Abstract
We assessed socio-structural and behavioral correlates of preexposure prophylaxis (PrEP) for HIV infection among a sample of high-risk HIV-negative men who have sex with men (MSM) in Los Angeles, California. Participants from an ongoing 5-year prospective cohort study investigating the direct impacts of substance use on HIV transmission dynamics were enrolled between February 2015 and January 2017. All men completed a computer-assisted self-interview every 6 months that assessed recent (past 6 months) PrEP use and socio-structural and behavioral factors. Of the total 185 MSM (mean age = 29 years) included in the study, majority were African American (40%) or Hispanic (41%) and reported current health insurance coverage (80%). In multivariable analysis using log-binomial regression, having health insurance coverage [adjusted prevalence ratio (aPR) 2.02; 95% confidence interval (CI) 1.01 to 4.01, p = 0.04] was associated with recent PrEP use. Unstable housing (aPR = 0.44, 95% CI 0.22 to 0.90, p = 0.02) was associated with lower PrEP use. Behavioral factors associated with recent PrEP use include sex with a HIV-positive partner (aPR = 3.63, 95% CI 1.45 to 9.10, p = 0.01), having six or more sex partners (aPR = 2.20, 95% CI 1.26 to 3.82, p = <0.01), and popper use (aPR = 2.76, 95% CI 1.58 to 4.84, p = <0.01). In this sample of predominantly racial/ethnic minority MSM, socio-structural and behavioral factors were important factors associated with recent PrEP use. These findings provide considerations for intervention development to promote PrEP use among key groups of MSM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men who have sex with men (MSM) remain disproportionately affected by HIV infection in the United States. Despite representing between 2 and 3% of the United States population, MSM accounted for 67% of new HIV diagnosis in 2015 [1]. High HIV infection rates among MSM have necessitated the development of more effective HIV prevention tools. Preexposure prophylaxis (PrEP) is a recent biomedical HIV prevention strategy that involves HIV-negative individuals taking antiretroviral medication prior to HIV exposure to prevent HIV infection. It has demonstrated safety and efficacy in reducing HIV acquisition among MSM and other high-risk groups [2,3,4].
Research assessing actual PrEP use is evolving; studies suggest low PrEP use among MSM with rates ranging from 1.5 to 12% [5,6,7,8,9,10,11,12], with one study reporting a prevalence rate as high as 23% [13]. Prior studies have identified barriers to PrEP use including high cost, concerns about side effects, accessibility, and lack of knowledge [12, 14]. There are also concerns that PrEP use may be associated with increased HIV sexual risk behaviors [14, 15]. However, data on socio-structural factors including income, unstable housing, and internalized homonegativity and their association with PrEP use have not being thoroughly described. The aim of this analysis was to understand the socio-structural and behavioral correlates of PrEP use among a sample of high-risk HIV-negative MSM in Los Angeles.
Methods
Participants
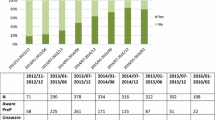
The Men who have sex with Men & Substance Use Cohort at UCLA Linking Infections, Noting Effects (mSTUDY) is an ongoing 5-year prospective cohort study measuring factors linked to substance use and HIV transmission dynamics for HIV-positive and HIV-negative male-identified MSM in Los Angeles. The mSTUDY is focused on enrolling Black/African American and Latino/Hispanic MSM between 18 and 45 years of age who were born male. In addition, HIV-negative MSM were eligible if they reported unprotected anal intercourse with a man in the past 6 months. Participants in the mSTUDY return every 6 months for physical examinations, laboratory testing, and completion of a survey collecting sociodemographic, psychosocial, and behavioral data. All behavioral questions were assessed using computer-assisted self-interview (CASI). The current analysis includes data from 185 HIV-negative MSM enrolled in the mSTUDY between February 2015 and January 2017. The mSTUDY protocols confirmed HIV-negative status at enrollment via rapid HIV antibody test. The UCLA Institutional Review Boards approved the mSTUDY protocols, and all participants provided informed consent.
