Abstract
Background
Tyrosine-kinase inhibitors (TKIs) markedly improve progression-free survival (PFS) of patients with advanced non-small-cell lung cancer (NSCLC) mutated for epidermal growth factor receptor (EGFR). Results on overall survival (OS) are less clear-cut. We performed a publication-based meta-analysis to address further this issue.
Methods
We did a PubMed query using keywords simultaneously (lung neoplasm, tyrosine kinase inhibitors, epidermal growth factor receptor mutation, survival, and randomized controlled trials). We also searched for relevant abstracts in annual proceedings of ASCO, ESMO, and WCLC meetings. We cross-checked all references from all eligible articles. Only phase III randomized controlled trials comparing TKI monotherapy and platinum-based doublet chemotherapy in first-line treatment of metastatic or advanced NSCLC were included. We used EasyMA software to perform statistical analyses. A random effect model was used in case of heterogeneity between studies (and a fixed effect model in absence of heterogeneity).
Results
The eight eligible studies included 2962 patients (780 males, 2182 females, mostly Asian, median age 60 years), 2909 adenocarcinomas (98 %), 1739 mutated tumors (897 exon 19 deletion, 699 L858 mutation), 448 stage IIIB, and 2222 stage IV (75 %) tumours and 2453 never smokers (83 %). Four studies assessed gefitinib, two studies assessed erlotinib, and two studies assessed afatinib. Chemotherapies were doublets including a platinum salt. All studies included patients with EGFR mutations, but six studies included only EGFR mutated patients. OS was similar among patients who first received TKI or chemotherapy (HR 0.98, 95 % CI 0.87-1.10, fixed effect model). Conversely, compared with chemotherapy, EGFR TKIs significantly improved PFS in patients with EGFR-mutated tumours (HR 0.37, 95 % CI 0.29-0.49, random effect model). Concerning side effects, rash (RR 6.29, 95 % CI 4.05-9.77), diarrhoea (RR 3.51, 95 % CI 2.15-5.75), stomatitis (RR 3.57, 95 % CI 1.81-7.04), and interstitial lung disease (RR 6.07, 95 % CI 1.66-22.2) were significantly more frequent after TKIs. As expected, fatigue (RR 0.38, 95 % CI 0.32-0.45), nausea/vomiting (RR 0.19, 95 % CI 0.11-0.32), and haematological disorders, including thrombocytopenia (RR 0.18, 95 % CI 0.09-0.35), anaemia (RR 0.22, 95 % CI 0.15-0.33), and grade 3-4 neutropenia (RR 0.06, 95 % CI 0.04-0.08), were significantly more frequent after chemotherapy.
Conclusion
The major discrepancy between a similar OS and a markedly improved PFS after first-line TKI compared with chemotherapy could be related to the high level of crossing-over between both groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Lung cancer represents the main cause of cancer-related mortality worldwide. In many of these patients, the initial diagnosis corresponds to an advanced disease, which contributes to a poor global prognosis. Non-small-cell lung cancer (NSCLC) is by far the most frequent form of lung cancer, since it represents about 85 % of all cases of lung cancer. Recently, epidermal growth factor receptor (EGFR) mutation has been shown to predict the efficacy of tyrosine-kinase inhibitors (TKIs) [1, 2]. Other clinical predictors of efficacy of EGFR TKIs are female sex, being never smoker, an Asian ethnicity, and a histo pathological diagnosis of adenocarcinoma [3, 4]. Consequently, gefitinib, erlotinib, and finally afatinib, three small molecule EGFR TKIs, have been approved by the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for use in first-line advanced NSCLC among EGFR-mutated patients, considering their marked beneficial effect on progression-free survival (PFS) compared to doublet chemotherapy including a platinum salt. It should be stressed that only 10-15 % of Caucasian patients with NSCLC harbour the EGFR mutation, whereas it is present in 30-35 % of patients of Asian ethnicity [5]. This is the reason why almost all randomized controlled trials (RCTs) have been performed in Asia, except EURTAC [6], performed in Europe. The primary outcome of all but one RCTs was PFS. Only FIRST SIGNAL had overall survival (OS) as the primary endpoint [7].
