Abstract
Persons who inject drugs (PWID) are at risk for adverse health outcomes as a result of their drug use, and the resulting social stigma makes this a difficult population to reach for interventions aimed at reducing morbidity and mortality. During our study of adult PWID aged ≤40 years living in San Diego during 2009 and 2010, we compared three different sampling methods: respondent-driven sampling (RDS), venue-based sampling at one syringe exchange program (SEP), and street-based outreach. We compared demographic, socioeconomic, health, and behavioral factors and tested participants for HIV, hepatitis B virus (HBV), and hepatitis C virus (HCV) and compared across the three methods. Overall, 561 (74.8%) of the targeted 750 PWID were enrolled. Venue-based convenience sampling enrolled 96% (242/250) of the targeted participants, followed closely by street-based outreach with 92% (232/250) recruited. While RDS yielded the fewest recruits, producing only 35% (87/250) of the expected participants, those recruited through RDS were more likely to be female, more racially diverse, and younger.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Persons who inject drugs (PWID) are at significant risk for a multitude of health problems, including infection with blood borne pathogens (BBP) such as HIV, hepatitis C virus (HCV), and hepatitis B virus (HBV). However, the illegal and stigmatized nature of substance use makes it difficult to access PWID for intervention to mitigate the risk of BBP infections [1]. Starting in 2006, an epidemic of injection drug use and opiate abuse among younger persons in primarily rural and suburban communities has been documented in the USA. [2, 3] This threatens to cause significant morbidity and mortality related to viral hepatitis and HIV infection. Recent examples include a large HIV and HCV outbreak among rural residents of Indiana [4] and HCV infection among rural and suburban residents of Wisconsin [5] and Massachusetts [6].
Respondent-driven sampling (RDS) is a chain referral method designed to recruit hidden populations by selecting “seed” recruiters from the target population to recruit other members of their peer network, who in turn recruit subsequent waves of participants from their own peer networks. This method can reach deep into isolated social networks to recruit participants that would otherwise be inaccessible to investigators through other recruitment methods [7, 8]. RDS can provide unbiased estimates of prevalence in these difficult-to-reach populations. Other potential recruitment methods include venue-based convenience sample and street outreach sampling, both of which use locations frequented by PWID and provide a quicker and less complex way of recruiting participants. However, these sampling methods are not random, thus, leading to selection bias, and may not be a representative of the entire population being studied [1]. Venue-based convenience sampling, which utilizes locations where PWID spend time (such as syringe exchange programs, drug treatment programs, bars, and shooting galleries), allows oversampling of underrepresented populations (i.e., risk factor, age, and race) [9], and street-based sampling allows for oversampling of populations more likely to be on the street (i.e., homeless and low income) [10]. However, these methods present analytical challenges for development of a valid mechanism for adjusting for unequal selection probabilities and unknown biases [9, 10].
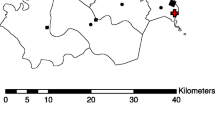
We recruited PWID aged 18–40 years residing in San Diego, California, for the Study to Assess Hepatitis C Risk (STAHR), a cross-sectional study to estimate the prevalence and identify correlates of HCV among young adult PWID [11]. One of the study objectives was to determine the optimal recruitment methods for ongoing national surveillance of HCV infection. The present analysis compares each recruitment method and identifies participant characteristics associated with each method. The study was approved by the institutional review board at the University of California, San Diego, and all participants provided written informed consent.
Methods
From March 2009 to June 2010, we recruited PWID aged 18–40 years, who had injected drugs at least once in the previous 6 months, resided in San Diego County at the time of recruitment, and agreed to a blood draw for serologic testing. Participants, who enrolled in one recruitment method, were automatically excluded from enrolling through other recruitment methods. Methods for this study are described elsewhere [11]. In brief, potential participants completed a brief screener to confirm eligibility. Eligible PWID were then invited to participate, gave their informed consent, and completed a behavioral risk assessment, followed by pre-test counseling and venipuncture for HIV, HCV, and HBV testing. Participants were scheduled to return 2 to 3 weeks later for their test results and post-test counseling. All participants were offered referrals for healthcare and prevention services including free hepatitis A and B vaccination and treatment for drug use. Audio computer-assisted self-interviewing (ACASI) technology was used to assess sociodemographic information, drug use and other behavioral risk factors for BBP infection, and access to care metrics. Following the interview and pre-test counseling, participants provided venous blood samples for hepatitis C antibodies (anti-HCV) using Abbott Axsym microparticle enzyme immunoassay (Abbott Laboratories, Chicago, IL, www.abbott.com), HCV, and HIV nucleic acid testing (NAT) (American Red Cross Blood Services National Testing Laboratory, St. Louis, MO). Stored specimens from participants were tested for HBV core antibody (anti-HBc) using a chemiluminescent immunoassay (VITROS ECi, Ortho Clinical Diagnostics, Rochester NY, www.orthoclinical.com).
