Abstract
The purpose of this study was to better understand residential segregation and child/youth health by examining the relationship between a measure of Black-White residential segregation, the index of dissimilarity, and a suite of child and youth health measures in 235 U.S. metropolitan statistical areas (MSAs). MSAs are urban areas with a population of 50,000 or more and adjacent communities that share a high degree of economic and social integration. MSAs are defined by the Office of Management and Budget. Health-related measures included child mortality (CDC WONDER), teen births (NCHS natality data), children in poverty (SAIPE program), and disconnected youth (Measure of America). Simple linear regression and two-level hierarchical linear regression models, controlling for income, total population, % Black, and census region, examined the association between segregation and Black health, White health, and Black-White disparities in health. As segregation increased, Black children and youth had worse health across all four measures, regardless of MSA total and Black population size. White children and youth in small MSAs with large Black populations had worse levels of disconnected youth and teen births with increasing segregation, but no associations were found for White children and youth in other MSAs. Segregation worsened Black-White health disparities across all four measures, regardless of MSA total and Black population size. Segregation adversely affects the health of Black children in all MSAs and White children in smaller MSAs with large Black populations, and these effects are seen in measures that span all of childhood. Residential segregation may be an important target to consider in efforts to improve neighborhood conditions that influence the health of families and children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The existence of racial and ethnic disparities in health outcomes, particularly in Black populations compared to other racial groups, has been widely documented. For example, compared to other racial/ethnic groups, Blacks have higher rates of infant mortality and preterm birth [1, 2]; they also have worse rates of cancer survival [3], lower life expectancy [2], lower rates of immunization, and higher rates of obesity and death from homicide [4]. Many factors have been implicated in these disparities including socioeconomic status, neighborhood poverty rate, institutional racism and discrimination, and differential access to new healthcare technologies. Recently, the effects of residential segregation have been postulated as an important community-level influence on health outcomes, and on the differences in outcomes among population groups [5, 6]. Segregation, considered a spatial manifestation of institutional discrimination, can be defined as the degree to which two or more groups live separately from one another in a geographic area [7]. Though segregation in US cities is not new or specific to any one racial/ethnic group, the history of Black-White residential segregation is unique. An understanding of the history of racist practices largely promulgated by Whites helps illuminate why Black-White residential segregation is an important measure of a historical process that has favored Whites and disadvantaged Blacks [8]. As articulated by Cutler et al. [8], in the early to mid-twentieth century, collective action racism helped construct and maintain segregated urban areas through laws (e.g., racial zoning), racially restrictive covenants (contracts that prohibited the sale or lease of property to Blacks), and planned overt acts of intimidation. Racial zoning and restrictive covenants were eventually outlawed, and a subtler decentralized racism took its place where Whites with the means and opportunities moved away from segregated urban areas to well-resourced neighborhoods.
Segregation can negatively impact health outcomes by exposing residents to lower housing quality [9, 10], concentrated poverty, and reduced access to economic and educational opportunities [9,10,11,12]. Patterns of segregation among Blacks in the U.S. remain the highest of all racial/ethnic groups, are more pronounced than economic segregation [13] and historically are less likely to be self-imposed than segregation that occurs among other racial/ethnic groups. For these reasons, the relationship of Black-White residential segregation to health must be better characterized to increase our understanding of the determinants of health disparities. So far, much of the research in this area has focused on infant or adult mortality. High levels of residential segregation appear to be related to worse outcomes for Black infants [14,15,16] and Black adults [17,18,19,20]. More recently, research inquiry has broadened to consider segregation’s effects on pregnancy. Here, again, segregation was usually associated with worse outcomes for Blacks [21,22,23,24]. There is some evidence, however, that segregation has no effect on or can be beneficial for Black health. [25,26,27,28] These discrepancies may be due to different measures of segregation, choice of geographic area in which segregation was measured and differences in consideration of covariates in the analysis.
