Abstract
Background
Patients harboring concomitant epidermal growth factor receptor (EGFR) mutations and anaplastic lymphoma kinase (ALK) arrangements constitute a small subgroup of non-small-cell lung cancer (NSCLC) patients. The efficacy of EGFR tyrosine kinase inhibitors (TKIs) and the ALK-specific TKI crizotinib in these patients has not been well-established.
Objective
This study investigated the efficacy of targeted therapies in these patients compared with patients with EGFR or ALK alterations alone.
Methods
Patients were screened for EGFR mutation and ALK rearrangement at the Shanghai Chest Hospital (2011–2017). Progression-free survival (PFS), objective response rate (ORR), and overall survival (OS) were retrospectively analyzed.
Results
A total of 5816 patients were screened, and 26 patients were identified as having concomitant EGFR mutations and ALK rearrangements; 22 patients were eligible for survival analysis. Additionally, 95 EGFR-mutant patients and 60 ALK-rearranged patients were randomly selected for analysis. The ORR to EGFR TKIs was 63.2% (12/19) for EGFR/ALK co-altered patients and 62.1% (59/95) for EGFR-mutant patients (p = 0.93) with a median PFS of 10.3 and 11.4 months, respectively (hazard ratio [HR] 0.96; 95% confidence interval [CI] 0.59–1.57; p = 0.87). The ORR to crizotinib was 66.7% (8/12) for double-positive patients and 65.0% (39/60) for ALK-rearranged patients (p = 1.00), with a median PFS of 11.1 and 12.5 months, respectively (HR 1.39; 95% CI 0.69–2.80; p = 0.28). OS was 27.1, 36.2, and 36.8 months for EGFR-mutant, ALK-rearranged, and EGFR/ALK co-altered patients, respectively, and the EGFR/ALK co-existing subgroup tended to have a longer survival period than EGFR-mutant cohorts, though no statistical difference was found (p = 0.12). The median PFS of crizotinib as a sequential therapy after failure of EGFR TKIs was 15.0 months, which exhibited no statistically significant difference compared with the median PFS of ALK-altered patients who received crizotinib (p = 0.80).
Conclusions
Both first-generation EGFR TKIs and the ALK TKI crizotinib were effective in these patients. Sequential treatment with EGFR TKIs and crizotinib should be considered as a management option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Lung cancer is the most common malignancy and the leading cause of cancer-related death both in China and worldwide [1,2,3]. Treatment of non-small-cell lung cancer (NSCLC) has changed dramatically in recent years with the advent of targeted therapies for different oncogenic drivers; hence, molecular analysis of NSCLC is routinely performed to screen for several major therapeutic targets, including activating mutations of the epidermal growth factor receptor (EGFR) and rearrangement involving the anaplastic lymphoma kinase (ALK) [4]. These two drivers have conventionally been considered to be mutually exclusive [5]. However, cumulative reports have revealed that concomitant occurrence of EGFR mutations and ALK rearrangement accounts for a small number of NSCLC cases, raising the issue of therapeutic strategies [6,7,8,9,10,11,12,13,14,15,16].
First-generation EGFR tyrosine kinase inhibitors (TKIs), including gefitinib, erlotinib, and icotinib, are effective in patients with EGFR mutations [17,18,19]. Crizotinib, a small-molecular TKI, also shows efficacy superior to that of conventional chemotherapy in ALK-positive patients [20]. Nevertheless, the efficacy of EGFR TKIs and crizotinib in EGFR/ALK double-positive patients has been controversial. Some reports have indicated that EGFR TKIs had a better response than ALK inhibitors in terms of objective response rate (ORR) and progression-free survival (PFS) [7, 9, 10], but others have come to the opposite conclusion [11, 14, 15, 21]. Moreover, the effectiveness of combination or sequential therapy remains to be elucidated because of the scant number of patients reporting with concomitant EGFR mutations and ALK rearrangements and receiving both TKIs. We performed a retrospective analysis of 22 patients harboring concomitant EGFR mutations and ALK rearrangements to analyze the therapeutic efficacy of first-generation EGFR TKIs and crizotinib in these patients compared with those with a single oncogenic driver and to highlight the effectiveness of sequential treatment with EGFR TKIs and crizotinib.
