Abstract
Purpose
To compare the dose calculation accuracy of plans done on a CT density-assigned MR image set for hypofractionated stereotactic radiotherapy (HSRT) using volumetric modulated radiation therapy containing non-coplanar beams.
Methods
Eighteen patients diagnosed with schwannoma treated with HSRT were selected retrospectively. These patients underwent planning CT (pCT) for radiation therapy (RT) and contrast-enhanced three-dimensional fast-spoiled gradient-echo image (3D FSPGR) to assist tumor delineation. CTplan is plan done on pCT. The structures body, bone, and air are contoured exclusively on MR image and assigned Hounsfield units of 25, + 1000, and − 1000, respectively. This is termed as MRCT. After registration, original plans from pCT are pasted on the MRCT. Dose calculation is done in two ways: (1) with preset MU values (DDC) and (2) with optimization (OPT_DC). Conformity indices and Dmax and D0.5cc of brainstem, gamma agreement index and correlation coefficient are analyzed. ANOVA test is carried out to find the significance of difference between plans.
Results
The mean deviations of Dmax and D0.5cc of brainstem for CTplan versus DDC are 2.49% and 1.45% respectively. The mean deviations of Dmax and D0.5cc of brainstem for CTplan versus OPT_DC are − 1.56% and − 1.97%, respectively. Mean deviations of conformity index for DDC and OPT_DC are 0.84% and 0.89%, respectively. No significant difference was found with ANOVA test.
Conclusion
Results show that there is no difference between plans generated with actual CT data and MRCT data. Thus MR scans could be employed for radiation planning provided the verification image is available. This gives us confidence to reduce treatment margins where image registration process is avoided.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acoustic neuromas or vestibular schwannomas (VSs) are benign tumors originated from Schwann cells of the myelin sheath that show a tendency for involvement of sensory nerves. Hypofractionated Stereotactic Radiotherapy (HSRT) with 3 or 5 fractions is the preferred mode of radiotherapy treatments for non-removable VS, where the gross tumor volume is bigger and/or of irregular shape [1, 2]. In addition, fractionated schedules are chosen to better save the organs at risk [3, 4]. Magnetic resonance imaging (MRI) has become a mandatory requirement for HSRT treatment planning and delivery in VS. Traditionally, 1.5 Tesla (T) magnetic resonance (MR) scanners have been used for acquiring MR scans for radiation treatment planning purpose. There is increasing interest to use 3-T MR scanners, which have a high signal-to-noise ratio and therefore higher spatial resolution and lesser image acquisition time [5]. The geometric accuracy of 1.5-T MRI for SRS planning is equally good with 3-T MRI [6]. In MR-only planning, the image registration between CT and MR scans is eliminated, and at the same time, one can get rid of the radiation exposure as a result of a CT scan.
Radiation therapy planning (RTP) depends on three-dimensional (3D) computed tomography (CT) for dose calculation. There is a linear relation between CT number and the electron density values. Significant development in treatment planning systems for past two decades has led to the generation of 3D dose color wash overlapped on the patient CT images at all three planes. Sole MRI-based radiation planning is developed and is successful at various institutes [7,8,9,10]. Many countries still depend on CT-based planning, and MRI primarily assists in delineation of targets and critical structures, where appropriate MR sequence is registered to the planning CT (pCT) images. CT scans are assumed to be geometrically accurate, but in case of MRI, there might be geometric imperfections due to main and gradient magnetic fields and/or due to distribution of magnetic susceptibility values with biological tissues [11].
There are quite a few studies that have employed MR images for radiation planning. Bulk density-assigned MR sequence was explored for dosimetric variation [12]. Autosegmentation of structures from one or more MR sequence(s) was developed where 3D-pseudo-CT is generated and used for subsequent radiation planning [13,14,15]. This study is one of a kind where bulk densities are assigned mainly to three structures (bone, air, and soft tissue), derived directly from MR images. Our aim is to compare the dose calculation accuracy of plans done on planning CT image and CT-value-assigned MR image.
