Abstract
The objective of this study was to evaluate the accuracy of independent hydric data for the quantification of total body water (V t), extracellular water (V e) and intracellular water (V i), obtained by a multifrequency impedancemeter Z-Métrix® (ZM), in standing and lying position, with respect to the Xitron reference. In a second step, the aim was to consider whether it is possible to quantify daily hydration. The average repeatability error of the ZM impedancemeter is less than 0.5 %. For total body water (V t), we note a low R 2 dispersion with an average of 0.9 for men and 0.6 for women. The estimation of extracellular water is equivalent to a maximum error of 3.1 % in standing position for women against 2.97 % for men in the same position. The estimation of the total body water by direct measurement and by summing the volumes of extracellular and intracellular water obtained by the Z-Metrix® shows very low dispersions with R 2 = 0.89 and average error from 1.3 % for healthy women in lying position to 3.9 % for healthy women in standing position. Finally, despite the impact of events on the daily measurements, it is viable to track a subject’s overall hydration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Most of foot-to-foot impedancemeters usually offer tissue data such as fat mass (FM), fat-free mass (FFM) and even estimates of bone mineral content (BMC) [7, 12–14]. Some have gradually evolved to provide water indices, usually obtained from the universal hydration rate of 73.2 % [4] or using anthropometry equations. Wrist–ankle impedancemeters more often provide extracellular water volume (V e) [2]. However, the intracellular water volume (V i) is usually derived by subtracting V e to total water volume (V t), or by using an equation that takes V e into account [8]; in that case, V t is the sum of V e and V i. This new impedancemeter offers to quantify water volumes of extracellular, intracellular and total compartments independently, in order to help locate with higher precision the compartment affected by a hydric disorder. It does not use intracellular as the difference between total and extracellular volume but three different equations using three different resistances.
When measured in clinical or sports routine, the subjects can be in supine or standing position. This is why it is necessary to have validated the equations for the two types of position; all the more so because the fluid accumulates especially in the lower body in standing position. This new impedancemeter enables to quantify V i, V e and V t indices, in both supine and standing position.
Thus, the objective of this study is to evaluate this device, which provides clinical and sports routine with a fast and inexpensive comprehensive diagnostic tool for detecting water edema (due to venous insufficiency, burns, heart failure, post-effort, etc.) or dehydration (malnutrition, post-effort, etc.).
2 Materials and methods
The reference device used in this study is the Hydra® 4200 Xitron (Xitron Tech, San Diego, USA), validated by isotope dilution [3]. It scans frequencies from 1 to 1000 kHz and requests that the subject be measured in supine position. Figure 1 shows the device.
The multifrequency impedancemeter evaluated is the Z-Metrix® (BIOPARHOM Company, France). It runs on a 9-V battery and delivers a sinusoidal current of about 77 µA. It uses ECG electrodes from the 3 M Company (reference 2660-5). It can be used to scan frequencies from 1 to 1000 kHz. Figure 2 shows the comparison between the data provided by the device and the theoretical curve of a phantom representing a healthy human body, according to Cole–Cole modeling [5], with Ri = 910 Ω, Re = 680 Ω and membrane capacitance of 2.7 nF.
The device provides an impedance with an average error of 0.95 ± 1.58 % with respect to the theory of the whole frequency range and of 0.980° ± 1.100° for the phase angle. We note repeatability errors on an average of 0.55 ± 0.38 % for Z and of 0.440° ± 0.350° for the phase angle on the same phantom. The device, on an healthy subject rather than on a phantom, gives an average repeatability error of 0.560° on the phase angle for the range of 1–1000 kHz and an average repeatability error of 1.3 % over the entire frequency range on the values of resistances R and reactances X. Electrical measurement accuracy is ensured through a system of compensation of the parasitic capacitances of cables and electrodes, as well as an internal self-calibration of the hard electronics. Figure 3 shows a picture of the multifrequency impedancemeter evaluated.
We conducted this clinical study in compliance with the Ethics Committee of Northwestern France, who gave us the following accreditation number: 2008-A01373-52. This work was carried out within the Center for Advanced Medical Imaging in the hospital of Compiegne (France). 48 women and 47 men underwent the Z-Metrix® measurements. These were made in standing and supine position, after the subject, wearing a light blouse, was weighed and measured. Table 1 shows the characteristics of the population of healthy subjects who participated in the study.
The average body mass index (BMI) is above the healthy limit for men because some obese subjects were tested during the study. The data are processed by Student’s paired statistical tests and Bland–Altman graphs [1].