Despite considerable research devoted to the effects of segregation on infant and adult health, there is a dearth of research describing the relationship between segregation and the health of children and youth, as well as potential disparities between Blacks and Whites for these age groups. It is well documented that early childhood experiences are important for healthy development, and that childhood health is important for adult socioeconomic achievement and health [29, 30]. Therefore, the purpose of this study was to examine the relationship between measures of Black-White residential segregation and a suite of child and youth health measures in U.S. metropolitan statistical areas (MSAs). We explored relationships between segregation and Black-White health disparities and differential associations by race. Our health measures included child mortality, teen births, child poverty, and disconnected youth, all important measures of child/youth health. Children born to teen mothers are more likely to be inactive, less likely to have high educational attainment and more likely to be poor [31]. Children in poverty have inadequate access to healthcare and have higher rates of hospital admissions and disability days [32]. Disconnected youth, like child poverty, is a proxy for the opportunities available to youth and young adults [33]. Disconnected youth are at an increased risk of violent behavior, smoking, alcohol consumption, and marijuana use and may have emotional deficits and less cognitive and academic skill, than their peers who are working and/or in school [34,35,36,37]. Elucidating whether residential segregation independently affects child or youth health may lend support to further research exploring how segregation specifically leads to adverse health outcomes and increase interest in interventions designed to reduce segregation and increase access to healthy neighborhoods in formative early life stages.
Materials and Methods
MSAs, as defined by the Office of Management and Budget, are areas comprised of at least one urban area with a population of 50,000 or more and adjacent communities that share a high degree of economic and social integration [38]. This level of geography was chosen because it is well suited to reflect the housing and labor markets that are responsible for creating patterns of segregation [39]; they also minimize selection bias, as forces operating to sort people into neighborhoods are weaker between metropolitan areas as opposed to within metropolitan areas [39]. Among the nation’s 382 MSAs, 11 are large enough to be further subdivided into 31 metropolitan divisions. To account for the size and variation in population and demographic characteristics of these large MSAs, metropolitan divisions were analyzed as if they were MSAs, resulting in a study sample of 402 MSAs.
The independent variable, MSA Black-White residential segregation, was operationally defined using the index of dissimilarity (D). D measures the evenness with which Blacks and Whites are distributed across the census tracts that make up MSAs. In the current study, D can be thought of as the percentage of the population that would have to move so that each census tract would have the same proportion of Black and White residents as the MSA overall. The index has a range from 0 to 1, with 1 reflecting complete segregation and 0 representing complete integration. While other measures of residential segregation were considered, D was chosen for several reasons, including precedent in the literature set [14,15,16,17,18, 20], to facilitate comparison to previous studies, and the ability to control for demographic covariates without affecting the integrity of the measure. These data were calculated at the census tract level using 2011–2015 data from the U.S. Census, American Community Survey and aggregated up to the MSA level.
Child heath was approximated with the following four health-related measures: child mortality, teen births, children in poverty, and disconnected youth. Child mortality data, the all-cause mortality per 100,000 population for those under age 18, were obtained from CDC WONDER for years 2011–2015. Four hundred and two individual queries were run, summing the deaths and population for each MSA’s constituent counties to obtain an age- and race-specific mortality rate estimate at the MSA level. Teen birth data at the MSA level were obtained through a custom calculation of individual level NCHS natality data by diversitydatakids.org. Teen births are defined as the percent of live births from 2011 to 2013 to mothers under age 20 from the demographic group of interest. Children in poverty is the percentage of children under age 18 living in poverty, calculated from data provided by the Small Area Income and Poverty Estimates (SAIPE) program for years 2011–2015. Poverty levels are defined each year by the federal Department of Health and Human Services using a set of income thresholds that vary by family size and composition. If a family’s income is less than their calculated threshold, then every individual in that family is considered in poverty. SAIPE provided the number of children in poverty at the county level, which was combined with county level total child population obtained from 2015 Census Population Estimates and aggregated up to the MSA level. Disconnected youth are defined as the percentage of teens and young adults ages 16–24 who are neither working nor in school. This measure is a Measure of America calculation of 2012–2015 U.S. Census, American Community Survey data at the Public Use Microdata Area level, aggregated up to the MSA level. All data were obtained by race for non-Hispanic White and Black children, except for children in poverty, where the data for Black children include those with Hispanic ethnicity. The disparity between Black and White child or youth health was calculated as the difference between Black and White health outcome values.