Materials and methods
Patient selection
The scientific and ethics board has approved this work. Eighteen patients diagnosed with schwannoma who had been treated with Linac-based HSRT during 2014–2017 were chosen retrospectively. These patients received HSRT with total dose of 25 Gy given in five fractions. The selected patients for HSRT treatments were based on the size of the tumor greater than 3 cm irrespective of the hearing function. The hypofractionation is physician preference and patients’ expectation. Tumor location is cerebellopontine angle (CP) and treatment beams include two non-coplanar and one coplanar arc. Patient characteristics are shown in Table 1.
Imaging and treatment protocol
Patients were molded with stereotactic masks noninvasively and subsequently CT scans (plain and contrast) were acquired using 64-slice Somotom® Definition AS (M/s Siemens AG) in treatment position with the slice thickness of 1 mm. All patients underwent high-resolution contrast-enhanced 3D fast-spoiled gradient-echo image using Brain volume Imaging (3D FSPGR BRAVO+C) as routine protocol to assist tumor delineation of VS. BRAVO is a high-resolution 3D imaging technique to produce heavily T1-weighted isotropic images of the brain. The MR scan is acquired with GE Signa™ HDxt 1.5-T MR scanner with plane separation of 1 mm and pixel resolution of 0.5 mm−2. Ultra-fast-spoiled gradient-echo image sequences use a small flip angle and very short repetition time and optimized k-space filling to reduce the overall acquisition time. The CT and MR scans are then imported with the Eclipse treatment planning version 11.0 provided by Varian Medical Systems, Palo Alto, USA, and labeled accordingly. FSPGR image is registered with the CT image using rigid registration algorithm version 11.0 (Varian Medical Systems, Palo Alto, USA).
Automatic registration is done using 3D coordinate system and it is followed by manual correction and verification by the oncologists for valid image fusion. An experienced neurosurgeon and radiation oncologist contour the target and its associated critical structures on pCT for isocenter placement and treatment planning. The treated plans on pCT are referred as CTplan. Since this study involves non-coplanar beams, the delineation structures were extended 15 cm in inferio-superior direction. Treatment planning was performed for 6 MV beams on Clinac-iX linear accelerator equipped with 120 leaves millennium multi-leaf collimator and with Eclipse treatment planning software (Varian Medical Systems, Palo Alto, USA) by senior clinical physicists. Progressive resolution optimization algorithm (PRO version 11.0.31) and anisotropic analytical algorithm (version 11.0.31) dose engine are used for the optimization and dose calculation, respectively. The dose calculation grid size greater than 2 mm gives a dose difference of 2.3% of the prescribed dose for IMRT treatments as compared with 1.5 mm especially in high-dose gradient areas [16]. Thus 1.5-mm grid size is used for dose calculation for all plans.
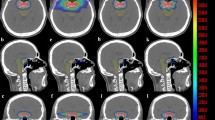
CT number assignment
For this study the structures bone and air are contoured on FSPGR MR Image, while body is autogenerated using MR image directly using body segmentation tool available in Eclipse contouring platform version 11.0. As the image registration is already performed, the structures, the treatment plan along with optimization parameters, and priorities are copied from pCT and pasted on FSPGR image set. In this study, the FSPGR image set is assigned Hounsfield Units (HU) values for three structures created viz: bone = + 1000, air = − 1000, and body (soft tissue) = 25. The corresponding mass densities recommended by ICRU 46 [17] are 1.61 g/cm3 for bone, 0.001 g/cm3 for air cavities and 1.025 g/cm3 for average soft tissue. This HU assigned CT set is called MRCT. Two different plans were generated for each patient on MRCT with (1) direct dose calculation (DDC) with preset MU values and without optimization. (2) Optimizing the same plan without changing the optimization parameters followed by dose calculation (OPT_DC). Figure 1 shows the comparison of 50% isodose coverage of plans generated on (a) planning CT (b) MRCT without optimization and (c) MRCT with optimization.