This ZM device quantifies extracellular water (V e) by the method of De Lorenzo et al. [2], total body water (V t) by the method of Jaffrin et al. [6] and intracellular water (V i) by an undisclosed method of the device. Same models are used in standing or supine position.
The innovative principle of the new method of Jaffrin et al. is to consider total body water as an electrically homogeneous compartment. They consider that there are always extracellular and intracellular compartments, but there are also communicating vessels, in particular ion channels and aquaporins. Therefore, it would be more appropriate to consider total body water as a whole rather than as the sum of two volumes [9].
A subpopulation consisting of 14 women and 15 men, ages 17–72 and BMI 21.4–38.6 kg/m2 were also measured by Xitron to validate the accuracy of the water volumes found. The population was deliberately very heterogeneous (in terms of weight, height, BMI, age, etc.) in order to be sure to validate the model on a wide variety of healthy subjects. The method has been previously validated [6] in a population of 95 healthy subjects, hemodialysis' patients and in anorexics too [11].
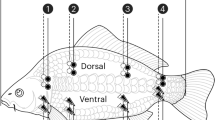
The device performs measurements of body composition with disposable medical electrodes, such as ECG, using a tetrapolar method with electrodes at the wrists and ankles, right or left body.
The “hand” electrode is positioned on the hand in bones of the phalanges. The “wrist” electrode is positioned at the wrist. The “ankle” electrode is positioned at the ankle bone (the outer ankle bone). The “leg” electrode is positioned 5 cm above the ankle.
3 Results and discussion
3.1 What is the repeatability of these hydric indices?
Table 2 shows the percentage of repeatability error (device, including cables and electrodes) in hydric indices in one healthy subject during 50 min. Any variation more than 0.25 % hydration rate comes from changes related to the individual and not from the device.
3.2 What is the accuracy of these water indexes?
As Table 3 shows, there is no significant difference between the total body water volume given by Z-Metrix and that given by the Xitron reference, whether for men or for women, in standing or supine position. There is an average error of 0.6 and 0.4 L in women, respectively, in supine and standing position. For men, there is an average error of 1.6 and 1.7 L, respectively, in supine and standing position.
For extracellular volumes, there is an insignificant 0.3 L error for women in supine position and a significant 0.4 L error (P = 0.04) in standing position. For men, there were insignificant errors of 0.2 L in supine position and of 0.6 L in standing position.
We have not tested Viz against Xitron Vix because this index is not validated for this device, obtained by including Vex.
Figure 4a, b shows an example of the distribution of total body water in calculated points for women and men, in standing and supine position, using Z-Metrix and Xitron. We note a low R 2 dispersion with an average of, respectively, 0.9 for men and 0.6 for women. The estimation of the total body water is more accurate in women with a maximum 1.8 % error rate for standing position against 3.9 % for men in the same position.
Figure 5a, b shows an example of the distribution of Ve calculated for women and men, in standing and supine position, using Z-Metrix and Xitron. We note a low R 2 dispersion of, respectively, 0.96 for men and of 0.84 for women. The estimation of extracellular water is equivalent to a maximum error of 3.1 % in standing position for women against 2.9 % for men in the same position.
Figure 6 shows the differences between the estimated total body water obtained by direct measurement and that obtained by summing the volumes of extracellular water and intracellular water found by the Z-Metrix®. We note very low R 2 dispersions with a high of 0.89 and errors ranging from 1.3 % for women in supine position to 3.9 % for women in standing position. This indirectly validates the independent estimation of the intracellular water volume (Viz).
If we compare V i as the difference between total and extracellular water (ICWdiff) and our new method (ICWnm), mean between ICWdiff and ICWnm is summarized in Table 4.
3.3 Application by monitoring daily hydration on a case study
A complaint is often made on the impedance sensitivity to everyday events (meals, travel, etc.), leading to difficulties in interpreting data for monitoring.
Like any measure, it is obviously preferable that it be taken each time in the same conditions (time, weight, etc.). We wanted to test whether it was possible to elaborate an interpretation of monitoring data for hydration, despite measures being taken at any time of the day and in different conditions.
To do so, we asked some subjects—two typical examples are given here—a sportsman (subject B) and a healthy woman (subject C), to submit to measurements throughout the day, before and after any action (meals, fluid intake, the toilet, travel, rest, work, etc.). In addition, we induced dehydration and rehydration, to try to understand these trends despite possible fluctuations in impedance measurements, due to everyday life events.
Thus, the protocol consists in eating and accurately performing the same events at the same time of the day for 2 days. The first day (D1) serves as normohydration reference. The subject should be hydrated. During D1, subjects have usual intakes. The subjects drank about 1 L of water during the day and ate vegetables at one of the two meals. However, no fluid intake is permitted during the second day (D2). Some measurements were taken on day 3 (D3) to see the effect of recovery drinking on the beginning of rehydration. The subjects began to drink water from the wake. Fat free mass (FFM) and lean body mass (LBM) are given by the device [10].