2 Patients and Methods
2.1 Patients
This study was a data-driven retrospective single institution clinical audit without a prospective protocol. We identified patients with NSCLC who underwent molecular analysis at the Shanghai Chest Hospital between January 2011 and March 2017. The aim of this study was to evaluate patients with advanced (stages IIIB–IV) disease with either EGFR mutations or ALK rearrangements and co-occurring EGFR/ALK aberrations who received first-generation EGFR TKIs, crizotinib, or both. Patients were excluded if they were diagnosed with early-stage IA–IIIA NSCLC, did not receive TKIs, or received next-generation TKIs first. Patients with ALK rearrangements that were weakly positive on immunohistochemistry (IHC) and not confirmed by fluorescent in-situ hybridization (FISH) were also excluded.
The primary outcome of this study was comparison of PFS in patients with EGFR mutations, ALK rearrangements, and EGFR/ALK co-alteration. Secondary outcomes included overall survival (OS) and ORR in these patients.
Positron emission tomography/computed tomography (PET/CT) or other radiological evaluation methods were used to confirm or exclude metastatic disease. Staging was performed according to the 7th edition of the tumor node metastasis (TNM) classification for NSCLC. The specimens used for molecular analyses were obtained from surgery, fine-needle small biopsies guided by CT or ultrasound, transbronchial biopsies, or malignant effusion cell blocks.
The study was approved by the institutional review board of the Shanghai Chest Hospital, and all patients signed written consent forms before invasive procedures and TKI treatments.
2.2 Molecular Analyses
EGFR mutations were evaluated with the direct sequence and amplification refractory mutation system (ARMS) according to the manufacturer’s protocol. DNA was extracted from various specimens, amplified with polymerase chain reaction (PCR), and analyzed with standard sequencing. Details of the two methods are previously described [22, 23].
ALK rearrangements were identified by IHC or FISH. Samples were sent as formalin-fixed and paraffin-embedded (FFPE) biopsies, and FISH tests were performed on these tissues using a Vysis ALK break-apart FISH probe kit (Abbott Molecular, Des Plaines, IL, USA). Patients were diagnosed as ALK FISH positive when ≥ 15% of the tumor cells showed split and/or isolated 3ʹ signals. ALK IHC was conducted with the anti-ALK (D5F3 Ventana) primary antibody combined with OptiView DAB IHC detection and OptiView amplification (Ventana Medical Systems, Inc., Tucson, AZ, USA). Patients were diagnosed as ALK IHC positive if strong granular cytoplasmic brown staining was present in tumor cells [24, 25].
2.3 Treatment and Follow-Up
Patients in three cohorts were treated with EGFR TKIs (gefitinib [Iressa, AstraZeneca Pharmaceuticals], erlotinib [Tarceva, Roche], or icotinib [Conmana, Betta]), crizotinib, or both. Clinical evaluation was performed every 4–6 weeks according to RECIST 1.1 (Response Evaluation Criteria in Solid Tumors) [26]. PFS was defined from the initiation of TKIs to radiographic or clinical progression or the last follow-up time. OS was calculated from pathological diagnosis of stage IIIB/IV NSCLC to death or last follow-up time. The median follow-up time was 33 months (range 4–100), and the last follow-up time was 23 January 2019.
2.4 Statistical Analyses
We eliminated the large difference in the numbers of patients among the EGFR-mutant or ALK-rearranged cohort, and the ALK/EGFR co-altered cohort. EGFR-mutant or ALK-rearranged patients included for survival analysis were randomly selected from those with a single oncogenic driver who received first-generation EGFR TKIs or crizotinib and had complete medical records. The ratio of selected patients to double-positive patients who received EGFR TKIs or crizotinib was 1:5. The randomization process using Excel 2013 (Microsoft, Redmond, WA, USA) was as follows: (1) every patient was given a random number using the RANDBETWEEN function, ranging from 0 to 1; (2) patients were ranked according to the assigned number; and (3) the top patients needed for analysis were selected. To test the representativeness of the selected patients, their baseline characteristics were compared with those of the whole population, including patients with missing data.