Several MSA level covariates were used in our model including: MSA median income, MSA total population, percent of MSA population that is Black, and MSA census region. Median income data at the county level for 2015 was provided by the Census Bureau’s SAIPE program. MSA level median income was calculated by population weighting the median incomes for each MSA’s constituent counties. MSA total population and proportion of MSA population that is Black were obtained from Census Population Estimates. MSAs were assigned to census regions, as defined by the U.S. Census Bureau, with those MSAs spanning multiple regions being assigned to the census region in which the majority of their population resided.
Analysis
To ensure our segregation measure had adequate reliability, we limited our sample to those MSAs with at least 10,000 Black residents. We also excluded MSAs with missing data for any relevant measures, which brought our analytic sample to 235 MSAs. Data were analyzed for normality, and MSA total population and MSA median income required log transformation. Descriptive statistics were calculated for our analytic sample and are presented as median (interquartile range). Three sets of OLS regression and two-level hierarchical linear regression were used to examine the association between Black-White residential segregation and White health, Black health, and the Black-White health disparity. Model 1, the base model, regressed the four health measures on residential segregation without adjustment for potential confounders. Model 2, the full model, was a hierarchical linear regression model that allowed for a random intercept by census region and included MSA total population and the proportion of the population that is Black as level one confounders. Socioeconomic factors, such as income, education, and employment, were postulated to serve as mediators, rather than confounders, to the relationship between residential segregation and health; thus, we did not want to control away the effect of segregation by including such factors in the full model. Therefore, model 3, included as a supplement, explores adding MSA level median household income to model 2 to investigate and provide evidence to support this assumption. Effect modification by MSA total population size and Black population size were hypothesized and found to affect the association between segregation and White child health, so models were stratified by these variables using the MSA median population (490,888 residents) and percentage of Black residents (12.97%). All analyses were done using SAS 9.4 (Cary, NC).
Results
To better understand the characteristics of the MSAs and the health of the population within them, descriptive statistics were calculated (Table 1). Among the MSAs included in our sample, residential segregation, as measured by D, had a median value of 0.53, with an interquartile range of 0.45–0.60. The largest proportion of MSAs were in the South census region (52%). This was also true of the large MSA (40%) and small MSA (64%) subgroups. Large MSAs appeared to have a higher median income, a smaller median proportion of Black residents and be more evenly spread throughout census regions. Examples of D for MSAs in our analysis include highly segregated MSAs like Milwaukee-Waukesha-West Allis, WI (0.81) and Muskegon, MI (0.75) to much less segregated MSAs like Las Vegas-Henderson-Paradise, NV (0.34) and Hinesville, GA (0.24). Across all MSA population size categories, values for health measures appear to be much worse for Black children than White children, with many outcomes being at least twice as bad. Additionally, small MSAs appeared to have worse values for all four of the child health measures: disconnected youth, child mortality, teen births, and child poverty.
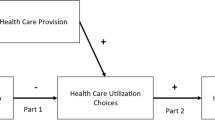
We then examined the relationship between residential segregation within MSAs and child/youth health, among Whites and Blacks, respectively. Table 2 displays effect estimates for White children stratified by MSA total population size and Black population size, because these factors were found to be effect modifiers. In the unadjusted base model (model 1), residential segregation appeared to be beneficial to White disconnected youth in large MSAs with small Black populations and detrimental to White teen birth rate in small MSAs with a large Black population. However, in the full model (model 2), increasing D was only associated with White child and youth health measures in small MSAs with large Black populations. These associations were characterized by higher percentages of disconnected youth and teen births (Fig. 1) and a nearly statistically significant increase in the percentage of children in poverty (p = 0.05). No statistically significant associations between segregation and White child and youth health measures were found in other MSA types.
