Abstract
Important contributors to quality of life (QOL), such as psychosocial factors, have received limited exploration in veteran populations, in contrast to a significant amount of research focused on health-related quality of life (HRQL). This study investigated QOL and HRQL amongst Gulf War veterans compared with an era-military comparison group 20 years after the 1990/91 Gulf War, and whether psychiatric status over time and psychiatric comorbidities predicted QOL and HRQL. We then investigated which of a range of psychological health, physical health and social factors contribute greatest to QOL. Psychological interviews and postal questionnaires were administered to a cohort of Gulf War veterans and a military-era comparison group in 2000–02 and 2011–12. Gulf War veterans had poorer QOL and HRQL compared with a military comparison group, but the pattern of factors that influenced QOL was the same for both groups. Poorer QOL and HRQL were significantly associated with more recent and persistent psychiatric morbidity over time. Further analyses showed that affective disorders, followed by anxiety disorders had the largest impact on QOL and HRQL, and that QOL and HRQL were negatively affected by each additional psychiatric diagnosis. The importance of these findings was highlighted in a structural equation model that revealed psychological health contributed most to QOL, social support contributed a moderate amount, but physical health contributed only a very small amount. QOL in veterans is an important issue even many years after deployment and psychological health plays a predominant role in QOL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Veterans have been shown to have significant physical and psychiatric morbidity post-deployment and, within this context, increasing number of deployments, medical conditions, and poorer psychological health have been associated with poorer health-related quality of life (HRQL) (Voelker et al. 2002). However, psychosocial factors in veterans have not been thoroughly examined on general Quality of Life (QOL).
Most tools for assessing QOL in military and veteran populations measure HRQL (e.g. Short-Form Health Survey 12 (SF-12)) (Voelker et al. 2002; Proctor et al. 2001). These assess health status with an emphasis on functionality, as distinct from QOL measures which assess a person’s individual evaluation of their life and subjective wellbeing (Guyatt 1997). Health status and associated functioning can be vastly different from QOL; the World Health Organization’s Quality of Life (WHOQOL) definition of QOL assumes it is at least partly independent of health status (Muldoon et al. 1998; The WHOQOL Group 1998). QOL includes both health related factors and factors such as employment, relationships, life circumstances and individual perspectives and values (Gill and Feinstein 1994). A review and meta-analysis of QOL and HRQL instruments supported the conclusion that the two are distinct constructs (Smith et al. 1999). Whilst QOL measures have been used extensively in health, epidemiology and psychological research, they have been used infrequently in veteran health studies.
In a cross-sectional study, U.S. Gulf War veterans were found to display poorer mental health, and poorer QOL and HRQL compared with a non-deployed comparison group ten years after the war (Toomey et al. 2007). Similarly, Australian Gulf War veterans displayed poorer HRQL than an era-military comparison group ten years after the war (McKenzie et al. 2004). Further studies have shown deployment to the Gulf War theatre to be a significant contributor to poorer HRQL, in addition to contributions from physical health, sociodemographic and psychological factors (Voelker et al. 2002).
When evaluating QOL, individuals may place greater emphasis on mental health compared to physical or social function (Smith et al. 1999). Psychological health affects both HRQL and QOL in a range of populations, including veterans (Toomey et al. 2007; Foster et al. 1999; Surìs et al. 2007; Mendlowicz and Stein 2000; Voelker et al. 2002), and whilst any psychiatric morbidity appears to affect QOL judgements, research into particular diagnoses reveals that, in civilian populations, posttraumatic stress disorder (PTSD) and depression in particular, have the greatest effect on QOL (Surìs et al. 2007; Cubo et al. 2002). Not only does psychiatric morbidity play an important role in QOL, but it has also been found that as the number of psychiatric comorbidities increase QOL decreases (Cubo et al. 2002) and, in veterans, HRQL decreases (Forman-Hoffman et al. 2005). Studies in veterans have assessed the influence of psychological health on HRQL at varying time points, but we have not identified previous veteran health research that has investigated how psychological health over time impacts QOL.