To compare baseline characteristics, we used the chi-squared test for categorical variables, Fisher’s exact test for small samples, and the Wilcoxon rank sum test for continuous variables. Survival curves were generated to compare PFS and OS using Kaplan–Meier methods and further compared using the log-rank test. A p value < 0.05 was considered statistically significant. All analyses were performed using the Statistical Package for Social Science (IBM; Armonk, NY, USA) version 22.0 for Windows. Figures were created using GraphPad Prism 7 (San Diego, CA, USA).
3 Results
3.1 Patient Characteristics
Between January 2011 and March 2017, a total of 5816 patients underwent both EGFR-mutation and ALK-rearrangement analysis. In total, 2392 patients had EGFR mutations, 503 had ALK alterations, and 26 had concomitant EGFR mutations and ALK alterations. The frequency of concomitant EGFR mutations and ALK rearrangement was about 0.45% (26/5816) of the entire NSCLC patient cohort, 1.1% (26/2418) of EGFR-mutation patients, and 4.91% (26/529) of ALK-positive patients.
Excluding patients diagnosed with stage IA–IIIA, who had not received TKIs, or who had received next-generation TKIs first left 1328, 259, and 23 patients with advanced (stage IIIB–IV) NSCLC in the EGFR-mutant, ALK-rearranged, and EGFR/ALK co-altered cohorts, respectively. Table 1 presents the demographic profiles and clinico-pathological characteristics of the three groups. The median age at diagnosis of stage IIIB/IV NSCLC for EGFR/ALK co-altered, EGFR-mutant, and ALK-rearranged groups was 61, 60, and 56 years, respectively. Patients from the ALK-rearranged cohort were younger than those from the EGFR-mutant or EGFR/ALK cohorts (p < 0.01). The specimens for diagnosis and molecular analysis were obtained in various ways (p < 0.01). There was no difference between the three groups with respect to sex, smoking status, pathologic type, performance status, or stage at initiation of TKIs. The EGFR-mutation types also showed no difference between the EGFR/ALK co-altered and EGFR-mutant groups.
3.2 Response and Survival Analyses
In the EGFR-mutant, ALK-rearranged, and EGFR/ALK co-altered cohorts, respectively, 367, 56, and 1 patient with stage IIIB/IV NSCLC and missing data received TKIs. Using the abovementioned procedure, 95 patients with EGFR mutations and 60 with ALK rearrangements were randomly selected from those with complete medical records. The patient selection process is outlined in Fig. 1.
Finally, 95, 60, and 22 patients from the EGFR-mutant, ALK-rearranged, and EGFR/ALK co-altered groups were included for survival analysis. Among the EGFR/ALK co-altered cohort, ten patients received EGFR TKIs (gefitinib, erlotinib, icotinib) alone, three patients received crizotinib alone, and nine patients received both EGFR TKIs and crizotinib. Therefore, a total of 19 patients previously received EGFR TKIs, and 12 patients were treated with crizotinib. All patients in the EGFR/ALK co-altered cohort experienced disease progression as assessed by RECIST while receiving EGFR TKIs and crizotinib.
The baseline characteristics of the entire EGFR-mutant cohort (all patients with EGFR-mutant stage IIIB/IV NSCLC treated with EGFR TKIs), selected EGFR-mutant patients, and EGFR/ALK co-altered patients who received EGFR TKIs were well-balanced (Table 2). The clinico-pathological characteristics of the entire ALK-rearranged cohort (all stage IIIB/IV NSCLC ALK patients treated with crizotinib), selected ALK-rearranged patients, and EGFR/ALK co-altered patients who received crizotinib were also well-balanced (Table 3). As a result, the randomly selected patients were considered to satisfactorily represent the entire EGFR-mutant and ALK-rearranged cohorts.
