Abstract
Neighborhood characteristics may moderate the effects of Medicaid coverage on health outcomes. Identifying this interplay can inform the design, targeting, and implementation of health policy. We combine data from the Oregon Health Insurance Experiment, which randomized access to Medicaid, with rich new data on multiple domains of neighborhood characteristics to assess the interaction between the local environment and the effect of insurance on health. Overall, we do not find that neighborhood characteristics substantially affect the relationship between gaining insurance and health outcomes, suggesting that Medicaid expansions are similarly effective across neighborhoods. This analysis highlights the complex relationship between health insurance coverage, neighborhood characteristics, and health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Policymakers have often implemented Medicaid expansions to improve population health in the USA. Access to Medicaid may reduce the price and increase the use of healthcare, or alleviate the stress or stigma associated with being uninsured [1]. Empirical evidence establishes a causal relationship between Medicaid coverage and health outcomes. For example, the Oregon Health Insurance Experiment (OHIE) used a lottery to randomize access to Medicaid to identify the effects of health insurance coverage on physical health, mental health, and health-related quality of life [2]. This analysis found that Medicaid coverage reduced the prevalence of depression and improved mental health-related quality of life among low-income adults approximately 2 years later, but had no detectable effects on physical health outcomes. However, a less-explored area of research is the extent to which environmental or social determinants of health interact with Medicaid coverage to shape health outcomes.
Neighborhood characteristics may play a key role in the effectiveness of Medicaid expansions. For instance, if gaining insurance results in enrollees receiving advice to modify their diet or to exercise more, they may be better able to follow that advice if they live in a neighborhood with more grocery stores or active living opportunities. Low-income populations, which have fewer resources and more limited mobility, may be particularly affected by local area features [3]. An extensive literature documents associations between neighborhood characteristics and health outcomes [4,5,6]. Furthermore, the US Department of Housing and Urban Development’s Moving to Opportunity intervention, which randomized families living in high-poverty housing with the ability to move to neighborhoods with less poverty, demonstrated reductions in long-run obesity and diabetes, and improved “subjective well-being” among participants [7,8,9]. Nonetheless, there is very limited evidence on the interplay between neighborhood characteristics and health insurance coverage.
In this study, we analyze how factors associated with specific neighborhood characteristics moderate the causal effects of Medicaid coverage on health using data from the OHIE. A previous, exploratory study using our data documented various associations between neighborhoods and health outcomes [10], and found that that areas with less socioeconomic deprivation, more grocery stores, and additional active living features experienced better health than other areas. Neighborhood characteristics may thus affect health directly, but they may also proxy for other factors associated with the people who live in neighborhoods with those characteristics. For example, higher-income populations likely have the resources to live in neighborhoods with more amenities, as well as better access to healthcare. Although this makes it difficult to attribute differences in outcomes to the neighborhood characteristics themselves, rather than correlated unobserved factors, a better understanding of these relationships has the potential to improve the effectiveness of health policy by identifying local areas where health insurance expansions are particularly effective or ineffective—and where targeting funding, programs, and other resources might generate the greatest health gains.
Methods
Study Participants
Our study population consists of participants in the Oregon Health Insurance Experiment (OHIE), a randomized controlled trial that evaluated the effects of health insurance coverage on uninsured, low-income adults in Oregon [1, 2]. OHIE participants signed up for a waitlist that provided their household with the opportunity to apply to Oregon’s Medicaid program. In 2008, the state conducted a random lottery in order to allocate the limited number of available slots. The study population represents these lottery participants, which include both lottery winners that were able to apply for Medicaid coverage and non-winners. Data on the OHIE and its participants have been previously described in detail [1].
Roughly 2 years after the OHIE lottery, between September 2009 and December 2010, an in-person assessment was conducted on OHIE participants living in the Portland area. This survey included clinical and subjective health measurements, as well as sociodemographic information, collected from 12,229 individuals. Our study sample consists of these in-person survey respondents. Details on this in-person survey, data, and analysis has been previously described in detail [2].