This paper aims to extend the current knowledge of QOL in veterans by utilising a QOL instrument to broaden the literature on HRQL and employing longitudinal psychiatric health data in a veteran population. We aim to investigate whether QOL is poorer amongst Gulf War veterans than a military comparison group 20 years after the 1990/91 Gulf War. We also aim to identify which of a range of psychological health, physical health and social factors contribute most to QOL through the following research questions:
Does psychiatric health status over time predict QOL and/or HRQL in veterans? Which psychiatric disorders and associated comorbidities have the greatest impact on QOL and/or HRQL?
Which of the following factors; psychological health, physical health, and social support, are the greatest contributors to QOL?
Methods
Study Population
The Australian Gulf War Veterans’ Health Study (2000–2002) involved 1456 Gulf War veterans (80.5% of eligible cohort) and 1588 (56.8%) of an era-military comparison group (Ikin et al. 2004). A follow-up study undertaken in 2011–12 invited all baseline study participants to take part by completing a postal questionnaire and telephone psychological interview. The study was approved by the relevant Ethics Committees in Australia; all participants provided voluntary informed consent.
Instruments
QOL was assessed with the World Health Organization Quality of Life questionnaire (WHOQOL-Bref) and the Life Satisfaction Sale, while HRQL was assessed with the 12-item Short Form Health Survey (SF-12).
The WHOQOL-Bref (The WHOQOL Group 1998) is a self-report inventory containing 26-items; two items provide a measurement of overall QOL and Health Satisfaction. The remaining 24-items produce four domains; physical health, psychological heath, social relationships and environment. Sample questions include, “To what extent do you feel your life to be meaningful?”, “How satisfied are you with your ability to perform daily activities?”, and “How satisfied are you with your personal relationships?” The scale has demonstrated good internal consistency with Cronbach’s alpha ranging from 0.80–0.88 per domain. It is rated on a five point Likert scale. The two general questions have a range of 1–5. The four domains were transformed to have final scores with a range of 0–100, higher scores indicate better QOL.
The Life Satisfaction scale assesses general satisfaction with life (F. Andrews and Withey 1976). The scale’s single question ("How do you feel about your life as a whole, taking into account what has happened in the last year and what you expect to happen in the future?”) has seven possible responses with the total score ranging from 1 to 7. The raw scores were reverse-scored to align with the direction of the WHOQOL-Bref, so that higher scores represented increased life satisfaction.
The SF-12 is scored to produce a Physical Component Summary score (PCS) and a Mental Component Summary score (MCS) with lower scores representing poorer physical functioning or psychological wellbeing (Ware Jr et al. 1996).
The CIDI v2.1 is a structured interview that evaluates participants for psychiatric disorders according to Diagnostic and Statistical Manual (DSM-IV) diagnostic criteria (World Health Organisation 1997), with good reliability and validity (Wittchen 1994). At baseline the CIDI was administered face-to-face by psychologists (Ikin et al. 2004). At follow up the CIDI was administered over-the-phone by trained interviewers. Current diagnoses were defined as any affective (including major depression), any anxiety (including PTSD) or any alcohol disorder present within the previous 12 months. For current analyses; CIDI-defined psychiatric conditions were defined as follows:
-
Persistent: Current at baseline and current at follow-up.
-
Incident: Not current at baseline and current at follow-up.
-
Remitted: Current at baseline and not current at follow-up.
-
Diagnoses Absent: Not current at baseline and not current at follow-up.
These labels were adopted for brevity in summarising outcomes. Persistence, in this instance, only indicates that the disorder was present at baseline and follow up; it does not indicate whether participants’ symptoms persisted continuously in the decade between baseline and follow-up. Similarly, Incident, Remitted and Diagnoses Absent do not capture symptom changes in the ten years between baseline and follow-up. Psychiatric comorbidity was defined as having more than one current psychiatric condition in different diagnostic categories.
The 9-item Patient Health Questionnaire (PHQ-9) (Kroenke et al. 2001) is a depression severity measure comprising nine questions based on the DSM-IV criteria for major depression. Total scores range from 0 to 27. The instrument is a reliable and valid measure of depression severity with excellent internal consistency, a Cronbach’s alpha of 0.92.