The ORR for patients treated with EGFR TKIs was 62.1% (59/95) for EGFR-mutant and 63.2% (12/19) for double-positive patients. The difference was not statistically significant (p = 0.93). The ORR for patients treated with crizotinib was 65% (39/60) for ALK-rearranged and 66.7% (8/12) for EGFR/ALK double-positive patients. The difference was not statistically significant (p = 1.00).
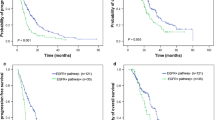
PFS was defined from the initiation of TKIs to radiographic or clinical progression or the last follow-up time. The median PFS of EGFR/ALK co-altered patients treated with EGFR TKIs was 10.3 months, which was not statistically different from that of EGFR-mutant patients (11.4 months; hazard ratio [HR] 0.96; 95% confidence interval [CI] 0.59–1.57; p = 0.87) (Fig. 2a). Additionally, the median PFS of crizotinib was 11.1 months and 12.5 months for EGFR/ALK double-positive and ALK-rearranged patients, respectively. No statistically significant difference was found between these two groups (HR 1.39; 95% CI 0.69–2.80; p = 0.28) (Fig. 2b).
a Kaplan–Meier curves for progression-free survival of selected EGFR-mutant patients and EGFR/ALK double-positive patients treated with EGFR TKIs. b Kaplan–Meier curves for progression-free survival of selected ALK-rearranged patients and EGFR/ALK double-positive patients treated with crizotinib. ALK anaplastic lymphoma kinase, EGFR epidermal growth factor receptor
OS was calculated from pathological diagnosis of stage IIIB/IV NSCLC to death or last follow-up date, with 68% (15/22), 72% (68/95), and 63.3% (38/60) of patients known to have died at the data cut-off date in the EGFR/ALK co-alteration, EGFR-mutation, and ALK-rearrangement groups, respectively. Median OS was 36.8, 27.1, and 36.2 months (p = 0.034) (Fig. 3). Although no statistically significant difference was found between the EGFR/ALK co-existing group and the selected EGFR-mutant group (HR 0.66; 95% CI 0.40–1.08), there was a trend toward increased long-term survival for double-positive patients.
Among a group of patients who were treated with both EGFR TKIs and crizotinib, only one patient received crizotinib before first-generation EGFR TKIs, and eight patients received crizotinib after failure of EGFR TKIs. In this subgroup, the ORR was 55.6% (5/9) and 66.7% (6/9), respectively, for EGFR TKIs and crizotinib. The median PFS of crizotinib as a sequential therapy after failure in EGFR TKIs was 15.0 months, which exhibited no statistically significant difference from that of ALK-altered patients who received crizotinib (12.5 months; HR 1.10; 95% CI 0.51–2.37; p = 0.80). Four patients received crizotinib as first-line therapy (three only received crizotinib; one received both crizotinib and an EGFR TKI), and the ORR for crizotinib in this subgroup was 75.0% (3/4).
4 Discussion
Our study suggests that the coexistence of EGFR mutations and ALK rearrangement accounts for about 0.45% (95% CI 0.28–0.62) of NSCLC, 1.1% (26/2418) of EGFR-mutant disease, and 4.91% (26/529) of ALK-positive disease. First-generation EGFR TKIs and crizotinib in patients with concomitant EGFR mutations and ALK rearrangement were equally efficacious as in patients with single-gene alterations. EGFR/ALK co-altered patients also appeared to have longer OS than patients with EGFR-mutant disease.
