Abstract
Local or small-area estimates to capture emerging trends across large geographic regions are critical in identifying and addressing community-level health interventions. However, they are often unavailable due to lack of analytic capabilities in compiling and integrating extensive datasets and complementing them with the knowledge about variations in state-level health policies. This study introduces a modeling approach for small-area estimation of spatial access to pediatric primary care that is data “rich” and mathematically rigorous, integrating data and health policy in a systematic way. We illustrate the sensitivity of the model to policy decision making across large geographic regions by performing a systematic comparison of the estimates at the census tract and county levels for Georgia and California. Our results show the proposed approach is able to overcome limitations of other existing models by capturing patient and provider preferences and by incorporating possible changes in health policies. The primary finding is systematic underestimation of spatial access, and inaccurate estimates of disparities across population and across geography at the county level with respect to those at the census tract level with implications on where to focus and which type of interventions to consider.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Data-driven local inferences on health care delivery and health outcomes across large geographic areas can facilitate targeted and comparative actions in a way that resources are effectively allocated for maximum impact.1 – 3 Local inferences rely on high geographic resolution measures, often called small-area estimates. Many existing studies in the fields of epidemiology, environmentrics,4 , 5 and health care planning literature6 – 10 have introduced and applied models for deriving small-area estimates from large, national administrative datasets or/and publicly available data.
Small-area estimates at high geographic resolution may not however be available for policymaking by federal agencies, state health departments, and community health organizations because of resource constraints in acquiring relevant data or/and lack of analytic capabilities to derive such estimates.11 , 12 While local health departments may collect some administrative data that can be used in small-area inferences, they likely do not collect the types of data that can aid in deriving small-area estimates and identifying emerging trends across large geographic regions (e.g., statewide or multiple states).
Because of this important challenge, it is common practice to derive estimates at lower geographic resolution (e.g., county) for statewide or national comparisons.6 – 10 , 13 , 14 However, division of states into counties varies greatly; for example, a large state such as California has 58 counties, whereas a smaller state such as Georgia has 159 counties. Within-county variations in demographics, population health, and economics can lead to high error rates of the county-level estimates. In turn, making decisions based on such estimates can suggest interventions that do not appropriately address health care disparities and/or improve outcomes. Estimation at the highest geographic resolution is important to overcome these limitations.
Small-area estimation at the highest geographic resolution is particularly critical in estimation of spatial access, measuring accessibility and availability of health care services.15 Spatial access is a system outcome varying across communities due to geographic variations in health care infrastructure and in population’s choice of health care provider,16 both coupled with variations in state-level health policies, for example, Medicaid reimbursement and eligibility.
To this end, this paper applies a modeling approach for obtaining small-area estimates of spatial access to pediatric primary care that is data “rich” and mathematically rigorous, integrating data and health policy in a systematic way. The model is general and can be applied widely to different types of care, different states, and different countries. The methodology is particularly relevant for deriving local estimates because it employs a systems approach, allowing for trade-offs between supply (providers) and need (patients), and for constraints in other forms of access such as acceptance rate of governmental insurance.17 , 18 The approach characterizes spatial access assuming that not all patients are covered or served by the system of care because of their lack of access in all its forms,19 and it separately provides estimates of spatial access for those served by private and public insurance while accounting for their competition on available resources. It incorporates timely information specified in the Patient Protection and Affordable Care Act (ACA); it considers all options of primary care for children, with preferences depending on the provider type and patient age; and it accounts for patient’s trade-off between accessibility (measured by distance traveled) and availability (measured by congestion at the provider or wait time).
Statistical inference is used to demonstrate the sensitivity of the model in capturing trends within states derived from estimates at different geographic resolution levels, i.e., census tract and county level, with implications in policy decision making on where to focus interventions for improving access and on which type of intervention to consider for more appropriate health care delivery, particularly for different population groups differentiated by insurance type.
We piloted our approach in two states, Georgia and California, selected because of the differences in their administrative geographic subdivisions.
Data Sources
Data: Administrative Subdivision in Georgia and California
Census tract-level data containing geographic information for the two states were downloaded from the census bureau’s website.20 Georgia has 1969 census tracts and 159 counties. After eliminating census tracts with missing data, the analysis includes 1951 census tracts. California has 8057 census tracts and 58 counties. After eliminating census tracts with missing data, the analysis includes 7984 census tracts.
Data: Demand for Pediatric Primary Care
Recommendations by the American Academy of Pediatrics21 about the type and frequency of visits are heeded resulting in consideration of three age classes requiring different numbers of visits/year: age 0–1, age 1–5, and age 6–18 with an average number of visits/year equal to 8, 1.6, and 1, respectively. Patient population is aggregated at the census tract level and located at the census tract centroid. The 2010 SF2 100 % census data and the 2012 American Community Survey data are used to compute the total number of children in each census tract and in each age class. Specifically, the following tables were used to compute the value of the parameters for the optimization model: PCT3, B17024, PCT10, PCT7, B19001, and B08201 (see Appendix 2 which provides a detailed description on the applied methodologies to derive model parameters from the different tables.)
Medicaid and the Children’s Health Insurance Program (CHIP) are social health care programs for families and individuals with low income and limited resources. They constitute the primary sources of coverage for low-income children in the USA. Several requirements need to be met to be eligible in the programs, including total family income which cannot be greater than a fixed threshold which varies by state. We derive the Medicaid and CHIP eligible population counts using a threshold of 247 % of the Federal Poverty Level (FPL) for the state of Georgia and a threshold of 261 % for the state of California, consistent with the new threshold limits of the ACA.22 It is assumed that patients can be assigned to a provider whose distance is less than or equal to 25 miles, in accordance with the guidelines of the Department of Health and Human Services (DHHS).23 Since patients without a private vehicle must use alternative means of transportation, we also assign a maximum distance threshold for these patients equal to 10 miles.
Data: Supply of Pediatric Primary Care
The set of providers and their addresses were obtained from the 2013 National Provider Identification (NPI) database.24 This dataset provides information of all providers currently being reimbursed for health care services. Individual and institutional records are distinguished by the entity type attribute where entity 1 corresponds to individual (e.g., physicians, sole proprietors) and entity 2 corresponds to health care providers who are not individual. We restricted our network of providers only to entity 125 because the dataset does not report how many providers of a particular type are represented by the organization’s listed taxonomies raising the possibility of double-counting between individuals and organizations.
We selected only those providers who have, among the declared set of taxonomy codes, one of the following: Family Medicine (207Q00000X), Internal Medicine (207R00000X), Pediatrics (208000000X), and Nurse Practitioner Pediatrics (363LP0200X). We used the Business Practice Address attribute in the dataset to geolocate each selected provider using the Texas A&M Geocoding Services.26 The NPI database is used not only because geolocation information of each provider was needed, but also because of the inconsistencies27 in other databases. Street network distances between census tract centroids and provider addresses are computed using the ArcGIS Network Analyst28 using the National Highway Planning Network downloadable from the Federal Highway Administration website.29 Total distances correspond to the shortest network path between the centroid location and the provider location. If a centroid does not fall onto the street network, it is moved to the closest street.
A maximum provider caseload of 7500 visits/year for an average patient panel size of 2500 patients28 is used. It is assumed that a higher value will significantly impair quality of access. Caseloads of General Pediatricians and Pediatric Nurse Practitioners are assumed to be completely devoted to pediatric care while Family/Internal Medicine physicians are assumed to devote only 10 % of their caseload to children.29
To account for different acceptance rates of Medicaid/CHIP insurance, varying by state,30 , 31 practice setting, and provider type,32 the 2009 MAX Medicaid claims data is used to obtain county-level estimates of the percentage of primary care physicians participating in the Medicaid program (see Appendix 1 which provides additional information on the data used and methodology used to compute county-level Medicaid acceptance ratios). Using these ratios, the same approach used in a previous work17 is applied, and a subset of providers is randomly selected in each county who accept Medicaid/CHIP insurance such that the total number of selected providers equals the estimated percentage of providers in the county.
Methods
The Mathematical Model
The optimization model in Nobles et al.17 is extended to take into account several additional factors that influence patients’ and providers’ behavior, including different patient age classes, different needs for age class, different provider types, and different patient preferences for provider types.
The decision variables of the model represent the total number of patients in each census tract of a given age class who are assigned to a specific provider. Since the Medicaid/CHIP eligible and privately insured populations may face different barriers to health care, the model considers the two populations separately when matched to providers, while accounting for their competing access to providers accepting both types of insurance.
Our model is based on the assumptions that both families and policy makers value children having a primary care provider, that patients prefer to visit nearby physicians, and that they prefer to schedule visits when the office is not too busy (low congestion); however, when physician congestion is considered too high, families prefer nonphysician providers such as Nurse Practitioners.33 Under these assumptions, the objective function of the optimization model is a weighted sum of the total distance traveled (which needs to be minimized) and the provider preference contingent upon demand volume (which needs to be maximized). The balance between these two components of the objective function is controlled by a trade-off parameter, which is used to define the relative importance of each component in the objective function. Its value is empirically selected such that (i) neither of the two components of the objective function dominates the other, and (ii) the optimized decision results in sufficient spatial autocorrelation to indicate that close neighbors experience similar travel distance and similar congestion level (see Appendix 3 for a detailed description of the empirical selection of the trade-off parameter).
Constraints in the model reflect trade-offs and behaviors in the system. From patients’ perspective, constraints in the resulting matching take into account the obstacles that patients encounter when choosing a provider (such as distance, provider congestion, Medicaid/CHIP insurance acceptance and provider type). From providers’ perspective, constraints are considered so that: (i) the total number of patients assigned to each provider does not exceed maximum caseload capacity, (ii) the total number of assigned patients under Medicaid/CHIP insurance does not exceed Medicaid/CHIP acceptance caseload, and (iii) different provider types have different caseload capacities and different Medicaid/CHIP acceptance levels. The detailed description of the model is provided in Appendix 3.
The output of the model consists of the optimal assignment of needed demand in each census tract to providers in the network, while the demand within a census tract may be assigned to different providers or/and a proportion of the demand may not be served. Hence, the model provides estimates of the served demand for primary care. The optimization model is implemented using the optimization programming language OPL34 and the CPLEX solver on a UNIX system.
Parameters of the model are estimated for each state by integrating the different data sources mentioned in the previous section together with the different health policies (i.e., Medicaid/CHIP eligibility criteria) implemented in each state. Table 1 provides a summarized description of the set of parameters, their values, and the data source we used to determine their value.
Spatial Access Measures: Accessibility and Availability
We use the results of the optimization model to measure accessibility and availability of primary care for overall population of children, Medicaid/CHIP-insured children, and privately insured children, both at the county and census tract levels. Accessibility is measured as the average distance a child must travel for each visit to his/her assigned provider. Availability is measured as the congestion a child in the census tract or in the county experiences for each visit at his/her assigned provider. Since children who are not assigned to a provider have the worst possible spatial access, regions whose population is not assigned to any provider are assumed to experience a distance of 25 miles and 100 % congestion.
Statistical Comparison of the Measures at the County and Census Tract Levels
Inference statistical methods are used to compare the distributions of accessibility and availability at the county and census tract levels and to compare the level of disparities in accessibility and availability between the Medicaid/CHIP-insured and the privately insured population when analyzed at the census tract level or at the county level.
In particular, denote by M(s) and by O(s) the spatial access measures (either the availability or the accessibility measure) derived from the optimization model for the Medicaid/CHIP-insured population and for the privately insured population, respectively, where s denotes the spatial aggregation (i.e., either census tract or county). We test whether summaries of the distributions of the two processes, including median and variance, are statistically different. Because both processes are observed over the same spatial units, we apply paired testing procedures.
We apply the nonparametric Wilcoxon test to test the null hypothesis for equality of medians at the census tract level and at the county level (H0 : μ CTY = μ CENSUS; H1 : μ CTY > μ CENSUS) of the two dimensions (accessibility and availability) for the two states. The nonparametric Wilcoxon test and a modified version of the nonparametric Wilcoxon test are used to test equality of medians (H0 : μ M = μ O ; H1 : μ M > μ O ) and equality of variances (H0 : σ 2 M = σ 2 O ; H1 : σ 2 M > σ 2 O ), respectively, of the two processes M(s) and O(s) both at the census tract level and at the county level (see Appendix 4 for details on the statistical methods used).
Threshold maps are constructed to visualize where accessibility and/or availability is higher or lower than the 85th percentile and the 15th percentile, respectively.
To analyze the association between accessibility and availability at the census tract and county levels, a nonparametric regression method is applied to find a smooth relationship between the two measures using the GAM function in the mgcv library in R.35
Simultaneous confidence bands for the difference measure of the two populations are estimated to identify census tracts or counties where the difference in either accessibility or availability between the two populations is statistically significant. Positive or negative significance maps are then derived at the 0.01 significance level (see Appendix 4 for details).
Results
The total number of children in the two states is approximately equal to 12.5 million, and the total number of children eligible for public insurance is equal to 6.8 million. The total number of providers under consideration in the state of Georgia is approximately equal to 8000, while in the state of California, it is approximately equal to 32,000. Fifty-three percent of the providers in the state of Georgia accept Medicaid/CHIP-insured children, for a total of approximately 4200 providers; 59 % of the providers in the state of California accept Medicaid/CHIP-insured children, for a total of approximately 18,800 providers.
Comparing Accessibility and Availability at the County and Census Tract Levels
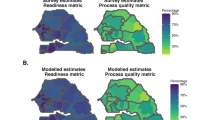
Summary statistics of the accessibility and availability measures are computed at the county and the census tract levels for each population group in each state and are given in Table 2. Boxplots of the distributions of the accessibility and availability measures for the two states, both at the county and census tract levels, are shown in Fig. 1. Tables 3 and 4 show the results of the statistical tests. Figure 2 shows the threshold maps, with the census tracts (or counties) with accessibility or availability measures higher than the 85th percentile or lower that the 15th percentile (denoted as “higher” or “lower”). Figure 3 shows the smooth nonparametric relationship between availability and accessibility. Figure 4 shows the significance maps at the census tract level and at the county level for both states and for both the accessibility and the availability dimensions.
