Abstract
This study evaluates the associations between the urban working-age population’s mental health, material possession, and social capital during the COVID-19 pandemic. The specific stressors examined in this empirical analysis are income level, food insecurity, and virtual psychological support. This paper further examines the differences across the employed and unemployed population groups. We obtained data from the COVID-19 Household Impact Survey and constructed four measures of mental health conditions: Nervous, Depressed, Lonely, and Hopeless. Our empirical analyses use an ordinal regression model that takes both time and regional factors into consideration to control for potential time effects and time-invariant confounders that only vary between regions. For the employed group, the main results suggest that lower income and food insecurity is correlated with a higher frequency of mental health symptoms, while virtual psychological support predicts a better mental health status. For the unemployed group, food insecurity is negatively associated with mental health, and virtual psychological might help alleviate nervousness and depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Studies have reported a high prevalence of psychological distress and disorder among U.S. adults (Iranpour et al., 2022). These mental health issues can lead to long-term post-traumatic stress symptoms, such as drug addiction, alcoholism, and suicide, which can harm both individuals and society as a whole (Moore et al., 2016). Further, mental health issues are associated with other comorbid conditions, such as cardiovascular disease, obesity, and diabetes (Stunkard et al., 2003; Suls & Bunde, 2005). It is evident that mental issues are associated with an increased mortality risk, which is associated with reduced physical activity, physical illnesses, and compromised cognitive functioning of patients (White et al., 2015).
Meanwhile, the COVID-19 pandemic has profoundly changed our daily lives in many ways, especially in terms of the population’s mental health. In the US, mental issues increased noticeably from 2017 to 2020 following the emergence of the COVID-19 pandemic (Brooks et al., 2020; Rajkumar, 2020). A large body of literature suggests that there is a negative correlation between COVID-19 and mental health status. Earlier research suggests that mental health illness is higher relative to pre-COVID-19 levels (Ettman et al., 2020a, 2020b; Liu et al., 2020; McGinty et al., 2020). Existing studies on the association between COVID-19 and mental health have examined the impacts of layoffs and government assistance programs (Fan & Nie, 2020), low assets, and financial stressors (Ettman et al., 2021), and decreased physical activity (Creese et al., 2021). But we do not know which specific population groups experience the consequence of COVID-19 more than others, or what are the roles of losing jobs and incomes in shaping this risk.
This study, therefore, specifically investigates the impacts of food insecurity, income levels, and virtual psychological support on the urban working-age population’s mental health during COVID-19. This research will focus on the urban working-age population during the pandemic. Densely inhabited urban areas are targeted as potential epicenters of infectious diseases, so more draconian policies, such as curfew, social distancing in public spaces, working from home, quarantine, and bars/clubs closing, are implemented in these areas. These control measures significantly affect the urban working-age population by curbing their face-to-face interactions within workplaces and social gatherings. To a certain extent, the COVID-19 pandemic removes the physical psychological support for urban working-age employees, which is achieved through physical or face-to-face interactions with colleagues and friends. Furthermore, existing empirical research highlights differences in dealing with depressive symptoms between urban and non-urban populations(Guo et al., 2018; Li et al., 2016; Norstrand & Xu, 2012; Vogelsang, 2016). Therefore, the empirical exercises in this study primarily focused on urban working-age employees.
This study specifically examines two forms of stressors. The first type of stressor is material possessions, which are proxied by income levels and food insecurity. Existing research finds that the stressors for mental disorders usually include financial losses and inadequate supplies (Pfefferbaum & North, 2020). A large volume of the literature suggests that income inequalities (Erdem et al., 2016; Fryers et al., 2005; Golberstein, 2015; Lorant et al., 2003; Pabayo et al., 2014, 2016; Zimmerman & Bell, 2006) and financial difficulties (Erdem et al., 2016; Ettman et al., 2020a, 2020b) contribute to mental disorders and depressive symptoms. Empirical analyses demonstrate that people with low income (Oh et al., 2018), low levels of education (Chrzastek et al., 2021; Lorant et al., 2003; Peyrot et al., 2013), or no job (Cygan-Rehm et al., 2017; Tefft, 2011; Zivin et al., 2011) are at an increased risk of depression. These inequalities can be explained by limited access to care for poor Americans (Dickman et al., 2017), lack of social support leading the rich to withdraw support for public services (Kawachi et al., 1999), feelings of insecurity and shame (Wilkinson & Pickett, 2006), and unhealthy behaviors (Stansfeld et al., 2003). An existing study focusing on non-elderly adults in the U.S. finds that income increases lead to improvements in depressive symptoms (Ettner, 1996).
During a crisis such as COVID-19, people are at the risk of being exposed to food insecurity due to job loss or reduced income (Wolfson & Leung, 2020). Since mid-March 2020, numerous surveys have documented unprecedented levels of food insecurity that eclipse anything seen in recent decades in the United States, including during the Great Recession. Existing empirical analyses across the globe have demonstrated that food insecurity is associated with poorer mental health and specific psychosocial stressors, independent of socioeconomic status (Jones, 2017). This result has been shown to hold in high-income countries (Maynard et al., 2018). Furthermore, food insecurity can provoke feelings of aggravation, worry, and depression concerning the ability to maintain food supplies or acquire sufficient food in the future (Campbell, 1991; Kessler, 1997; Whitaker et al., 2006). Although more prevalent in low-income countries (Weaver & Hadley, 2009), food insecurity has become a growing and persistent concern in high-income countries. In North America, for example, rates of household food insecurity have remained stable or even increased in the last several years (Maynard et al., 2018). The limited access to food caused by economic and financial losses during COVID-19 puts individuals and families under the same stress. As the Food and Agriculture Organization of the United Nations stated in June, 2020, although globally there is enough food for everyone, the significant decline in economic growth due to the pandemic has translated into an issue of access to food (FAO, 2020).
The second potential stressor is social capital. According to Putnam (1993), social capital is the “features of social organization, such as trust, norms, and networks that can improve the efficiency of society by facilitating coordinated actions.” At the individual level, Glaeser et al. (2002) highlight social capital as the individual’s social characteristics including social skills, charisma, and material possessions that enable non-market returns via interaction with others. Social capital can also involve membership in groups and networks to secure benefits (Sobel, 2002). Prior empirical research shows that higher social capital has protective effects on depressive symptoms (Nummela et al., 2008; Takagi et al., 2013). Economic research using U.S. data finds that a higher degree of individual social capital is associated with higher objective social status (Bucciol et al., 2019). Individuals care about social status as a distinctive feature within society (Truyts, 2010), which is strongly correlated with psychological functioning and other important health-related factors (Lorant et al., 2003; Macleod et al., 2007; Sakurai et al., 2010; Singh-Manoux et al., 2005).
Moreover, social network theory suggests that one’s social capital includes social status, social contact, and opportunity for control (Atkinson et al., 1987; Jahoda, 1982; Warr, 1994), which is the enabling mechanism for social participation (Almedom, 2005; Putnam, 1995). In addition, income and feelings of financial security are significant predictors of subjective social status (Singh-Manoux et al., 2003). On top of that, people with a lower social status generally have lower levels of social capital, and that lack of social capital is related to reduced health status (Uphoff et al., 2013, p. 8). This relationship is supported by strong evidence from empirical studies conducted in the United States (Dean & Sharkey, 2011; German & Latkin, 2011; Kawachi et al., 1997). Based on these findings, social capital could be further divided into three categories—physical psychological support through direct interaction with others, like work-related social participation, virtual psychological support through indirect interaction with people, such as phone calls and text messages, and income levels that reflect one’s social status.