Remarkable progress has been made in the treatment of NSCLC due to the discovery of several critical activating pathways. Among these pathways, EGFR-activating mutations and ALK rearrangements are routinely screened for and clinically relevant [27]. Although these two driver alterations were previously considered mutually exclusive [5], recent reports have shown that EGFR/ALK double-positive patients account for a small proportion of NSCLC [6,7,8,9,10,11,12,13,14,15,16]; however, previous data has been inconsistent with regard to the frequency of double-positive patients in NSCLC, ranging from 0.1 to 1.6% [9, 15, 21, 28]. The prevalence of double-positive patients in our study is within this range when using ARMS and IHC/FISH techniques to detect EGFR mutations and ALK rearrangement. Won et al. [15] reported the frequency of EGFR and ALK coexistence in ALK-positive patients to be 4.4% when using Sanger sequencing, but this increased to 15% with high-sensitivity next-generation sequencing (NGS). Therefore, as more advanced techniques emerge, the proportion of double-positive patients could be much higher than previously expected, which will have implications for the treatment of these patients.
First-generation EGFR TKIs such as gefitinib, erlotinib, and icotinib provide survival benefits over conventional chemotherapy and have revolutionized the therapy of patients with NSCLC with EGFR-activating mutations [17,18,19], as has crizotinib, a TKI targeting ALK in activating rearrangements, for ALK-positive patients [20]. These TKIs play irreplaceable roles in managing NSCLC with a single oncogenic driver, but there is no consensus on their effects in double-positive patients because of the limited number of reported cases. Lou et al. showed that the median PFS was 11.2 months for EGFR/ALK co-altered patients treated with EGFR TKIs and 13.2 months for EGFR-mutant patients. A less favorable result for crizotinib was found in double-positive patients, with a median PFS of 1.9 months compared with 6.9 months in ALK-rearranged patients, although no statistical significance was demonstrated because of the small number of patients included in this analysis [9]. Sweis et al. [12] illustrated a poor response to both EGFR and ALK TKIs with a disease control rate (DCR) of 33.3% (1/3) and 25% (1/4), respectively, among four patients with coexisting EGFR mutations and ALK rearrangement. However, some reports showed encouraging responses when EGFR and ALK TKIs were given to these patients. Baldi et al. [6] reported a double-positive long-term survivor achieving 3 years of stable disease using erlotinib and a partial response to crizotinib afterwards. Lo Russo et al. [8] conducted a literature review of 100 cases, among which 51 cases received EGFR TKIs and 37 received ALK TKIs. Disease control or disease response were reported as best response in 69.8% and 43.4% compared with 79.5% and 51.3% of reviewed cases treated with EGFR and ALK TKIs, respectively. It is hard to draw firm conclusions from these results, partly because most of these patients were presented in single case reports, and no large-scale study was conducted. In our study, the ORR for EGFR TKIs and crizotinib for dual-positive patients was 63.2% (12/19) and 66.7% (8/12), and the median PFS was 10.3 months and 11.1 months, respectively, which showed no statistically significant difference from patients with single gene drivers. Thus, we may conclude that both EGFR and ALK TKIs were effective in the treatment of EGFR/ALK double-positive patients.
Although we found no difference between ALK-rearranged and EGFR/ALK co-altered patients with respect to OS, there was a tendency towards longer OS for double-positive patients compared with those with EGFR mutations alone. This was probably related to their effective response to both EGFR and ALK TKIs. In contrast to our results, Lou et al. reported that double-positive patients had relatively shorter OS than those with either an EGFR mutation or an ALK rearrangement [9], possibly because of the smaller sample size.
Among the 22 patients included for analysis in our study, nine patients received both EGFR TKIs and crizotinib. EGFR TKIs were administered before crizotinib in the majority of cases (eight patients). In this subgroup, we found that the ORRs were 55.6% (5/9) and 66.7% (6/9) for EGFR TKIs and crizotinib, respectively. The median PFS for crizotinib as sequential therapy after failure in EGFR TKIs was 15.0 months, which exhibited no statistical significance compared with that of patients with an ALK rearrangement who only received crizotinib (p = 0.80). This all suggests that sequential treatment with EGFR and ALK TKIs is effective in treating double-positive patients. Furthermore, EGFR TKIs did not influence the efficacy of crizotinib as a subsequent therapy after progression on EGFR TKIs. Four patients received crizotinib as first-line treatment, with an ORR of 75% (3/4). Given the limited number of patients who received crizotinib before EGFR TKIs in our study, it was infeasible to determine the optimal sequence of administration.