Health Outcomes
We selected a subset of health measures from the in-person survey data to use as outcomes. We chose primary summary health outcomes to represent three dimensions of health (physical, mental, and health-related quality of life), in order to minimize multiple comparisons issues. In addition, we included a handful of secondary outcomes to test specific hypotheses. There is additional discussion of the selection of outcomes and hypotheses elsewhere [11].
First, we use the Framingham risk score to represent the physical health dimension [12]. The Framingham risk score is a continuous measure of the 10-year risk of a cardiovascular event, where higher values indicate greater risk. This outcome is calculated for respondents aged 30 and older based on age, systolic blood pressure, total cholesterol, high-density lipoprotein (HDL) cholesterol, medication use for high blood pressure, current smoking, and a glycated hemoglobin level greater than or equal to 6.5% (diabetes), with separate computations for men and women.
Next, we select the continuously measured Patient Health Questionnaire (PHQ-8) total score to represent mental health. The PHQ-8 is a standard means of measuring depression, and captures how frequently a respondent experiences eight depression symptoms: depressed mood, anhedonia, trouble sleeping, fatigue, problems eating, feeling like a failure, trouble concentrating, and moving or speaking more slowly or rapidly than usual [13]. The total score ranges from zero to 24 and is obtained as the sum of each symptom scored from zero to three (“not at all” to “nearly every day”). A higher score implies a greater severity of depression symptoms.
Finally, we summarize health-related quality of life using the SF-8 physical and mental component scores (PCS and MCS, respectively) [14]. These composites are continuously measured indices that range from zero to 100, with a higher score suggesting a better health-related quality of life.
We also organized the secondary outcomes of interest used for specific hypothesis testing along these dimensions. Physical secondary outcomes include systolic and diastolic blood pressure (continuously measured in mmHg), total and HDL cholesterol (continuously measured in mg/dL), glycated hemoglobin (continuously measured HbA1c level), and body mass index (BMI) calculated from weight and height measurements. For secondary mental health, we also examine a positive depression screen result, which is an indicator for scoring a ten or greater on the PHQ-8. Health-related quality of life outcomes additionally include indicators for self-reported “not poor or very poor” general health in the last 12 months (self-reported general health status in the last 12 months categorizes health as “excellent,” “very good,” “good,” or “fair” health versus “poor” or “very poor” health), and for being “very happy” or “pretty happy” versus “not too happy.”
Medicaid Coverage
The in-person survey data provided indicators that represent selection in the randomized lottery and Medicaid coverage status. Medicaid coverage is defined as ever having been on Medicaid during the study period. This data also provides information on the number of household members included on the lottery list.
Covariates
We also obtained information on sociodemographic characteristics to include as covariates: continuous age in years; a dummy for gender; a continuous measure of approximate household income (average household income is coded using midpoints and top coded at $50,000); dummies for educational attainment (less than high school, high school diploma or GED, post-high school but less than a 4-year degree, and 4-year degree or more); dummies for employment status (not currently employed, employed less than 20 h per week, employed 20 to 30 h per week, and employed 30 h or more per week); and indicators for race/ethnicity (White, Black, Hispanic, and Other, where respondents can report more than one race or ethnicity).
Neighborhood Characteristics
We collected primary and secondary data on neighborhood characteristics and organized these measures into five separate domains representing different aspects of the local environment: socioeconomic deprivation, food access, park access and green space, attributes that promote active living, and land use. We selected one representative neighborhood characteristic variable for each domain from a large number of potential variables using principal component analyses and based on the strength of its association with health outcomes in prior analyses [10]. Potential underlying mechanisms linking Medicaid coverage, neighborhoods, and health are outlined elsewhere, though we are unable to test if these particular channels are responsible for results [11]. Additional details on data collection, sampling, and variable construction and selection were also described previously [10, 11].
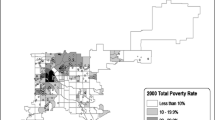
Socioeconomic deprivation is represented by a census tract-level index that was generated using 2005–2009 5-year American Community Survey data. This socioeconomic deprivation index was constructed following the methodology of Messer et al. (2006) [15]. Specifically, we used principal component analyses to select and combine tract-level data on neighborhood deprivation-related variables. The final index score reflects neighborhood ethnicity, education, employment, poverty, and housing/crowding, and a higher value suggests a greater level of socioeconomic deprivation.