Analyses of health measures for Black child and youth and Black-White health disparities were not stratified by MSA total population size and Black population size, because these factors were not found to be effect modifiers as they were for White child and youth health. In other words, the effects of residential segregation on Black child and youth health and Black/White health disparities were similar across MSA types. Regarding Black child and youth health (Table 3), apart from child mortality, all outcomes were worse with higher residential segregation in model 1. In the full model, the association between higher residential segregation and worse health grew stronger and the association for child mortality became statistically significant (model 2). Similarly, Black-White health disparities were consistently worse as segregation increased, but across all four measures in both models (Table 4). In our unadjusted model, disparities increased for all child and youth health measures as residential segregation increased. Adjustment for confounders in model 2 attenuated some of the associations, but all remained statistically significant.
Discussion
The purpose of this study was to examine the differential effects of residential segregation on child and youth health by race, as well as the disparities in health measures by race. Our findings suggest that Black-White residential segregation may have an adverse effect on the health of both Black and White children and youth. Higher residential segregation was strongly associated with worse health for Black children and youth across all four health measures. For White children and youth, the effect of higher levels of segregation was not as strong or consistent and may depend on the MSA characteristics in which they reside.
Consistent with the majority of research on this topic, our study found that measures of Black child and youth health were significantly worse as residential segregation increased. This was true for all four health measures. These results were not surprising, as many studies have documented segregation’s detrimental effects on Black health outcomes, including infant mortality [14,15,16], adult mortality [17,18,19,20], and birth outcomes [21,22,23]. This study further solidifies the evidence that higher residential segregation is associated with worse Black health by adding novel evidence from children. Notably, these associations remained statistically significant in our mediator model (model 3, Supplement), suggesting socioeconomic status is not the only means through which segregation exerts its detrimental effect. Research has investigated other possible mediators including residential segregation’s effects on the built environment of neighborhoods, [40,41,42] healthcare quality [43,44,45,46], or environmental exposures [47, 48]. Further research is required to examine the relative contributions of these different pathways to health outcomes, as well as investigating other possible factors, such as gender, baseline health status, or developmental stage/age.
For White children and youth, segregation may have a differential effect on health depending on the characteristics of the MSA. White children and youth in smaller MSAs with larger Black populations had more disconnected youth, higher teen birth rate and more children in poverty as segregation increased. This effect was not seen in other MSA types, where residential segregation showed no association in the full adjusted models. Segregation adversely affecting White children’s health in small MSAs with large Black populations is a novel finding that is inconsistent with the majority of residential segregation and health literature, where higher residential segregation is usually not found to be associated with worse health outcomes in Whites [14, 18, 22, 49, 50]. Why the health of White children and youth is worse in small MSAs with large Black populations is unclear and warrants further exploration. Kramer and Hogue [9] observed that, when an adverse effect of segregation on White health outcomes is found, it usually involves poor Whites living in mostly Black neighborhoods. This could be the case for the White children and youth in the current study; however, we have no information about the neighborhood- or individual-level characteristics of our sample.
Disparities in health measures between Black and White children and youth all increased as residential segregation increased, suggesting that there is a significant independent effect of residential segregation on the large disparities seen between Black and White health measures. In the residential segregation and health literature, there is less research on using disparities as the outcome measure as opposed to absolute outcome measures. However, the research that does examine disparities in outcomes has found a similar increase in Black-White health disparities as residential segregation increases [16, 21].