Our goal was to recruit 250 young adult PWIDs through each of the three sampling methods including RSD, venue-based convenience sampling, and street outreach. For RDS, participants were recruited for 12 months (March 2009 to April 2010), but for the other two methods, participants were recruited for only 9 months (August 2009 to April 2010). RDS, as previously described, employs PWID “seeds” to recruit other PWID. The primary incentive was $25 for the completed interview and blood draw, $10 for returning for results, and each recruiter received a $10 incentive for each recruit (up to 3). This method uses mathematical modeling to adjust for potential bias that could result from the non-random selection of seeds. To avoid recruiting the same participants through RDS and the other two approaches, RDS was conducted for 3 months before recruitment with the other methods was instituted. Seeds with large social networks who were popular among their peers were selected; we also attempted to select seeds with a range of ages, genders, races, drugs of choice, and preferred venues. Venue-based convenience sampling used a local syringe exchange program to recruit participants. Street-based sampling was conducted using outreach workers who recruited PWID from neighborhoods with known high prevalence of injection drug use, as well as passing out flyers and other information about the study at businesses and establishments frequented by PWID. Participants recruited using these two methods were encouraged to tell their peers about the study, but no incentives were offered for recruitment. Comparisons were made between the three groups using multinomial logistic regression. A bivariate analysis was performed for each factor, and those significant at the p = 0.1 level were included in multivariable analysis. All analyses were performed using SAS version 9.3.
Results
A total of 561 (75%) participants of the expected 750 were successfully recruited using the three methods. Of these, 87 (16%) participants were recruited through RDS, 242 (43%) were recruited through venue-based convenience sampling, and 232 (41%) were recruited through street-based sampling (Table 1). We had a total of 16 seeds from RDS, the longest chain was five waves, but the majority of our RDS seeds only resulted in two waves. Seed ages ranged from 22 to 39 years (median 28), eight (53%) were male, and nine (60%) were white, non-Hispanic race. We recruited 35% (87/250) of the target number of participants for RDS compared to 96% and 92% of the target number for venue-based convenience sample and street-based sample, respectively. In the bivariate analysis, participants recruited using RDS, compared to the other two methods, started injecting at a younger age, were more likely to be biological women, were less likely to be white race and more likely to be black race, more likely to have less than a high school education or GED, and more likely to be homeless in the past 6 months. RDS participants were equally likely to have been tested for HIV and HCV, be HIV infected, or ever diagnosed with an STI, than those recruited through the other two methods. RDS participants were more likely to have been injecting more than 5 years compared to those recruited through the other two methods.
Participants recruited through the venue-based convenience sampling (SEP) were more likely to have used only heroin in the last 3 months, more likely to have been HCV infected in the past, more likely to have some income, and more likely to have a high school diploma or GED than participants recruited through street outreach or RDS. Street outreach participants were more likely to be male and more likely to use methamphetamine alone than either RDS or SEP recruited participants.
Because of strong collinearity among variables, we included all covariates reaching a level of significance of p < 0.1 in a multivariable model (age at first injection, sex, race, less than high school/GED education, no income, anti-HBc positive, anti-HCV positive, duration of injection >5 years, and drug injected most often in the past 3 months). Only sex remained significantly associated with sampling method.
Discussion
This study shows that street-outreach and venue-based convenience sampling methods were able to enroll more PWID in a shorter time period than RDS. This failure to enroll sufficient numbers in a set amount of time using RDS was different in our study compared to previous studies of older PWID in urban areas [12,13,14,15]. However, our results were similar to other studies [1, 7, 8, 12, 13, 15] showing that participants recruited through RDS are younger, more racially diverse, and more likely to be female than traditional recruitment methods. Additionally, this study found RDS sampling yielded participants who were less educated, more likely to have no income, and more likely to be homeless. All three recruitment methods targeted slightly different populations. Participants recruited through the venue-based convenience method had characteristics that would be expected among PWID populations (e.g., injecting only heroin, longer duration of injecting, and more likely to have been HCV infected in the past) compared to street-based and RDS-recruited participants. Street-based participants were more likely to be male and use methamphetamine only compared to venue-based and RDS-recruited participants. Furthermore, only sex was significant after controlling for other factors in the multivariable analysis.
Our study had some limitations. All risk behaviors were self-reported and could not be verified. In addition, cross-sectional studies cannot establish temporal relationships between risk factors and primary outcomes. Further, the representativeness of our sample to all PWID in San Diego is uncertain due to the hidden nature of this population and the age range (18–40 years). We used three different recruitment methods to maximize the number and diversity of participants recruited into the study, but this can also affect the representativeness of the population.