Our meta-analysis (MA) has been updated in March 2015. The pooling of the eight available RCTs including recent data allowed us to assess OS as the primary outcome (main goal), in addition to PFS. Additional goals were the comparison of side-effects of TKIs monotherapy and chemotherapy among EGFR-mutated patients. The rationale of our MA was to include only EGFR TKI single drug studies (and not studies combining an EGFR TKI with chemotherapy) since these agents are only approved as monotherapies. Our MA represents the updated answer to the question of whether or not an EGFR TKI should be preferred to chemotherapy in advanced NSCLC among EGFR mutated patients.
2 Materials and Methods
2.1 Publication Selection
The aim of our MA was to update the previous MAs by including the two RCTs assessing afatinib among mutated EGFR NSCLC patients. We performed our MA according to a predefined written protocol. To be eligible, studies had to be phase III RCTs, to deal with first-line treatment of metastatic or advanced NSCLC (stage IIIB or IV) comparing, exclusively among mutated patients, a platinum-based doublet chemotherapy to an EGFR TKI monotherapy, and to be published either as full articles or as informative abstracts. These studies often compared efficacy (OS, PFS) and toxicity (clinical and biological side-effects) of both treatments.
Publications were identified by an electronic search using online using PubMed, updated on March 6, 2015, with the following keywords used simultaneously: lung neoplasm, tyrosine kinase inhibitor, Epidermal Growth Factor Receptor mutation, survival, and randomized controlled trials. An EMBASE query did not bring additional references. Abstracts were obtained and reviewed from the annual proceedings of the American Society of Clinical Oncology (ASCO) since 2009, World Congress on Lung Cancer (WCLC,) and the European Society of Medical Oncology (ESMO) since 2011. We also cross-checked all references of publications to obtain additional references.
2.2 Study Selection and Data Extraction
Each article or abstract was carefully read by two reviewers (GDG putting the emphasis on oncological aspects and BU putting the emphasis on methodological aspects). Both reviewers had to fill in separately a pre-defined form. Disagreements were resolved by discussion between both reviewers. The data extracted from each publication were: the geographical origin of the study, the study acronym, the first author, the title of the article, the full reference of the article, the type of chemotherapy, the main characteristics of the patients (mean or median age, male/female, smokers/non-smokers, ethnic origin of patients) and of the tumours (mainly adenocarcinomas, stage IIIB or IV, number of mutated tumours, and type of mutation), numbers of patients in both groups who crossed-over, numbers of events (relapse, death), and total numbers of patients in each group. We assessed OS (main outcome) and PFS from all studies. We did not assess the quality of studies by “Jadad score” because there is no general agreement on the suitability of such scores.
2.3 Statistical Analysis
For each study, the hazard ratios (HRs) were estimated by the direct collection of HRs with their 95 % confidence intervals (95 % CIs), which were always mentioned in the original publications. For each kind of side-effect, the relative risk (RR) was calculated from the absolute numbers of patients exposed or presenting with the side-effect. By convention, in each study, we chose as reference the doublet chemotherapy and HRs lower than 1 meant that survival was better among patients under first-line TKI or that side-effects were more frequent among patients treated with first-line chemotherapy.
We calculated HR estimates and their 95 % CI by using a fixed effect model (Mantel-Haenszel) in case of the absence of heterogeneity between studies and a random-effect model when heterogeneity was present. The statistical calculations used EasyMA.Net software (http://www.spc.univ-lyon1.fr/easyma.net/), available online (Department of Clinical Pharmacology, Cardiology hospital, Lyon, France). PN performed the statistical analysis.
3 Results
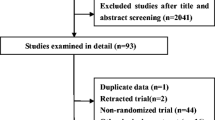
Our PubMed query performed on March 6, 2015 found 22 references (Fig. 1). Of these, careful reading of titles and abstracts only retrieved two phase III RCTs fulfilling our inclusion criteria [8, 9]. By cross-checking references, we found 14 additional publications assessing gefitinib (250 mg orally once daily (PO od)) [7, 10–14, 19], erlotinib (150 mg PO od) [6, 15, 20, 21], and afatinib [16–18]. Concerning gefitinib, there were six published articles [9–14] and two abstracts [7, 19]. For erlotinib, there were two full-length articles [6, 8] and three abstracts [15, 20, 21]. Concerning afatinib, there were two published articles [16, 18] and one abstract [17].