Given the above explanation, material possessions and social capital can be divided into the stressors of food insecurity, income level, virtual psychological support, and physical psychological support. For material possessions, the specific stressors are income level and food insecurity, which are fundamentally related to social capital. Regarding social capital, the specific stressors include income level, virtual psychological support, and physical psychological support. As illustrated in Fig. 1a, quarantine policies, layoffs, and furloughs could remove physical psychological support related to work-based social networks (Goldman-Mellor et al., 2010). This will reduce an individual’s resilience to mental health conditions (Koltai, 2018). Figure 1b illustrates how unemployed and furloughed individuals in the urban population are further deprived of their typical income level.
Our research brings a contribution to the current studies on mental health during Covid-19, which adds to the existing studies that have examined the associations between income, social capital, and mental health (Cygan-Rehm et al., 2017; Golberstein, 2015; Jones, 2017; Maynard et al., 2018; Sorsdahl et al., 2011; Takagi et al., 2013; Tefft, 2011). However, these studies tend to focus on limited stressors. For example, Wolfson and Leung (2020), Fang et al. (2021), and McAuliffe et al. (2021) only investigated the effects of food insecurity. Ettman et al. (2021) only focused on the influences of asset and financial stressors on depression. Creese et al. (2021) focused on reduced physical activities but the mental health measurement is limited to only loneliness. Liu et al. (2020) discussed the significance of family and social support to mental health, but their scope is focused on young adults instead of the working population. Fan and Nie (2020) studied the mental health of the urban working population yet the stressors focus on income losses and government assistance programs. Our study integrated both food insecurity, financial stressors, as well as social support in the investigation, providing a more comprehensive picture of the association between the stressors and mental health.
This empirical study evaluates the impacts of food insecurity, income level, and virtual psychological support during COVID-19 on the urban working-age population’s mental health. In order to differentiate the impact of income level from the impacts of food insecurity and virtual psychological support, we stratify the analysis by the employed urban population and the unemployed and furloughed urban population.
Data, Variables, and Methods
Data Source
The data source for this study is the COVID-19 Household Impact Survey, which is a philanthropic project funded by the Data Foundation and conducted by the University of Chicago’s National Opinion Research Center (NORC) (Wozniak et al., 2020). The survey was originally based on a proposal developed by the Federal Reserve Bank of Minneapolis and further applied by advisors to the COVID-19 Household Impact Survey project. The survey includes three core modules—physical health, social and mental health, and economic and financial health. For the physical health module, questions include symptoms related to COVID-19, relevant existing conditions, and health insurance coverage. In the social and mental health module, questions are designed to align with the current population survey, focusing on communication with friends and family, volunteerism, and anxiety. The last module on economic and financial health prioritizes questions about government cash assistance, employment, and food security. The survey also collects important demographic characteristics, such as age, gender, race, and household income.
The survey targets two types of samples—a nationally representative sample of adults ages 18 and above in the United States and a regional representative sample of adults ages 18 and older living in 18 different geographic areas, including 10 states and 8 Metropolitan Statistical Areas (MSAs). These states include California, Colorado, Florida, Louisiana, Minnesota, Missouri, Montana, New York, Oregon, and Texas, while the MSAs include Atlanta-Sandy Springs-Alpharetta, Georgia; Baltimore-Columbia-Towson, Maryland; Birmingham-Hoover, Alabama; Chicago-Naperville-Elgin, Illinois-Indiana-Wisconsin; Cleveland-Elyria, Ohio; Columbus, Ohio; Phoenix-Mesa-Chandler, Arizona; and Pittsburgh, Pennsylvania. These regions are fixed effects in the empirical analysis because interregional income and socioeconomic status inequalities exist across the U.S. (Pabayo et al., 2014; Rey, 2018). NORC employs two sampling techniques—AmeriSpeak, a probability-based panel designed to be representative of the U.S. household population, and a Multi-mode Address Based Sample (ABS), which is a sampling frame based on an extract of the U.S. Postal Service delivery-sequence file. The field reports on the COVID Impact Survey official website provide details on both techniques.
As of June, three waves of the samples have been collected and made available with survey field periods of April 20–26, May 4–10, and May 30-June 8. These samples contain 25,269 observations with completed interviews with 34.79% (8,790) from the first wave, 35.51 (8,974) from the second wave, and 29.7% (7,505) from the third wave, consisting of 92.64% (23,408) web interviews and 7.36% (1,861) phone interviews. Among these samples, 74.38% (18,794) are sampled through the ABS approach and 25.62% (6,475) are sampled through the AmeriSpeak approach.
Urban Working-Age Employees
As mentioned earlier, the urban working-age population is affected by shutting down face-to-face interactions within workplaces and social gatherings, like bars and clubs. It removes the source of physical psychological support for urban working-age employees. This lays a good foundation for the study to differentiate the association of virtual psychological support and income level with mental health. Virtual conversations with friends and family members by phone or text could relieve pressure and provide social support(Almedom, 2005; Atkinson et al., 1987; Jahoda, 1982; Putnam, 1995; Warr, 1994). In this analysis, we use the change in frequency of communication with friends and family by phone, text, email, app, or the Internet to represent virtual psychological support.
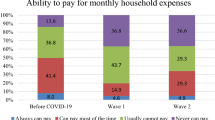
After cleaning the raw data, the three survey waves include 7,295 non-retired, non-self-employed urban working individuals ages 18 and above within specified geographic areas. None of these individuals have been diagnosed with mental health conditions, infected with or recovered from COVID-19, isolated due to COVID-19 exposure, or lived with and cared for someone infected by the virus. In the 7 days prior to the field interview, the sampled individuals have not felt hot, feverish, chilly, cold, or bad chills. To investigate “precisely” the correlations between mental health and income levels and food insecurity during COVID-19, those who had not worked any hours before March 1st, 2020 (when the virus started spreading in the U.S.) are dropped from the relevant sample. The samples are described with sensitivity across four dimensions—layoff status, income levels, food insecurity status, and age intervals. In the relevant sample, 22.81% are laid off during the virus outbreak, 13.13% experienced food insecurity, 3.74% are aged 18–22, 86.22% are aged 23–64, and 10.03% are aged 65 and above. For the income levels (individual total pre-tax income in 2019 from all sources including wages, salaries, tips, business, interest, and alimony), 25.3% report earning more than $125 k, 38.17% report earning $60 k to less than $125 k, 21.51% report earning $30 k to less than $60 k, and 15.01% report earning less than $30 k. These cut-offs are based on the original dataset of NORC. Fig. 2 in the Appendix shows more details.