3.3.1 Subject B: young male athlete
In Fig. 7, there is no direct link between fluid intakes and V t/W ratio, and even the result is the opposite of what one would expect with increased hydration after using the bathroom. It seems that the water volume is well measured in tissues and the “wrist–ankle” electric currents do not pass into the bladder or stomach, which is not unlikely. In addition, with regard to the stomach, one might think that measurements taken on the left side of the body would show this kind of variation. Regarding the bladder, foot-to-foot measures compare well measurements made on the whole body.
Thus again we find a discrepancy between the drinking and the impact on the hydration measure, which, as we have already explained, is not necessarily inconsistent. Furthermore, if indeed all the drinking water is not absorbed and a consistent part of it goes to the bladder, it is normal not to find it in the extracellular volume. The rehydration on day 3 should be further analyzed on both the extracellular and intracellular levels to better understand the dehydration day. It seems that for proper hydration it is better to take small drinks in order to allow a better and probably faster absorption that is directly accessible to the tissues.
Regarding the overall hydration rate of the body, there is therefore a normohydration average on day 1 with a mean change of 0.06 % despite the variations due to the different actions done during the day. Then, we note a dehydration average of 12 % during the second day, and finally, the average goes back down to 7 % at the beginning of rehydration on day 3.
As already mentioned, the increase on day 3 was difficult for every subject, as they all absorbed large amounts of water. The first goal was to observe the dehydration phase so there were no restrictions to subjects on day 3. They have not quantified or rationed their fluid intake in the morning of day 3. It is true that part of this protocol would require a rehydration phase including comparisons of the rationed quantities with body composition measured on the left side and the right side and by foot-to-foot method.
Figure 8 reinforces the conclusions of Fig. 7.
Figure 9 shows the variations of the ratio V t/LBM. We find the same information in the global Figs. 7 and 8.
Unexpectedly, although the hydration degree is very stable, the total water volume shows an average increase of about 900 mL as shown in Fig. 10. This is averaged in the moisture by an increase in weight. Although he drinks very little in general, on this day the subject shows unusual normohydration for his body. Therefore, these new water supplies may have been stored unexpectedly. A total water loss of 1.5 L on average was noted at bedtime on day 2, but it was 3.5 L in the morning of day 3. This subject tends to urinate in the night. We note the same point between days 1 and 2 with a water loss of approximately 1.5 L overnight with two urinations.
In the morning of day 3, there is already a total body water recovery of 1.1 L.
We note in Figs. 11 and 12 that the increase in total body water on the first day is divided into the extracellular and the intracellular compartments with an average increase of 250 mL for V ez and of 500 mL for Viz. Day 2 indicates an average loss of 750 mL for each compartment. There was a recovery of 500 mL for each compartment at the beginning of the 3rd day.
It may be interesting to focus on measures 11–15 which noted a sharp decrease in intracellular combined with an increase in extracellular volume. A dump intracellular to extracellular can therefore be assumed.
3.3.2 Subject C: healthy young woman
Women’s monitoring tends to be more complex because of hormonal changes. Models are more difficult to establish with the same precision as for men. It is why it was essential that a woman participated in the protocol.
We note in Fig. 13, as was the case for subject B, an average increase in overall body hydration during day 1 with a 1.9 % rate and not considering the average slope. This day, intended to serve as reference shows that hydration is already back to normal. We noted a 1.7 % average rate during day 2, but a 4 % hydration loss if one looks at the maximum rate at sunset after a normal day of drinking. Day 3 then indicates a hydration recovery of about 1 %.
Figures 14 and 15 show the same trends as Fig. 13. Again we note a very noisy graph despite the weight gained independently. We do not see any explanation for this observation.
We note, in Fig. 16, an average increase of 1.5 L in total body water on day 1. Again, a significant loss of about 2 L occurred in the night. The nights were particularly warm during the month of July. The alcohol intake in the evening was meant to imitate normal life habits but also to test the impact of dehydration on the subjects. Presumably, as is also the case with soft drinks, the impact of alcohol intake (the evening before) occurs only after a certain period of digestion and does not yet appear in the evening measures but rather in the next morning. Day 2 saw a day loss of 1 L but a total of over 3 L if one also considers the night loss. The early morning and early recovery drink did not have a real immediate impact, showing a recovery of about 400 mL in the morning of day 3. Only three measurements were performed.