The main characteristics of patients included in the eight studies are described in the Table 1. The eight assessed trials included 2962 patients (780 males and 2182 females), mostly of Asian ethnicity, with a median age of 60 years [57 - 64.5 years]. Six studies (LUX Lung 3, LUX Lung 6, NEJ002, WJTOG 3405, OPTIMAL, and EURTAC) included only EGFR-mutated patients, the two others had both EGFR-mutated and wild-type patients (IPASS and FIRST-SIGNAL). Among these 2962 patients (1926 in gefitinib studies, 327 in erlotinib studies, and 709 in afatinib studies), there were 2909 adenocarcinomas (98 %, 1906 among patients receiving gefitinib, 294 among those under erlotinib, and 709 afatinib), 1739 mutated tumors (897 showing a deletion in exon 19, 699 with L858R mutation) (143 uncommon mutation including Thr790Met, exon 20 insertions, Gly719X (Gly719Ser, Gly719Ala, or Gly719Cys), Ser768Ile, and Leu861Gln, alone or as complex mutations in two or more exons). Only a small proportion of the patients from IPASS and First SIGNAL trials were assessable for EGFR mutational status. Thus, it is quite possible that more than 1739 EGFR-mutated tumours were indeed included across the trials. There were 448 stage IIIB (373 in the gefitinib group), 2222 stage IV (75 %) (1434 in the gefitinib group), and 2453 never smokers (83 %) (1708 in the gefitinib group, 229 in the erlotinib group and 516 in the afatinib group). Eight hundred and sixty-six patients were ECOG PS 0 (595 in the gefitinib group), 1863 were PS1 (1148 in the gefitinib group), and 187 were PS2 (157 in the gefitinib group).
Compared to chemotherapy, OS was similar among EGFR-mutated patients who first received a TKI or chemotherapy (HR 0.98, 95 % CI 0.87-1.10, fixed-effect model) (Fig. 2). Compared to chemotherapy, EGFR TKIs significantly improved PFS in patients with EGFR mutations (HR 0.37, 95 % CI 0.29-0.49, random-effect model) (Fig. 3). There was no statistically significant difference between gefitinib and erlotinib (RRR 1.73, 95 % CI 0.656-4.566; p = 0.29) or afatinib and erlotinib (RRR 1.53, 95 % CI 0.47-5.05, p = 0.24). However, in the subgroups of patients bearing an exon 19 deletion of both studies involving afatinib, afatinib showed an improved OS compared to chemotherapy [18].
Forest plot of the effect on PFS of EGFR TKIs compared with doublet CT in patients with EGFR mutated NSCLC. 95 % CI 95 % confident interval; CT chemotherapy; EGFR epidermal growth factor receptor; HR hazard ratio; NSCLC non-small-cell-lung cancer; PFS progression free survival; TKIs tyrosine kinase inhibitors
Concerning side-effects, skin rashes (RR 6.29, 95 % CI 4.05-9.77, random-effect model), diarrhoea (RR 3.51, 95 % CI 2.15-5.75, random-effect model), stomatitis (RR 3.57, 95 % CI 1.81-7.04, random-effect model), and interstitial lung disease (RR 6.07, 95 % CI 1.66-22.20, fixed-effect model) were significantly more frequent among the patients receiving first-line TKI, whereas fatigue (RR 0.38, 95 % CI 0.32-0.45, fixed-effect model), anorexia (RR 0.42, 95 % CI 0.34-0.54, random-effect model), nausea/vomiting (RR 0.19, 95 % CI 0.11-0.32, random-effect model), and alopecia (RR 0.12, 95 % CI 0.06-0.24, fixed-effect model) were significantly more frequent among patients receiving first-line chemotherapy. As expected, the biological side-effects leucopenia (RR 0.14, 95 % CI 0.08-0.24, random-effect model), thrombocytopenia (RR 0.18, 95 % CI 0.09-0.35, random-effect model), and anaemia (RR 0.22, 95 % CI 0.15-0.33, random-effect model) were significantly more frequent among patients receiving first-line chemotherapy. Concerning grade 3-4 side-effects, similarly rashes and diarrhoea were significantly more frequent after TKIs (RRs 4.60, 95 % CI 2.37-8.95 and 3.88, 2.00-7.56, both with fixed-effect model), whereas nausea/vomiting (RR 0.22, 95 % CI 0.09-0.54, fixed-effect model), neutropenia (RR 0.06, 95 % CI 0.04-0.08, fixed-effect model), thrombocytopenia (RR 0.11, 95 % CI 0.04-0.32, fixed-effect model), and anaemia (RR 0.10, 95 % CI 0.04-0.27, fixed-effect model) were significantly more frequent after first-line chemotherapy.