Mental Health
We construct four measures of mental health conditions based on the survey question SOC5—Nervous, Depressed, Lonely, and Hopeless. In this question, interviewees were asked to report the frequency of feeling these four emotions in the 7 days prior to the survey. The responses range from not at all or less than 1 day, 1–2 days, 3–4 days, to 5–7 days. Out of the 7,295 observations among the urban working-age population, 64% of the interviewees did not have the symptoms at all or experienced them less than 1 day, 23–24% experience them for 1–2 days, 8.37–8.82% had them for 3–4 days, and 4.3–4.77% had them for 5–7 days. Refer to Fig. 3 in the Appendix for the distributions of the four specific symptoms.
Covariates
We compile 11 covariates that are indexed at the individual and regional levels. The 3 major independent variables include income level, food insecurity, and virtual psychological support, which is represented by the probability of increased virtual communication frequency with friends and family. The income level, which reports 2019 annual pre-tax income from all sources (including wages, salaries, tips, business, interest, and so on), ranges from more than $125 k, $60 k to less than $125 k, $30 k to less than $60 k, to less than $30 k. Food insecurity evaluates if the two phrases “urban employees worried the food would run out before getting money to buy more” and “the food that urban employees bought just did not last, and they did not have money to get more” are often true or sometimes true.
The probability of increased virtual communication with friends and family is constructed following Hayes (1973), where the frequency of events is dependent on the number of intervals that are Poisson-distributed. Based on the two questions in the survey, “During a typical month prior to March 1, 2020, when COVID-19 began spreading in the United States, how often did you communicate with friends and family by phone, text, email, app, or using the Internet” and “In the past month, how often did you communicate with friends and family by phone, text, email, app, or using the Internet”, we naturally have two-time frames—the first is the one month prior to March and the second is the one month before the field interview. The frequency expected in the second period is based on the occurrences in the first period. This refers to the mean of the Poisson distribution for the events happening in the second time window, which is \(m\) in the below equation. According to the potential responses, we categorize “basically every day” as 30 times, “a few times a week” as 16 times, “a few times a month” as 4 times, “once a month” as 1 time, and “not at all” as 0 times. We use the standard Poisson formula
where \(f\left(x\right)\) is the expected frequency or probability of exactly \(x\) occurrences, \(e\) is the natural base of logarithms (2.71828…), \(m\) is the number of occurrences expected in the second time window, and \(x\) is the number of occurrences observed in the second time window. Instead of only calculating the exact probability of \(x\) occurrences for the second time window, we compute the probability that an individual communicated virtually with his or her friends and family at least \(x\) times based on the expected number of occurrences in the second time window and the actual number of occurrences observed in the second time window, which captures the change in willingness to virtually communicate. Fig. 4 in the Appendix illustrates the Poisson distributions with different means.
The other 8 control variables include general self-rated health (ranging from excellent, very good, good, fair, to poor), age categories (divided into 18–29, 30–44, 45–59, 60 +), gender, education (ranging from no high school diploma, high school graduate or equivalent, some college, to the bachelor of arts or above), marital status (whether single, including widowed, divorced, separated, and never married, or married), race (African American or not), insurance (whether covered by health insurance), and household size (including children).
Method
Our statistical analysis uses an ordinal regression model (ordered logit model) that implements both week and region fixed effects. This model appropriately captures the ordinal frequency of the four mental health condition measures, as reflected by the number of days those interviewees felt nervous, depressed, lonely, or hopeless during the outbreak of COVID-19. By adding both time and region factors, we can account for the potential time effects and time-invariant confounders that only vary between regions. Standard errors are clustered at the regional level. The estimating equation is specified as.
\(ln\left({\theta }_{j}\right)={\alpha }_{j}+\beta {E}_{iwr}+{\varvec{X}}{\varvec{C}}{\varvec{o}}{\varvec{n}}{\varvec{t}}{\varvec{r}}{\varvec{o}}{\varvec{l}}+{\mu }_{w}+{\delta }_{r}+{\epsilon }_{iwr}\),
where \({\theta }_{j}\) defines the odds of feeling nervous, depressed, lonely, or hopeless for fewer days than in category j for individual \(i\) in week \(w\) residing in region\(r\), \({\varvec{C}}{\varvec{o}}{\varvec{n}}{\varvec{t}}{\varvec{r}}{\varvec{o}}{\varvec{l}}\) is a vector of control variables, \({\mu }_{w}\) is the time fixed effects, \({\delta }_{r}\) is region fixed effects, and \({\epsilon }_{iwr}\) is the error term. \({E}_{iwr}\) is one of the three major independent variables,\(Foo{dInsecurity}_{iwr}\),\({IncomeLevel}_{iwr}\), and \({VirtualComm}_{iwr}\), measured by whether or not an individual has money to buy food, four levels of 2019 annual total pre-tax income, and the probability of increasing virtual communication with friends and family, respectively. To reduce the potential influence among the independent variables, for example, low-income families might be more likely to have food insecurity and lack of psychological support, we only test one major independent variable in each regression analysis.Footnote 1 In addition, due to data availability, only 2019 pre-tax income information is collected for both employed and unemployed individuals. To identify the difference in income caused by individuals becoming unemployed in 2020, we include an interaction term \({IncomeLevel}_{iwr}*{Laidoff}_{iwr}\) that nullifies the income of individuals who are still employed in 2020. The parallel lines assumption for the ordinal regression model assumes three different intercepts for each category, but a constant slope across categories.
Based on theory, material possessions encompass food insecurity and income level, while social capital encompasses income level, physical psychological support, and virtual psychological support. To further identify the “clean” impacts of income level, we take advantage of the quarantine and social distancing policies implemented primarily in urban areas, which basically cut off physical interactions with others, especially work-related and face-to-face psychological support. We divide the urban working-age population sample into two groups— the employed group and the unemployed group, which includes individuals who are laid off and furloughed. We do this to remove the effects of income for the unemployed group, so the effects of material possessions and social capital can be clearly distinguished.
Results
Table 1 outlines how material possessions and social capital are associated with the frequency of feeling nervous, depressed, lonely, and hopeless through waves 1, 2, and 3 with both week and regional fixed effects. The results are controlled for individual characteristics, including health status, age, gender, education, marital status, race, insurance, and household size.Footnote 2 Significant differences are identified between the employed and unemployed groups in columns (1), (3), and (4). The odds ratios show that feeling nervous, lonely, and hopeless may not be significantly associated with changes in income for employed individuals but could be positively correlated with income level if an individual is laid off. Columns (5)-(8) shows that food insecurity has a significant and strong association with mental health (Nervous: \(\beta =1.498\), 95% CI: 1.234, 1.820Footnote 3). In columns (9)-(12), the odds ratios on the probability of increasing virtual communication with family and friends are significant and less than one, indicating the beneficial correlation with mental health (Nervous: \(\beta =0.654\), 95% CI: 0.517, 0.827).