Figures 17 and 18 show the variations of subject C’s extra and intracellular compartments. Unlike B whose water intake on the first day was primarily extracellular with 900 mL against 100 mL for intracellular, there is a difference of about 0.5 L with water measured directly by V tz. The timing of the menstrual cycle of the woman is not known. We know, for example, that during menstruation, metabolic index rates can be caused to increase due to high membrane activity. Thus, menstrual periods could perhaps explain this difference. Day 2 indicates a loss of 600 mL in extracellular compartment against 300 mL in intracellular compartment, which summed to many diurnal total water losses. If we consider also the night losses, there is an extracellular water loss of 1.7 L and an intracellular water loss of 800 mL. The beginning of day 3 indicates average recovery of approximately 200 and 100 mL for extracellular and intracellular.
We note that the intracellular data are very noisy. One might think that this is a particular behavior of cell membranes. This could be checked with other women.
4 Conclusion
The objective of this study was to evaluate a new multifrequency impedancemeter enabling measurements of water volumes, in standing and supine position, and independently giving total, extracellular and intracellular water compartments.
It has been shown that the device gave more accurate measurements in supine position than in standing position even if the error rate for values in standing position was inferior to 4 %, offering an ergonomic advantage for clinical and sports routine. In addition, the variability of the device, essential when monitoring, remains on average below 1 %, which means that any greater variation comes from the patient.
Finally, although these results need to be clarified in a larger population, it was noted that although the impedance is indeed impacted by daily hazards, it still allows the hydration trend to be observed.
References
Bland J, Altmann DG (1996) Statistical methods for assessing agreement between two methods of clinical measurements. Lancet 1:307–313
De Lorenzo A, Andreoli A, Matthie JR, Withers P (1997) Predicting body cell mass with bio-impedance by using theoretical methods: a technological review. J Appl Physiol 82:1542–1558
Ellis KJ, Wong WW (1998) Human hydrometry comparison of multifrequency bioelectrical impedance with H2O and bromine dilution. J Appl Physiol 85:1056–1062
Genton L, Hans D, Kyle UG, Pichard C (2002) Dual energy X-ray absorptiometry and body composition: differences between devices and comparison with reference methods. Nutrition 18:66–70
Grimnes S, Martinsen OG (2005) Cole electrical impedance model-A critique and an alternative. IEEE Trans Biomed Eng 52(1):132–135
Jaffrin MY, Fenech M, Moreno MV, Kieffer R (2006) Total body water measurements by a modification of the bioimpedance spectroscopy method. Med Biol Eng Comput 44:873–882
Lazzer S, Boirie Y, Meyer M, Vermorel M (2003) Evaluation of two foot-to-foot bioelectric impedance analyzers to assess body composition in overweight and obese adolescents. Br J Nutr 90:987–992
Matthie J (2005) Second generation mixture theory equation for estimating intracellular water using bioimpedance spectroscopy. J Appl Physiol 99:780–781
Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A, Korth O, Muller MJ, Ellegard L, Malmros V, Kaitwatcharachai C, Kuhlmann MK, Zhu F, Fuller NJ (2006) Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas 27:921–933
Moreno M-V, Ribbe E, Rebeyrol J, Vannicatte A, Krief L Evaluation of a multifrequency impedancemeter by biphotonic Densitometry, measuring independent tissue indices, in supine and standing position. Comparison with skin folds. (Under Press, Gazetta Medica Italiana)
Moreno M-V, Djeddi D, Jaffrin MY (2008) Assessment of body composition in adolescent subjects with anorexia nervosa by bioimpedance. Med Eng Phys 30(6):783–791
Nunez C, Gallagher D, Visser M, Pi-Sunyer FX, Wang Z, Heymsfield SB (1997) Bioimpedance analysis: evaluation of leg-to-leg system based on pressure contact foot-pad electrodes. Med Sci Sports Exerc 29:524–531
Swartz AM, Evans MJ, King GA, Thompson DL (2002) Evaluation of foot-to-foot bioelectrical impedance analyzer in highly active and less active young men. Br J Nutr 88:205–210
Utter AC, Nieman DC, Ward AN, Butterworth DE (1999) Use of leg-to-leg bioelectrical impedance method in assessing body-composition change in obese women. Am J Clin Nutr 6:603–607
Acknowledgments
We, the authors, thank Mr. Jaffrin for lending us the Xitron instrument.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moreno, MV., Ribbe-Cornet, E., Rebeyrol, J. et al. Evaluation of a new impedancemeter to independently measure extracellular, intracellular and total body water volumes: application to the measurement of hydration. Med Biol Eng Comput 53, 989–999 (2015). https://doi.org/10.1007/s11517-015-1305-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-015-1305-8