This study adds to a small, but growing body of evidence linking residential segregation to poor health in childhood and adolescence. The “suite” of child and youth health measures we chose (teen birth rate, children in poverty, child mortality, and disconnected youth) gives a more complete picture of segregation’s effects on health throughout life stages of child and youth development, from how likely a child is to be born to a teenage mother to how likely they are to have a job or be in school when they are an adult. This suite of health measures, combined with a large analytic sample of 235 MSAs, helped us elucidate segregation’s effects in a broader and more powerful manner.
Several limitations to our study design should also be noted. Because the study employs a cross-sectional ecologic study design, one must be careful in interpreting the results of our study as causal or assume our results can be applied to any individual children. Additionally, our cross-sectional design was not able to measure cumulative exposure to segregation over time and only provides a one-time “snapshot” of the level of segregation and child and youth health in an MSA. Because the effects of segregation on health are hypothesized to work across the life course, future research should attempt to quantify cumulative exposure to segregation and prospective health outcomes. Finally, the use of MSAs as the geographic unit of analysis does not allow examination of within-MSA, neighborhood-level, or individual-level effects of segregation, which may act by unique pathways not captured in an inter-MSA analysis. For example, some research suggests that high levels of neighborhood segregation can protect against experiences of discrimination [51], increase social support, and political power for residents of these communities [52, 53]. These interpersonal effects may be overlooked in studies that use larger geographic areas like MSAs as their unit of analysis.
Our study expands the field of residential segregation and health research by focusing on children and youth, a window of early development that has not been adequately studied. We found that segregation adversely affects the health of Black children and youth, as well as White children and youth in certain MSAs, and these effects are seen in measures that span all of child and youth development. This finding runs counter to what often is hypothesized about segregation that segregation will benefit White residents by concentrating social and economic resources in their neighborhoods. It seems that, instead, there may be some harmful aspects of segregation, or the historical processes that brought about segregation, that affect both Black and White children and youth.
Our results suggest that the effects of segregation may exist throughout childhood into early adulthood, offering multiple timepoints for interventions aimed at providing children with healthy neighborhoods in which they can live. But what exactly those interventions should be is still unknown. One must not too quickly presume the best answer is affording families the ability to move to less impoverished communities. Evidence from the Moving to Opportunity trial suggests individuals may be reluctant to move and break the social connections they have established [54]. Further, if they do move, they may still end up in segregated communities that are disadvantaged relative to their more integrated counterparts. Clearly, a more nuanced approach is needed to address such a complex problem; consequently, many experts in this field promote an expansion of what is considered “health policy,” so that interventions like housing mobility programs, increased enforcement of housing antidiscrimination laws, and neighborhood level healthy infrastructure projects are viewed, in part, as public health initiatives [55]. This expansion in health policy’s scope could help public and population health officials justify needed collaboration with colleagues in other sectors, especially those in housing policy. There are already opportunities for collaboration. For example, some state and local governments are seeking to define and identify “opportunity neighborhoods” for their housing assistance programs (e.g., Baltimore Regional Housing Campaign). Our research suggests that it may be wise to incorporate measures of segregation into these community assessments, though further study is needed to identify which measures of segregation and at what level of geographic analysis would be most appropriate. Incorporating residential segregation into these program assessments could inform community development projects that are intended to improve community conditions that support stable and healthy families and foster inclusive neighborhoods with strong social capital.
References
Rossen LM, Schoendorf KC. Trends in racial and ethnic disparities in infant mortality rates in the United States, 1989–2006. Am J Public Health. 2014;104(8):1549–56.
National Center for Health S. Health, United States. In: Health, United States, 2015: with special feature on racial and ethnic health disparities. Hyattsville (MD): National Center for Health Statistics (US), 2016.
Zeng C, Wen W, Morgans AK, Pao W, Shu X-O, Zheng W. Disparities by race, age, and sex in the improvement of survival for major cancers. JAMA Oncology. 2015;1(1):88–96.