Since we are using the same independent variable to identify the association with the survived dependent variables, it might raise the issue of type-I error that rejects the null hypothesis with mistakes by applying the standard 0.05 significance level. For example, income level could directly make an unemployed individual feel nervous, and the symptom of feeling nervous could as well lead to feeling lonely or hopeless. To identify what symptoms are more significantly related to the independent variables when they are logically or statistically related in our analysis, we further our analysis by restricting the significance level to 0.01. The results are reported in Table 15. The dependent variables that are more significantly related to income level, food insecurity, and virtual communication are loneliness, nervousness and hopelessness, and depression, respectively. This indicates that for an unemployed individual, a reduced income level leads to feeling loneliness, which could also lead to nervousness or hopelessness. Food insecurity leads to feeling nervousness and hopelessness, which then could lead to experiencing depression or loneliness. The lack of virtual communication leads to feelings of depression, which then could make the person feel nervous, lonely, and hopeless.Footnote 4
Tables 2 and 3 exhibit the results after dividing the urban working-age population into employed and unemployed groups, which include individuals both being laid off and furloughed during COVID-19. Specifically, in columns (1)-(4) of Table 2, lower income levels could predict an increase in the frequency of feeling nervous and hopeless (Nervous: \(\beta =1.102\), 95% CI: 1.025, 1.184). In columns (5), (7), and (8), food insecurity is significantly associated with more days of feeling nervous, lonely, and hopeless (Nervous: \(\beta =1.455\), 95% CI: 1.199, 1.766). Columns (9)-(12) show that talking to family and friends over the phone has a significant negative correlation with the frequency of expressing mental health issues (Nervous: \(\beta =0.658\), 95% CI: 0.519, 0.836).
In Table 3, columns (1), (2), and (3) display the significant associations between food insecurity and deteriorated status of feeling nervous, depressed, and lonely. This pattern is similar to the pattern expressed by the employed group (Nervous: \(\beta =1.558\), 95% CI: 1.101, 2.204). Table 13 shows the Wald test on equality of coefficients for food insecurity between the employed and unemployed individuals, and we fail to reject the equality at the 10% level. On the other hand, being different from the employed individuals, the odds ratios reveal that virtual communication has no significant association with the mental health status of unemployed individuals, as presented in columns (5)-(8) (Nervous: \(\beta =0.704\), 95% CI: 0.485, 1.024). However, in Table 13, the Wald test cannot reject the difference in the magnitude of coefficients between the two groups at the 10% significance level except for the coefficient for virtual communication regressing on the odds of being lonely.
Robustness Analysis
Considering that the fixed-effects analysis examines the relationship between changes in both material possessions and social capital on mental health symptoms across survey waves, we assume that respondents who participated in the survey in all three waves lost their work-based social networks of psychological support due to quarantine policies. As a robustness check, we use the occupation information collected by the AmeriSpeak approach. Out of the 476 individuals who reported their job information, the essential workers who are most likely to continue to have face-to-face interactions at work are dropped. These include the community and social service occupations, healthcare support occupations, healthcare practitioners and technicians, sales and related occupations, food preparation and serving related occupations, and transportation and material moving occupations. Table 4 shows that the robustness analysis results are qualitatively similar to the main results: the direction and magnitude of the associations remain similar, whereas only some associations become statistically significant under the new sample.
In our main sample, about 78% of the individuals are employed and 22% are unemployed. This might lessen the comparability of the two groups in Tables 2 and 3 because a smaller unemployed sample size might mean greater variability around the mean and lower odds of achieving significance. To reduce the discrepancy between these two groups, we first apply propensity score matching with Mahalanobis distance using individual characteristics. Next, we randomly draw a sample size of 1,500 from the employed group to match the sample size of the unemployed group. Tables 5 and 6 report the robustness analysis results. Compared to the results in Tables 2 and 3, for the employed group, the robustness results show that food insecurity significantly aggravates nervous, depressed, and hopeless feelings, but not the lonely feeling, and contacting family and friends over the phone significantly helps improve symptoms of those negative feelings. For the unemployed group, similar to the results in Table 3, food insecurity significantly worsens the frequency of feeling nervous, depressed, and lonely. Virtual communication helps alleviate nervousness and depression but not lonely and hopeless, while in Table 3, the coefficients for virtual communication are insignificant for all symptoms.
Limitations
This paper uses data from the COVID-19 Household Impact Survey. However, the dataset does not collect information on individuals’ access to health care facilities or physicians, either physically or over the phone. This could be one limitation because the compromised access to health care services could be a potential stressor that affects individuals’ mental health status, especially during a pandemic. Secondly, there are limitations in the dataset when describing mental health conditions. The mental health status of the participants before COVID-19 is not described and other potential confounders such as personality traits that could influence both psychological support levels and feelings of loneliness are also not identified. The measurement of mental health status could also be subjective, for example, compared to the outcomes from validated depression or anxiety screeners, and single-item measures of mental health are not strong. Thirdly, the dataset only describes income levels in the pre-COVID time in 2019. Lastly, future studies could explore the mechanism behind material possessions and social capital that influence the population’s mental well-being. Although this study identifies the associations between mental health and food insecurity, income level, and virtual psychological support, more detailed data could help to find out the channels through which these variables work.
Discussion
The existing literature on this topic examines the simple correlation between a crisis and an individual’s mental health. This study contributes to the literature by examining the comparative associations between the working-age urban population’s mental well-being during the pandemic and income level, food insecurity, and virtual psychological support. These results could provide policymakers with novel perspectives on how to prioritize policy goals during a crisis. Our results show that food insecurity has a significant and strong correlation with mental health, which is consistent with previous findings that food supply worries contribute to worse mental well-being (Campbell, 1991; Kessler, 1997; Whitaker et al., 2006). The odds ratios on the virtual communication variable are significant and less than one, indicating the beneficial mental health effects of virtual contact. This finding confirms our theoretical assumption that communicating with friends and family provides psychological support (Almedom, 2005; Warr, 1994).
Furthermore, we compared the results across the three survey waves, April 20–26, May 4–10, and May 30-June 8 (see Table 16 in the Appendix). We found that food insecurity remains a significant determinant of mental health. Moreover, we found the benefits of virtual communication vary across the three windows. It significantly reduces the symptoms of feeling depressed and lonely during the first window when lockdown and quarantine policies substantially changed people’s lifestyles, alleviates nervousness and loneliness in the second window when people worry about the consequences of the pandemic and perhaps access to health care, and relieves depression in the third window when people were more used to being alone but generally frustrated about the longevity of the pandemic.
In addition, we as also found that people at a younger age or with a higher education level are more prone to mental health issues. This could be caused by the sudden lifestyle change by the Covid outbreak. On the one hand, children and university students are prone to Covid-related mental health issues (Elharake et al., 2022; Hawrilenko et al., 2021). Compared to the elderlies, youth is especially sensitive to lockdown and school closure (Viner et al., 2022). At the same time, the working population is also more easily affected by the deprivation of physical connection with work-related individuals and environments compared to the elderly. On the other hand, people with higher education levels are more likely to engage in office- or lab-related work environments, therefore they are more vulnerable to the sudden physical disconnection with work environments caused by quarantine policies compared to the population with lower education levels.