The food access, park access and green space, and active living domains of neighborhood characteristics were similarly constructed by linking each respondent’s address to various address-level data using ArcGIS. First, to characterize the food access domain, we use the count of grocery stores in a one-mile radius. This variable was generated by linking each respondent’s address to various types of food stores within specific radii in 2009 INFOUSA business licensing data. The park access and green space domain is represented by acres of tree coverage within a quarter-mile radius, created by mapping each respondent’s address to Metro regional planning data. Next, the active living domain focuses on frequency of transit service, measured as average stops per day in a half-mile radius, constructed by connecting each respondent’s address to 2009 Tri-Met transit systems data.
Finally, the land use domain is represented by the share of street segments in a census tract with retail or small business land use. This variable ranges between 0 and 1 (representing zero to 100% of street segments within a tract) and was generated from 2011 street audit data collected using the Active Neighborhood Checklist [16]. Retail or small business land use is defined as the presence of: a small grocery or convenience store, a pharmacy, a home-based business (e.g., daycare, tax prep, salon), a food establishment, an entertainment establishment, a small commercial building, an indoor fitness facility, a big box store, a mall or strip mall, or a supermarket.
Analytic Sample
Our cross-sectional analytic sample consists of the OHIE in-person survey data linked to the selected neighborhood characteristics of respondents, with complete data on health outcomes, neighborhoods, and sociodemographic controls. The sample represents 8413 respondents residing in 196 census tracts.
We also separately test specific hypotheses using two particularly vulnerable subgroups in our analytic sample: individuals with a preexisting “high risk” diagnosis (2095 respondents with a pre-lottery diagnosis of diabetes, hypertension, hypercholesterolemia, myocardial infarction, or congestive heart failure) and individuals with a pre-lottery diagnosis of depression or anxiety (2797 respondents) [11].
Statistical Analysis
The OHIE provided participants with the opportunity to apply for Medicaid coverage. However, not all lottery winners obtained coverage, due to failure to submit an application or pass the eligibility requirements. Nonetheless, winning the lottery increased the probability of Medicaid enrollment by 22.7 percentage points (p < 0.01) in our analytic sample [11].
Our empirical strategy is adapted from an instrumental variable approach based on previous OHIE methods that identify the causal effects of Medicaid coverage on health [2]. We fit two stage least squares (2SLS) regressions, using lottery selection and a lottery selection-neighborhood characteristic interaction term as instruments for Medicaid coverage and a Medicaid coverage-neighborhood characteristic interaction term. The estimate on the latter interaction term captures how a neighborhood characteristic moderates the causal impacts of Medicaid coverage on health outcomes. We interpret this coefficient as the extent to which the local average treatment effect (LATE) of Medicaid coverage varies based on a neighborhood characteristic. We additionally obtain estimates of variation in intent-to-treat (ITT) effects across neighborhood characteristics to document how neighborhoods moderate the causal effects of lottery selection on health.
All regressions include sociodemographic covariates. We also control for the number of individuals within a household included on the lottery list; selection in the lottery allowed the entire household to apply for Medicaid coverage; thus, household size is correlated with winning the lottery. All regressions are weighted in order to account for the sampling design [2], and all standard errors are clustered by census tract in order to allow for correlation of the error term at the most aggregate neighborhood level. Our analyses were pre-specified and publicly archived, unless otherwise noted, to minimize data and specification mining concerns [11]. We address the issue of multiple comparisons by focusing primarily on four pre-specified summary outcomes (rather than implementing multiple inference adjustment across discrete domains).
Results
Summary Statistics
Table 1 presents the mean individual and neighborhood characteristics for the analytic sample. We find that there are no statistically significant differences between the control group and lottery winners. Furthermore, Table 2 presents the control group means for the selected summary and secondary health outcomes, as well as the causal effects of Medicaid coverage for our analytic sample.