In conclusion, RDS was found to be a reliable method for recruiting PWIDs who are harder to reach, such as women and young adults. However, in populations where drug use is currently epidemic (i.e., young adults from rural and suburban communities) and less time is available for enrollment, it may be difficult to recruit sufficient numbers, particularly in small drug use networks such as in rural areas. Although we do not have sufficient data to determine why RDS did not perform as expected, possible contributing factors include a delay in the study initiation that resulted in the loss of key seed participants, the study location which required significant travel expenses not covered by the study, low reimbursement amounts (anecdotal reports), and the focus on younger PWID, with anecdotal reports of many of the peers of these younger PWID being too old for the study. If researchers want to recruit persons using drugs inclusive of any route of administration, who are younger in age, and want to recruit more PWID who are not receiving services, RDS can be a good method. If PWID specifically are the target population, venue-based convenience sampling using a venue frequented by PWID populations (such as SEPs or shooting galleries) would likely be most efficient. However, the distribution of syringe exchange programs is limited by local and state policy; programs might not necessarily be located in areas where the drug use epidemic and HCV epidemic have converged. In light of new curative HCV therapies, selecting the most representative population might not be as important as simply reaching at-risk PWID for testing and referral to treatment, particularly in small communities and non-urban settings.
References
Magnani R, Sabin K, Saidel T, Heckathorn D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS. 2005;19(Suppl 2):S67–72.
Rudd RA, Paulozzi LJ, Bauer MJ, et al. Increases in heroin overdose deaths—28 States, 2010 to 2012. MMWR Morb Mortal Wkly Rep. 2014;63(39):849–54.
Suryaprasad AG, White JZ, Xu F, et al. Emerging epidemic of hepatitis C virus infections among young non-urban persons who inject drugs in the United States, 2006–2012. Clin Infect Dis. 2014;59(10):1411–9.
Conrad C, Bradley HM, Broz D, et al. Community outbreak of HIV infection linked to injection drug use of Oxymorphone—Indiana, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(16):443–4.
Stanley MM, Guilfoyle S, Vergeront JM. Hepatitis C virus infections among young adults—rural Wisconsin, 2010. Morbid Mortal Wkly Rep MMWR. 2012;61(19):358.
Church D, Barton K, Elson F, et al. Risk factors for hepatitis C virus infections among young adults—Massachusetts, 2010. Morb Mortal Wkly Rep. 2015;60(42):1457.
Heckathorn DD. Snowball versus respondent-driven sampling. Sociol Methodol. 2011;41(1):355–66.
Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Soc Probl. 2015;44(2):174–99.
MacKellar DA, Gallagher KM, Finlayson T, et al. Surveillance of HIV risk and prevention behaviors of men who have sex with men—a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(supp 1):39–47.
Muhib FB, Lin LS, Stueve A, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep. 2001;116(supp 1):216–22.
Garfein RS, Rondinelli A, Barnes RF, et al. HCV infection prevalence lower than expected among 18–40-year-old injection drug users in San Diego. CA J Urban Health. 2013;90(3):516–28.
Burt RD, Hagan H, Sabin K, Thiede H. Evaluating respondent-driven sampling in a major metropolitan area: comparing injection drug users in the 2005 Seattle area national HIV behavioral surveillance system survey with participants in the RAVEN and Kiwi studies. Ann Epidemiol. 2010;20(2):159–67.
Burt RD, Thiede H. Evaluating consistency in repeat surveys of injection drug users recruited by respondent-driven sampling in the Seattle area: results from the NHBS-IDU1 and NHBS-IDU2 surveys. Ann Epidemiol. 2012;22(5):354–63.
Burt RD, Thiede H. Assessing differences in groups randomized by recruitment chain in a respondent-driven sample of Seattle-area injection drug users. Ann Epidemiol. 2014;24(11):861–7.
McKnight C, Des Jarlais D, Bramson H, et al. Respondent-driven sampling in a study of drug users in New York City: notes from the field. J Urban Health. 2006;83(6 Suppl):i54–9.
Acknowledgements
The authors sincerely appreciate the study participants of STAHR for their contributions to this important research, as well as current and past researchers and staff. The study was supported by the Centers for Disease Control and Prevention National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Cooperative agreement number 200-2007-21016. None of the authors have any conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
CDC Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Rights and permissions
About this article
Cite this article
Collier, M.G., Garfein, R.S., Cuevas-Mota, J. et al. Comparison of Three Popular Methods for Recruiting Young Persons Who Inject Drugs for Interventional Studies. J Urban Health 94, 587–591 (2017). https://doi.org/10.1007/s11524-017-0158-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-017-0158-x