Evaluation parameters
Parameters such as conformity indices (CI), max dose (Dmax) to brainstem (BS), and dose received by 0.5 cc of brainstem (D0.5cc) were chosen for evaluation of the quality of plans generated. Gamma agreement index (GAI) and correlation coefficient (r) are used to predict the agreement of plans generated on MRCT versus pCT using OmniPro I’mRT Quality Assurance (QA) software (IBA Dosimetry, GmbH, Germany). Dose difference of 3% and distance to agreement of 3 mm was the GAI criteria [18]. The extent of correlation coefficient varies between minus one and plus one, i.e., − 1 ≤ 0 ≥ 1 where r = − 1 indicates perfect inverse correlation, while r = + 1 indicates perfect direct linear correlation between two variables [19]. Detailed descriptions of characteristics of parameters selected for evaluation are found in Table 2 with respect to HSRT treatments.
Single-factor analysis of variance (ANOVA) test is carried out to find the statistically significant difference between the plans generated on CTplan, DDC and OPT_DC. If p value < 0.05, we reject the null hypothesis and conclude that there is a significant difference between the parameters generated from plans.
Results
The metrics mentioned in Table 2 are applied to the extracted data and the results of deviation of DDC and OPT_DC of MRCT from original plan done on pCT are obtained. Figure 2 shows plots of conformity index CI1 (a) comparison between CTplan and DDC (b) comparison between CTplan and OPT_DC. The mean deviation of CI1 for CTplan versus DDC is 3.40%, whereas for CTplan versus OPT_DC is 1.65%. The p value of ANOVA test for conformity index CI1 and CI2 for all three methods is 0.8229 and 0.9444 respectively.
Plots of conformity index CI1a comparison between CTplan and DDC b comparison between CTplan and OPT_DC. CI1-ratio of the prescription isodose volume to the planning target volume; CTplan—plans done on planning CT; DDC—Plans dose on MRCT without optimization; OPT_DC—plans done on MRCT with optimization
The conformity index CI2 with respect to the original planning target volume (PTV) and corresponding passing criteria are given in Table 3. The range and mean deviation values of Dmax and D0.5cc of BS for DDC versus CTplan and OPT_DC versus CTplan are given in Table 4. GAI and correlation coefficient values are also inferred from Table 4. Figure 3 shows radar plot showing mean deviations of (a) maximum dose (Dmax) to the brainstem (b) dose received by 0.5 cc (D0.5cc) of brainstem. The ANOVA test reveals the p value for Dmax and D0.5cc of BS as 0.0586 and 0.4941, respectively.
Discussion
Plan quality comparison
The rationality behind the use of conformity indices (CI1 and CI2) is to ensure that the qualities of the plans are not compromised with the use of MRCT. It is inferred from Fig. 1 that the plans done on MRCT with and without optimization are qualitatively similar to those plans done on pCT and statistically proved with ANOVA test. The gamma analysis and correlation coefficient indices from Table 3 also signify the same. Refer Fig. 4 for a dose color wash in coronal plane in OmniPro I’mRT software for (a) original CT (b) DDC and (c) OPT_DC. GAI and r value was performed to ensure that the plan qualifies for a 2D matrix in transverse plane. This proves that there is no significant bias in the fluences (both DDC and OPT_DC) generated with MRCT. The differences in dose volume histogram of various structures and dose calculation accuracy between original CT and bulk density-assigned CT for different regions (for 3D conformal treatments) have been reported by Jonsson et al [20]. The dosimetric verification of MR versus CT-based planning for prostate patients using intensity modulated radiation therapy has been validated by Chen et al [8].
In this study, the delivered fluences of DDC and OPT_DC were not acquired/analyzed and compared only with approved plans (calculated fluences) done using CTplan. This criterion is sufficient since the treated plans done using pCT passes the routine QA procedures of HSRT treatments.Footnote 1 The mean values of CI2 are not relevant and not discussed here since the passing criterion of CI2 value falls under a range of value and are different for different PTV volumesFootnote 2. (Refer Table 3.) Although the CI1 qualifies the required criteria for individual plans, the mean deviation of CI1 (3.40%) for CTplan versus DDC plans was slightly higher when compared with the mean deviation of CI1(1.65%) for CTplan versus OPT_DC plans. Also, the mean deviations of brainstem doses (Dmax and D0.5cc) are either less or mostly present in the negative quadrant for OPT_DC plans (refer Fig. 2). It is obvious that the optimization done on an MRCT closely matches the CI1 values of OPT_DC plans with CI1 values of the plans done on pCT.