The Posttraumatic Stress Disorder Checklist – Civilian version (PCL-C) (Weathers et al. 1993) is a 17-item self-report instrument; items reflect DSM-IV PTSD symptom criteria. The PCL–C yields a total score between 17 and 85. Internal consistency of the PCL-C total scale score was .96.
Social support was defined in two ways. Structural support was assessed by asking participants the number of close friends and relatives they have. Additionally, they were asked how many voluntary or ex-service groups they belong to and how active they were in these groups. Functional support was measured using the Medical Outcomes Study Social Support Survey (MOS) (Sherbourne and Stewart 1991). This survey contains 19-items that assessed the support available if the individual should require assistance. Subscale scores (Tangible support, Affective support, Emotional/Informational Support, and Positive Social Interaction) were calculated by averaging the scores for each item in the subscale. The subscales demonstrated excellent internal consistency with Cronbach’s alphas ranging from 0.90–0.95.
The physical health construct was measured via several outcomes. A 63-item self-report symptom questionnaire assessed the presence of symptoms in the past month; symptoms rated as ‘moderate’ or ‘severe’ were included. Participants were asked about self-reported doctor-diagnosed medical conditions including arthritis (other than rheumatoid) and musculoskeletal conditions (other than arthritis), respiratory health, eye or vision problems, hearing loss, diabetes, and high blood pressure, and whether they had been treated in the past 12-months. Smoking status was categorised as current, former or never smoked. Pain was measured using the Chronic Pain Grade questionnaire (Von Korff et al. 1992), a 7-item questionnaire that measures severity of chronic pain. Results were classified into five grades: grade 0 (pain free), grade I (low disability, low intensity), grade II (low disability, high intensity), grade III (high disability, moderately limiting), and grade IV (high disability, severely limiting) (Von Korff et al. 1992). Level of physical activity (moderate or vigorous exercise in the past two weeks) was self-reported. Body Mass Index (BMI) (kg/m2) was used to indicate overweight and obesity. Cancer data was collected via linkage with the Australian Cancer Database.
Statistical Analyses
Statistical analyses were performed using SPSS version 20 and AMOS version 20.
Skewed outcome data were transformed using reflected square-root and reflected log10 transformations. Sociodemographic differences between the two groups were tested with independent t-tests for continuous variables (age) and chi-square for categorical variables (marital status, education level and total household income category). Differences between the Gulf War veterans’ and comparison group members’ mean scores on overall QOL, Health Satisfaction and the four WHOQOL-Bref domains, as well as life satisfaction, were tested using independent t-tests. The magnitude of the effect size was calculated using Cohen’s d (Cohen 1988). One-way ANOVAs were used to assess differences in QOL and HRQL between psychiatric status and psychiatric comorbidities; and post-hoc Tukey tests were conducted to determine which group means were significantly different. Further to these analyses, ANCOVAS were used to test for an interaction effect between study group and psychiatric status on QOL and HRQL. Regression analysis was used to investigate which psychiatric disorders explained the most variance in QOL and HRQL.
Structural Equation Modelling (SEM) was used to examine the contributions of psychological health, physical health and social support to QOL. SEM links observed variables with latent constructs as well as a structural model characterising the relationships among the latent constructs. The relationships in the model are based on theoretical predictions. The model was assessed via; (a) path coefficients assessed by their corresponding critical ratios for direct effects, and (b) fit indices corresponding to the overall model. Commonly reported fit indexes were used to interpret the overall fit of the SEM model; the Comparative Fit Index (CFI), the Tucker-Lewis Index (TLI), and Root Mean Square Error of Approximation (RMSEA) (Hu and Bentler 1999).
Results
Study Groups
Of eligible Gulf War veterans, 715 (53.8%) participated, of whom 712 completed a postal questionnaire, and 675 (46.6%) comparison group members, of whom 674 completed a questionnaire. Of these, 660 veterans and 621 comparison group also completed a telephone CIDI interview. The current analysis was restricted to male participants (due to very small number of female participants, n = 30) who completed the postal questionnaire or CIDI interview: 697 Gulf War veterans and 659 comparison group, total = 1356.