4 Discussion
Our meta-analysis of the eight phase III randomized controlled trials comparing first-line treatment by an EGFR TKI monotherapy or by doublet chemotherapy in advanced NSCLC showed that TKIs (gefitinib, erlotinib, and afatinib) did not improve OS, but significantly improved PFS in EGFR-mutated patients compared to chemotherapy. The major discrepancy between a markedly improved PFS and an unchanged OS when first-line TKI treatment was compared to first-line chemotherapy could be explained by the high level of crossing-over, many patients treated with first-line TKI receiving thereafter second-line chemotherapy and conversely, many patients treated with first-line chemotherapy receiving second-line TKI. This probably led to a carryover effect, which could bias the results. In EGFR-mutated patients, TKIs should be prescribed as first line therapy due to a better safety profile. There is a general agreement in the literature that wild type patients should receive chemotherapy first.
Several other MAs have assessed studies of front-line therapy with EGFR TKIs in the setting of NSCLC.
The MA by Lee CK et al. [22] found 13 studies of front-line therapy with TKIs. Among these 13 front-line trials, eight compared EGFR TKIs as monotherapy with chemotherapy, four compared TKIs plus chemotherapy with chemotherapy alone, and one was a placebo-controlled trial. The authors of this MA only provided overall results from the 13 front-line trials but did not provide specific results from the eight trials comparing TKIs as monotherapy with chemotherapy, the comparison which seems the most appropriate and that we performed. Thus, the results of this MA cannot be compared with ours.
The MA by Gao [23] included only the four trials with gefitinib as monotherapy vs. chemotherapy and the two trials with erlotinib as monotherapy. Like our MA, these authors found that TKIs significantly increased PFS but did not modify OS. Our MA updates the results of this previous MA by adding more recent data for some of the six trials included dealing with gefitinib and erlotinib and by including two additional trials assessing afatinib, namely, LUX Lung 3 and LUX Lung 6. In addition, our MA assessed the side effects of TKIs and chemotherapy.
Very recently, a network meta-analysis (NMA) was published by Popat et al. [24]. This NMA included RCTs comparing EGFR-TKIs with doublet chemotherapy in first line NSCLC but also all trials comparing various regimens of chemotherapy in order to perform indirect comparisons between the 3 TKIs (no statistically significant difference either in PFS or in OS between the 3 TKIs). It did not assess side-effects of TKIs and of chemotherapy. It did not compare the efficacy on OS of EGFR TKIs among mutated and wild-type patients.
Finally, the MA by Haaland et al. [25] , which assessed separately the HRs PFS for each of the three TKIs compared with chemotherapy (with each of all three TKIs being statistically significantly better than chemotherapy, with no difference between TKIs) and no evidence that gefitinib, erlotinib of afatinib improved OS compared with chemotherapy.
Considering these results (no superior effect on OS of TKIs over chemotherapy in mutated patients, contrasting with a marked beneficial effect on PFS), studies of longer duration, perhaps with a different design (run-in phase of fixed duration with a TKI for all mutated patients, followed by randomization between chemotherapy and prolonged TKI before the appearance of a resistance to TKI therapy) should be undertaken. Future studies should compare various TKIs, such as the LUX-Lung 7 study, a head-t- head phase IIb trial comparing afatinib with gefitinib in first line treatment of mutated lung adenocarcinomas.