The boxplots of the distributions of the accessibility dimension (distance (miles)—on the left) and of the availability dimension (congestion—on the right) at the census tract level and at the county level for the Medicaid/CHIP-insured population and the privately insured (non-Medicaid) population for the state of Georgia (top) and for the state of California (bottom). Horizontal lines in the figures represent mean values at the state level for the overall population.
The threshold maps for both states and for both accessibility (i.e., distance (miles)) and availability (i.e., congestion). In each map on the left, the gray-shaded areas and triangles correspond to counties and census tracts, respectively, where the local estimates are lower than the 15th percentile (denoted “Lower”). In each map on the right, the gray-shaded areas and dots correspond to counties and census tracts, respectively, where the local estimates are higher than the 85th percentile (denoted “Higher”).
The smoothed nonparametric relationship between accessibility (distance) and availability (congestion) obtained using the “gam” function in the library mgcv in the R statistical software. The resulting function for the county level is shown on the left, and the function for the census tract level is shown on the right. Results for Georgia are on the top, and results for California are on the bottom.
Significance maps both at the census tract level (on the left) and at the county level (on the right) for the two dimensions of access (i.e., accessibility and availability). Each dot on the map corresponds to a census tract or a county where Medicaid/CHIP-insured population has a statistically significantly lower accessibility (i.e., greater distance) or lower availability (i.e., greater congestion) than the privately insured population, at α = 0.01 significance level. The gray-shaded regions on the maps correspond to counties where the Medicaid/CHIP-insured population does not experience a significantly worse accessibility or availability.
Accessibility
The median distance traveled at the census tract level for the three population groups for Georgia and California is 7.94 miles (standard deviation (SD) = 6.65) and 4.92 miles (SD = 5.86) for the overall population, 8.62 miles (SD = 7.29) and 6.92 miles (SD = 7.03) for the Medicaid/CHIP population, and 6.07 miles (SD = 6.03) and 1.01 miles (SD = 4.73) for the privately insured population, respectively.
The median distance at the county level is greater than the median distance at the census tract level in both states, and for all the three population groups, such a difference is statistically significant for both states (Table 3).
The 85th percentile of the travel distance distribution at the census tract (county) level is 15.84 (19.58) miles in Georgia and 10.55 (15.69) miles in California. The 15th percentile of the travel distance distribution at the census tract (county) level is 1.07 (7.39) miles in Georgia and 0.45 (5.55) miles in California (Fig. 2).
Availability
The median congestion experienced at the census tract level for the three population groups for Georgia and California is 0.43 (SD = 0.27) and 0.49 (SD = 0.25) for the overall population, 0.42 (SD = 0.28) and 0.43 (SD = 0.26) for the Medicaid/CHIP population, and 0.39 (SD = 0.28) and 0.49 (SD = 0.29) for the privately insured population, respectively.
The median congestion at the county level is greater than the median congestion at the census tract level in both states, and for all the three population groups, such a difference is statistically significant for both states (Table 3).
The 85th percentile of the congestion distribution at the census tract (county) level is 0.78 (0.85) in Georgia and 0.81 (0.73) in California. The 15th percentile of the congestion distribution at the census tract (county) level is 0.15 (0.39) in Georgia and 0.23 (0.45) in California (Fig. 2).
The correlation coefficient between availability and accessibility at the census tract level is r = 0.73 for Georgia and r = 0.59 for California, while at the county level it is, respectively, r = 0.85 and r = 0.88 (Fig. 3).
Disparities between Population Groups at the Census Tract and the County Levels
The significance maps (Fig. 4) show that in Georgia (California), the Medicaid/CHIP-insured population has a statistically significantly lower accessibility than the privately insured population in 53 % (74 %) of the census tracts and in 100 % (98 %) of the counties. The Medicaid/CHIP-insured population in Georgia (California) experiences a statistically significantly higher congestion than the privately insured population in 18 % (12 %) of the census tracts and 47 % (31 %) of the counties. As shown in Table 4, the median and variance of distance (accessibility) for the Medicaid/CHIP-insured population are statistically significantly higher than for the privately insured population at both the census tract and county levels for both states. The median congestion (availability) for the Medicaid/CHIP-insured population is statistically significantly higher than for the privately insured population both at the census tract and county levels, only for the state of Georgia.
Discussion
A modeling approach for small-area estimates of spatial access to pediatric primary care is introduced along with a systematic comparison of estimates of spatial access at the census tract and county levels for Georgia and California.
The approach can address the limitations of other existing models such as simple ratios of providers to population15 and the two-phase catchment method (2SFCA)36 which does not account for the unserved demand due to lack of access in all its dimensions and the trade-offs between supply and need of care. The proposed approach is able to capture patient and provider preferences17 , 18 and to incorporate health policies changes by a different setting of the values of the model parameters. Additionally, the model is able to capture the differences in the trends across large regions derived from estimates with different resolution levels. The constraints included in the model are basic barriers to accessibility, availability, and acceptability; the model can take into account other dimensions of access such as accommodation.
For both availability and accessibility, the results show that county-level estimates tend to underestimate spatial access. The medians of the measures estimated at the county level are significantly greater than the medians of the measures at the census tract level, because the within-county distributions of the estimates are highly skewed. Hence, spatial access is underestimated at the county level. The implication of this finding is that decisions based on the county-level estimates about where to locate or incentivize new practices could be misaligned to need.
The results show also that geographic disparities for each population group (public and privately insured) are consistently underestimated when measured at the county level: variability of the measures at the county level is lower than variability at the census tract level on all but one measure reported here.
For the two states, the choice of where to focus interventions for improving access, if based on the county-level estimates, would target regions that do not experience greater needs for improvement in spatial access. For Georgia, many areas of the state would not be identified as “in need” according to the county estimates, although it is evident from the census tract estimates. For example, Burke County in Georgia with six census tracts has an average travel distance at the county level of 17.7 miles, which is lower than 19.5 miles, the 85th percentile of the travel distance distribution at the county level for this state. However, the average travel distance of the six census tracts in the county is 23.6, 22.5, 18.1, 13.3, 8.9, and >25 miles. The high variability of the travel distances at the census tract level is not captured at the county level, and an intervention based on county-level estimates would neglect in this case to intervene in communities which are potentially most in need.
County estimates are misleading when trying to understand which type of intervention is more appropriate to deliver. In the two states, the county-level estimates suggest that regions with low (high) availability also have consistently low (high) accessibility. Thus, although appointments may be available, they are practices that are difficult to travel to. In contrast, the census tract estimates reveal a different relationship; specifically, in Georgia, these estimates show that there are several regions that experience lower distance but higher congestion.
Finally, local estimates are a much better tool for capturing disparities across populations. Our results reveal that disparities in access between Medicaid/CHIP-insured and privately insured populations based on the county level metrics are underestimated. Specifically, the county-level estimates for availability in Georgia do not capture the statistically significant gaps in some counties in the northern part of the state, as evident from the census tract estimates. In California, according to the county-level estimates for availability, there is no county with a statistically significant difference in the central and south regions. However, the census tract estimates reveal statistically significant differences for many areas in these regions. In terms of accessibility, 100 % of the counties in Georgia show a statistically significant difference between the two population groups; however, the census tract estimates show that this is not true for some areas in the southeastern region of the state.
The study has several limitations. The primary challenge in this study is the limited availability of data. Because of limited state-level information, eligible populations are evaluated considering federal net income thresholds instead of modified adjusted gross income (MAGI)-equivalent thresholds. The procedure for evaluating the MAGI-equivalent threshold depends on state-level policies with too many unknown parameters to be realistically considered. Additionally, because of lack of data, multiple data sources are considered for different years to estimate demand parameters. Finally, Medicaid/CHIP acceptance rates are computed using 2009 data; although this limitation does not affect the overall findings of the analysis, these parameters could be underestimated because of the implementation of the ACA.
A second limitation is the set of assumptions specifying some of the system constraints. For example, the provider capacity is assumed to be uniform across geographies (i.e., 2500 patients or 7500 visits/year). Similarly, the same willingness to travel for all populations in rural and urban areas is assumed. Moreover, variations in the percentage of physicians practicing pediatric primary care after the implementation of the ACA are not accounted for. These assumptions can be relaxed, and the system constraints can be better informed with the acquisition of detailed local-level data.
Our study brings us to several conclusions. Much research in health services considers access to care, either as a primary study topic or as a factor for which to control.8 , 37 – 43 These existing studies often rely on measures of access that are too simple to account for systemwide trade-offs, or measures computed at high geographic aggregation levels. This paper demonstrates that these limitations can result in misleading policies and interventions and that high geographic resolution estimates are needed to understand the nuances in health care access where county-level estimates wash out important differences.
By understanding access at high geographic resolution, it is also possible to separate out different dimensions of access and may facilitate designing targeted interventions that will have the highest impact at the community level. Local estimation approaches are the best available tool and can ultimately help improve the health of our nation’s children. The models used in this paper (and the associated code) are available at www.healthanalytics.gatech.edu so that other researchers or health organizations can use them to assist in quantifying measures of access, with no software license required.
References
Cooper RA, Cooper MA, McGinley EL, Fan X, Rosenthal JT. Poverty, wealth, and health care utilization: a geographic assessment. J Urban Health. 2012; 89(5): 828–847.
Fried B. Using small area estimates for ACA outreach. San Diego presentation at the Academy Health Annual Research Meeting (ARM), June 10, 2014. Downloadable from: http://www.shadac.org/publications/using-small-area-estimates-aca-outreach. Accessed February 2015.
Osypuk TL, Galea S. What level macro? Choosing appropriate levels to assess how place influences population health. In: Galea S, ed. Macrosocial determinants of population health. New York, NY: Springer Media; 2007: 399–435. http://deepblue.lib.umich.edu/handle/2027.42/55742. Accessed February 2015.
Elliott P, Wartenberg D. Spatial epidemiology: current approaches and future challenges. Environ Health Perspect. 2004; 112(9): 998–1006.
Leroux B, Lei X, Breslow N. Estimation of disease rates in small areas: a new mixed model for spatial dependence. In: Halloran ME, Berry D, eds. Statistical models in epidemiology, the environment, and clinical trials, vol. 116. New York: Springer; 2000: 179–191.
Chan L, Hart LG, Goodman DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health. 2006; 22(2): 140–146.
Crooks V, Schuurman N. Interpreting the results of a modified gravity model: examining access to primary health care physicians in five Canadian provinces and territories. BMC Health Serv Res. 2012; 12(1): 230.
Lasser KE, Himmelstein DU, Woolhandler S. Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. Am J Public Health. 2006; 96: 1300–1307.
Rosero-Bixby L. Spatial access to health care in Costa Rica and its equity: a GIS-based study. Soc Sci Med. 2004; 58(7): 1271–1284.
Ye H, Kim H. Measuring spatial health disparity using a network-based accessibility index method in a GIS environment: a case study of Hillsborough County, Florida. Int J Geospatial Environ Res. 2014; 1(1): 2.
Fielding JE, Frieden TR. Local knowledge to enable local action. Am J Prev Med. 2004; 27(2): 183–184.
Laugesen MJ, Isett KR. Evidence use in New York City public health policymaking. Front Public Health Services Syst Res. 2013; 2(7): 2.
Holt AB, Zhang X. Geospatial data methods for estimating population health outcomes. http://www.cste2.org/webinars/webinarpdfs/GeospatialDataMethods82313.pdfCDC webminar, August 2013.
D’Agostino-McGowan L, Gennarelli RL, Lyons SA, Goodman MS. Using small-area analysis to estimate county-level racial disparities in obesity demonstrating the necessity of targeted interventions. Int J Environ Res Public Health. 2013; 11(1): 418–428.
Gautam S, Li Y, Johnson TG. Do alternative spatial healthcare access measures tell the same story? GeoJournal. 2014; 79(2): 223–235.
Guagliardo MF. Spatial accessibility of primary care: concepts, methods and challenges. Int J Health Geogr. 2004; 3(1): 3.
Nobles M, Serban N, Swann J. Measurement and inference on pediatric healthcare accessibility. Ann Appl Stat. 2014; 8(4): 1922–1946.
Li Z, Serban N, Swann J. “An optimization framework for measuring spatial access over healthcare networks”, to appear, BMC Health Services Research. 2015.
Garfield R, Young K. Adults who remained uninsured at the end of 2014. http://kff.org/health-reform/issue-brief/adults-who-remained-uninsured-at-the-end-of-2014/view/footnotes/Jan 29, 2015. Accessed February 2015.
United States Census Bureau. ftp://ftp2.census.gov/geo/pvs/tiger2010st/13_Georgia. Accessed October 2014.
Recommendations for Preventive Pediatric Health Care. http://brightfutures.aap.org/pdfs/AAP_Bright_Futures_Periodicity_Sched_101107.pdf: American Academy of Pediatrics. Accessed October 2013.
CMS. State Medicaid and CHIP Income Eligibility Standards. April, 2014; http://medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/Medicaid-and-CHIP-Eligibility-Levels-Table.pdf. Accessed July 2014.
Health Professional Shortage Areas (HPSAs) and Medically Underserved Areas (MUAs). http://www.hrsa.gov/shortage/mua/index.html, website accessed Aug 2014.
National Provider Identifier Standard (NPI) http://www.cms.gov/Regulations-and-Guidance/HIPAA-Administrative-Simplification/NationalProvIdentStand/index.html. Accessed Oct 2013.