Finding biomarkers to predict the efficacy of EGFR and ALK TKIs is another challenge. The burden of EGFR mutations in the double-positive patients may be a predictor of response to EGFR TKIs. Meanwhile, Yang et al. [16] proposed that relative phospho-ALK and phospho-EGFR levels, as well as the level of phosphorylation of downstream proteins in the signaling pathway, could predict the efficacy of EGFR TKIs and crizotinib.
Different theories exist concerning the coexistence of EGFR mutations and ALK rearrangement in NSCLC. Cai et al. [29] demonstrated that the two gene alterations were not from the same tumor cell and that coexistence was due to intratumor heterogeneity. However, Yang et al. [16] found mutant EGFR proteins co-expressed with an ALK fusion protein in the same cell population using IHC, and Sasaki et al. [30] showed that co-activation of EGFR signaling occurred in an ALK-rearranged cell line.
As mentioned, EGFR/ALK co-altered patients can benefit from sequential treatment with both TKIs and have long-term survival, so a more effective way to find these co-altered patients is needed. NGS is now widely available, and more EGFR/ALK patients can be identified using highly sensitive NGS [15]. Therefore, we recommend that NGS would be better performed in all patients with advanced NSCLC to find all targetable gene alterations; additionally, in areas with limited access to NGS, patients should also be analyzed for both EGFR mutations and ALK rearrangements using conventional methods.
This was a retrospective single-center study, which cannot accurately reflect the entire double-positive patient population. Although the study comprised the highest number of patients with concomitant EGFR mutations and ALK rearrangements in one institution, to our knowledge, the sample size was still relatively small. Additionally, chemotherapy and radiation therapy could have been used in different lines of treatment, which might interfere with the result.
5 Conclusions
EGFR/ALK double-positive patients accounted for 0.45% (26/5816) of all patients with NSCLC, 1.1% (26/2418) of EGFR-mutant patients, and 4.91% (26/529) of ALK-positive patients. Both first-generation EGFR TKIs, including gefitinib, erlotinib, and icotinib, as well as crizotinib, were effective in these patients, which showed no statistically significant difference from patients with a single gene driver in terms of PFS and ORR. The sequential treatment with EGFR TKIs and crizotinib appears promising, and EGFR TKIs did not influence the efficacy of crizotinib as a subsequent treatment in these patients.
References
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32. https://doi.org/10.3322/caac.21338.
Chen W, Zheng R, Zeng H, Zhang S, He J. Annual report on status of cancer in China, 2011. Chin J Cancer Res Chung-kuo yen cheng yen chiu. 2015;27(1):2–12. https://doi.org/10.3978/j.issn.1000-9604.2015.01.06.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. https://doi.org/10.3322/caac.20107.
Kris MG, Johnson BE, Berry LD, Kwiatkowski DJ, Iafrate AJ, Wistuba II, et al. Using multiplexed assays of oncogenic drivers in lung cancers to select targeted drugs. JAMA. 2014;311(19):1998–2006. https://doi.org/10.1001/jama.2014.3741.
Gainor JF, Varghese AM, Ou SH, Kabraji S, Awad MM, Katayama R, et al. ALK rearrangements are mutually exclusive with mutations in EGFR or KRAS: an analysis of 1,683 patients with non-small cell lung cancer. Clin Cancer Res. 2013;19(15):4273–81. https://doi.org/10.1158/1078-0432.ccr-13-0318.
Baldi L, Mengoli MC, Bisagni A, Banzi MC, Boni C, Rossi G. Concomitant EGFR mutation and ALK rearrangement in lung adenocarcinoma is more frequent than expected: report of a case and review of the literature with demonstration of genes alteration into the same tumor cells. Lung Cancer. 2014;86(2):291–5. https://doi.org/10.1016/j.lungcan.2014.09.011.