Medicaid Coverage and Neighborhood Characteristics
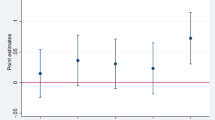
In general, factors associated with neighborhood characteristics appear to play a limited role in moderating the effects of health insurance coverage on health in our analytic sample. Table 3 presents all LATE results for summary health outcomes (complete results from all pre-specified analyses, including ITT and LATE estimates for summary and secondary outcomes are available in Tables 7, 8, and 9 in the Appendix). In all tables, we present our estimates of the effects of Medicaid coverage on the Framingham risk score and all indicator outcomes as percentage point changes. The socioeconomic deprivation, food access, park access and green space, and land use domains do not statistically significantly interact with Medicaid coverage to influence summary or secondary health outcomes, although several results are borderline significant (p < 0.1).
Active living characteristics, however, do significantly moderate the effects of insurance. Features associated with this domain, measured as the frequency of transit service in average stops per day in a half-mile radius, moderate the impacts of Medicaid coverage on two of our selected physical health outcomes. First, Medicaid coverage has limited effect on cardiovascular risk in areas with few transit stops, but worsens cardiovascular risk in areas with more frequent transit service. Table 4 highlights and expands upon these LATE results. We find that Medicaid coverage increases cardiovascular risk by 0.3 percentage points in areas with mean frequency of transit service, and by 1.1 percentage points in areas where frequency of transit service is one standard deviation above the mean.
To further explore this result, we analyze the component inputs into the cardiovascular risk score: systolic blood pressure (mmHg), total and HDL cholesterol (mg/dL), use of medication for high blood pressure, current smoking status, and diabetic glycated hemoglobin (this analysis was not pre-specified). We do not find evidence that any single input is driving the Framingham risk score result. Table 5 presents these findings. Medicaid worsens total cholesterol, current smoking, and diabetic hemoglobin more in areas with more frequent transit service, but none of these moderating effects is statistically significant. Similarly, Medicaid coverage diminishes the probability of taking high blood pressure medication in areas with more frequent transit service. However, this is unlikely to drive our result; a decrease in the use of blood pressure medication is associated with improvements in the Framingham risk score.
Second, active living features moderate the effects of health insurance coverage on BMI, a secondary physical outcome. Table 6 presents our LATE estimates (ITT results are available in Table 8 in the Appendix). Medicaid coverage increases BMI by 0.8 in areas with mean frequency of transit service and decreases BMI by 0.4 in areas with frequency of transit service one standard deviation above the mean. Thus, living in a neighborhood with more transit stops enables Medicaid to reduce BMI. In order to test if this result is determined by reductions in obese or overweight groups, we examine additional outcomes: indicators for an overweight BMI (a BMI value greater than or equal to 25) and obese BMI (BMI greater than or equal to 30) (these analyses were not pre-specified). We further show in Table 6 that this effect is mainly driven by beneficial impacts on the probability of obesity.
We explore this result through two (non-pre-specified) follow-up analyses. To investigate whether the moderating effects of active living features are driven by areas with particularly low or particularly high frequency of transit stops, we examine the extent to which the effects of Medicaid coverage are heterogeneous across quartiles of this metric. Our results in Table 10 in the Appendix do not show consistent or significant patterns. To explore the extent to which respondent characteristics vary across active living features, we evaluate the mean values of our sociodemographic covariates by quartile of this neighborhood characteristic. This analysis, available in Table 11 in the Appendix, suggests that residents of areas with greater frequency of transit service are more male, slightly older, less likely to be White and Hispanic and more likely to be Black, more likely to work less than 30 h per week, and have lower household income compared to residents of areas with less transit service. We control for the direct effect of these individual characteristics, though unobserved individual characteristics may of course also vary across areas. As noted above, we are unable to differentiate between the moderating effects of neighborhood characteristics themselves and the moderating effect of factors correlated with those neighborhood characteristics.