Participation Bias
Gulf War veterans who participated at follow-up were slightly older and more likely to have been Officers in 1991 and had a slightly lower SF-12 MCS score compared to those who did not participate. There were no significant differences between participating and non-participating veterans in regards to service branch, still serving in the Australian Defence Force (ADF) at the time of the baseline study, their SF-12 Physical Component Summary score or CIDI diagnoses for PTSD, major depression or alcohol dependence in the 12 months prior to the baseline study.
Participating comparison group members were slightly older, more likely to have been in the Air Force and more likely to have been Officers in 1991 relative to comparison group members who did not participate. There were no significant differences across whether they were serving in the ADF at baseline, SF-12 PCS or MCS scores, or any CIDI diagnoses.
A similar pattern of non-participation amongst young and lower-ranked members was observed in both study groups. Furthermore, the small difference in SF-12 MCS for Gulf War veterans is unlikely to have a substantial impact on the results presented.
Participant Characteristics
Gulf War veterans were marginally younger (mean age 49.4 years (SD = 6.6) vs 50.9 years (SD = 6.2; p < 0.001) than the comparison group). The two groups were similar in regard to marital status, education level and total household income. More than 80% of participants were married/de facto, approximately 50% had a trade certificate or diploma as their highest level of education, and approximately 50% reported a total household income of $100,000–199,000. Gulf War veterans were more likely to have served in the Navy and less likely to have served in the Army or Air Force than the comparison group. A small proportion of all participants (17.5%) were still serving in the ADF at follow-up.
Differences in Overall QOL and QOL Domains in Gulf War Veterans and Comparison Group at Follow Up
Table 1 shows that, more than 20 years after the Gulf War, Gulf War veterans reported significantly lower QOL and HRQL on all measures than the comparison group. These differences remained statistically significant when the mean differences were adjusted for deployment. The effect size calculation (Cohen’s d) showed that the greatest differences between the groups were observed for SF-12 MCS, Overall QOL, Health Satisfaction and Psychological QOL; however these differences were categorised as small effect sizes (Cohen 1988). For subsequent analyses, the QOL variables of interest were restricted to those that provided subjective evaluations into important QOL areas and also allowed for a comparison between these and HRQL. Thus, Overall QOL, the SF-12 MCS and Psychological QOL were considered.
Psychiatric Status Over Time
The majority of Gulf War veterans (67.7%) and comparison group (76.4%) did not meet CIDI criteria for any psychiatric diagnosis at baseline or follow-up. In relation to any CIDI diagnosis in Gulf War veterans and comparison group respectively, 7.4% vs 6.5% had a Remitted diagnosis, 14.6% vs 11.4% had an Incident diagnosis, and 10.4% vs 5.8% had Persistent psychiatric diagnoses at baseline and follow-up. Multinomial logistic regression revealed that veterans were more likely than the comparison group to have Persistent or Incident diagnoses compared with Diagnoses absent.
Psychiatric Status Over Time and Overall QOL (WHOQOL-Bref)
There was a significant effect of psychiatric status over time, on Overall QOL. Table 2 shows the means and standard deviations of Overall QOL for psychiatric status over time. A post-hoc analysis using Tukey’s test indicated that the mean score for the ‘Diagnoses Absent group was significantly different from the Persistent, Remitted and Incident groups. The Remitted group were significantly different from the Incident and the Persistent group. The Incident group was not significantly different from the Persistent group. The pattern of deterioration in QOL in relation to recency and persistence of diagnosis indicates that if the person has had a psychiatric diagnosis at both time points and if the diagnosis is current, Overall QOL is poorer.
The second analysis examined if there was an interaction between study group (Gulf War veteran vs. comparison group) and psychiatric health over time on Overall QOL. An ANCOVA did not indicate an interaction effect (p > 0.05).
Psychiatric Status Over Time and SF-12 MCS (HRQL)
There was also a significant effect of longitudinal psychiatric status on the SF-12 Mental Component for all study participants. Post- hoc Tukey test results indicated that the mean SF-12 MCS score for the Diagnoses Absent group was significantly different from Persistent, Remitted and Incident. The Remitted group were significantly different from the Persistent and Incident. The Incident group were significantly different from the Remitted but not the Persistent group. There was a similar pattern for both Gulf War veterans and comparison group members, and the ANCOVA indicated that there was no significant interaction (p > .05) of study group on the association.