Kuo YW, Wu SG, Ho CC, Shih JY. Good response to gefitinib in lung adenocarcinoma harboring coexisting EML4-ALK fusion gene and EGFR mutation. J Thorac Oncol. 2010;5(12):2039–40. https://doi.org/10.1097/JTO.0b013e3181f43274.
Lo Russo G, Imbimbo M, Corrao G, Proto C, Signorelli D, Vitali M, et al. Concomitant EML4-ALK rearrangement and EGFR mutation in non-small cell lung cancer patients: a literature review of 100 cases. Oncotarget. 2017;8(35):59889–900. https://doi.org/10.18632/oncotarget.17431.
Lou NN, Zhang XC, Chen HJ, Zhou Q, Yan LX, Xie Z, et al. Clinical outcomes of advanced non-small-cell lung cancer patients with EGFR mutation, ALK rearrangement and EGFR/ALK co-alterations. Oncotarget. 2016;7(40):65185–95. https://doi.org/10.18632/oncotarget.11218.
Popat S, de Vieira Araujo A, Min T, Swansbury J, Dainton M, Wotherspoon A, et al. Lung adenocarcinoma with concurrent exon 19 EGFR mutation and ALK rearrangement responding to erlotinib. J Thorac Oncol. 2011;6(11):1962–3. https://doi.org/10.1097/jto.0b013e31822eec5e.
Sahnane N, Frattini M, Bernasconi B, Zappa F, Schiavone G, Wannesson L, et al. EGFR and KRAS mutations in ALK-positive lung adenocarcinomas: biological and clinical effect. Clin Lung Cancer. 2016;17(1):56–61. https://doi.org/10.1016/j.cllc.2015.08.001.
Sweis RF, Thomas S, Bank B, Fishkin P, Mooney C, Salgia R. Concurrent EGFR mutation and ALK translocation in non-small cell lung cancer. Cureus. 2016;8(2):e513. https://doi.org/10.7759/cureus.513.
Tanaka H, Hayashi A, Morimoto T, Taima K, Tanaka Y, Shimada M, et al. A case of lung adenocarcinoma harboring EGFR mutation and EML4-ALK fusion gene. BMC Cancer. 2012;12:558. https://doi.org/10.1186/1471-2407-12-558.
Tiseo M, Gelsomino F, Boggiani D, Bortesi B, Bartolotti M, Bozzetti C, et al. EGFR and EML4-ALK gene mutations in NSCLC: a case report of erlotinib-resistant patient with both concomitant mutations. Lung Cancer. 2011;71(2):241–3. https://doi.org/10.1016/j.lungcan.2010.11.014.
Won JK, Keam B, Koh J, Cho HJ, Jeon YK, Kim TM, et al. Concomitant ALK translocation and EGFR mutation in lung cancer: a comparison of direct sequencing and sensitive assays and the impact on responsiveness to tyrosine kinase inhibitor. Ann Oncol. 2015;26(2):348–54. https://doi.org/10.1093/annonc/mdu530.
Yang JJ, Zhang XC, Su J, Xu CR, Zhou Q, Tian HX, et al. Lung cancers with concomitant EGFR mutations and ALK rearrangements: diverse responses to EGFR-TKI and crizotinib in relation to diverse receptors phosphorylation. Clin Cancer Res. 2014;20(5):1383–92. https://doi.org/10.1158/1078-0432.ccr-13-0699.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–57. https://doi.org/10.1056/NEJMoa0810699.
Shi YK, Wang L, Han BH, Li W, Yu P, Liu YP, et al. First-line icotinib versus cisplatin/pemetrexed plus pemetrexed maintenance therapy for patients with advanced EGFR mutation-positive lung adenocarcinoma (CONVINCE): a phase 3, open-label, randomized study. Ann Oncol. 2017;28(10):2443–50. https://doi.org/10.1093/annonc/mdx359.
Zhou C, Wu YL, Chen G, Feng J, Liu XQ, Wang C, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12(8):735–42. https://doi.org/10.1016/s1470-2045(11)70184-x.