When we stratify the sample by the employed and unemployed population, the analyses exhibit quite different results. For the employed population, which is now deprived of physical psychological support, the results are qualitatively similar to those of the entire population. For income levels, explanations can be from both material possessions and social capital. From the perspective of material possessions, higher income ensures access to material supplies (Ettner, 1996) and access to care (Dickman et al., 2017). In regards to social capital, higher income alleviates feelings of insecurity (Wilkinson & Pickett, 2006) and could improve one’s self-perceived subjective social status (Bucciol et al., 2019). However, the compounding impact of income level is weaker than the impacts of food insecurity and virtual psychological support. Food insecurity can provoke feelings of anxiety and depression (Campbell, 1991; Kessler, 1997; Whitaker et al., 2006) about the ability to maintain food supplies or acquire sufficient food in the future. Even when the employed population earns their typical income level, they nevertheless worry about their access to food. On the other hand, virtual psychological support can significantly improve the employed population’s mental well-being because it is a form of social support and enabling environment for social participation (Almedom, 2005; Putnam, 1995), which together have protective effects on depressive symptoms (Nummela et al., 2008; Takagi et al., 2013).
For the unemployed population, the empirical results differ dramatically. Food insecurity remains the primary stressor, with the most significant effect on increased frequencies of feeling nervous, depressed, and lonely. However, the mitigating effect of virtual psychological support is compromised for the unemployed group feeling lonely and hopeless, although it remains helpful for alleviating nervous and depressed feelings. This is because of the protective effects of virtual psychological support on depressive symptoms, as suggested by existing theory and prior empirical results. But food insecurity is still the primary concern of this group. This has an important conceptual implication regarding the differentiation between the employed and unemployed groups. In Figs. 1a and b, a major difference in mental health stressors for the employed and unemployed groups is income level. Covid-19 removes income for the unemployed group, therefore, compared to the employed group whose material possession could be assured by a sustained income, food insecurity could translate into a more extreme condition of food insufficiency for the unemployed group due to being unable to afford food (Sorsdahl et al., 2011).
Food insufficiency refers to when household members do not have enough to eat and is comparable to “food insecurity with hunger” (Alaimo et al., 1998). Under extreme food insufficiency that could threaten survival, people could feel hopeless, and virtual psychological support as a form of social capital is unable to cause a meaningful change. Other recent studies have also suggested similar results that food insecurity, which may result from job loss, is associated with mental issues (Fang et al., 2021; McAuliffe et al., 2021). It is interesting to note, however, that for unemployed individuals, loneliness and hopelessness are not alleviated by virtual psychological support either in this case, which a lot of studies assume otherwise. In addition, food insecurity itself is not significantly correlated with hopelessness for the unemployed group, meaning that this group may feel hopeless not because of the present status of being unable to afford food, but rather the unpredictable future of staying unable to afford food. Therefore, instead of psychological support, material sustenance is still the primary concern of households without income sources during a crisis.Footnote 5
Conclusion
In conclusion, this paper uses current data collected during COVID-19 to explore the impacts of material possessions and social capital on the urban working-age population’s mental well-being. The specific stressors examined in the empirical analyses are income level, food insecurity, and virtual psychological support. The main findings align with those of the existing literature, while important novel findings are identified to complement the existing literature. First, food insecurity has an adverse association with mental health for the unemployed urban populations. Second, virtual psychological support, while significantly mitigating mental issues for the employed population, might only have a significant correlation with the nervous and depressed feelings in the unemployed population. In general, the unemployed group mainly worries about their access to food. Third, income level has a significantly moderate mitigating association with the employed population’s mental well-being, although this correlation disappears for the unemployed. These findings can help policymakers better understand how to prioritize the needs of the urban population during a crisis. While virtual psychological support should be prioritized in alleviating mental issues of the employed urban population, the material substance is the priority for the unemployed urban population. Policies targeting this population group could consider granting them various forms of material support, including but not limited to reoccurring small amount checks or food coupons that could assure them a forceable guaranteed survival.
Notes
Table 12 reports the results of mental health symptoms for the full sample by ignoring potential collinearity among major independent variables. The coefficients for income level and the interactive term income level * laid off are consistently smaller in magnitude than in Table 1, and the coefficients for food insecurity and virtual communication are consistently larger in magnitude than in Table 1. It indicates potential multicollinearity in the empirical analysis.
Only coefficients and confidence intervals on Nervous regressions are presented in the parentheses.
We thank the anonymous reviewer for pointing this out.
One of the coauthors of this study experienced the strict lockdown in Shanghai during Spring 2022 that shut every store including food supplies, and his anxiety that was caused by food insecurity due to nowhere to get food for the incoming days provides personal evidence for this argument.
References
Alaimo, K., Briefel, R. R., Frongillo, E. A., & Olson, C. M. (1998). Food Insufficiency Exists in the United States: Results from the Third National Health and Nutrition Examination Survey (NHANES III). American Journal of Public Health (1971), 88(3), 419–426. https://doi.org/10.2105/AJPH.88.3.419
Almedom, A. M. (2005). Social Capital and Mental Health: An Interdisciplinary Review of Primary Evidence. Social Science & Medicine, 61(5), 943–964. https://doi.org/10.1016/j.socscimed.2004.12.025
Atkinson, T., Liem, R., & Liem, J. (1987). The Social Costs of Unemployment: Implications for Social Support. Journal of Health and Social Behavior, 27(Dec 87), 317–331.
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. The Lancet, 395(10227), 912–920. https://doi.org/10.1016/S0140-6736(20)30460-8
Bucciol, A., Cicognani, S., & Zarri, L. (2019). Social Status Perception and Individual Social Capital: Evidence from the US. The B.E. Journal of Economic Analysis & Policy, 20(1), The B.E. Journal of Economic Analysis & Policy, 2019–2010–2001, Vol.2020 (2011). https://doi.org/10.1515/bejeap-2019-0071
