7875
Pinto A, Brunese L (2010) Spectrum of diagnostic errors in radiology. World J Radiol 2(10):377–383
Sistrom CL, Dang PA, Weilburg JB, Dreyer KJ, Rosenthal DI, Thrall JH (2009) Effect of computerized order entry with integrated decision support on the growth of outpatient procedure volumes: seven-year time series analysis. Radiology 251(1):147–155
Lee SI, Krishnaraj A, Chatterji M, Dreyer KJ, Thrall JH, Hahn PF (2012) When does a radiologist’s recommendation for follow-up result in high-cost imaging? Radiology 262(2):544–549. https://doi.org/10.1148/radiol.11111091
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This study was approved and waived for patients’ consents by the institutional review board (IRB). The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Details that might disclose the identity of the subjects under study were omitted.
Rights and permissions
About this article
Cite this article
Squillaci, E., Bolacchi, F., Ricci, F. et al. Radiologists’ recommendations for additional imaging (RAI) in the inpatient setting. Radiol med 124, 432–437 (2019). https://doi.org/10.1007/s11547-018-0982-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-018-0982-4