Kaplan L, Skillman SM, Fordyce MA, McMenamin PD, Doescher MP. Understanding APRN distribution in the United States using NPI data. J Nurse Pract. 2012; 8(8): 626–635.
Texas A&M Geocoding Services http://geoservices.tamu.edu/Services/Geocode/. Accessed October 2013.
Freed GL, Nahra TA, Wheeler JR. Research Advisory Committee of American Board of P. Counting physicians: inconsistencies in a commonly used source for workforce analysis. Acad Med: J Assoc Am Med Coll. 2006; 81(9): 847–852.
Altschuler J, Margolius D, Bodenheimer T, Grumbach K. Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. The Annals of Family Medicine. 2012; 10(5): 396–400.
Bazemore AW, Makaroff LA, Puffer JC, et al. Declining numbers of family physicians are caring for children. J Am Board Family Med. 2012; 25(2): 139–140.
Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Affairs (Project Hope). 2012; 31(8): 1673–1679.
2011/12 Survey of Pediatrician Participation in Medicaid, CHIP and VFC. . http://www.aap.org/en-us/professional-resources/Research/pediatrician-surveys/Documents/NationalStateReports.pdf: American Academy of Pediatrics. Elk Grove Village, Illinois; American Academic of Pediatrics, 2011. Accessed October 2013.
Cunningham P, May J. Medicaid patients increasingly concentrated among physicians. Track Rep, 2006(16): 1–5.
Dill MJ, Pankow S, Erikson C, Shipman S. Survey shows consumers open to a greater role for physician assistants and nurse practitioners. Health Affairs (Project Hope). 2013; 32(6): 1135–1142.
Optimization Programming Language (OPL). http://www-01.ibm.com/software/commerce/optimization/modeling/. Accessed October 2013.
Wood SN. Generalized Additive Models: An Introduction with R. Boca Raton, Florida: CRC/Chapman & Hall; 2006.
Neutens T. Accessibility, equity and health care: review and research directions for transport geographers. J Transp Geogr. 2015; 43: 14–27.
White K, Yeager VA, Menachemi N, Scarinci IC. Impact of Alabama’s immigration law on access to health care among Latina immigrants and children: implications for national reform. Am J Public Health. 2014; 104(3): 397–405.
Jones E, Shi LY, Hayashi AS, Sharma R, Daly C, Ngo-Metzger Q. Access to oral health care: the role of federally qualified health centers in addressing disparities and expanding access. Am J Public Health. 2013; 103(3): 488–493.
Quinn SC, Kumar S, Freimuth VS, Musa D, Casteneda-Angarita N, Kidwell K. Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. Am J Public Health. 2011; 101(2): 285–293.
Herman PM, Rissi JJ, Walsh ME. Health insurance status, medical debt, and their impact on access to care in Arizona. Am J Public Health. 2011; 101(8): 1437–1443.
Delen D, Fuller C, McCann C, Ray D. Analysis of healthcare coverage: a data mining approach. Expert Syst Appl. 2009; 36(2, Part 1): 995–1003.
Formicola AJ, Ro M, Marshall S, et al. Strengthening the oral health safety net: delivery models that improve access to oral health care for uninsured and underserved populations (Reprinted from Am J Public Health, vol 94, pg 702–704, 2004). Am J Public Health. 2008; 98: S86–S88.
Aliu O, Auger KA, Sun GH, et al. The effect of pre-Affordable Care Act (ACA) Medicaid eligibility expansion in New York State on access to specialty surgical care. Med Care. 2014; 52(9): 790–795.
Alexander GC, Kurlander J, Wynia MK. Physicians in retainer (“concierge”) practice. A national survey of physician, patient, and practice characteristics. Journal of general internal medicine. 2005; 20(12): 1079–1083.
Freed GL, Dunham KM, Gebremariam A, Wheeler JRC, Research Advisory Committee of the American Board of Pediatrics. Which pediatricians are providing care to America’s children? An update on the trends and changes during the past 26 years. J Pediatr-Us. 2010; 157(1): 148–U199.
Serban N. A space–time varying coefficient model: the equity of service accessibility. Ann Appl Stat. 2011; 5(3): 2024–2051.
Krivobokova T, Kneib T, Claeskens G. Simultaneous confidence bands for penalized spline estimators. J Am Stat Assoc. 2010;105(490).
Freed GL, Stockman JA. Oversimplifying primary care supply and shortages. JAMA. 2009; 301(18): 1920–1922.
Freed GL, Dunham KM, Clark SJ, Davis MM. Perspectives and preferences among the general public regarding physician selection and board certification. J Pediatr. 2010; 156(5): 841–845. 845.e841.
Phillips RL, Bazemore AW, Dodoo MS, Shipman SA, Green LA. Family physicians in the child health care workforce: opportunities for collaboration in improving the health of children. Pediatrics. 2006; 118(3): 1200–1206.
Waller LA, Gotway CA. Applied spatial statistics for public health data, vol. 368. New York: Wiley; 2004.
Acknowledgments
This research was supported in part by a grant from the National Science Foundation (CMMI-0954283), gifts from the Nash family to Georgia Tech, and by the Institute for People and Technology (IPaT) at the Georgia Institute of Technology.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
In this appendix, additional information on data used in our optimization model is presented and the procedure applied to compute the providers’ Medicaid acceptance ratio at the county level is detailed.
Patient Data
The total number of children in the two states under consideration is approximately equal to 12.5 million, and the total number of children eligible for public insurance is equal to 6.8 million.
For the state of Georgia, the distribution of the proportion of population eligible for Medicaid/CHIP at the census tract level has a median equal to 0.60, mean equal to 0.58, and standard deviation equal to 0.23. The same distribution at the county level has a median equal to 0.66, mean equal to 0.65, and standard deviation equal to 0.18.
For the state of California, the distribution of the proportion of population eligible for Medicaid/CHIP at the census tract level has a median equal to 0.53, mean equal to 0.51, and standard deviation equal to 0.26. The same distribution at the county level has a median equal to 0.56, mean equal to 0.55, and standard deviation equal to 0.12.
The distribution of the proportion of population eligible for Medicaid/CHIP at the county and census tract levels for the two states is shown in Fig. 5.
Provider Data
An NPI is assigned to entities that respect the definition of “health care provider.” The definition of health care provider includes several categories of providers such as hospitals, nursing homes, ambulatory care facilities, durable medical equipment suppliers, clinical laboratories, pharmacies, and many other “institutional” type providers; physicians, dentists, psychologists, pharmacists, nurses, chiropractors and many other health care practitioners and professionals; group practices, health maintenance organizations, and others.
Individual and institutional records are distinguished by the entity type attribute:
-
Entity 1
Individual (e.g., physicians, sole proprietors)
-
Entity 2
Health care providers that are not individual
Data for organizational NPIs were excluded because the dataset does not report how many providers of a particular type are represented by the organization’s listed taxonomies (each organization can list up to 15 different taxonomy codes). It is also unknown how many of the providers listed under an organization’s umbrella have their own individual NPI, raising the possibility of double-counting between individuals and organizations.
The total number of providers under consideration in the state of Georgia is approximately equal to 8000, while in the state of California it is approximately equal to 32,000.
Fifty-three percent of the providers in the state of Georgia accept Medicaid/CHIP-insured children, for a total of approximately 4200 providers; 59 % of the providers in the state of California accept Medicaid/CHIP-insured children, for a total of approximately 18,800 providers.
The network of providers in Georgia consists of 21 % pediatricians, 74 % Family Internal Medicine physicians, and 5 % Nurse Pediatrics, and in California, it consists of 21 % pediatricians, 76 % Family Internal Medicine physicians, and 3 % Nurse Pediatrics. Given our capacity assumptions, the capacity of our network of providers for children care is such that, for the state of Georgia, 63 % of the visits are provided by General Pediatricians, 22 % are provided by Family/Internal Medicine physicians, and the remaining 15 % are provided by Nurse Pediatrics. Meanwhile, the capacity of the network of providers for children care for the state of California is such that 67 % of the visits are provided by General Pediatricians, 24 % are provided by Family/Internal Medicine physicians, and the remaining 9 % are provided by Nurse Pediatrics.
The distribution of the providers in the two states under consideration is mapped in Fig. 6. In Georgia, at the county level, six counties have zero providers, and 50 % of the remaining counties have fewer than 10 providers. The average number of providers in each county is equal to 53.
When analyzing census tracts, 40 % of the census tracts (953 out of 1951) have zero providers, and 50 % of the remaining census tracts have less than 4 providers. The average number of providers in each census tract is equal to 8, and the standard deviation is equal to 17 providers.
In California, at the county level, two counties have zero providers, and 50 % of the remaining counties have less than 164 providers. The average number of providers in each county is equal to 593. At the census tract level, 54 % of the census tracts (4354 out of 7984) have zero providers, and 50 % of the remaining tracts have fewer than 4 providers. The average number of providers in each census tract is equal to 8, and the standard deviation is equal to 15 providers.
Information about the provider distribution for Georgia (top) and California (bottom). On the left, boxplot of the distribution of the number of providers per 100,000 children at the census tract level and the county level are shown. On the right, histograms of the distribution of the total number of providers per 100,000 children at the census tract level and the county level are shown.
Additional Tables and Figures
Procedure to Compute Providers’ Medicaid Acceptance Ratio at County Level
-
1.
Data used
-
The Medicaid claims data: specifically the OT (other services) file and PS (personal summary) file.
-
NPI data: This data is used to locate the number of providers in each state.
-
Zip code to county code crosswalk: map from zip code to the county it resides. The crosswalk can be downloaded here: http://www.huduser.org/portal/datasets/usps_crosswalk.html.
-
-
2.
Assumptions
-
Billing Provider ID behaves like NPI where it has a one-to-one match with the actual provider.
-
The county with the greatest number of visits from a provider is the county where the provider is located.
-
-
3.
Procedure
-
Calculation of providers in each county.
-
Convert the zip code of the providers in the NPI data into county code using the zip code-county code crosswalk.
-
Count the number of providers in each county.
-
-
Calculation of providers that accept Medicaid in each county.
-
Join the OT file and PS file in the claims data to get patient’s zip code for each of the claims.
-
Covert the zip code into county code using the zip code-county code crosswalk.
-
Count the number of providers in each county that accepts Medicaid.
-
-
Calculation of the Medicaid acceptance ratio
-
Divide the number of providers accepting Medicaid by the total number of providers in each county.
-
-
The resulting ratios for the state of Georgia and California are provided in Table 5.
Appendix 2: Main Steps to Compute Values of the Parameters for the Optimization Model
-
1.
Summary...................................................................................................................................2
-
2.
Medicaid Eligibility for Children in GA after ACA................................................................2
-
3.
Data Sources............................................................................................................................3
-
PCT3: Sex by Age...................................................................................................................4
-
B17024: Age by Ratio of Income to Poverty Level in the Past 12 Months............................5
-
PCT10: Household by Presence of People under 18 by Household Type by Age of People Under 18 Years...............................................................................6
-
PCT7: Average Household Size by Age...............................................................................7
-
B19001: Household Income in the Past 12 Months (in 2012 Inflation-Adjusted Dollars)....7
-
B08201: Household Size by Vehicles Available....................................................................8
-
-
4.
Procedure to Obtain the Desired Parameter Values..............................................................9
-
1.
Summary
This appendix explains the main steps we carried out to obtain the information needed to calculate the values of the parameters for the mathematical model described in the paper. The parameters are specified considering both CHIP and Medicaid eligibility criteria for children in Georgia and California after the Affordable Care Act (ACA). The steps are explained considering numerical examples for the state of Georgia. Similar steps were carried out when considering the state of California.
-
2.
Medicaid Eligibility for Children in GA after ACA
We defined three age classes:
-
Age class 1: children under 1 year of age (i.e., the child has not yet reached his or her first birthday)
-
Age class 2: children at least 1 year old and less than 6 years old (i.e., the child is age 1 or older, but has not yet reached his or her sixth birthday)
-
Age class 3: children at least 6 years old and no more than 19 years old (i.e., the child is age 6 or older, but has not yet reached his or her 19th birthday)
To be eligible for Medicaid after the ACA, a child in age class 1, age class 2, and age class 3 must be living in a household with an income below 205, 149, and 133 % of the Federal Poverty Level (FPL), respectively.
To be eligible for CHIP insurance after the ACA in the state of Georgia, a child in any age class must be living in a household with an income below 247 % of the FLP. We consider eligible for Medicaid/CHIP insurance those children that have access to either Medicaid or CHIP.
For each census tract in Georgia, we need to compute the values of the following parameters:
-
1.
Age class 1: the total number of children in age class 1
-
2.
Age class 2: the total number of children in age class 2
-
3.
Age class 3: the total number of children in age class 3
-
4.
Total population <= 18: the total number of children who are no more than 18 years old
-
5.
Age class 1 eligible: the total number of children in age class 1 who are eligible for Medicaid (parameter p M i1 in the optimization model)
-
6.
Age class 2 eligible: the total number of children in age class 2 who are eligible for Medicaid (parameter p M i2 in the optimization model)
-
7.
Age class 3 eligible: the total number of children in age class 3 who are eligible for Medicaid (parameter p M i3 in the optimization model)
-
8.
Total eligible population <= 18: the total number of children no more than 18 years old who are eligible for Medicaid
-
9.
mob_med: the proportion of households with at least one child less than 18 years old that have at least one vehicle and are eligible for Medicaid (parameter mob M i in the optimization model)
-
10.
mob_oth: the proportion of households with at least one child less than 18 years old that have at least one vehicle and are ineligible for Medicaid (parameter mob O i in the optimization model)
Parameters p O ik , k = 1, 2, 3 in the optimization model were computed as the difference between the total number of children in census tract i and age class k minus the total number of children in census tract i and age class k who are eligible for Medicaid/CHIP (i.e., age class k eligible).