Campbell, C. C. (1991). Food Insecurity: A Nutritional Outcome or a Predictor Variable?". The Journal of Nutrition, 121(3), 408–415. https://doi.org/10.1093/jn/121.3.408
Chrzastek, Z., Guligowska, A., Soltysik, B., Pigłowska, M., Borowiak, E., Kostka, J., & Kostka, T. (2021). Association of Lower Nutritional Status and Education Level with the Severity of Depression Symptoms in Older Adults-A Cross Sectional Survey. Nutrients, 13(2), 515. https://doi.org/10.3390/nu13020515
Creese, B., Khan, Z., Henley, W., O’Dwyer, S., Corbett, A., Vasconcelos Da Silva, M., Mills, K., Wright, N., Testad, I., Aarsland, D., & Ballard, C. (2021). Loneliness, physical activity, and mental health during COVID-19: A longitudinal analysis of depression and anxiety in adults over the age of 50 between 2015 and 2020. International Psychogeriatrics, 33(5), 505–514. https://doi.org/10.1017/S1041610220004135
Cygan-Rehm, K., Kuehnle, D., & Oberfichtner, M. (2017). Bounding the causal effect of unemployment on mental health: Nonparametric evidence from four countries. Health Economics, 26(12), 1844–1861. https://doi.org/10.1002/hec.3510
Dean, W. R., & Sharkey, J. R. (2011). Food insecurity, social capital and perceived personal disparity in a predominantly rural region of Texas: An individual-level analysis. Social Science & Medicine (1982), 72(9), 1454–1462. https://doi.org/10.1016/j.socscimed.2011.03.015
Dickman, S. L., Himmelstein, D. U., & Woolhandler, S. (2017). Inequality and the Health-care System in the USA. The Lancet (british Edition), 389(10077), 1431–1441. https://doi.org/10.1016/S0140-6736(17)30398-7
Elharake, J. A., Akbar, F., Malik, A. A., Gilliam, W., & Omer, S. B. (2022). Mental Health Impact of COVID-19 among Children and College Students: A Systematic Review. Child Psychiatry and Human Development. https://doi.org/10.1007/s10578-021-01297-1
Erdem, Ö., Lenthe, F., Prins, R., Voorham, T., & Burdorf, A. (2016). Socioeconomic Inequalities in Psychological Distress among Urban Adults: The Moderating Role of Neighborhood Social Cohesion. PLoS ONE, 11(6), e0157119–e0157119. https://doi.org/10.1371/journal.pone.0157119
Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2020a). Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Network Open, 3(9), e2019686–e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2021). Low assets and financial stressors associated with higher depression during COVID-19 in a nationally representative sample of US adults. Journal of Epidemiology and Community Health (1979), 75(6), 501–508. https://doi.org/10.1136/jech-2020-215213
Ettman, C. K., Cohen, G. H., & Galea, S. (2020b). Is Wealth Associated with Depressive Symptoms in the United States? Annals of Epidemiology, 43, 25-31.e21. https://doi.org/10.1016/j.annepidem.2020.02.001
Ettner, S. L. (1996). New Evidence on the Relationship between Income and Health. Journal of Health Economics, 15(1), 67–85. https://doi.org/10.1016/0167-6296(95)00032-1
Fan, H., & Nie, X. (2020). Impacts of Layoffs and Government Assistance on Mental Health during COVID-19: An Evidence-Based Study of the United States. Sustainability (basel, Switzerland), 12(18), 7763. https://doi.org/10.3390/su12187763
Fang, D., Thomsen, M. R., Nayga, J., & Rodolfo, M. (2021). The association between food insecurity and mental health during the COVID-19 pandemic. BMC Public Health, 21(1), 607–607. https://doi.org/10.1186/s12889-021-10631-0
FAO. (2020). Global food markets still brace for uncertainty in 2020/21 because of COVID-19 says FAO. Retrieved from http://www.fao.org/news/story/en/item/1287515/icode/
Fryers, T., Melzer, D., Jenkins, R., & Brugha, T. (2005). The distribution of the common mental disorders: Social inequalities in Europe. Clinical Practice and Epidemiology in Mental Health, 1(1), 14–14. https://doi.org/10.1186/1745-0179-1-14
German, D., & Latkin, C. A. (2011). Social Stability and Health: Exploring Multidimensional Social Disadvantage. Journal of Urban Health, 89(1), 19–35. https://doi.org/10.1007/s11524-011-9625-y
Glaeser, E. L., Laibson, D., & Sacerdote, B. (2002). An Economic Approach to Social Capital. The Economic Journal (london), 112(483), F437-458. https://doi.org/10.1111/1468-0297.00078
Golberstein, E. (2015). The Effects of Income on Mental Health: Evidence from the Social Security Notch. The Journal of Mental Health Policy and Economics, 18(1), 27–37.
Goldman-Mellor, S. J., Saxton, K. B., & Catalano, R. C. (2010). Economic Contraction and Mental Health: A Review of the Evidence, 1990–2009. International Journal of Mental Health, 39(2), 6–31. https://doi.org/10.2753/IMH0020-7411390201
Guo, Q., Bai, X., & Feng, N. (2018). Social participation and depressive symptoms among Chinese older adults: A study on rural–urban differences. Journal of Affective Disorders, 239, 124–130. https://doi.org/10.1016/j.jad.2018.06.036
Hawrilenko, M., Kroshus, E., Tandon, P., & Christakis, D. (2021). The Association Between School Closures and Child Mental Health During COVID-19. JAMA Network Open, 4(9), e2124092–e2124092. https://doi.org/10.1001/jamanetworkopen.2021.24092
Hayes, R. E. (1973). Identifying and Measuring Changes in the Frequency of Event Data. International Studies Quarterly, 17(4), 471–493. https://doi.org/10.2307/2600222
Iranpour, S., Sabour, S., Koohi, F., & Saadati, H. M. (2022). The trend and pattern of depression prevalence in the U.S.: Data from National Health and Nutrition Examination Survey (NHANES) 2005 to 2016. Journal of Affective Disorders, 298(Pt A), 508–515. https://doi.org/10.1016/j.jad.2021.11.027
Jahoda, M. (1982). Employment and Unemployment: A Social-psychological Analysis. Cambridge [Cambridgeshire] ; New York: Cambridge University Press.
Jones, A. D. (2017). Food Insecurity and Mental Health Status: A Global Analysis of 149 Countries. American Journal of Preventive Medicine, 53(2), 264–273. https://doi.org/10.1016/j.amepre.2017.04.008
Kawachi, I., Kennedy, B. P., & Glass, R. (1999). Social Capital and Self-rated Health: A Contextual Analysis. American Journal of Public Health (1971), 89(8), 1187–1193. https://doi.org/10.2105/AJPH.89.8.1187
Kawachi, I., Kennedy, B. P., Lochner, K., & Prothrow-Stith, D. (1997). Social capital, income inequality, and mortality. American Journal of Public Health (1971), 87(9), 1491–1498. https://doi.org/10.2105/AJPH.87.9.1491
Kessler, R. C. (1997). The Effects of Stressful Life Events on Depression. Annual Review of Psychology, 48(1), 191–214. https://doi.org/10.1146/annurev.psych.48.1.191
Koltai, J. (2018). Recession-related Stress, Mental Health, and the Buffering Role of Psychosocial Resources. European Journal of Public Health, 28(Suppl4), 124–124. https://doi.org/10.1093/eurpub/cky213.362
Li, L. W., Liu, J., Xu, H., & Zhang, Z. (2016). Understanding Rural-Urban Differences in Depressive Symptoms Among Older Adults in China. Journal of Aging and Health, 28(2), 341–362. https://doi.org/10.1177/0898264315591003
Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S., & Hahm, H. C. (2020). Factors Associated with Depression, Anxiety, and PTSD Symptomatology during the COVID-19 Pandemic: Clinical Implications for U.S Young Adult Mental Health. Psychiatry Research, 290, 113172–113172. https://doi.org/10.1016/j.psychres.2020.113172
Lorant, V., Deliège, D., Eaton, W., Robert, A., Philippot, P., & Ansseau, M. (2003). Socioeconomic Inequalities in Depression: A Meta-Analysis. American Journal of Epidemiology, 157(2), 98–112. https://doi.org/10.1093/aje/kwf182
Macleod, J., Davey Smith, G., Metcalfe, C., & Hart, C. (2007). Is Subjective Social Status a More Important Determinant of Health than Objective Social Status? Evidence from a Prospective Observational Study of Scottish Men. Social Science & Medicine (1982), 61(9), 1916–1929. https://doi.org/10.1016/j.socscimed.2005.04.009