Together, exon 19 deletions and punctual mutation L858R located inside exon 21 represent 85 % of all EGFR mutations and confer a major sensitivity of tumour cells to TKIs [26]. More generally, all kinds of mutations do not confer the same sensitivity to TKIs. Some mutations confer a resistance to TKIs. Actually, tumours from patients treated with gefitinib or erlotinib may present a secondary resistance to these TKIs, possibly related to the T790M mutation inside exon 20. This later mutation is present in about 50 % of patients with acquired resistance to TKIs [27]. The occurrence of this mutation is probably related to selection pressure since it is rarely detected in naive patients. Another mutation conferring resistance to TKIs is D761Y mutation in exon 19, although much more frequently found than T790M [27]. Punctual insertions in exon 20 are also associated with poorer responses to TKIs. A recent study confirmed that sensitivity of tumour cells to TKIs varies greatly with the kind of mutation and that some mutations confer a modified sensitivity to erlotinib or gefitinib [28]. For both LUX-Lung 3 and LUX-Lung 6 studies, results were better in the Del19 subgroup. Therefore, the effects of TKIs should be studied more specifically in the various kinds of EGFR mutations.
5 Conclusion
The present MA shows no benefit on OS of first-line TKIs monotherapy compared with first-line chemotherapy in NSCLC. However, afatinib shows promising results in del19 patients. In EGFR-mutated patients, TKIs should be prescribed as first line therapy due to a better safety profile. Ongoing studies aim to compare the effects of various TKIs in order to determine the best therapeutic option. In wild-type patients or patients with unknown mutational status, first-line treatment should be chemotherapy.
References
Douillard JY, Shepherd FA, Hirsh V, Mok T et al (2010) Molecular predictors of outcome with gefitinib and docetaxel in previously treated non-small-cell lung cancer: data from the randomized phase III INTEREST trial. J Clin Oncol 28:744–52
Cappuzzo F, Ciuleanu T, Stelmakh L, Cicenas S et al (2010) Erlotinib as maintenance treatment in advanced non-small-cell lung cancer: a multicentre, randomised, placebo-controlled phase 3 study. Lancet Oncol 11:521–9
Tsao MS, Sakurada A, Cutz JC, Zhu CQ et al (2005) Erlotinib in lung cancer - molecular and clinical predictors of outcome. N Engl J Med 353:133–44
Marchetti A, Felicioni L, Buttitta F (2006) Assessing EGFR mutations. N Engl J Med 354:526–8
Calvo E, Baselga J (2006) Ethnic differences in response to epidermal growth factor receptor tyrosine kinase inhibitors. J Clin Oncol 24:2158–63
Rosell R, Carcereny E, Gervais R, Vergnenegre A et al (2012) Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer(EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 13:239–46
Lee JS, Park K, Kim SW A randomized phase III study of gefitinib versus standard chemotherapy (gemcitabin plus cisplatin) as a first-line treatment for neversmokers with advanced or metastatic adenocarcinoma of the lung. 13th World Conference on Lung Cancer 2009; abstr PRS.4
Zhou C, Wu Y, Chen G, Feng J et al (2011) Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 12:735–42
Mitsudomi T, Morita S, Yatabe Y, Negoro S et al (2010) Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open-label, randomised phase 3 trial. Lancet Oncol 11:121–8
Maemondo M, Inoue A, Kobayashi K, Sugawara S et al (2010) Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 362:2380–8
Mok TS, Wu Y, Thongprasert S, Yang C et al (2009) Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 361:947–57
Han JY, Park K, Kim SW, Lee DH et al (2012) First-SIGNAL: firstline single-agent iressa versus gemcitabine and cisplatin trial in never-smokers with adenocarcinoma of the lung. J Clin Oncol 30:1122–8