Centers for Disease Control and Prevention U. Health disparities experienced by black or African Americans—United States. MMWR: Morb Mortal Wkly Rep. 2005;54(1):1–3.
Diez Roux AV. Neighborhoods and health: where are we and were do we go from here? Rev Epidemiol Sante Publique. 2007;55(1):13–21.
Kawachi I, Berkman LF. Neighborhoods and health: Oxford, UK: Oxford University Press; 2003.
Massey DS, Denton NA. The dimensions of residential segregation. Social Forces. 1988;67(2):281–315.
Cutler David M, Glaeser Edward L, Vigdor Jacob L. The rise and decline of the American ghetto. J Polit Econ. 1999;107(3):455–506.
Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31(1):178–94.
Williams DR. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–16.
Schulz AJ, Williams DR, Israel BA, Lempert LB. Racial and spatial relations as fundamental determinants of health in Detroit. The Milbank Quarterly. 2002;80(4):677–707.
Mays VM, Cochran SD, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annu Rev Psychol. 2007;58(1):201–25.
Massey DS, Rothwell J, Domina T. The changing bases of segregation in the United States. Ann Am Acad Polit Soc Sci. 2009;626(1):74–90.
Bird ST. Separate black and white infant mortality models: differences in the importance of structural variables. Soc Sci Med. 1995;41(11):1507–12.
Polednak AP. Black-white differences in infant mortality in 38 standard metropolitan statistical areas. Am J Public Health. 1991;81(11):1480–2.
LaVeist TA. Segregation, poverty, and empowerment: health consequences for African Americans. The Milbank Quarterly. 1993;71:41–64.
Collins CA. Racism and health: segregation and causes of death amenable to medical intervention in major U.S. cities. Ann N Y Acad Sci. 1999;896(1):396–8.
Hart KD, Kunitz SJ, Sell RR, Mukamel DB. Metropolitan governance, residential segregation, and mortality among African Americans. Am J Public Health. 1998;88(3):434–8.
Jackson SA, Anderson RT, Johnson NJ, Sorlie PD. The relation of residential segregation to all-cause mortality: a study in black and white. Am J Public Health. 2000;90(4):615–7.
Polednak AP. Poverty, residential segregation, and black/white mortality ratios in urban areas. J Health Care Poor Underserved. 1993;4(4):363–73.
Osypuk TL, Acevedo-Garcia D. Are racial disparities in preterm birth larger in Hypersegregated areas? Am J Epidemiol. 2008;167(11):1295–304.
Ig E. Is segregation bad for your health? The case of low birth weight [with comments]. Brookings-Wharton Papers on Urban Affairs. 2000;203
Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med. 2006;63(12):3013–29.
Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med. 2006;63(12):3030–45.
Masi CM, Hawkley LC, Harry Piotrowski Z, Pickett KE. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Soc Sci Med. 2007;65(12):2440–57.
Fang J, Madhavan S, Bosworth W, Alderman MH. Residential segregation and mortality in New York City. Soc Sci Med. 1998;47(4):469–76.
Hutchinson RN, Putt MA, Dean LT, Long JA, Montagnet CA, Armstrong K. Neighborhood racial composition, social capital and black all-cause mortality in Philadelphia. Soc Sci Med. 2009;68(10):1859–65.
Inagami S, Borrell LN, Wong MD, Fang J, Shapiro MF, Asch SM. Residential segregation and Latino, Black and White mortality in New York City. J Urban Health. 2006;83(3):406–20.
Acevedo-Garcia D, McArdle N, Osypuk T, Lefkowitz B, Krimgold B. Children left behind. Boston, MA: Center for Advancement of Health at Harvard School of Public Health;2007.
Phillips DA, Shonkoff JP. From neurons to neighborhoods: the science of early childhood development: Washington, DC: National Academies Press; 2000.
Francesconi M. Adult outcomes for children of teenage mothers. Scand J Econ. 2008;110(1):93–117.