Maynard, M., Andrade, L., Sara, P.-M., Christopher, P., Leos-Toro, C., & Kirkpatrick, S. (2018). Food Insecurity and Mental Health among Females in High-Income Countries. International Journal of Environmental Research and Public Health, 15(7), 1424. https://doi.org/10.3390/ijerph15071424
McAuliffe, C., Daly, Z., Black, J., Pumarino, J., Gadermann, A., Slemon, A., Thomson, K. C., Richardson, C., & Jenkins, E. K. (2021). Examining the associations between food worry and mental health during the early months of the COVID-19 pandemic in Canada. Canadian Journal of Public Health, 112(5), 843–852. https://doi.org/10.17269/s41997-021-00557-w
McGinty, E. E., Presskreischer, R., Han, H., & Barry, C. L. (2020). Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA : The Journal of the American Medical Association, 324(1), 93–94. https://doi.org/10.1001/jama.2020.9740
Moore, T. H. M., Kapur, N., Hawton, K., Richards, A., Metcalfe, C., & Gunnell, D. (2016). Interventions to reduce the impact of unemployment and economic hardship on mental health in the general population: A systematic review. Psychological Medicine, 47(06), 1062–1084. https://doi.org/10.1017/S0033291716002944
Norstrand, J. A., & Xu, Q. (2012). Social Capital and Health Outcomes Among Older Adults in China: The Urban-Rural Dimension. The Gerontologist, 52(3), 325–334. https://doi.org/10.1093/geront/gnr072
Nummela, O., Sulander, T., Rahkonen, O., Karisto, A., & Uutela, A. (2008). Social Participation, Trust and Self-rated Health: A Study among Ageing People in Urban, Semi-urban and Rural Settings. Health and Place, 14(2), 243–253. https://doi.org/10.1016/j.healthplace.2007.06.006
Oh, S., Salas-Wright, C. P., & Vaughn, M. G. (2018). Trends in depression among low-income mothers in the United States, 2005–2015. Journal of Affective Disorders, 235, 72–75. https://doi.org/10.1016/j.jad.2018.04.028
Pabayo, R., Dunn, E. C., Gilman, S. E., Kawachi, I., & Molnar, B. E. (2016). Income Inequality within Urban Settings and Depressive Symptoms among Adolescents. Journal of Epidemiology and Community Health, 70(10), 997–1003. https://doi.org/10.1136/jech-2015-206613
Pabayo, R., Kawachi, I., & Gilman, S. E. (2014). Income Inequality among American States and the Incidence of Major Depression. Journal of Epidemiology and Community Health, 68(2), 110–115. https://doi.org/10.1136/jech-2013-203093
Peyrot, W. J., Middeldorp, C. M., Jansen, R., Smit, J. H., de Geus, E. J. C., Hottenga, J.-J., Willemsen, G., Vink, J. M., Virding, S., Barragan, I., Ingelman-Sundberg, M., Sim, S. C., Boomsma, D. I., & Penninx, B. W. J. H. (2013). Strong Effects of Environmental Factors on Prevalence and Course of Major Depressive Disorder Are Not Moderated by 5-HTTLPR Polymorphisms in a Large Dutch Sample. Journal of Affective Disorders, 146(1), 91–99. https://doi.org/10.1016/j.jad.2012.08.044
Pfefferbaum, B., & North, C. S. (2020). Mental Health and the Covid-19 Pandemic. The New England Journal of Medicine, 383(6), 510–512. https://doi.org/10.1056/NEJMp2008017
Putnam, R. D., Leonardi, R., & Nanetti, R. Y. (1993). Making democracy work : civic traditions in modern Italy. Princeton, NJ: Princeton University Press.
Putnam, R. D. (1995). Bowling alone: America’s declining social capital. Journal of Democracy, 6, 65–78. https://doi.org/10.1353/jod.1995.0002
Rajkumar, R. P. (2020). COVID-19 and Mental Health: A Review of the Existing Literature. Asian Journal of Psychiatry, 52, 102066–102066. https://doi.org/10.1016/j.ajp.2020.102066
Rey, S. J. (2018). Bells in Space: The Spatial Dynamics of US Interpersonal and Interregional Income Inequality. International Regional Science Review, 41(2), 152–182. https://doi.org/10.1177/0160017615614899
Sakurai, K., Kawakami, N., Yamaoka, K., Ishikawa, H., & Hashimoto, H. (2010). The Impact of Subjective and Objective Social Status on Psychological Distress among Men and Women in Japan. Social Science & Medicine, 70(11), 1832–1839. https://doi.org/10.1016/j.socscimed.2010.01.019
Singh-Manoux, A., Adler, N. E., & Marmot, M. G. (2003). Subjective Social Status: Its Determinants and Its Association with Measures of Ill-health in the Whitehall II Study. Social Science & Medicine (1982), 56(6), 1321–2333. https://doi.org/10.1016/S0277-9536(02)00131-4
Singh-Manoux, A., Marmot, M. G., & Adler, N. E. (2005). Does Subjective Social Status Predict Health and Change in Health Status Better Than Objective Status? Psychosomatic Medicine, 67(6), 855–861. https://doi.org/10.1097/01.psy.0000188434.52941.a0
Sobel, J. (2002). Can We Trust Social Capital? Journal of Economic Literature, 40(1), 139–154. https://doi.org/10.1257/jel.40.1.139
Sorsdahl, K., Slopen, N., Siefert, K., Seedat, S., Stein, D. J., & Williams, D. R. (2011). Household Food Insufficiency and Mental Health in South Africa. Journal of Epidemiology and Community Health (1979), 65(5), 426–431. https://doi.org/10.1136/jech.2009.091462
Stansfeld, S. A., Head, J., Fuhrer, R., Wardle, J., & Cattell, V. (2003). Social Inequalities in Depressive Symptoms and Physical Functioning in the Whitehall II Study: Exploring a Common Cause Explanation. Journal of Epidemiology and Community Health, 57(5), 361–367. https://doi.org/10.1136/jech.57.5.361
Stunkard, A. J., Faith, M. S., & Allison, K. C. (2003). Depression and Obesity. Biological Psychiatry (1969), 54(3), 330–337. https://doi.org/10.1016/S0006-3223(03)00608-5
Suls, J., & Bunde, J. (2005). Anger, Anxiety, and Depression as Risk Factors for Cardiovascular Disease. Psychological Bulletin, 131(2), 260–300. https://doi.org/10.1037/0033-2909.131.2.260
Takagi, D., Kondo, K., & Kawachi, I. (2013). Social Participation and Mental Health: Moderating Effects of Gender, Social Role and Rurality. BMC Public Health, 13(1), 701–701. https://doi.org/10.1186/1471-2458-13-701
Tefft, N. (2011). Insights on Unemployment, Unemployment Insurance, and Mental Health. Journal of Health Economics, 30(2), 258–364. https://doi.org/10.1016/j.jhealeco.2011.01.006
Truyts, T. (2010). Social Status in Economic Theory. Journal of Economic Surveys, 24(1), 137–169. https://doi.org/10.1111/j.1467-6419.2009.00579.x
Uphoff, E. P., Pickett, K. E., Cabieses, B., Small, N., & Wright, J. (2013). A systematic review of the relationships between social capital and socioeconomic inequalities in health: A contribution to understanding the psychosocial pathway of health inequalities. International Journal for Equity in Health, 12(1), 54–54. https://doi.org/10.1186/1475-9276-12-54
Viner, R., Russell, S., Saulle, R., Croker, H., Stansfield, C., Packer, J., Nicholls, D., Goddings, A.-L., Bonell, C., Hudson, L., Hope, S., Ward, J., Schwalbe, N., Morgan, A., & Minozzi, S. (2022). School Closures During Social Lockdown and Mental Health, Health Behaviors, and Well-being Among Children and Adolescents During the First COVID-19 Wave: A Systematic Review. Archives of Pediatrics & Adolescent Medicine, 176(4), 400–409. https://doi.org/10.1001/jamapediatrics.2021.5840
Vogelsang, E. M. (2016). Older Adult Social Participation and Its Relationship with Health: Rural-urban Differences. Health and Place, 42, 111–119. https://doi.org/10.1016/j.healthplace.2016.09.010
Warr, P. (1994). A Conceptual Framework for the Study of Work and Mental Health. Work & Stress, 8(2), 84–97. https://doi.org/10.1080/02678379408259982
Weaver, L. J., & Hadley, C. (2009). Moving Beyond Hunger and Nutrition: A Systematic Review of the Evidence Linking Food Insecurity and Mental Health in Developing Countries. Ecology of Food and Nutrition, 48(4), 263–284. https://doi.org/10.1080/03670240903001167