-
-
3
Data Sources
The primary data sources are the 2010 SF2 100 % census data and the 2012 American Community Survey data, downloaded from the website: http://factfinder2.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t.
Remarks on data processing:
-
Tract names and locations specified by a unique Geographic Identifier code (GEOID) can be found in any census table.
-
Data from tracts present in the ACS data but not in the census data are ignored.
We used the following tables:
-
PCT3: Sex by Age
-
B17024: Age by Ratio of Income to Poverty Level in the Past 12 Months
-
PCT10: Household by Presence of People under 18 by Household Type by Age of People Under 18 Years
-
PCT7: Average Household Size by Age
-
B19001: Household Income in the Past 12 Months (in 2012 Inflation-Adjusted Dollars)
-
B08201: Household Size by Vehicles Available
A snapshot and a brief explanation of each table are provided in the tables below.
PCT3: Sex by Age
This table lists the total number of people of a particular age and sex in each census tract. Using this table, we find the total population within a specific age range.
Snapshot 1:
Census track 9501, Appling County, Georgia | Census track 9502, Appling County, Georgia | Census track 9503, Appling County, Georgia | Census track 9504, Appling County, Georgia | Census track 9505, Appling County, Georgia | Census track 9601, Atkinson County, Georgia | Census track 9602, Atkinson County, Georgia | Census track 9603, Atkinson County, Georgia | Census track 9701, Bacon County, Georgia | Census track 9702.01, Bacon County, Georgia | Census track 9702.02, Bacon County, Georgia | Census track 9601, Baker County, Georgia | Census track 9602, Baker County, Georgia | Census track 9701, Baldwin County, Georgia | Census track 9702, Baldwin County, Georgia | Census track 9703, Baldwin County, Georgia | Census track 9704, Baldwin County, Georgia | Census track 9705, Baldwin County, Georgia | |
Total | 3190 | 4530 | 5176 | 1476 | 3864 | 2077 | 5053 | 1245 | 3057 | 4233 | 3806 | 2198 | 1253 | 5401 | 6883 | 6098 | 4336 | 7114 |
Male | 1507 | 2319 | 2534 | 746 | 1953 | 1035 | 2565 | 640 | 1540 | 2008 | 1943 | 1048 | 625 | 2629 | 3288 | 2920 | 1980 | 3414 |
Under 1 year | 32 | 27 | 34 | 13 | 30 | 16 | 40 | 0 | 23 | 30 | 19 | 14 | 9 | 30 | 63 | 42 | 21 | 29 |
1 year | 18 | 30 | 36 | 13 | 21 | 17 | 44 | 15 | 13 | 30 | 18 | 12 | 6 | 30 | 56 | 59 | 22 | 24 |
2 years | 14 | 34 | 44 | 6 | 35 | 23 | 44 | 6 | 23 | 45 | 29 | 12 | 4 | 36 | 71 | 35 | 23 | 21 |
3 years | 27 | 40 | 34 | 12 | 24 | 19 | 47 | 12 | 17 | 39 | 40 | 12 | 15 | 37 | 40 | 40 | 12 | 29 |
4 years | 10 | 32 | 47 | 8 | 26 | 15 | 41 | 13 | 16 | 34 | 33 | 15 | 7 | 51 | 52 | 46 | 22 | 25 |
5 years | 21 | 10 | 10 | 15 | 23 | 16 | 37 | 9 | 21 | 29 | 23 | 13 | 7 | 35 | 15 | 55 | 18 | 23 |
6 years | 17 | 31 | 37 | 12 | 22 | 13 | 51 | 0 | 21 | 20 | 30 | 15 | 1 | 45 | 63 | 38 | 15 | 20 |
7 years | 28 | 34 | 31 | 7 | 17 | 16 | 37 | 12 | 24 | 23 | 21 | 14 | 8 | 40 | 60 | 45 | 27 | 28 |
8 years | 21 | 38 | 43 | 7 | 37 | 17 | 40 | 11 | 19 | 41 | 27 | 18 | 5 | 37 | 45 | 40 | 17 | 20 |
9 years | 17 | 50 | 35 | 14 | 18 | 15 | 33 | 6 | 15 | 26 | 29 | 15 | 10 | 38 | 45 | 25 | 21 | 24 |
10 years | 19 | 35 | 35 | 8 | 34 | 21 | 34 | 11 | 21 | 39 | 20 | 8 | 13 | 34 | 45 | 33 | 19 | 29 |
11 years | 23 | 17 | 36 | 9 | 20 | 17 | 31 | 6 | 18 | 30 | 17 | 12 | 9 | 50 | 31 | 35 | 17 | 18 |
12 years | 28 | 40 | 48 | 5 | 29 | 22 | 48 | 7 | 26 | 32 | 29 | 9 | 8 | 46 | 44 | 28 | 20 | 19 |
13 years | 22 | 30 | 41 | 16 | 29 | 24 | 40 | 5 | 31 | 25 | 19 | 8 | 8 | 39 | 50 | 35 | 12 | 17 |
14 years | 33 | 34 | 40 | 12 | 30 | 11 | 52 | 9 | 19 | 33 | 19 | 17 | 10 | 35 | 36 | 48 | 14 | 17 |
15 years | 33 | 40 | 34 | 3 | 32 | 10 | 43 | 16 | 28 | 36 | 16 | 17 | 7 | 44 | 48 | 35 | 21 | 25 |
16 years | 35 | 30 | 50 | 10 | 32 | 19 | 42 | 8 | 21 | 32 | 26 | 15 | 10 | 46 | 34 | 40 | 24 | 19 |
17 years | 22 | 31 | 38 | 10 | 37 | 10 | 49 | 9 | 22 | 27 | 22 | 13 | 10 | 38 | 37 | 50 | 22 | 27 |
18 years | 21 | 42 | 44 | 9 | 23 | 14 | 45 | 8 | 15 | 21 | 27 | 16 | 5 | 50 | 45 | 42 | 31 | 133 |
19 years | 17 | 33 | 31 | 11 | 23 | 14 | 40 | 10 | 18 | 14 | 29 | 15 | 7 | 20 | 46 | 28 | 78 | 348 |
20 years | 24 | 37 | 30 | 8 | 23 | 20 | 41 | 7 | 13 | 23 | 37 | 21 | 6 | 32 | 60 | 39 | 107 | 271 |
21 years | 11 | 30 | 19 | 1 | 20 | 25 | 13 | 9 | 16 | 23 | 32 | 20 | 8 | 31 | 79 | 33 | 126 | 233 |
22 years | 20 | 42 | 35 | 7 | 20 | 13 | 28 | 9 | 19 | 37 | 31 | 10 | 5 | 21 | 83 | 29 | 113 | 179 |
23 years | 21 | 32 | 37 | 3 | 11 | 14 | 31 | 5 | 14 | 29 | 18 | 16 | 7 | 23 | 66 | 28 | 79 | 106 |
24 years | 14 | 44 | 34 | 8 | 27 | 5 | 39 | 12 | 25 | 31 | 34 | 16 | 4 | 30 | 81 | 37 | 59 | 56 |
25 years | 9 | 31 | 30 | 6 | 23 | 13 | 33 | 14 | 15 | 24 | 27 | 12 | 1 | 27 | 68 | 31 | 45 | 50 |
26 years | 10 | 33 | 40 | 11 | 33 | 17 | 34 | 7 | 14 | 16 | 38 | 8 | 7 | 20 | 48 | 42 | 31 | 37 |
27 years | 28 | 39 | 33 | 5 | 18 | 10 | 36 | 8 | 21 | 21 | 16 | 8 | 6 | 19 | 50 | 35 | 25 | 32 |
28 years | 15 | 36 | 40 | 11 | 16 | 10 | 40 | 5 | 17 | 18 | 33 | 9 | 7 | 29 | 36 | 25 | 26 | 27 |
Female | 1583 | 2211 | 2642 | 730 | 1911 | 1042 | 2488 | 605 | 1517 | 2225 | 1863 | 1150 | 628 | 2772 | 3595 | 3178 | 2356 | 3700 |
Under 1 year | 20 | 32 | 33 | 8 | 24 | 22 | 43 | 8 | 21 | 25 | 40 | 11 | 8 | 29 | 31 | 43 | 15 | 23 |
1 year | 18 | 33 | 43 | 5 | 31 | 15 | 40 | 10 | 24 | 39 | 34 | 25 | 4 | 36 | 59 | 37 | 15 | 19 |
2 years | 24 | 48 | 35 | 11 | 31 | 21 | 37 | 6 | 19 | 33 | 27 | 15 | 10 | 34 | 58 | 43 | 24 | 20 |
3 years | 12 | 31 | 44 | 3 | 29 | 15 | 47 | 4 | 27 | 29 | 23 | 16 | 4 | 33 | 58 | 47 | 16 | 22 |
4 years | 32 | 39 | 25 | 13 | 35 | 15 | 48 | 9 | 18 | 33 | 24 | 15 | 6 | 34 | 52 | 45 | 7 | 19 |
5 years | 22 | 30 | 41 | 11 | 27 | 30 | 33 | 9 | 22 | 30 | 30 | 11 | 6 | 27 | 53 | 36 | 29 | 28 |
6 years | 22 | 30 | 49 | 11 | 29 | 12 | 43 | 5 | 27 | 32 | 25 | 11 | 7 | 39 | 42 | 33 | 18 | 33 |
7 years | 20 | 33 | 33 | 6 | 24 | 14 | 40 | 15 | 17 | 36 | 33 | 18 | 10 | 37 | 44 | 39 | 16 | 24 |
8 years | 25 | 28 | 34 | 3 | 28 | 16 | 34 | 7 | 30 | 39 | 27 | 23 | 9 | 40 | 50 | 37 | 15 | 23 |
9 years | 20 | 27 | 36 | 12 | 27 | 18 | 41 | 9 | 14 | 29 | 27 | 14 | 7 | 40 | 49 | 40 | 13 | 15 |
10 years | 19 | 43 | 32 | 5 | 17 | 18 | 33 | 11 | 15 | 30 | 32 | 20 | 5 | 47 | 43 | 47 | 26 | 16 |
11 years | 23 | 30 | 38 | 15 | 28 | 14 | 48 | 12 | 29 | 21 | 23 | 13 | 9 | 38 | 38 | 41 | 17 | 31 |
12 years | 28 | 32 | 28 | 3 | 25 | 18 | 51 | 11 | 29 | 34 | 19 | 23 | 12 | 45 | 42 | 50 | 11 | 19 |
13 years | 28 | 34 | 42 | 8 | 33 | 16 | 41 | 5 | 24 | 40 | 33 | 11 | 9 | 45 | 30 | 25 | 14 | 16 |
14 years | 19 | 11 | 24 | 6 | 29 | 16 | 40 | 7 | 16 | 36 | 20 | 11 | 8 | 44 | 30 | 24 | 18 | 26 |
15 years | 23 | 16 | 39 | 8 | 19 | 8 | 37 | 7 | 13 | 32 | 28 | 13 | 10 | 33 | 31 | 35 | 14 | 24 |
16 years | 15 | 33 | 35 | 8 | 17 | 21 | 38 | 6 | 22 | 25 | 21 | 12 | 7 | 38 | 38 | 37 | 20 | 8 |
17 years | 18 | 34 | 37 | 8 | 24 | 9 | 45 | 15 | 10 | 18 | 27 | 12 | 10 | 41 | 42 | 37 | 25 | 24 |
18 years | 14 | 33 | 30 | 10 | 36 | 20 | 36 | 7 | 21 | 38 | 24 | 11 | 9 | 28 | 36 | 42 | 59 | 284 |
19 years | 18 | 21 | 27 | 13 | 27 | 16 | 38 | 11 | 14 | 19 | 15 | 20 | 3 | 33 | 51 | 41 | 111 | 572 |
20 years | 19 | 24 | 25 | 6 | 15 | 14 | 40 | 7 | 22 | 33 | 19 | 15 | 6 | 17 | 59 | 36 | 172 | 496 |
21 years | 19 | 20 | 24 | 2 | 27 | 12 | 23 | 4 | 19 | 21 | 22 | 10 | 6 | 24 | 85 | 39 | 185 | 338 |
22 years | 17 | 18 | 20 | 10 | 13 | 8 | 27 | 7 | 11 | 19 | 13 | 16 | 10 | 26 | 114 | 48 | 132 | 214 |
23 years | 20 | 28 | 28 | 6 | 22 | 9 | 24 | 11 | 17 | 26 | 22 | 12 | 5 | 25 | 81 | 47 | 60 | 100 |
24 years | 8 | 19 | 39 | 7 | 17 | 15 | 33 | 10 | 17 | 22 | 24 | 9 | 7 | 28 | 68 | 38 | 36 | 51 |
25 years | 18 | 27 | 18 | 5 | 29 | 18 | 31 | 10 | 12 | 29 | 13 | 14 | 6 | 30 | 70 | 37 | 25 | 33 |
26 years | 17 | 30 | 34 | 15 | 23 | 14 | 29 | 10 | 18 | 28 | 26 | 20 | 7 | 31 | 53 | 42 | 39 | 31 |
27 years | 15 | 25 | 25 | 12 | 22 | 10 | 35 | 9 | 20 | 25 | 27 | 15 | 4 | 32 | 58 | 44 | 26 | 32 |
28 years | 12 | 24 | 29 | 7 | 17 | 14 | 31 | 10 | 22 | 35 | 24 | 18 | 4 | 32 | 54 | 36 | 28 | 26 |
B17024: Age by Ratio of Income to Poverty Level in the Past 12 Months
This table lists the number of people in a particular age group and income to poverty level ratio intervals for each census tract. This table is used to determine the proportion of Medicaid eligible children based on age and income.