Psychiatric Status Over Time and Psychological Domain of WHOQOL-Bref
Psychiatric status over time had a significant effect on the Psychological domain of QOL for all study participants. The post-hoc Tukey test indicated that the mean score for the Diagnoses Absent group was significantly different from Persistent, Remitted and Incident. The Remitted group were significantly different from the Incident and Persistent groups. The Incident group was significantly different from the Persistent group and Remitted group. The ANCOVA did not support an interaction effect between study group and psychological health over time on the psychological domain of QOL (p > .05).
Psychiatric Disorders with the Greatest Impact on Overall QOL and SF-12 MCS
A stepwise regression analysis revealed that affective disorders, followed by anxiety disorders accounted for the largest variance in both Overall QOL and the SF-12 MCS (Table 3), but Alcohol disorders did not explain sufficient variance to be included in the regression model. A greater proportion of variance was explained for the SF-12 MCS than Overall QOL. There remained a large variance that was unexplained, which was further investigated via SEM.
Further investigation of the effect of individual psychiatric disorders (major depression, PTSD, and alcohol abuse/dependence) found a significant relationship with Overall QOL, F(3,1250) = 75.802, p < 0.001, with an R2 of 0.15. Reflecting the results of psychiatric categories, major depression explained the largest variance in Overall QOL (β = −.24, p < 0.001), followed by PTSD (β = −.21, p < 0.001) and alcohol abuse/dependence. (β = −.12, p < 0.001). A significant relationship was also found with the SF-12 MCS, F(3,1210) = 128.993, p < 0.001, with an R2 of 0.24. The same pattern was observed with major depression explaining the largest variance in the SF-12 MCS (β = −.33, p < 0.001), followed by PTSD (β = −.25, p < 0.001) and alcohol abuse/dependence. (β = −.13, p < 0.001).
Number of Psychiatric Comorbidities and Overall QOL, SF-12 MCS and Psychological QOL
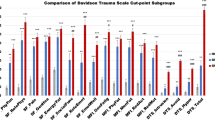
There were 947 (69.8%) participants with no current psychiatric diagnoses, 157 (11.6%) with one diagnosis, 73 (5.4%) with two diagnoses and 15 (1.1%) with three diagnoses; 12.1% of current diagnosis data was missing. A one-way ANOVA indicated that for all study participants there was a significant and increasing effect for number of psychiatric disorders at follow-up on Overall QOL (F(3816) = 63.48, p < .001), SF-12 MCS (F(3788) = 126.38, p < .001), and Psychological QOL (F(3811) = 123.78, p < .001), see Fig. 1. Post-hoc comparison using Tukey tests indicated that for Psychological QOL all comorbidity groups were significantly different from each other, at p < .05. For Overall QOL and SF-12 MCS, all differences between number of comorbidities were statistically significant, except between two or three psychiatric comorbidities.
Psychological Health, Physical Health and Social Support in Predicting QOL
All physical health variables were initially included in the SEM. Eye or vision problems, hearing loss, diabetes, high blood pressure, physical activity, obesity, respiratory health and cancer were removed to improve the fit of the measurement model; and self-reported symptoms (moderate or severe), smoking, pain, and self-reported doctor-diagnosed and treated in past 12 months arthritis (other than rheumatoid) and musculoskeletal conditions (other than arthritis) remained in the final model.
Standardised regression coefficients for the final SEM analysis are depicted graphically in Fig. 2. The model demonstrated good fit (CFI = 0.94, TLI = 0.92, RMSEA = 0.06). For the purposes of the SEM analysis, QOL was the focus of the investigation rather than HRQL. The overall pattern of results showed that psychological health was the biggest contributor to QOL, with social support also a moderately strong contributor to QOL, while physical health contributed a negligible amount. The latent variables for psychological health and physical health were strongly correlated, while social support was moderately correlated with psychological health and physical health.