Measures
The survey included questions about participant’s age, racial/ethnicity status, sexual orientation, current employment status, current insurance status, and annual income. ‘Outness’ was measured with the question “Who have you told that you have sex with men?.” Five dichotomous (not mutually exclusive) variables were created from their response to indicate being out to doctors, family members, their priest, straight friends, and work colleagues. To measure internalized homonegativity, we used an adapted measure originally developed by Herek et al. [16]. Participants indicated their level of agreement with nine statements (such as, “I wish I were not gay/bisexual/attracted to men”) using a five-point Likert scale. Response options for each item ranged from 1 = strongly disagree to 5 = strongly agree. Scores were summed and ranged from 9 to 45, with higher scores indicating greater internalized homonegativity. The survey also asked about sexual behaviors in the past 6 months, history of sexually transmitted infections (STI), and substance use in the past 6 months. PrEP use was assessed by self-reported recent (past 6 months) use of an anti-HIV medication. Participants who reported to have taken PrEP or both PrEP and postexposure prophylaxis were classified as recent PrEP users.
Data Analyses
We used Chi-square or Fisher’s exact tests to compare the distributions of sociodemographic, psychosocial, and behavioral characteristics by recent PrEP use. We performed multivariable log-binomial regression models on data from all available participant study visits using generalized estimating equations. The final multivariable model included variables previously associated with PrEP use [11, 12] and variables significant (p < 0.10) in the bivariable analyses. We also adjusted for participant enrollment, because some mSTUDY participants were enrolled from a prior study facilitating PrEP use.
Results
Sample Characteristics
The current study includes data from 185 HIV-negative MSM who contributed 429 person-visits. The mean age of the sample was 29 years [standard deviation (SD) = 6.5] (Table 1). Most participants were African American (40%) or Hispanic (41%), reported current health insurance coverage (80%), and earned $9, 999 or less in annual income (57%).
Bivariable Associations
In bivariable analysis, participants who reported recent PrEP use compared to non-PrEP users were significantly more likely to have been enrolled in a prior study facilitating PrEP use (27 vs. 6.9%; p = <0.01), to have inhaled poppers in the past 6 months (56.8 vs. 24.8%; p = <0.01), to have reported anal sex with six or more partners in the past 6 months (48.6 vs. 24.1%; p = <0.01), and to be ‘out’ to both their doctor (97.2 vs. 74.8%; p = <0.01) and colleagues (85.7 vs. 62.4%; p = <0.01). Recent PrEP users were also less likely to have slept in a place not designed for sleep (10.8 vs. 29.7%; p = <0.01) than non-PrEP users. There was no significant difference in levels of internalized homonegativity and recent PrEP use.
Correlates of Recent PrEP Use in Multivariable Analyses
In the multivariable model (Table 2), those with current health insurance had significantly greater prevalence of recent PrEP use compared to those with no health coverage (adjusted prevalence ratio [aPR] = 2.02, 95% confidence interval [CI] 1.01 to 4.01; p = 0.04). Participants with annual income > $30,000 compared to those who made <$9, 999 were significantly more likely to report recent PrEP use (aPR = 2.56, 95% CI 1.15 to 5.69; p = 0.02). The men who reported sleeping in a place not designed for sleep were less likely to report recent PrEP use (aPR = 0.44, 95% CI 0.22 to 0.90; p = 0.02). Having sex with six or more anal sex partners in the past 6 months compared to less than five anal sex partners was significantly associated with greater prevalence of recent PrEP use (aPR = 2.20, 95% CI 1.26 to 3.82; p = <0.01). Sex with a HIV-positive partner compared to sex with a HIV-negative/unknown status partners was also associated with greater prevalence of recent PrEP use (aPR = 3.63, 95% CI 1.45 to 9.10; p = 0.01). Finally, the men who reported popper use in the past 6 months had a higher prevalence of recent PrEP use compared to those who had not used poppers (aPR = 2.76, 95% CI 1.58 to 4.84; p = <0.01). No other substance use variables were significantly associated with PrEP use.
Discussion
In this sample of predominantly high-risk HIV-negative MSM in the Los Angeles area, indicators of higher socio-structural status including having health insurance, greater annual income, and having a stable place to sleep were positively associated with recent PrEP use. Also, practice of behaviors such as many anal sex partners, sex with a HIV-positive partner, and popper use was associated with greater prevalence of PrEP use.