Robustness Tests
We conduct several robustness tests to examine the strength of our statistically significant findings (these analyses were not pre-specified). First, we investigate whether other metrics of active living produce similar findings to those using frequency of transit service. As shown in Table 12 in the Appendix, we find similar patterns using other metrics, such as population and business densities per acre within a quarter mile radius (these variables were similarly constructed by linking each respondent’s address to Metro regional land information system data and 2009 INFOUSA business licensing data, respectively, using ArcGIS). This result is perhaps not surprising given that the other metrics are highly correlated with frequency of transit service (correlation coefficients of 0.85 and 0.82). The estimates of the moderating effect of population density for BMI are particularly strong.
Next, we include multiple domains of neighborhood characteristics in the same regression, including transit service, food access, and park access and green space metrics. These domains were selected due to their borderline statistical significance in the main LATE analysis of the cardiovascular risk score (Table 3, p < 0.1), as well as their independent potential to influence physical health outcomes. Table 13 in the Appendix shows these results. Accounting for these, other domains attenuate the extent to which transit service moderates the effects of Medicaid coverage on cardiovascular risk. However, the impact of Medicaid coverage on BMI is stable across specifications.
Vulnerable Subgroups
We further evaluate the extent to which each domain of neighborhood characteristics moderates the effects of Medicaid coverage for vulnerable subgroups. First, we investigate these moderating effects on the Framingham risk score for respondents with a preexisting “high risk” diagnosis; our estimates of frequency of transit service are larger for this subgroup. Next, we examine the depression screen score for respondents with a pre-lottery diagnosis of depression or anxiety and find no moderating effects from any domain of neighborhood characteristics for this subgroup. Complete results are presented in Table 14 in the Appendix.
Discussion
Neighborhood characteristics may themselves have important effects on health, but we find that they exert only limited moderating effects on the relationship between Medicaid coverage and health outcomes. These null results for multiple neighborhood domains have implications for health policy. Our results suggest that Medicaid coverage and a variety of neighborhood characteristics are not consistent substitutes or complements. Targeting Medicaid expansions based on neighborhood characteristics may successfully identify people who are eligible for coverage but appears to hold limited promise for amplified effectiveness through the interaction of health insurance coverage and neighborhoods. Absent compelling evidence of moderating effects, Medicaid expansions appear to be similarly effective across different neighborhoods.
That said, our results generate several intriguing hypotheses. First, our findings suggest that the mechanisms linking Medicaid coverage, neighborhood characteristics, and health do not conform to common narratives with simple policy prescriptions. For example, we find no evidence to support the hypothesis that insurance is much more effective in reducing blood sugar levels when new enrollees live in places with more grocery stores (Table 8 in the Appendix). Second, this study highlights some potentially important interactions where additional study may help illuminate complex pathways, such as the relationship between transit service and the effects of Medicaid on cardiovascular risk and obesity. Further study is needed to explore causal mechanisms.
Limitations
Our study has several limitations that highlight critical areas for future research. First, by exploiting the randomized lottery, we can identify the causal effects of Medicaid coverage; however, neighborhood characteristics are not similarly randomly assigned. As previously discussed, we cannot disentangle the direct moderating effects of neighborhood characteristics from the moderating effects of other factors associated with those neighborhoods or their residents.
Second, we examine the moderating effects of five domains of neighborhood characteristics (socioeconomic deprivation; food access; park access and green space; attributes that promote active living; and land use), but other area-related factors that were not considered in the analysis may be important, such as the supply of health services.
In addition, our analysis focuses on the effects of a Medicaid expansion on a low-income population in neighborhoods within Portland, Oregon. These estimates may not generalize to other people or locations with different residential or area characteristics, especially rural areas.
Other limitations may affect our ability to detect relatively small effects. For example, although we generally find statistically insignificant moderating effects of neighborhood characteristics, our confidence intervals are often wide enough to include effect sizes that might be clinically meaningful. In addition, we may not have a sufficient sample size to explore effects among subgroups such as those with specific preexisting health conditions. These limitations should be considered in future research using alternative empirical strategies.