Brainstem dose comparison
Dmax and D0.5 cc are considered for evaluation because, in all patients considered under this study, BS lies in close proximity to the PTV and in addition HSRT involves delivering unusually high dose per fraction of 5 Gy (steep dose fall off). The slightly higher deviation of mean CI1 and mean deviation of BS doses for DDC plans may be due to the registration errors between pCT and MRCT (FSPGR MR Image set) and/or heterogeneous HU values between them. This deviation may also because of mild/negligible peripheral distortions from MR image set as the soft tissue structure (body) is created using MR image set. The peripheral distortions from MR images is considered negligible because the mean CI1 and mean deviation of BS doses still pass for plans created using DDC. This is also evident from the ANOVA tests where p value is > 0.05.
The location of tumors in this study is in the region of hetero-density area (CP angle). The effect of mass density assignment of bone, soft tissue, and air cavities on the BS doses and PTV are not significantly different as evaluated here. There have been several studies suggesting the use of MR images directly for radiation planning [11,12,13,14,15] which involves generation of pseudo-CT/synthetic CT generation. Although RTP is feasible, the delivery requires generation of verification images (2D or 3D) for comparison at the treatment table. An in-house solution has been developed by Christiansen et al [12] to facilitate daily online setup verification with the planning image. Refer Fig. 5 for comparison of (a) present radiotherapy workflow with (b) simple MR-only workflow for radiation therapy.
Limitations and future outlook
Although geometric distortions (both peripheral and medial) are not considered in this study, results show that they have least influence in plans compared. Such assessment along with other MR QA procedures will boost the confidence to use appropriate MR image set in RTP not only qualitatively but quantitatively too. Also generation of verification image set is not discussed, as this work is confined to the radiation treatment planning on density-assigned MR sequence. Future study involves the development of robust algorithms to auto-generate CT equivalent HU values from appropriate MR sequences and creation of verification image set. The Philips MRCAT approach for an MR-only-based dose planning provides CT-like density information calculated from MR images for dose calculations, as well as high-contrast anatomical T2-weighted images for target delineation [21]. Evaluation of biological advantage (focused on the normal tissue complication probability) in reducing PTV margins with the direct use of MR image also holds good prospects in the future.
Conclusion
Results show that there is no evidence of difference between the plans generated with actual CT data and MRCT data. MR scans could possibly be employed for radiation planning if verification image is generated and validated for treatment. Thus, MR-only planning is possible as attempted here for small focal brain lesions, and it gives us further room for reducing treatment margins especially in SRS/HSRT treatments where image registration process is avoided.
Notes
RTOG Radiosurgery guidelines, 1993.
Refer Table 1 in page no. 17 from RTOG 0915.