Prior studies have documented associations between higher income [14] and health insurance coverage [17] as facilitators of PrEP use. Our study also found that sleeping in a place not designed for sleep—an indicator of unstable housing—was associated with lower rates of recent PrEP use. Collectively, these findings emphasize that stable structural factors of health are key to PrEP access in this group. Yet, in this group nearly 80% had health insurance, which suggests those without coverage, as those whose survival needs trump those over their sexual health, limiting access for low-income and uninsured MSM to PrEP services. Manufacturer medication assistance programs [18]—which provide support for medication costs and co-pays for PrEP—may help to minimize cost barriers to PrEP access. But these findings signal that, even with assistance, many low-income and uninsured MSM are simply not able or not interested in accessing PrEP.
In our study, we did not find a significant association between internalized homonegativity and recent PrEP use. One prior study found that higher levels of internalized homonegativity were significantly associated with increased PrEP use [5]. However, because it has been suggested that higher levels of internalized homonegativity can manifest as reduced self-worth and self-care and thus diminished motivations to use PrEP [19], links between internalized homonegativity and PrEP use warrant further investigation.
We also found that elevated individual risk behaviors, such as many male anal sex partners and sex with an HIV-positive partner, were significantly associated with greater PrEP use. This is consistent with prior research [12] and indicates that those MSM on PrEP are precisely the group that would most likely benefit from prophylaxis. Interestingly, poppers emerged as the only substance use significantly associated with PrEP use. While we have no data on this, it is possible that poppers are being used to enhance pleasure during receptive anal sex. Popper use has also been associated with increased practice of behaviors that enhance risk of HIV exposure, such as condomless anal sex [20]. Thus, the men who reported using poppers and high individual risk behaviors for HIV exposure perceived themselves at elevated risk for HIV and engaged in PrEP. Therefore, these correlates of recent PrEP use identified in our study provide direction for intervention development to increase PrEP uptake among MSM with low income and unstable housing.
Our study has some limitations. The data are correlational and cannot assess causality. These analyses do not include specific sexual risk behaviors linked to HIV transmission (e.g., condomless anal sex with serodiscordant or unknown serostatus partners) that are criteria for PrEP eligibility [12]. It is possible that there is some misclassification of PrEP use because we relied on self-reports. Finally, the recruitment of some men from a prior study facilitating PrEP use may have inflated our rates of PrEP use in this population.
Conclusion
In summary, in this sample of predominantly racial/ethnic minority MSM, we found that socio-structural factors such as health insurance coverage, greater income, and stable housing were important factors that were associated with PrEP use. Interventions that address these factors may help enhance PrEP use.
References
Centers for Disease Control and Prevention. HIV Surveillance Report, 2015. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed February 10, 2017.
Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. doi:10.1056/NEJMoa1011205.
Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. doi:10.1056/NEJMoa1108524.
Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9. doi:10.1016/S1473-3099(14)70847-3.
Eaton LA, Matthews DD, Driffin DD, et al. A multi-US city assessment of awareness and uptake of pre-exposure prophylaxis (PrEP) for HIV prevention among Black men and transgender women who have sex with men. Prev Sci Off J Soc Prev Res. January 2017; doi:10.1007/s11121-017-0756-6.
Adams JW, Shinefeld J, Brady KA. Acceptability of oral preexposure prophylaxis among men who have sex with men in Philadelphia. J Acquir Immune Defic Syndr 1999. 2016;73(3):e62–5. doi:10.1097/QAI.0000000000001139.
Rucinski KB, Mensah NP, Sepkowitz KA, Cutler BH, Sweeney MM, Myers JE. Knowledge and use of pre-exposure prophylaxis among an online sample of young men who have sex with men in New York City. AIDS Behav. 2013;17(6):2180–4. doi:10.1007/s10461-013-0443-y.
Strauss BB, Greene GJ, Phillips G, et al. Exploring patterns of awareness and use of HIV pre-exposure prophylaxis among young men who have sex with men. AIDS Behav. July 2016; doi:10.1007/s10461-016-1480-0.