Snapshot 2:
Census Tract 9501, Appling County, Georgia | Census Tract 9502, Appling County, Georgia | Census Tract 9503, Appling County, Georgia | Census Tract 9504, Appling County, Georgia | Census Tract 9505, Appling County, Georgia | Census Tract 9601, Atkinson County, Georgia | Census Tract 9602, Atkinson County, Georgia | Census Tract 9603, Atkinson County, Georgia | Census Tract 9701, Bacon County, Georgia | ||||||||||
Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | |
Total | 3009 | +/−428 | 4363 | +/−453 | 5092 | +/−491 | 1353 | +/−284 | 4099 | +/−455 | 2254 | +/−301 | 4832 | +/−382 | 1230 | +/−367 | 2674 | +/−405 |
Under 6 years | 176 | +/−100 | 354 | +/−129 | 449 | +/−132 | 53 | +/−41 | 313 | +/−118 | 224 | +/−107 | 509 | +/−91 | 135 | +/−92 | 175 | +/−111 |
Under .50 | 0 | +/−13 | 26 | +/−30 | 113 | +/−101 | 0 | +/−13 | 32 | +/−39 | 120 | +/−111 | 132 | +/−66 | 26 | +/−34 | 0 | +/−13 |
.50 to .74 | 28 | +/−44 | 60 | +/−54 | 59 | +/−75 | 0 | +/−13 | 0 | +/−13 | 24 | +/−24 | 52 | +/−54 | 47 | +/−66 | 0 | +/−13 |
.75 to .99 | 0 | +/−13 | 100 | +/−88 | 80 | +/−111 | 0 | +/−13 | 28 | +/−48 | 9 | +/−13 | 79 | +/−51 | 0 | +/−13 | 15 | +/−27 |
1.00 to 1.24 | 0 | +/−13 | 32 | +/−47 | 0 | +/−19 | 0 | +/−13 | 72 | +/−64 | 14 | +/−16 | 25 | +/−26 | 0 | +/−13 | 0 | +/−13 |
1.25 to 1.49 | 0 | +/−13 | 31 | +/−54 | 0 | +/−19 | 0 | +/−13 | 7 | +/−11 | 9 | +/−14 | 73 | +/−69 | 0 | +/−13 | 0 | +/−13 |
1.50 to 1.74 | 9 | +/−15 | 0 | +/−13 | 88 | +/−93 | 8 | +/−12 | 0 | +/−13 | 0 | +/−13 | 27 | +/−30 | 0 | +/−13 | 0 | +/−13 |
1.75 to 1.84 | 21 | +/−34 | 24 | +/−38 | 0 | +/−19 | 0 | +/−13 | 106 | +/−80 | 0 | +/−13 | 34 | +/−50 | 0 | +/−13 | 36 | +/−63 |
1.85 to 1.99 | 0 | +/−13 | 16 | +/−27 | 0 | +/−19 | 0 | +/−13 | 0 | +/−13 | 15 | +/−25 | 12 | +/−19 | 7 | +/−12 | 0 | +/−13 |
2.00 to 2.99 | 10 | +/−18 | 60 | +/−61 | 0 | +/−19 | 26 | +/−30 | 12 | +/−20 | 12 | +/−15 | 43 | +/−44 | 35 | +/−44 | 28 | +/−37 |
3.00 to 3.99 | 37 | +/−41 | 5 | +/−9 | 23 | +/−32 | 0 | +/−13 | 27 | +/−41 | 11 | +/−21 | 32 | +/−39 | 0 | +/−13 | 48 | +/−66 |
4.00 to 4.99 | 26 | +/−42 | 0 | +/−13 | 86 | +/−113 | 19 | +/−26 | 0 | +/−13 | 2 | +/−16 | 0 | +/−13 | 20 | +/−32 | 23 | +/−40 |
5.00 and over | 45 | +/−54 | 0 | +/−13 | 0 | +/−19 | 0 | +/−13 | 29 | +/−37 | 8 | +/−14 | 0 | +/−13 | 0 | +/−13 | 25 | +/−40 |
6 to 11 years | 315 | +/−133 | 496 | +/−162 | 492 | 189 | 74 | +/−56 | 360 | +/−123 | 208 | +/−63 | 376 | +/−101 | 127 | +/−82 | 235 | +/−108 |
Under .50 | 0 | +/−13 | 51 | +/−58 | 96 | +/−99 | 0 | +/−13 | 91 | +/−81 | 84 | +/−61 | 96 | +/−53 | 32 | +/−45 | 0 | +/−13 |
.50 to .74 | 0 | +/−13 | 87 | +/−89 | 94 | +/−126 | 0 | +/−13 | 38 | +/−66 | 49 | +/−46 | 26 | +/−32 | 17 | +/−25 | 0 | +/−13 |
.75 to .99 | 0 | +/−13 | 105 | +/−80 | 21 | +/−34 | 13 | +/−18 | 43 | +/−49 | 14 | +/−16 | 100 | +/−66 | 0 | +/−13 | 54 | +/−73 |
1.00 to 1.24 | 97 | +/−107 | 53 | +/−50 | 19 | +/−30 | 0 | +/−13 | 25 | +/−36 | 15 | +/−17 | 0 | +/−13 | 0 | +/−13 | 52 | +/−48 |
1.25 to 1.49 | 0 | +/−13 | 23 | +/−31 | 0 | +/−19 | 0 | +/−13 | 15 | +/−24 | 3 | +/−5 | 27 | +/−24 | 12 | +/−22 | 0 | +/−13 |
1.50 to 1.74 | 36 | +/−39 | 0 | +/−13 | 23 | +/−36 | 38 | +/−51 | 30 | +/−41 | 0 | +/−13 | 57 | +/−37 | 0 | +/−13 | 0 | +/−13 |
1.75 to 1.84 | 11 | +/−20 | 0 | +/−13 | 0 | +/−19 | 0 | +/−13 | 32 | +/−26 | 0 | +/−13 | 0 | +/−13 | 0 | +/−13 | 0 | +/−13 |
1.85 to 1.99 | 0 | +/−13 | 0 | +/−13 | 0 | +/−19 | 0 | +/−13 | 0 | +/−13 | 9 | +/−15 | 15 | +/−26 | 5 | +/−10 | 0 | +/−13 |
2.00 to 2.99 | 86 | +/−74 | 86 | +/−106 | 105 | +/−75 | 23 | +/−26 | 0 | +/−13 | 16 | +/−28 | 31 | +/−34 | 61 | +/−55 | 11 | +/−19 |
3.00 to 3.99 | 37 | +/−44 | 44 | +/−45 | 40 | +/−63 | 0 | +/−13 | 35 | +/−51 | 9 | +/−17 | 6 | +/−10 | 0 | +/−13 | 60 | +/−93 |
4.00 to 4.99 | 0 | +/−13 | 18 | +/−28 | 71 | +/−74 | 0 | +/−13 | 37 | +/−53 | 9 | +/−19 | 18 | +/−27 | 0 | +/−13 | 11 | +/−19 |
5.00 and over | 48 | +/−47 | 26 | +/−28 | 23 | +/−37 | 0 | +/−13 | 14 | +/−24 | 0 | +/−13 | 0 | +/−13 | 0 | +/−13 | 47 | +/−51 |
12 to 17 years | 310 | +/−177 | 430 | +/−131 | 338 | +/−100 | 97 | +/−56 | 423 | +/−168 | 265 | +/−84 | 510 | +/−119 | 114 | +/−81 | 214 | +/−96 |
Under .50 | 10 | +/−16 | 71 | +/−55 | 31 | +/−34 | 20 | +/−28 | 64 | +/−77 | 27 | +/−22 | 47 | +/−40 | 8 | +/−12 | 0 | +/−13 |
.50 to .74 | 0 | +/−13 | 39 | +/−43 | 0 | +/−19 | 0 | +/−13 | 26 | +/−30 | 55 | +/−59 | 16 | +/−23 | 25 | +/−40 | 0 | +/−13 |
.75 to 99 | 0 | +/−13 | 71 | +/−74 | 13 | +/−21 | 14 | +/−18 | 3 | +/−5 | 23 | +/−34 | 99 | +/−62 | 0 | +/−13 | 0 | +/−13 |
1.00 to 1.24 | 117 | +/−135 | 58 | +/−69 | 0 | +/−19 | 15 | +/−27 | 30 | +/−29 | 44 | +/−39 | 10 | +/−15 | 0 | +/−13 | 90 | +/−73 |
1.25 to 1.49 | 30 | +/−52 | 38 | +/−59 | 6 | +/−12 | 9 | +/−15 | 21 | +/−31 | 20 | +/−25 | 44 | +/−37 | 32 | +/−47 | 0 | +/−13 |
1.50 to 1.74 | 0 | +/−13 | 54 | +/−62 | 23 | +/−38 | 0 | +/−13 | 12 | +/−17 | 0 | +/−13 | 101 | +/−87 | 19 | +/−34 | 0 | +/−13 |
1.75 to 1.84 | 22 | +/−3435 | 24 | +/−3438 | 0 | +/−3419 | 0 | +/−3413 | 86 | +/−3465 | 0 | +/−3413 | 7 | +/−3410 | 0 | +/−3413 | 27 | +/−3442 |
1.85 to 1.99 | 29 | +/−51 | 0 | +/−13 | 0 | +/−19 | 3 | +/−5 | 0 | +/−13 | 0 | +/−13 | 0 | +/−13 | 4 | +/−8 | 0 | +/−13 |
2.00 to 2.99 | 14 | +/−26 | 39 | +/−45 | 127 | +/−90 | 8 | +/−14 | 86 | +/−97 | 0 | +/−13 | 114 | +/−79 | 0 | +/−13 | 24 | +/−38 |
3.00 to 3.99 | 27 | +/−44 | 7 | +/−12 | 18 | +/−29 | 0 | +/−13 | 44 | +/−46 | 18 | +/−25 | 4 | +/−6 | 0 | +/−13 | 13 | +/−22 |
4.00 to 4.99 | 61 | +/−70 | 0 | +/−13 | 60 | +/−76 | 28 | +/−33 | 38 | +/−39 | 2 | +/−5 | 53 | +/−76 | 20 | +/−34 | 18 | +/−25 |
5.00 and over | 0 | +/−13 | 29 | +/−31 | 60 | +/−60 | 0 | +/−13 | 13 | +/−22 | 76 | +/−48 | 15 | +/−19 | 6 | +/−10 | 42 | +/−40 |
18 to 24 years | 159 | +/−105 | 266 | +/−131 | 469 | +/−214 | 126 | +/−81 | 236 | +/−121 | 154 | +/−80 | 527 | +/−116 | 54 | +/−58 | 280 | +/−129 |
Under .50 | 0 | +/−13 | 14 | +/−24 | 30 | +/−48 | 0 | +/−13 | 35 | +/−32 | 0 | +/−13 | 128 | +/−61 | 0 | +/−13 | 28 | +/−35 |
.50 to .74 | 37 | +/−52 | 12 | +/−20 | 24 | +/−48 | 0 | +/−13 | 4 | +/−7 | 24 | +/−36 | 54 | +/−59 | 17 | +/−28 | 14 | +/−27 |
.75 to .99 | 0 | +/−13 | 96 | +/−114 | 0 | +/−19 | 10 | +/−19 | 0 | +/−13 | 13 | +/−22 | 49 | +/−41 | 0 | +/−13 | 0 | +/−13 |
1.00 to 1.24 | 0 | +/−13 | 36 | +/−54 | 0 | +/−19 | 1 | +/−2 | 5 | +/−9 | 30 | +/−33 | 22 | +/−19 | 0 | +/−13 | 0 | +/−13 |
1.25 to 1.49 | 0 | +/−13 | 0 | +/−13 | 15 | +/−29 | 0 | +/−13 | 13 | +/−20 | 5 | +/−10 | 5 | +/−10 | 0 | +/−13 | 0 | +/−13 |
1.50 to 1.74 | 0 | +/−13 | 0 | +/−13 | 97 | +/−127 | 10 | +/−15 | 43 | +/−54 | 0 | +/−13 | 43 | +/−44 | 0 | +/13 | 0 | +/−13 |
1.75 to 1.84 | 0 | +/−13 | 0 | +/−13 | 0 | +/−19 | 0 | +/−13 | 0 | +/−13 | 44 | +/−53 | 13 | +/−15 | 0 | +/−13 | 0 | +/−13 |
1.85 to 1.99 | 0 | +/−13 | 0 | +/−13 | 0 | +/−19 | 3 | +/−5 | 0 | +/−13 | 0 | +/−13 | 0 | +/−13 | 7 | +/−13 | 0 | +/−13 |
2.00 to 2.99 | 30 | +/−55 | 35 | +/−44 | 247 | +/−208 | 44 | +/−52 | 83 | +/−89 | 16 | +/−22 | 142 | +/−93 | 0 | +/−13 | 29 | +/−36 |
3.00 to 3.99 | 51 | +/−50 | 37 | +/−40 | 0 | +/−19 | 38 | +/−51 | 3 | +/−6 | 22 | +/−28 | 43 | +/−47 | 30 | +/−44 | 87 | +/−91 |
4.00 to 4.99 | 17 | +/−34 | 0 | +/−13 | 0 | +/−19 | 0 | +/−13 | 28 | +/−45 | 0 | +/−13 | 28 | +/−42 | 0 | +/−13 | 26 | +/−34 |
5.00 and over | 24 | +/−40 | 36 | +/−54 | 56 | +/−67 | 20 | +/−25 | 22 | +/−34 | 0 | +/−13 | 0 | +/−13 | 0 | +/−13 | 96 | +/−76 |
PCT10: Household by Presence of People under 18 by Household Type by Age of People under 18 Years
This table lists the number of households that include a child of a particular age range, divided by the type of household (e.g., one with both a husband and wife). This table is used to find the total number of households with a child in each age group.