Solomon BJ, Mok T, Kim DW, Wu YL, Nakagawa K, Mekhail T, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371(23):2167–77. https://doi.org/10.1056/NEJMoa1408440.
Lee JK, Kim TM, Koh Y, Lee SH, Kim DW, Jeon YK, et al. Differential sensitivities to tyrosine kinase inhibitors in NSCLC harboring EGFR mutation and ALK translocation. Lung Cancer. 2012;77(2):460–3. https://doi.org/10.1016/j.lungcan.2012.04.012.
Kim HJ, Lee KY, Kim YC, Kim KS, Lee SY, Jang TW, et al. Detection and comparison of peptide nucleic acid-mediated real-time polymerase chain reaction clamping and direct gene sequencing for epidermal growth factor receptor mutations in patients with non-small cell lung cancer. Lung Cancer. 2012;75(3):321–5. https://doi.org/10.1016/j.lungcan.2011.08.005.
Newton CR, Graham A, Heptinstall LE, Powell SJ, Summers C, Kalsheker N, et al. Analysis of any point mutation in DNA. The amplification refractory mutation system (ARMS). Nucleic Acids Res. 1989;17(7):2503–16.
Mino-Kenudson M, Chirieac LR, Law K, Hornick JL, Lindeman N, Mark EJ, et al. A novel, highly sensitive antibody allows for the routine detection of ALK-rearranged lung adenocarcinomas by standard immunohistochemistry. Clin Cancer Res. 2010;16(5):1561–71. https://doi.org/10.1158/1078-0432.ccr-09-2845.
Yi ES, Boland JM, Maleszewski JJ, Roden AC, Oliveira AM, Aubry MC, et al. Correlation of IHC and FISH for ALK gene rearrangement in non-small cell lung carcinoma: IHC score algorithm for FISH. J Thorac Oncol. 2011;6(3):459–65. https://doi.org/10.1097/JTO.0b013e318209edb9.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Lindeman NI, Cagle PT, Beasley MB, Chitale DA, Dacic S, Giaccone G, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Mol Diagn. 2013;15(4):415–53. https://doi.org/10.1016/j.jmoldx.2013.03.001.
Ulivi P, Chiadini E, Dazzi C, Dubini A, Costantini M, Medri L, et al. Nonsquamous, non-small-cell lung cancer patients who carry a double mutation of EGFR, EML4-ALK or KRAS: frequency, clinical-pathological characteristics, and response to therapy. Clin Lung Cancer. 2016;17(5):384–90. https://doi.org/10.1016/j.cllc.2015.11.004.
Cai W, Lin D, Wu C, Li X, Zhao C, Zheng L, et al. Intratumoral heterogeneity of ALK-rearranged and ALK/EGFR coaltered lung adenocarcinoma. J Clin Oncol. 2015;33(32):3701–9. https://doi.org/10.1200/jco.2014.58.8293.
Sasaki T, Koivunen J, Ogino A, Yanagita M, Nikiforow S, Zheng W, et al. A novel ALK secondary mutation and EGFR signaling cause resistance to ALK kinase inhibitors. Cancer Res. 2011;71(18):6051–60. https://doi.org/10.1158/0008-5472.can-11-1340.
Acknowledgements
The authors acknowledge all the patients and their families for their contributions to this study. No writing assistance was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of interest
Yiming Zhao, Shuyuan Wang, Bo Zhang, Rong Qiao, Jianlin Xu, Lele Zhang, Yanwei Zhang and Baohui Han have no conflicts of interest that might be relevant to the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Zhao, Y., Wang, S., Zhang, B. et al. Clinical Management of Non-Small Cell Lung Cancer with Concomitant EGFR Mutations and ALK Rearrangements: Efficacy of EGFR Tyrosine Kinase Inhibitors and Crizotinib. Targ Oncol 14, 169–178 (2019). https://doi.org/10.1007/s11523-019-00628-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-019-00628-6