Gupta S, Lounsbury DW, Patel VV. Low awareness and use of preexposure prophylaxis in a diverse online sample of men who have sex with men in New York City. J Assoc Nurses AIDS Care. 2017;28(1):27–33. doi:10.1016/j.jana.2016.10.001.
Khanna AS, Michaels S, Skaathun B, et al. Preexposure prophylaxis awareness and use in a population-based sample of young Black men who have sex with men. JAMA Intern Med. 2016;176(1):136–8. doi:10.1001/jamainternmed.2015.6536.
Snowden JM, Chen Y-H, McFarland W, Raymond HF. Prevalence and characteristics of users of pre-exposure prophylaxis (PrEP) among men who have sex with men, San Francisco, 2014 in a cross-sectional survey: implications for disparities. Sex Transm Infect. 2016:sextrans-2015-052382. doi:10.1136/sextrans-2015-052382.
Holloway IW, Dougherty R, Gildner J, et al. Brief report: PrEP uptake, adherence, and discontinuation among California YMSM using geosocial networking applications. J Acquir Immune Defic Syndr 1999.2017; 74(1):15–20. doi:10.1097/QAI.0000000000001164.
Hood JE, Buskin SE, Dombrowski JC, et al. Dramatic increase in preexposure prophylaxis use among MSM in Washington state. AIDS Lond Engl. 2016;30(3):515–9. doi:10.1097/QAD.0000000000000937.
Brooks RA, Kaplan RL, Lieber E, Landovitz RJ, Lee S-J, Leibowitz AA. Motivators, concerns, and barriers to adoption of preexposure prophylaxis for HIV prevention among gay and bisexual men in HIV-serodiscordant male relationships. AIDS Care. 2011;23(9):1136–45. doi:10.1080/09540121.2011.554528.
Pérez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of PrEP uptake among racially/ethnically diverse young men who have sex with men: the P18 study. AIDS Educ Prev Off Publ Int Soc AIDS Educ. 2015;27(2):112–25. doi:10.1521/aeap.2015.27.2.112.
Herek GM, Cogan JC, Gillis JR, Glunt EK. Correlates of internalized homophobia in a community sample of lesbians and gay men. J Gay Lesbian Med Assoc. 1998;2:17–26.
Arnold T, Brinkley-Rubinstein L, Chan PA, et al. Social, structural, behavioral and clinical factors influencing retention in pre-exposure prophylaxis (PrEP) care in Mississippi. PLoS One. 2017;12(2):e0172354. doi:10.1371/journal.pone.0172354.
Truvada® for PrEP Medication Assistance Program. http://www.gilead.com/responsibility/us-patient-access/truvada%20for%20prep%20medication%20assistance%20program. Accessed March 28, 2017.
Garcia J, Parker C, Parker RG, Wilson PA, Philbin M, Hirsch JS. Psychosocial implications of homophobia and HIV stigma in social support networks: insights for high-impact HIV prevention among Black men who have sex with men. Health Educ Behav. 2016;43(2):217–25. doi:10.1177/1090198115599398.
Plankey MW, Ostrow DG, Stall R, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. J Acquir Immune Defic Syndr 1999. 2007;45(1):85–92. doi:10.1097/QAI.0b013e3180417c99.
Acknowledgements
We are grateful to the participants for contributing their time in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Institutional Review Boards at the University of California, Los Angeles, approved the study.
Funding
This work was supported by the National Institute on Drug Abuse grant U01DA036267, the MStudy (PI: Gorbach, Shoptaw); the UCLA Postdoctoral Fellowship Training Program in Global HIV Prevention Research grant T32MH080634 (PI: Currier, Gorbach); and the Center for HIV Identification, Prevention, and Treatment Services NIMH grant PS30 MH58107. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Rights and permissions
About this article
Cite this article
Okafor, C.N., Gorbach, P.M., Ragsdale, A. et al. Correlates of Preexposure Prophylaxis (PrEP) Use among Men Who Have Sex with Men (MSM) in Los Angeles, California. J Urban Health 94, 710–715 (2017). https://doi.org/10.1007/s11524-017-0172-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-017-0172-z