Whitaker, R. C., Phillips, S. M., & Orzol, S. M. (2006). Food Insecurity and the Risks of Depression and Anxiety in Mothers and Behavior Problems in Their Preschool-Aged Children. Pediatrics (evanston), 118(3), e859-E868. https://doi.org/10.1542/peds.2006-0239
White, J., Zaninotto, P., Walters, K., Kivimäki, M., Demakakos, P., Shankar, A., Kumari, M., Gallacher, J., & Batty, G. D. (2015). Severity of depressive symptoms as a predictor of mortality: The English longitudinal study of ageing. Psychological Medicine, 45(13), 2771–2779. https://doi.org/10.1017/S0033291715000732
Wilkinson, R. G., & Pickett, K. E. (2006). Income Inequality and Population Health: A Review and Explanation of the Evidence. Social Science & Medicine (1982), 62(7), 1768–1784. https://doi.org/10.1016/j.socscimed.2005.08.036
Wolfson, J. A., & Leung, C. W. (2020). Food Insecurity During COVID-19: An Acute Crisis With Long-Term Health Implications. American Journal of Public Health (1971), 110(12), 1763–1765. https://doi.org/10.2105/AJPH.2020.305953
Wozniak, A., Willey, J., Benz, J.,, & Hart, N. COVID Impact Survey: Version 1 [dataset]. Chicago, IL: National Opinion Research Center, 2020.
Zimmerman, F. J., & Bell, J. F. (2006). Income Inequality and Physical and Mental Health: Testing Associations Consistent with Proposed Causal Pathways. Journal of Epidemiology and Community Health, 60(6), 513–521. https://doi.org/10.1136/jech.2005.040154
Zivin, K., Paczkowski, M., & Galea, S. (2011). Economic Downturns and Population Mental Health: Research Findings, Gaps Challenges and Priorities. Psychological Medicine, 41(7), 1343–1348. https://doi.org/10.1017/S003329171000173X
Acknowledgements
We give thanks to the editor in chief Daniel Shek and three anonymous reviewers; their comments have helped improve our study. The authors are grateful to the Data Foundation for funding the COVID Impact Survey and NORC at the University of Chicago for conducting the survey. The authors thank them for their generosity in sharing these data.
Funding
This study is supported by the Innovative Research Project Grant at the Shanghai Academy of Social Sciences. Both the first and corresponding authors had full access to the data used in the study and had final responsibility for the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
Haobin Fan: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Visualization; Writing—original draft; Xuanyi Nie: Conceptualization; Investigation; Methodology; Project administration; Visualization; Writing—original draft; Sarah Wilson: Writing—review & editing.
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Table
11 outlines the full table results of Table 1. This table reports the odds ratio coefficients for the 8 control variables, including general self-rated health (ranging from excellent, very good, good, fair, to poor), age categories (divided into 18–29, 30–44, 45–59, 60 +), gender, education (ranging from no high school diploma, high school graduate or equivalent, some college, to the bachelor of arts or above), marital status (whether single, including widowed, divorced, separated, and never married, or married), race (African American or not), insurance (whether covered by health insurance), and household size (including children).
African Americans show a lower frequency of having mental health issues than other races. As one’s self-rated health status deteriorates, her/his mental health declines as well. Older people are having less mental health symptoms than younger people, which might imply that as individual ages, it could be better to deal with mental health status during a crisis like the pandemic. Females are significantly reporting worse symptoms than males. More educated people might exhibit more days of feeling nervous, depressed, lonely, and hopeless, but this pattern is not significant for all regressions. The marital status of being single reports insignificant coefficients with mental health. Health insurance might help alleviate the feeling of nervousness, depression, and hopelessness during the pandemic. Household size is significantly and negatively associated with days of having mental health issues, which might suggest the importance of physical psychological support within a family.
Table
14 shows the full table results for the full sample, employed individuals, and unemployed individuals. This table reports the odds ratio coefficients for both the major independent variables and the 8 control variables. Similar to Tables 1, 2, and 3, the significant coefficient for the interactive term income level and laid off reveals the difference between employed and unemployed groups in column (1), and as income level decreases, the symptoms of having mental health issues are getting worse for the employed individuals in column (4). Food insecurity is consistently and significantly associated with the deteriorated status of mental well-being but talking to family and friends over the phone could ease those nervous, depressed, lonely, and hopeless feelings.
Table
15 reports the results of mental health symptoms for the full sample by restricting the significance level to 0.01 and below, and the p values for those coefficients are in the parentheses for easy comparison. The purpose of this estimation is to identify which symptoms are relatively significant. As shown in the table, if an individual is laid off, feeling lonely is still significantly associated with changes in income. Food insecurity reveals significant correlations with symptoms of nervousness and hopelessness. Virtual communication with family and friends exhibits a significant association with feeling depressed. As the results indicate, the symptoms that the three independent variables significantly predict are different. Besides the direct correlation between independent variables and mental health symptoms, another possible path is that the symptoms significantly affected by the independent variables could as well affect the other symptoms that are not significantly affected after restricting the p values.
In Table
16, we include all the four major independent variables in each regression for comparison across the three survey waves, April 20–26, May 4–10, and May 30-June 8. The results in general report a similar pattern as in Table 1. The odds ratios show that feeling symptoms may not be significantly correlated with changes in income across those three survey windows. Food insecurity exhibits a strong and significant association with mental health. As an individual or a family facing the issue of a shortage of food under the shock of COVID-19, his/her frequency of having symptoms rises. The odds ratios on the probability of increasing virtual communication with family and friends show different patterns across the three waves. During the first window when the early diagnosed cases emerged, talking to family and friends significantly reduce the symptoms of feeling depression and loneliness. In the second window, virtual communication is significantly associated with less frequency of nervousness and loneliness, but merely significantly benefits for relieving depression in the third window.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fan, H., Nie, X. & Wilson, S. Mental Health, Material Possessions, and Social Capital During COVID-19: A Study of the United States Urban Working-Age Population. Applied Research Quality Life 18, 561–599 (2023). https://doi.org/10.1007/s11482-022-10093-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-022-10093-5