References
Apicella G, Paolini M, Deantonio L, Masini L, Krengli M (2016) Radiotherapy for vestibular schwannoma: review of recent literature results. Rep Pract Oncol Radiother 21(4):399–406
Murphy ES, Suh JH (2011) Radiotherapy for vestibular schwannomas: a critical review. Int J Radiat Oncol Biol Phys 79:985–997
Thomas C, Di Maio S, Ma R, Vollans E, Chu C, Math M, Clark B, Lee R, McKenzie M, Martin M, Toyota B (2007) Hearing preservation following fractionated stereotactic radiotherapy for vestibular schwannomas: prognostic implications of cochlear dose. J Neurosurg 107(5):917–926
Mulder JJ, Kaanders JH, van Overbeeke JJ, Cremers CW (2012) Radiation therapy for vestibular schwannomas. Curr Opin Otolaryngol Head Neck Surg 20(5):367–371
Schmidt MA et al (2017) Stereotactic radiosurgery planning of vestibular schwannomas: is MRI at 3 Tesla geometrically accurate? Med Phys 44(2):375–381
Zhang B, MacFadden D, Damyanovich AZ, Rieker M, Stainsby J, Bernstein M, Jaffray DA, Mikulis D, Ménard C (2010) Development of a geometrically accurate imaging protocol at 3 Tesla MRI for stereotactic radiosurgery treatment planning. Phys Med Biol 55(22):6601
Lambert J, Greer PB, Menk F, Patterson J, Parker J, Dahl K, Gupta S, Capp A, Wratten C, Tang C, Kumar M (2011) MRI-guided prostate radiation therapy planning: investigation of dosimetric accuracy of MRI-based dose planning. Radiother Oncol 98(3):330–334
Chen L, Price RA, Wang L, Li J, Qin L, McNeeley S, Ma CM, Freedman GM, Pollack A (2004) MRI-based treatment planning for radiotherapy: dosimetric verification for prostate IMRT. Int J Radiat Oncol Biol Phys 60(2):636–647
Beavis AW, Gibbs P, Dealey RA, Whitton VJ (1998) Radiotherapy treatment planning of brain tumours using MRI alone. Br J Radiol 71(845):544–548
Tyagi N, Fontenla S, Zelefsky M, Chong-Ton M, Ostergren K, Shah N, Warner L, Kadbi M, Mechalakos J, Hunt M (2017) Clinical workflow for MR-only simulation and planning in prostate. Radiat Oncol 12(1):119
Schmidt MA, Payne GS (2015) Radiotherapy planning using MRI. Phys Med Biol 60(22):R323
Wang H, Chandarana H, Block KT, Vahle T, Fenchel M, Das IJ (2017) Dosimetric evaluation of synthetic CT for magnetic resonance-only based radiotherapy planning of lung cancer. Radiat Oncol 12(1):108
Christiansen RL, Jensen HR, Brink C (2017) Magnetic resonance only workflow and validation of dose calculations for radiotherapy of prostate cancer. Acta Oncol 56(6):787–791
Edmund JM, Nyholm T (2017) A review of substitute CT generation for MRI-only radiation therapy. Radiat Oncol 12(1):28
Johansson A, Karlsson M, Nyholm T (2011) CT substitute derived from MRI sequences with ultrashort echo time. Med Phys 38(5):2708–2714
Chung H, Jin H, Palta J, Suh TS, Kim S (2006) Dose variations with varying calculation grid size in head and neck IMRT. Phys Med Biol 51(19):4841
White GR, Wilson IJ (1992) Photon, electron, proton and neutron interaction data for body tissues. ICRU report 46
Low DA (2010) Gamma dose distribution evaluation tool. J Phys Conf Ser 250(1):012071
Varatharaj C, Ravikumar M, Sathiyan S, Supe SS, Vivek TR, Manikandan A (2010) Dosimetric verification of brain and head and neck intensity-modulated radiation therapy treatment using EDR2 films and 2D ion chamber array matrix. J Cancer Res Ther 6(2):179
Jonsson JH, Karlsson MG, Karlsson M, Nyholm T (2010) Treatment planning using MRI data: an analysis of the dose calculation accuracy for different treatment regions. Radiat Oncol 5(1):62
Köhler M, Vaara T, Grootel MV, Hoogeveen R, Kemppainen R, Renisch S (2015) MR-only simulation for radiotherapy planning. Philips White Paper. Koninklijke Philips NV, Amsterdam
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors contributed to this study declare that they have no conflict of interest with respect to the manuscript.
Ethical standards
Institutional scientific and ethics board has approved this study. This article does not contain any studies with human participants performed by any of the authors.
Informed consent
The informed consent has been waived off by the ethics board of the institute considering this as a retrospective study.
Rights and permissions
About this article
Cite this article
Ilamurugu, A., Chandrasekaran, A.R., Ayyalusamy, A. et al. Feasibility of MR-only radiation planning for hypofractionated stereotactic radiotherapy of schwannomas using non-coplanar volumetric modulated arc therapy. Radiol med 124, 400–407 (2019). https://doi.org/10.1007/s11547-018-0981-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-018-0981-5