Snapshot 3:
Census Tract 9501, Appling County Georgia | Census Tract 9502, Appling County Georgia | Census Tract 9503, Appling County Georgia | Census Tract 9504, Appling County Georgia | Census Tract 9505, Appling County Georgia | Census Tract 9601, Atkinson County Georgia | Census Tract 9602, Atkinson County Georgia | Census Tract 9603, Atkinson County Georgia | Census Tract 9701, Bacon County Georgia | Census Tract 9702.01, Bacon County Georgia | Census Tract 9702.02, Bacon County Georgia | Census Tract 9601, Baker County Georgia | Census Tract 9602, Baker County Georgia | Census Tract 9701, Baldwin County Georgia | Census Tract 9702, Baldwin County Georgia | Census Tract 9703, Baldwin County Georgia | Census Tract 9704, Baldwin County Georgia | Census Tract 9705, Baldwin County Georgia | |
Total | 1270 | 1631 | 1969 | 606 | 1493 | 770 | 1763 | 450 | 1167 | 1606 | 1441 | 862 | 510 | 2075 | 2882 | 2437 | 1810 | 2132 |
Households with one or more people under 18 years | 436 | 612 | 696 | 170 | 522 | 300 | 752 | 178 | 416 | 594 | 504 | 271 | 141 | 755 | 910 | 803 | 375 | 444 |
Family households: | 433 | 608 | 680 | 170 | 514 | 298 | 737 | 176 | 406 | 589 | 500 | 266 | 139 | 747 | 905 | 798 | 372 | 440 |
Husband-wife family | 326 | 324 | 421 | 124 | 360 | 171 | 471 | 129 | 303 | 325 | 300 | 150 | 94 | 447 | 407 | 511 | 159 | 203 |
Under 6 years only | 79 | 64 | 86 | 31 | 79 | 43 | 98 | 27 | 64 | 65 | 67 | 35 | 19 | 94 | 112 | 144 | 48 | 40 |
Under 6 years and 6 to 17 years | 58 | 88 | 121 | 37 | 78 | 54 | 133 | 30 | 69 | 90 | 72 | 37 | 22 | 108 | 91 | 122 | 29 | 41 |
6 to 17 years only | 189 | 172 | 214 | 56 | 203 | 74 | 240 | 72 | 170 | 170 | 161 | 78 | 53 | 245 | 204 | 245 | 82 | 122 |
Other family | 107 | 284 | 259 | 46 | 154 | 127 | 266 | 47 | 103 | 264 | 200 | 116 | 45 | 300 | 498 | 287 | 213 | 237 |
Male householder, no wife present | 31 | 69 | 72 | 12 | 61 | 28 | 69 | 23 | 46 | 37 | 47 | 19 | 11 | 61 | 68 | 50 | 35 | 25 |
Under 6 years only | 7 | 24 | 17 | 2 | 17 | 3 | 19 | 5 | 15 | 10 | 15 | 3 | 2 | 12 | 26 | 13 | 10 | 7 |
Under 6 years and 6 to 17 years | 5 | 19 | 12 | 0 | 8 | 7 | 9 | 6 | 7 | 5 | 7 | 2 | 1 | 12 | 9 | 11 | 8 | 4 |
6 to 17 years only | 19 | 26 | 43 | 10 | 36 | 18 | 41 | 12 | 24 | 22 | 25 | 14 | 8 | 37 | 33 | 26 | 17 | 14 |
Female householder, no husband present. | 76 | 215 | 187 | 34 | 93 | 99 | 197 | 24 | 57 | 227 | 153 | 97 | 34 | 239 | 430 | 237 | 178 | 212 |
Under 6 years only | 22 | 34 | 45 | 9 | 22 | 27 | 47 | 7 | 7 | 76 | 37 | 24 | 7 | 44 | 121 | 57 | 34 | 66 |
Under 6 years and 6 to 17 years | 8 | 61 | 53 | 6 | 27 | 30 | 44 | 4 | 14 | 45 | 42 | 25 | 8 | 50 | 118 | 53 | 37 | 46 |
6 to 17 years only | 46 | 120 | 89 | 19 | 44 | 42 | 106 | 13 | 36 | 106 | 74 | 48 | 19 | 145 | 191 | 127 | 107 | 100 |
Nonfamily households | 3 | 4 | 16 | 0 | 8 | 2 | 15 | 2 | 10 | 5 | 4 | 5 | 2 | 8 | 5 | 5 | 3 | 4 |
Male householder | 3 | 2 | 16 | 0 | 7 | 2 | 14 | 1 | 10 | 4 | 4 | 4 | 1 | 5 | 1 | 3 | 1 | 3 |
Under 6 years only | 2 | 0 | 2 | 0 | 2 | 0 | 1 | 1 | 2 | 0 | 2 | 0 | 1 | 2 | 0 | 1 | 1 | 0 |
Under 6 years and 6 to 17 years | 1 | 0 | 2 | 0 | 1 | 0 | 3 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
6 to 17 years only | 0 | 2 | 12 | 0 | 4 | 2 | 10 | 0 | 8 | 4 | 2 | 3 | 0 | 3 | 1 | 2 | 0 | 2 |
Female householder | 0 | 2 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 3 | 4 | 2 | 2 | 1 |
Under 6 years only | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 4 | 0 | 2 | 0 |
Under 6 years and 6 to 17 years | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
6 to 17 years only | 0 | 2 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 0 | 1 |
Households with no people under 18 years | 834 | 1019 | 1273 | 436 | 971 | 470 | 1011 | 272 | 751 | 1012 | 937 | 591 | 369 | 1320 | 1972 | 1634 | 1435 | 1688 |
Family households | 477 | 510 | 657 | 267 | 578 | 248 | 541 | 159 | 463 | 524 | 478 | 291 | 196 | 806 | 892 | 938 | 484 | 438 |
Husband-wife family | 408 | 396 | 538 | 223 | 500 | 186 | 411 | 132 | 403 | 420 | 374 | 207 | 155 | 644 | 696 | 773 | 302 | 316 |
Other family | 69 | 114 | 119 | 44 | 78 | 62 | 130 | 27 | 60 | 104 | 104 | 84 | 41 | 162 | 196 | 165 | 182 | 122 |
Male householder, no wife present | 26 | 34 | 43 | 18 | 33 | 20 | 55 | 9 | 19 | 28 | 34 | 22 | 16 | 42 | 46 | 40 | 59 | 31 |
Female householder, no husband present | 43 | 80 | 76 | 26 | 45 | 42 | 75 | 18 | 41 | 76 | 70 | 62 | 25 | 120 | 150 | 125 | 123 | 91 |
Nonfamily households | 357 | 509 | 616 | 169 | 393 | 222 | 470 | 113 | 288 | 488 | 459 | 300 | 173 | 514 | 1080 | 696 | 951 | 1250 |
Male householder | 189 | 234 | 240 | 87 | 216 | 115 | 243 | 68 | 163 | 219 | 218 | 145 | 90 | 256 | 500 | 297 | 389 | 512 |
Female householder | 168 | 275 | 376 | 82 | 177 | 107 | 227 | 45 | 125 | 269 | 241 | 155 | 83 | 258 | 580 | 399 | 562 | 738 |
PCT7: Average Household Size by Age
This table provides the average size of a household, specifying the portions of adults and of children in the household. The data in this table is used to compute the total household average size to estimate the FPL in dollars.
Snapshot 4:
Census Tract 9501, Appling County, Georgia | Census Tract 9502, Appling County, Georgia | Census Tract 9503, Appling County, Georgia | Census Tract 9504, Appling County, Georgia | Census Tract 9505, Appling County, Georgia | Census Tract 9601, Atkinson County, Georgia | Census Tract 9602, Atkinson County, Georgia | Census Tract 9603, Atkinson County, Georgia | Census Tract 9701, Bacon County, Georgia | Census Tract 9702.01, Bacon County, Georgia | Census Tract 9702.02, Bacon County, Georgia | Census Tract 9601, Baker County, Georgia | Census Tract 9602, Baker County, Georgia | Census Tract 9701, Baldwin County, Georgia | Census Tract 9702, Baldwin County, Georgia | Census Tract 9703, Baldwin County, Georgia | Census Tract 9704, Baldwin County, Georgia | Census Tract 9705, Baldwin County, Georgia | |
Average household size | ||||||||||||||||||
Total | 2.49 | 2.61 | 2.57 | 2.44 | 2.59 | 2.70 | 2.85 | 2.77 | 2.62 | 2.55 | 2.51 | 2.55 | 2.46 | 2.60 | 2.38 | 2.50 | 2.28 | 2.43 |
Under 18 years | 0.61 | 0.76 | 0.69 | 0.53 | 0.65 | 0.78 | 0.85 | 0.73 | 0.65 | 0.71 | 0.65 | 0.60 | 0.56 | 0.67 | 0.58 | 0.59 | 0.36 | 0.39 |
18 years and over | 1.87 | 1.85 | 1.88 | 1.90 | 1.94 | 1.92 | 2.00 | 2.04 | 1.97 | 1.84 | 1.86 | 1.95 | 1.89 | 1.93 | 1.80 | 1.92 | 1.92 | 2.04 |
B19001: Household Income in the Past 12 Months (in 2012 Inflation-Adjusted Dollars)
This table lists the number of households in a particular income interval in dollars. The data in this table is used to determine the number of households below the FPL.
Snapshot 5:
Census Tract 9501, Appling County, Georgia | Census Tract 9502, Appling County, Georgia | Census Tract 9503, Appling County, Georgia | Census Tract 9504, Appling County, Georgia | Census Tract 9505, Appling County, Georgia | Census Tract 9601, Atkinson County, Georgia | Census Tract 9602, Atkinson County, Georgia | Census Tract 9603, Atkinson County, Georgia | Census Tract 9701, Bacon County, Georgia | ||||||||||
Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | |
Total: | 1189 | +/−145 | 1670 | +/−152 | 2099 | +/−230 | 583 | +/−111 | 1506 | +/−152 | 711 | +/−84 | 1634 | +/−133 | 374 | +/−71 | 976 | +/−124 |
Less than $10,000 | 55 | +/−44 | 154 | +/−61 | 283 | +/−125 | 59 | +/−34 | 162 | +/−70 | 108 | +/−46 | 341 | +/−84 | 26 | +/−31 | 135 | +/−75 |
$10,000 to $14,999 | 80 | +/−58 | 201 | +/−78 | 205 | +/−87 | 36 | +/−36 | 56 | +/−43 | 51 | +/−27 | 234 | +/−88 | 52 | +/−39 | 106 | +/−68 |
$15,000 to $19,999 | 89 | +/−62 | 141 | +/−65 | 146 | +/−112 | 75 | +/−46 | 182 | +/−78 | 111 | +/−52 | 56 | +/−34 | 25 | +/−30 | 23 | +/−36 |
$20,000 to $24,999 | 56 | +/−42 | 172 | +/−111 | 61 | +/−51 | 31 | +/−26 | 142 | +/−80 | 125 | +/−68 | 61 | +/−36 | 16 | +/−19 | 113 | +/−71 |
$25,000 to $29,999 | 113 | +/−76 | 108 | +/−65 | 122 | +/−108 | 32 | +/−26 | 92 | +/−58 | 22 | +/−18 | 133 | +/−64 | 37 | +/−33 | 66 | +/−37 |
$30,000 to $34,999 | 125 | +/−83 | 189 | +/−81 | 161 | +/−105 | 16 | +/−14 | 78 | +/−51 | 39 | +/−36 | 119 | +/−64 | 13 | +/−15 | 52 | +/−44 |
$35,000 to $39,999 | 108 | +/−61 | 138 | +/−71 | 93 | +/−86 | 43 | +/−30 | 115 | +/−77 | 16 | +/−15 | 118 | +/−69 | 51 | +/−41 | 28 | +/−32 |
$40,000 to $44,999 | 65 | +/−40 | 90 | +/−65 | 69 | +/−52 | 51 | +/−41 | 42 | +/−35 | 21 | +/−24 | 65 | +/−45 | 0 | +/−13 | 10 | +/−16 |
$45,000 to $49,999 | 24 | +/−25 | 43 | +/−41 | 144 | +/−117 | 7 | +/−8 | 49 | +/−46 | 4 | +/−8 | 72 | +/−46 | 0 | +/−13 | 45 | +/−37 |
$50,000 to $59,999 | 53 | +/−36 | 115 | +/−79 | 113 | +/−77 | 32 | +/−24 | 116 | +/−68 | 44 | +/−28 | 70 | +/−47 | 69 | +/−48 | 29 | +/−36 |
$60,000 to $74,999 | 71 | +/−67 | 122 | +/−66 | 183 | +/−95 | 98 | +/−49 | 137 | +/−75 | 22 | +/−17 | 116 | +/−51 | 43 | +/−31 | 69 | +/−44 |
$75,000 to $99,999 | 120 | +/−67 | 108 | +/−80 | 239 | +/−103 | 88 | +/−48 | 52 | +/−44 | 56 | +/−37 | 136 | +/−54 | 24 | +/−18 | 142 | +/−72 |
$100,000 to $124,999 | 139 | +/−64 | 62 | +/−54 | 180 | +/−88 | 0 | +/−13 | 168 | +/−94 | 33 | +/−33 | 69 | +/−52 | 18 | +/−20 | 76 | +/−49 |
$125,000 to $149,999 | 55 | +/−60 | 11 | +/−18 | 39 | +/−35 | 15 | +/−20 | 52 | +/−35 | 49 | +/−32 | 10 | +/−16 | 0 | +/−13 | 15 | +/−26 |
$150,000 to $199,999 | 24 | +/−28 | 16 | +/−18 | 54 | +/−66 | 0 | +/−13 | 29 | +/−28 | 0 | +/−13 | 34 | +/−24 | 0 | +/−13 | 51 | +/−45 |
$200,000 or more | 12 | +/−19 | 0 | +/−13 | 7 | +/−12 | 0 | +/−13 | 34 | +/−46 | 10 | +/−18 | 0 | +/−13 | 0 | +/13 | 16 | +/−27 |
B08201: Household Size by Vehicles Available
This table lists the number of households, both overall and by size category, with a given number of vehicles. We use this table to find the percentage of households with at least one vehicle.