Wood D. Effect of child and family poverty on child health in the United States. Pediatrics. 2003;112(3 Part 2):707–11.
Lewis K, Burd-Sharps S. Zeroing in on place and race. Brooklyn, NY: Measure of America, 2015.
Besharov DJ, Gardiner KN. Preventing youthful disconnectedness. Child Youth Serv Rev. 1998;20(9):797–818.
Tandon SD, Marshall B, Templeman AJ, Sonenstein FL. Health access and status of adolescents and young adults using youth employment and training programs in an urban environment. J Adolesc Health. 43(1):30–7.
Vancea M, Utzet M. How unemployment and precarious employment affect the health of young people: a scoping study on social determinants. Scand J Public Health. 2017;45(1):73–84.
Morrell SL, Taylor RJ, Jobless KCB. Unemployment and young people’s health. Med J Aust. 1998;168(5):236–40.
Office of Management and Budget. 2010 standards for delineating metropolitan and micropolitan statistical areas. Fed Regist. 2010;75(23):37245–52.
Osypuk TL, Galea S. What level macro? Choosing appropriate levels to assess how place influences population health. In: Macrosocial determinants of population health. p. 399–435.
Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med. 2007;33(4, Supplement):S240–5.
Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: a national study. Am J Public Health. 2006;96(9):1676–80.
Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44(3):189–95.
Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94(8):666–8.
Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575–84.
Lurie N, Buntin MB. Health disparities and the quality of ambulatory care. N Engl J Med. 2002;347(21):1709–10.
Smith DB, Feng Z, Fennell ML, Zinn JS, Mor V. Separate and unequal: racial segregation and disparities in quality across U.S. nursing homes. Health Aff. 2007;26(5):1448–58.
Morello-Frosch R, Shenassa ED. The environmental ‘riskscape’ and social inequality: implications for explaining maternal and child health disparities. Environ Health Perspect. 2006;114(8):1150–3.
Morello-Frosch R, Lopez R. The riskscape and the color line: examining the role of segregation in environmental health disparities. Environ Res. 2006;102(2):181–96.
Chang VW. Racial residential segregation and weight status among US adults. Soc Sci Med. 2006;63(5):1289–303.
Bower KM, Thorpe RJ, Yenokyan G, McGinty EEE, Dubay L, Gaskin DJ. Racial residential segregation and disparities in obesity among women. J Urban Health. 2015;92(5):843–52.
Hunt MO, Wise LA, Jipguep M-C, Cozier YC, Rosenberg L. Neighborhood racial composition and perceptions of racial discrimination: evidence from the black women’s health study. Soc Psychol Q. 2007;70(3):272–89.
LaVeist TA. Segregation, poverty, and empowerment: health consequences for African Americans. The Milbank Quarterly. 1993;71(1):41–64.
LaVeist TA. The political empowerment and health status of African-Americans: mapping a new territory. Am J Sociol. 1992;97(4):1080–95.
Clampet-Lundquist S, Massey Douglas S. Neighborhood effects on economic self-sufficiency: a reconsideration of the moving to opportunity experiment. Am J Sociol. 2008;114(1):107–43.
Acevedo-Garcia D, Osypuk TL, McArdle N, Williams DR. Toward a policy-relevant analysis of geographic and racial/ethnic disparities in child health. Health Aff. 2008;27(2):321–33.
Acknowledgments
This project was financially sponsored by the University of Wisconsin School of Medicine and Public Health, the Herman and Gwendolyn Shapiro Foundation, and the University of Wisconsin Department of Population Health Sciences. The sponsor played no role in the study design; in the collection, analysis, and interpretation of the data; in the writing of the article; or in the decision to submit it for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Kotecki, J.A., Gennuso, K.P., Givens, M.L. et al. Separate and Sick: Residential Segregation and the Health of Children and Youth in Metropolitan Statistical Areas. J Urban Health 96, 149–158 (2019). https://doi.org/10.1007/s11524-018-00330-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-018-00330-4