Conclusion
There has been much speculation about the interaction between neighborhood characteristics and health insurance coverage in driving health outcomes. Using in-person survey data from the Oregon Health Insurance Experiment linked to information on neighborhood characteristics in Portland, OR, we evaluate the extent to which neighborhood characteristics moderate the causal effects of health insurance on physical health, mental health, and health-related quality of life. Overall, we find limited evidence that neighborhood characteristics influence the impacts of health insurance coverage. Understanding the interplay between neighborhoods and health insurance coverage can inform health policy to improve the effectiveness of future health insurance expansions.
References
Finkelstein A, Taubman S, Wright B, et al. The Oregon health insurance experiment: evidence from the first year. Q J Econ. 2012;127(3):1057–106.
Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment — effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–22.
Betancur J. Gentrification and community fabric in Chicago. Urban Stud. 2011;48(2):383–406.
Duncan DT, Kawachi I. Neighborhoods and Health. 2nd Edition. Oxford University Press; 2018.
Kawachi I, Berkman LF. Neighborhoods and Health. Oxford University Press; 2003.
Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Commun Health. 2001;55(2):111–22.
Ludwig J, Duncan GJ, Gennetian LA, et al. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337(6101):1505–10.
Ludwig J, Duncan GJ, Gennetian LA, et al. Long-term neighborhood effects on low-income families: evidence from moving to opportunity. Am Econ Rev. 2013;103(3):226–31.
Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes — a randomized social experiment. N Engl J Med. 2011;365(16):1509–19.
Dennett JM, Wright BJ, Cohen-Cline H, Baicker K. Connecting neighborhood characteristics and clinical health outcomes: novel data from the oregon health insurance experiment. Available at: https://ssrn.com/abstract=3582108. Accessed 21 Apr 2020.
Baicker K, Dennett J. Oregon health insurance experiment analysis plan: the moderating role of neighborhood characteristics. Available at: https://www.socialscienceregistry.org/trials/28 and https://www.nber.org/oregon/5.documents.html. Accessed 21 Apr 2020
D’Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care. Circulation. 2008;117(6):743–53.
Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Dis. 2009;114(1):163–73.
Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8 health survey. Lincoln, RI: QualityMetric Incorporated. 2001;15(10):5.
Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041–62.
Hoehner CM, Ivy A, Ramirez LKB, Handy S, Brownson RC. Active neighborhood checklist: a user-friendly and reliable tool for assessing activity friendliness. Am J Health Promot. 2007;21(6):534–7.
Acknowledgements
We are indebted to Bill J. Wright for data collection, support, and expertise, which were critical to this study, and we are grateful to the survey research team at CORE. We are also grateful to several anonymous reviewers for their helpful comments and suggestions, and to Haidong Lu for his statistical insights. Julia Dennett is additionally indebted to her advisors, David Cutler, Katherine Baicker, Thomas McGuire, and Ateev Mehrotra. We gratefully acknowledge funding for the Oregon Health Insurance Experiment from the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services; the California HealthCare Foundation; the John D. and Catherine T. MacArthur Foundation; the National Institute on Aging (P30AG012810, RC2AGO36631, and R01AG0345151); the Robert Wood Johnson Foundation; the Alfred P. Sloan Foundation; the Smith Richardson Foundation; and the Social Security Administration (5 RRC 08098400-03-00, to the National Bureau of Economic Research as part of the Retirement Research Consortium of the Social Security Administration); and by the Centers for Medicare and Medicaid Services. Julia Dennett acknowledges support from the National Science Foundation Graduate Research Fellowship Program (DGE1144152), the Agency for Healthcare Research and Quality (T32HS000055), the National Institute on Aging, Grant Number T32-AG000186, and a Harvard University GSAS Dissertation Completion Fellowship. The findings and conclusions expressed are solely those of the authors and do not represent the views of SSA, the National Institute on Aging, the National Institutes of Health, the Agency for Healthcare Research and Quality, the National Science Foundation, any agency of the Federal Government, any of our funders, or the NBER.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Dennett, J.M., Baicker, K. Medicaid, Health, and the Moderating Role of Neighborhood Characteristics. J Urban Health 99, 116–133 (2022). https://doi.org/10.1007/s11524-021-00579-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-021-00579-2