Snapshot 6:
Census Tract 9501, Appling County, Georgia | Census Tract 9502, Appling County, Georgia | Census Tract 9503, Appling County, Georgia | Census Tract 9504, Appling County, Georgia | Census Tract 9505, Appling County, Georgia | Census Tract 9601, Atkinson County, Georgia | Census Tract 9602, Atkinson County, Georgia | Census Tract 9603, Atkinson County, Georgia | Census Tract 9701, Bacon County, Georgia | ||||||||||
Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | Estimate | Margin of error | |
Total | 1189 | +/−145 | 1670 | +/−152 | 2099 | +/−230 | 583 | +/−111 | 1506 | +/−152 | 711 | +/−84 | 1634 | +/−133 | 374 | +/−71 | 976 | +/−124 |
No vehicle available | 31 | +/−32 | 150 | +/−79 | 228 | +/−121 | 31 | +/−27 | 71 | +/−44 | 55 | +/−30 | 214 | +/−65 | 13 | +/−22 | 36 | +/−35 |
1 vehicle available | 339 | +/−122 | 676 | +/−149 | 728 | +/−176 | 209 | +/−69 | 468 | +/−138 | 317 | +/−75 | 638 | +/−127 | 56 | +/−35 | 321 | +/−119 |
2 vehicles available | 461 | +/−116 | 634 | +/−130 | 840 | +/−180 | 170 | +/−56 | 597 | +/−115 | 208 | +/−63 | 398 | +/−102 | 177 | +/−76 | 270 | +/−99 |
3 vehicles available | 246 | +/−99 | 146 | +/−64 | 250 | +/−116 | 154 | +/−64 | 283 | +/−88 | 70 | +/−41 | 286 | +/−100 | 97 | +/−53 | 232 | +/−91 |
4 or more vehicles available | 112 | +/−69 | 64 | +/−40 | 53 | +/−48 | 19 | +/−19 | 87 | +/−75 | 61 | +/−31 | 98 | +/−48 | 31 | +/−24 | 117 | +/−57 |
1-person household | 264 | +/−107 | 466 | +/−122 | 901 | +/−229 | 186 | +/−70 | 375 | +/−122 | 241 | +/−71 | 419 | +/−111 | 55 | +/−37 | 301 | +/−113 |
No vehicle available | 13 | +/−14 | 60 | +/−57 | 176 | +/−99 | 21 | +/−23 | 36 | +/−24 | 42 | +/−23 | 107 | +/−53 | 0 | +/−13 | 36 | +/−35 |
1 vehicle available | 173 | +/−96 | 280 | +/−80 | 447 | +/−163 | 119 | +/−55 | 272 | +/−115 | 140 | +/−64 | 250 | +/−98 | 20 | +/−19 | 213 | +/−99 |
2 vehicles available | 64 | +/−43 | 95 | +/−65 | 210 | +/−125 | 14 | +/−18 | 67 | +/−54 | 54 | +/−42 | 39 | +/−25 | 20 | +/−24 | 38 | +/−40 |
3 vehicles available | 14 | +/−21 | 31 | +/−36 | 68 | +/−86 | 32 | +/−24 | 0 | +/−13 | 5 | +/−8 | 23 | +/−26 | 0 | +/−13 | 14 | +/−25 |
4 or more vehicles available | 0 | +/−13 | 0 | +/−13 | 0 | +/−19 | 0 | +/−13 | 0 | +/−13 | 0 | +/−13 | 0 | +/−13 | 15 | +/−16 | 0 | +/−13 |
2-person household | 476 | +/−123 | 513 | +/−128 | 518 | +/−140 | 234 | +/−63 | 578 | +/−103 | 163 | +/−55 | 503 | +/−114 | 166 | +/−57 | 261 | +/−81 |
No vehicle available | 0 | +/−13 | 51 | +/−46 | 52 | +/−70 | 10 | +/−12 | 28 | +/−31 | 5 | +/−11 | 76 | +/−57 | 0 | +/−13 | 0 | +/−13 |
1 vehicle available | 76 | +/−48 | 184 | +/−95 | 77 | +/−66 | 49 | +/−32 | 112 | +/−66 | 70 | +/−34 | 150 | +/−61 | 16 | +/−19 | 70 | +/−54 |
2 vehicles available | 199 | +/−81 | 220 | +/−87 | 276 | +/−110 | 99 | +/−33 | 322 | +/−85 | 64 | +/−38 | 125 | +/−54 | 82 | +/−48 | 132 | +/−58 |
3 vehicles available | 161 | +/−84 | 38 | +/−42 | 105 | +/−63 | 64 | +/−38 | 116 | +/−48 | 24 | +/−24 | 120 | +/−64 | 68 | +/−45 | 47 | +/−34 |
4 or more vehicles available | 40 | +/−32 | 20 | +/−25 | 8 | +/−12 | 12 | +/−16 | 0 | +/−13 | 0 | +/−13 | 32 | +/−22 | 0 | +/−13 | 12 | +/−14 |
3-person household | 250 | +/−105 | 275 | +/−106 | 230 | +/−130 | 126 | +/−49 | 233 | +/−95 | 140 | +/−60 | 305 | +/−92 | 81 | +/−44 | 160 | +/−73 |
No vehicle available | 18 | +/−29 | 18 | +/−23 | 0 | +/−19 | 0 | +/−13 | 0 | +/−13 | 8 | +/−15 | 9 | +/−12 | 13 | +/−22 | 0 | +/−13 |
1 vehicle available | 70 | +/−65 | 43 | +/−34 | 87 | +/−103 | 41 | +/−31 | 19 | +/−27 | 71 | +/−46 | 127 | +/−56 | 20 | +/−23 | 0 | +/−13 |
2 vehicles available | 113 | +/−67 | 162 | +/−89 | 89 | +/−61 | 38 | +/−27 | 94 | +/−58 | 30 | +/−21 | 67 | +/−41 | 9 | +/−15 | 27 | +/−27 |
3 vehicles available | 0 | +/−13 | 30 | +/−32 | 54 | +/−48 | 40 | +/−35 | 86 | +/−58 | 22 | +/−24 | 71 | +/−66 | 23 | +/−28 | 87 | +/−55 |
4 or more vehicles available | 49 | +/−43 | 22 | +/−24 | 0 | +/−19 | 7 | +/−11 | 34 | +/−46 | 9 | +/−11 | 31 | +/−32 | 16 | +/−20 | 46 | +/−45 |
4- or more person household | 199 | +/−90 | 416 | +/−134 | 450 | +/−132 | 37 | +/−33 | 320 | +/−107 | 167 | +/−61 | 407 | +/−98 | 72 | +/−49 | 254 | +/−78 |
No vehicle available | 0 | +/−13 | 21 | +/−33 | 0 | +/−19 | 0 | +/−13 | 7 | +/−11 | 0 | +/−13 | 22 | +/−19 | 0 | +/−13 | 0 | +/−13 |
1 vehicle available | 20 | +/−27 | 169 | +/−98 | 117 | +/−95 | 0 | +/−13 | 65 | +/−44 | 36 | +/−23 | 111 | +/−57 | 0 | +/−13 | 38 | +/−43 |
2 vehicles available | 85 | +/−50 | 157 | +/−72 | 265 | +/−84 | 19 | +/−21 | 114 | +/−72 | 60 | +/−47 | 167 | +/−84 | 66 | +/−47 | 73 | +/−52 |
3 vehicles available | 71 | +/−68 | 47 | +/−35 | 23 | +/−40 | 18 | +/−24 | 81 | +/−52 | 19 | +/−24 | 72 | +/−35 | 6 | +/−11 | 84 | +/−54 |
4 or more vehicles available | 23 | +/−28 | 22 | +/−25 | 45 | +/−47 | 0 | +/−13 | 53 | +/−65 | 52 | +/−26 | 35 | +/−36 | 0 | +/−13 | 59 | +/−51 |
-
4.
Procedure to Obtain the Desired Parameter Values
In this section, we provide a numeric example of how we computed the model parameters. Examples are provided for one census tract (9501, Appling County, Georgia).
-
1.
Age class 1:
-
Using PCT3, sum the data in the columns corresponding to “Male: - Under 1 year” and “Female: - Under 1 year.”
Example (refer to Snapshot 1):
Age class 1 = 32 + 20 = 52
-
-
2.
Age class 2:
-
Using PCT3, sum the data in the columns corresponding to “Male: - 1 year” through “Male: - 5 years” and “Female: - 1 year” through “Female: - 5 years.”
Example (refer to Snapshot 1):
Age class 2 = (18 + 14 + 27 + 10 + 24) + (18 + 24 + 12 + 32 + 22) = 201
-
-
3.
Age class 3:
-
Using PCT3, sum the data in the columns corresponding to “Male: - 6 years” through “Male: - 18 years” and “Female: - 6 years” through “Female: - 18 years.”
Example (refer to Snapshot 1):
Age class 3 = (17 + 28 + 21 + 17 + 19 + 23 + 28 + 22 + 33 + 33 + 35 + 22 + 21) + (22 + 20 + 25 + 20 + 19 + 23 + 28 + 28 + 19 + 23 + 15 + 18 + 14) = 593
-
-
4.
Total Population <= 18:
-
Sum the values of age class 1, age class 2, and age class 3.
Example
Total Population <= 18 = 52 + 201 + 593 = 846
-
-
5.
Age class 1 eligible:
-
Using B17024, in the “Under 6 years” age interval, find the value A = the total number of children under 6 with income under 2.47 of the FPL. This is the sum of all income intervals under 2.00 plus a fraction of the number in the 2.00 to 2.99 interval assuming a uniform distribution within that interval. That is:
$$ \mathrm{A}=\mathrm{A}1+\mathrm{A}2 + \mathrm{A}3+\mathrm{A}4+\mathrm{A}5+\mathrm{A}6+\mathrm{A}7+\mathrm{A}8+\mathrm{A}9\ast \mathrm{A}10 $$Where:
- A1:
-
Total number of children with income under 0.50
- A2:
-
Total number of children with income between 0.50 and 0.74
- A3:
-
Total number of children with income between 0.75 and 0.99
- A4:
-
Total number of children with income between 1 and 1.24
- A5:
-
Total number of children with income between 1.25 and 1.49
- A6:
-
Total number of children with income between 1.50 and 1.74
- A7:
-
Total number of children with income between 1.75 and 1.84
- A8:
-
Total number of children with income between 1.85 and 1.99
- A9:
-
Total number of children with income between 2.00 and 2.99
$$ \mathrm{A}10 = \frac{2.47-2.00}{2.99-2.00} $$ -
Using Table B17024, find the total number of children under 6 ➔ Obtain value B
-
Find the eligible proportion ➔ Obtain value C
$$ C = A/B $$ -
Find the total eligible population in age class 1 by multiplying C by total people in age class 1:
$$ \mathrm{Age}\ \mathrm{Class}\ 1\ \mathrm{Eligible} = \mathrm{Age}\ \mathrm{Class}\ 1\ast C. $$Example (refer to Snapshot 2 for Census Tract 9501, Appling County, Georgia):
$$ A = 0 + 28 + 0 + 0 + 0 + 9 + 21 + 0 + 10*\frac{2.47-2.00}{2.99-2.00} = 62.747 $$$$ B = 176 $$$$ C=\frac{62.747}{176}=0.3565 $$$$ \mathrm{Age}\ \mathrm{Class}\ 1\ \mathrm{Eligible} = 52*0.3565 = 18.539 $$
-
-
6.
Age class 2 eligible:
-
Multiply the value of C by the total people in age class 2 to get the desired value, that is:
$$ \mathrm{Age}\ \mathrm{Class}\ 2\ \mathrm{Eligible} = \mathrm{Age}\ \mathrm{Class}\ 2\ast C $$
Example:
Age Class 2 Eligible = 201 * 0.3565 = 71.660
-
-
7.
Age class 3 eligible:
-
Using the “6 to 11 years” age interval in Table B17024 and the same method to obtain value B, find value D1 = the total number of children 6 to 11 years with income under 2.47 of the FPL
-
Repeat the previous step for the age interval “12 to 17 years” → Obtain value D2
-
Repeat again for the age interval “18 to 24 years” → Obtain value D3
-
Find the value E = the total number of children 6 to 18 years that are eligible in B17024, assume a uniform distribution in the “18 to 24 years” interval obtained by dividing the number of children from that interval by the width of that interval, that is:
$$ \mathrm{E} = \mathrm{D}1 + \mathrm{D}2 + \mathrm{D}3/\left(24-18 + 1\right) $$ -
Using Table B17024, find the value F = total population whose age is 6 to 18:
$$ \mathrm{F} = \mathrm{F}1 + \mathrm{F}2 + \mathrm{F}3 $$Where:
- F1:
-
Total number of children 6 to 11 years
- F2:
-
Total number of children 12 to 17 years
- F3:
-
Total number of children of children whose age is 18 in the class 18 to 24 (assuming a uniform distribution obtained by dividing the total number of children in the class by the width of the class that is 24 − 18 + 1 = 7)
-
Find the eligible proportion →Obtain value G: \( G=E/F \)
-
Find the total eligible population in age class 1 by multiplying F by total people in age class 3:
$$ \mathrm{Age}\ \mathrm{Class}\ 3\ \mathrm{Eligible} = \mathrm{Age}\ \mathrm{Class}\ 3\ast G $$Example (refer to Snapshot 2):
$$ \mathrm{D}1=0+0+0+97+0+36+11+0+86\ast \frac{2.47-2.00}{2.99-2.00}=184.828 $$$$ \mathrm{D}2=10+0+0+117+30+0+22+29+14\ast \frac{2.47-2.00}{2.99-2.00} = 214.646 $$$$ \mathrm{D}3=0+37+0+0+0+0+0+0+30\ast \frac{2.47-2.00}{2.99-2.00} = 51.242 $$$$ E=184.828+214.646+51.242/7=406.795 $$$$ F=315+310+159/7=647.714 $$$$ G=406.795/647.714=0.6280 $$$$ \mathrm{Age}\ \mathrm{Class}\ 3\ \mathrm{Eligible}=593\ast 0.6280=372.432 $$
-
-
8.