Inoue A, Kobayashi K, Maemondo M, Sugawara S et al (2013) Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin-paclitaxel for chemo-naïve non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002). Ann Oncol 24:54–9
Fukuoka M, Wu YL, Thongprasert S, Sunpaweravong P et al (2011) Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). J Clin Oncol 21:2866–74
Zhou C, Wu YL, Liu X, Wang C, et al Overall survival (OS) results from OPTIMAL (CTONG0802), a phase III trial of erlotinib (E) versus carboplatin plus gemcitabine (GC) as first-line treatment for Chinese patients with EGFR mutation-positive advanced non-small cell lung cancer (NSCLC). ASCO MEETING ABSTRACTS May 30, 2012:7520
Sequist LV, Yang JC, Yamamoto N, O’Byrne K et al (2013) Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 31:3327–34
Wu YL, Zhou C, Hu CP, Feng JF, et al LUX-Lung 6: a randomized, open-label, Phase III study of afatinib (A) vs gemcitabine/cisplatin (GC) as first-line treatment for Asian patients (pts) with EGFR mutation-positive (EGFR M+) advanced adenocarcinoma of the lung. ASCO Annual Meeting 2013. Abstract 8016
Yang JC, Wu YL, Schuler M, Sebastian M et al (2015) Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol 16:141–51
Yoshioka H, Mitsudomi T, Morita S, Yatabe Y et al (2014) Final overall survival results of WJTOG 3405, a randomized phase 3 trial comparing gefitinib (G) with cisplatin plus docetaxel (CD) as the first-line treatment for patients with non-small cell lung cancer (NSCLC) harboring mutations of the epidermal growth factor receptor (EGFR). Proc Am Soc Clin Oncol 32(suppl):8117, abstr
Zhou C, Wu YL, Liu X, Wang C et al (2012) Overall survival (OS) results from OPTIMAL (CTONG0802), a phase III trial of erlotinib (E) versus carboplatin plus gemcitabine (GC) as fi rst-line treatment for Chinese patients with EGFR mutation-positive advanced non-small cell lung cancer (NSCLC). Proc Am Soc Clin Oncol 30(suppl):7520, abstr
Leon LF, Golsorkhi A, Liu S, Drozdowskyj A, et al Overall survival analyses of first-line erlotinib versus chemotherapy in the EURTAC study population controlling for the use of post-study therapy. ESMO 2014; 1273(P)
Lee CK, Brown C, Gralla RJ, Hirsh V et al (2013) Impact of EGFR inhibitor in non-small cell lung cancer on progression-free and overall survival: a meta-analysis. J Natl Cancer Inst 105:595–605
Gao G, Ren S, Li A, Xu J et al (2012) Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor (EGFR TKI) therapy is effective as first-line treatment of advanced non-small-cell lung cancer with mutated EGFR: A meta-analysis from 6 phase III randomized controlled trials. Int J Cancer 131:822–9
Popat S, Mok T, Yang JC, Wu YL et al (2014) Afatinib in the treatment of EGFR mutation-positive NSCLC–a network meta-analysis. Lung Cancer 85:230–8
Haaland B, Tan PS, de Castro G, Jr LG (2014) Meta-analysis of first-line therapies in advanced non-small-cell lung cancer harboring EGFR-activating mutations. J Thorac Oncol 9:805–11
Rosell R, Perez-Roca L, Sanchez JJ, Cobo M et al (2009) Customized treatment in non-small-cell lung cancer based on EGFR mutations and BRCA1 mRNA expression. PLoS One 4:5133
Sharma SV, Bell DW, Settleman J, Haber DA (2007) Epidermal growth factor receptor mutations in lung cancer. Nat Rev Cancer 7:169–81
Kancha RK, von Bubnoff N, Peschel C, Duyster J (2009) Functional analysis of epidermal growth factor receptor (EGFR) mutations and potential implications for EGFR targeted therapy. Clin Cancer Res 15:460–7
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guetz, G.D., Landre, T., Uzzan, B. et al. Is There a Survival Benefit of First-Line Epidermal Growth Factor Receptor Tyrosine-Kinase Inhibitor Monotherapy Versus Chemotherapy in Patients with Advanced Non-Small-Cell Lung Cancer?: A Meta-Analysis. Targ Oncol 11, 41–47 (2016). https://doi.org/10.1007/s11523-015-0373-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-015-0373-x