Total eligible population <= 18:
-
Sum the values of age class 1 eligible, age class 2 eligible, and age class 3 eligible.
Example
Total eligible population <= 18 = 18.539 + 71.660 + 372.432 = 462.631
-
-
9.
mob_med:
-
From PCT10, find the number of households with one or more people under 18 years → Obtain value H
Observation 1: to be consistent with the age class definition, we should consider the total number of households with at least one child less than 19 years old; however, this information is not available in the table.
-
From PCT7, find the total average household size → Obtain value I
-
Using the 2012 Department of Health and Human Services poverty guidelines formula found on http://aspe.hhs.gov/poverty/12poverty.shtml and the average household size, estimate value J = 247 % of the FPL in dollars. That is
$$ J=2.47*\left(11,170+3960*\left(I-1\right)\right) $$ -
Using B19001, find the value K = percent of households below 247 % of the FPL. This is done by summing the number of households below the estimated FPL (assuming a uniform distribution in the interval containing the FPL) and dividing that sum by the total number of households listed in that same table. That is:
$$ K = \left(\mathrm{K}1+\mathrm{K}2*\frac{J-\mathrm{K}3}{\mathrm{K}4-\mathrm{K}3}\right)/\mathrm{K}5 $$Where:
- K1:
-
The sum of the data in all income intervals with an upper bound lower than J
- K2:
-
The number of households in the income interval containing J
- K3:
-
The value of the lower bound of the income interval containing J
- K4:
-
The value of the upper bound of the income interval containing J
- K5:
-
The total number of households given in the table
-
Using B08201, divide the total number of households with no vehicle available by the total number of households to get the proportion of all households with no vehicles → Obtain value N
-
Multiply M and the complement of N to obtain mob_med, that is:
$$ \mathrm{mob}\_\mathrm{m}\mathrm{e}\mathrm{d}=K\ast \left(1-N\right) $$
Observation 2: This number is calculated assuming independence between income level, size of household, and vehicle ownership.
Example (refer to Snapshot 3, Snapshot 4, Snapshot 5, and Snapshot 6):
-
H = 436
-
I = 2.49
-
J = 2.47 * (11,170 + 3960 * (2.49 − 1)))) = $42,163.89
-
\( K=\left(55+80+89+56+113+125+108+65*\frac{42,163.89-40,000}{44,999-40,000}\right)/1189=0.5502 \)
-
\( N=\frac{31}{1189}=0.0261 \)
-
mob_med = .5502 * (1 − 0.0261) = 0.5358
-
-
10.
mob_oth:
-
Multiply the proportion of ineligible households, the complement of K, by the proportion of households with at least one vehicle, the complement of N. That is:
$$ \mathrm{mob}\_\mathrm{o}\mathrm{t}\mathrm{h}=\left(1-K\right)*\left(1-N\right) $$
Observation 3: The same assumption as noted above applies here.
Example
$$ \mathrm{mob}\_\mathrm{o}\mathrm{t}\mathrm{h}=\left(1-0.5502\right)*\left(1-0.0261\right)=0.4381 $$ -
Appendix 3: Mathematical Model and Selection Value of the Trade-off Parameter
Optimization models are a very common mathematical tool in the operations research community to make decision about complex system. The three main components of an optimization model are the following: (i) the decision variables, which are a mathematical representation of the decisions that need to be made; (ii) the constraints of the model, which together restrict the set of the decisions that can be made; and (iii) the objective function, which assigns a performance value to each decision. Solving an optimization model means choosing, among all the decisions represented by the constraints of the model, the one whose associated value of the objective function is the best (either the minimum value or the maximum value). The output of the model is represented by the values of the variables, which represent the best-chosen decision.
In our context, the decision variables represent the total number of patients in each census tract of a given age class who are assigned to a specific provider, namely x M ijk and x O ijk , where index i ∈ S represents a census tract, index j ∈ P represents a provider, and index k = 1, 2, 3 denotes a specific age class. We also use the superscripts M and O to distinguish between those children covered by the Medicaid/CHIP insurance (x M ijk ) and those children covered by private insurance (x O ijk ). Constraints in the model ensure that the assignment of patients to providers mimics the process by which families choose primary care for their children. However, the Medicaid/CHIP eligible population and private insurance covered population may face different barriers to health care. For this reason, the model considers the two populations separately.
Our model is based on the assumptions that both families and policy makers value children having a primary care provider, that patients prefer to visit nearby physicians, and that they prefer to schedule visits when the office is not too busy (congestion); however, when physician congestion is considered too high, families prefer nonphysician providers such as Nurse Practitioners.33 Under these assumptions, the objective function of the model is a weighted sum of the total distance traveled (which needs to be minimized) and the provider preference contingent upon demand volume (which needs to be maximized).
To be more specific, the objective function of the model is as follows:
where f k is the yearly number of visits required by a patient in age class k, d ij is the distance between the centroid of census tract i and physician j, y j is the level of congestion at physician j computed as the ratio between assigned number of visits and maximum physician caseload, and u j is a weight assigned to each provider. We note that the congestion level for Family/Internal Medicine is computed considering the physicians’ caseload that is devoted to visits to children. That is, we are assuming that these physicians are fully loaded, respecting the general perception of shortage of primary care supply for adult population.48
This objective function takes into account both the total distance and the total utility associated with the final assignment. In particular, the total weighted distance, represented by the first summation, is minimized, and the total patient satisfaction, represented by the second summation, is maximized. Different from the model in Nobles et al. 17 we add the second component to take into account preferences of patients toward different provider types. Existing studies show a general preference for physicians with respect to nurse practitioners, but nurse practitioners could be preferred to physicians when the latter are too congested.33 , 49 The model mimics this behavior by assigning the utility u j to each provider j; this parameter is initially set such that physicians (that is, Family/Internal Medicine and Pediatric physicians) are preferred to nurse practitioners. Such a utility is, however, penalized in the function so that the more congested the provider is, the less utility is gained. The two components of the objective function are weighted by the nonnegative trade-off parameter λ ∈ [0, 1]. This parameter is used to define the relative importance of each component in the objective function. Its value is empirically evaluated by performing several runs of the model to choose the value of the parameter such that (i) neither of the two components of the objective functions dominates the other, and (ii) the resulting optimized decision reflects the fact that close neighbors experience the same travel distance and the same congestion level. Details of this experimental evaluation of the trade-off parameter are given in the next section.
There are several sets of constraints in the model. Figure 8 in this appendix shows the complete mathematical formulation, while Table 6 provides a summarized view of the set of parameters. A brief explanation of the constraints of the model is given next.
The first set of constraints is assignment constraints that ensure that the assignment of patients to providers is nonnegative and that the total number of patients assigned to a provider in each census tract is not greater than the census tract population.
The second set of constraints takes into account the individual mandate provision in the ACA. The individual mandate requires every person to be insured; hence, the total number of patients to be assigned to providers should be equal to the total population of the state; however, we take into account the fact that the response of people to the individual mandate will not be universal, but we require that at least a given percentage of the total state population is assigned to providers.
The third set of constraints mimics distance barriers encountered by patients (accessibility constraints), taking into account a maximum distance allowed between patients and providers and barriers due to the ownership of a vehicle.
The fourth set of constraints takes into account provider capacity and mimics availability barriers (availability constraints). In particular, since providers have a maximum patient capacity based on the time they must spend with each patient to provide quality care, we consider constraints that ensure that the total number of patients assigned to each pediatric specialist cannot exceed his or her maximum caseload. Moreover, we add constraints that mimic the fact that for a provider to remain in practice, he or she must maintain a sufficiently large number of visits per year. Finally, we consider constraints that allow for different participation in the Medicaid program by limiting the total number of patients covered by Medicaid/CHIP insurance who can be assigned to each provider.
Finally, the last set of constraints considered in the model specifies that pediatric specialists cover a greater percentage of visits by children45 , 50 with respect to Family/Internal Medicine physicians (preference constraints). To this end, these constraints ensure that a given percentage α k of the total patients in age class k is served by pediatric physicians and pediatric nurse practitioners.
The optimization model described above is implemented using the optimization programming language OPL and the CPLEX solver on a UNIX system. The result of the model is a matching of patients to providers that satisfies all the constraints and optimizes the objective function.
Choice of the Trade-off Parameter Value
We run our optimization model several times to choose the value of the trade-off parameter λ in the objective function of the optimization model. Parameter λ should be such that the two following criteria hold:
-
A1: Neither one of the two components of the objective function dominates the other
-
A2: Close neighbors should experience same travel cost and congestion
The optimization model is run (for each state separately) for different values of the parameter λ and the following metrics are evaluated for each run:
-
Total distance traveled: the total weighted distance traveled is computed by summing up the distances for each patient for each assigned visit (first element of the objective function)
-
Total patient satisfaction: sum, over all the providers of the network, of the associated utility computed as a function of the provider congestion (second element of the objective function)
-
Spatial autocorrelation Geary index for the total congestion and the total distance traveled: the Geary index is a global index of spatial autocorrelation and provides a summary over the entire study area of the level of spatial similarity of a given measure observed among neighboring census tracts.51 The index varies between 0 and 2. Values of the index less than 1 denote positive spatial autocorrelation among neighboring census tracts. The Geary index is computed both for the average congestion experienced by patients at each census tract and for the total distance traveled by patients in each census tract.
The values of the first two metrics are evaluated to check whether the first assumption A1 holds, while the value of the Geary indices is considered to check whether assumption A2 holds.
Figure 9 shows the four abovementioned metrics for the optimization model for the state of Georgia and for the state of California computed for different values of the trade-off parameter, where the values of the total traveled distance and total patient satisfaction are normalized [0,1]. The leftmost parameter value corresponds to shortest distance, and the far right corresponds to a scenario with best patient satisfaction. Both total distance traveled and total patient satisfaction increase with the trade-off parameter. For small values of the trade-off parameter, distance is very important in the assignment, and thus, providers that are close to each other may have different levels of congestion and, therefore, different level of patient satisfaction. For larger values of the trade-off parameter, the situation is reversed and total patient utility plays an important role in the assignment while distance is not considered at all. The figures also show that the Geary indices for both distance and congestion are always lower that 1, denoting positive spatial autocorrelation. Using the two principles, reasonable values for the parameter λ are selected within the gray-shaded bands.
Appendix 4: Details on Statistical Methods Used
Hypothesis Test for Equality of Variances of Two Population Samples
We test the null hypothesis of equality of the variances. In particular, we consider the process Z(s), for each spatial unit s ∈ S, representing either the availability or the accessibility of either one of the two populations. The process can be decomposed as follows: Z(s) = μ(s) + Δ ϵ(s), where μ(s) is its mean trend, Δ its standard deviation, and ϵ(s) is a random error. To obtain an estimation of the variance of the process:
-
(i)
We apply nonparametric regression for estimation of the mean trend \( \hat{\mu}(s) \) through the use the gam function of the mgcv library in the R statistical software;
-
(ii)
We compute the squared residuals \( {Y}^2(s)={\left(Z(s)-\hat{\mu}(s)\right)}^2 \) and their log transformation: log(Y 2(s)) ≈ log(Δ ϵ(s))2 = log Δ2 + log ϵ 2(s).
From the above considerations, it follows that \( { \log \Delta}^2=\mathbb{E}\Big( \log \left({Y}^2(s)\right) \) and the mean or median of the log transformation of the squared residual of Z(s) are an estimate of the variance of the process. We apply the Wilcoxon-paired test to the log-transformed squared residuals of the processes Z M(s) and Z O(s), to test the null hypothesis of equality of the variances, i.e., H0 : σ 2MED = σ 2OTH H1 : σ 2MED > σ 2OTH .
We apply the two tests both for the census tract and the county aggregation levels.
Significance Maps
To locate where the difference in either accessibility or availability between the two populations is statistically significant, we construct significance maps. In particular, we consider the difference process Z(s) = M(s) − O(s) for each spatial unit s for s ∈ S a geographic domain. We decompose Z(s) using nonparametric regression, i.e, Z(s) = f(s) + ϵ s with \( f(s)={\displaystyle \sum_k}{\theta}_k{\varphi}_k(s) \) where φ k (s), k = 1, 2, … is a prespecified orthogonal basis of functions and θ k , k = 1, 2,.., are coefficients to be estimated. In our implementation, we used the penalized splines regression for estimating f(s) using the mgcv library in the R statistical software.
Furthermore, we used the method proposed by Serban46 and Krivobokova et al.47 to estimate the simultaneous confidence bands [l s , u s ] for the regression functions f(s). Using the confidence bands, we are able to identify where the difference process Z(s) is statistically significantly positive or negative. Indeed, for those spatial units s such that u s < 0, we can say that the difference is statistically significantly negative, while for those spatial units s such that l s > 0, we can say that the difference is statistically significantly positive. These units can then be visualized on a significance map.
Rights and permissions
About this article
Cite this article
Gentili, M., Isett, K., Serban, N. et al. Small-Area Estimation of Spatial Access to Care and Its Implications for Policy. J Urban Health 92, 864–909 (2015). https://doi.org/10.1007/s11524-015-9972-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-015-9972-1