Discussion
Gulf War veterans had significantly poorer QOL and HRQL across all domains compared with an era-military comparison group, although the differences were small. QOL, for both Gulf War veterans and the comparison group, was significantly affected by psychiatric health status over time; and the effect of recency and persistence of psychiatric diagnoses on QOL and HRQL was significant and similar in both study groups. Affective disorders, followed by anxiety disorders were the psychiatric disorders which had the largest impact on both QOL and HRQL; furthermore, both were further negatively affected by each additional comorbid psychiatric diagnosis. The importance of these findings is highlighted in the modelling of commonly reported factors, which revealed psychological health to be the biggest contributor to QOL, with social support contributing a moderate amount, and physical health very little.
Australian Gulf War veterans reported poorer HRQL ten years after the war (McKenzie et al. 2004); and now twenty years after the war they have reported poorer QOL and HRQL on all measures compared with the military-era comparison group, although these differences were considered small (Cohen 1988). This extends the current understanding of health in Gulf War veterans by demonstrating that not only their HRQL but also their QOL was impaired twenty years after the Gulf War. When compared to Australian population norms, Australian Gulf War veterans were consistently lower by a small amount over the four domains of the WHOQOL-Bref, whilst the comparison group was approximately similar (Hawthorne et al. 2006). This would indicate that even though twenty years have passed since the Gulf War, there are still significant issues which affect this group of veterans and consequently impact their HRQL and QOL.
Psychiatric status over time significantly affected Overall QOL, SF-12 MCS and Psychological QOL, and this was true for Gulf War veterans and the comparison group. The general pattern across these analyses indicated that the recency of diagnosis (past 12 months vs. 10 years ago) in conjunction with accumulative time experienced with the diagnosis (one time point vs. two time points) combined to affect QOL and HRQL alike. Psychiatric morbidity at any time point, even ten years in the past, affected current QOL, but the persistence and recency of morbidity appear to have affected QOL in a predictable pattern (Pirkola et al. 2009). This result emphasises the importance of treating psychological and psychiatric problems early, especially as it has been well documented that a significant delay exists between appearance of first symptoms and treatment-seeking (Chan et al. 2014; Wang et al. 2005). Veteran populations, in particular, may be resistant to acknowledging and seeking assistance for psychological distress; however, early detection and treatment are important to reduce future impairment.
Thus, with it clear that psychological health plays an important role in individual veterans’ assessments of their QOL; the next important question considered was which psychiatric diagnoses produced the most burden. Our findings showed that from the three categories of psychiatric disorders included; affective disorders, followed by anxiety disorders were the biggest contributors to poorer QOL and HRQL. Similarly, in investigating individual psychiatric disorders, major depressive disorder, followed by PTSD and alcohol abuse/dependence, were found to account for poorer QOL and HRQL. Individuals may use their mood or current state to draw upon as evidence or to inform their judgments regarding their QOL; which may be more likely to occur with affective and anxiety disorders compared to alcohol use disorders (Slade et al. 2009; Schwarz and Clore 1983). This explanation is consistent with our finding that Persistent and Incident groups, which have current diagnoses, had the lowest QOL and HRQL scores and these groups were not significantly different for Overall QOL and SF-12 MCS, suggesting that perhaps a current psychiatric diagnosis has a particularly important influence on QOL and HRQL evaluations. Indeed, research has found that depression mediates the relationship between military service and life satisfaction (Britton et al. 2012). Furthermore, research on the relationship between alcohol dependence and QOL has indicated mixed results (Volk et al. 1997; Duffy et al. 2002). A review by Foster et al., indicated that psychiatric comorbidity is an important contributor to the relationship between alcohol use and QOL (Foster et al. 1999; Singh et al. 2005); it may be that the influence of alcohol use is mediated through its comorbidities. This may also have contributed to affective and anxiety disorders being the predominant contributors to QOL.
While research has shown that psychiatric comorbidities affect HRQL in veterans (Forman-Hoffman et al. 2005; Der-Martirosian et al. 2013), our study has now shown that QOL domains were similarly affected and that current patterns of comorbidity also affected QOL and HRQL. It is important to know in respect to diagnosing and treating veterans that affective and anxiety disorders need to be recognised and treated early, and that comorbidity plays a compounding role. Treatment services need to offer effective treatments for the combination of these disorders (Andrews et al. 2002). Efforts to improve diagnosis and aggressively treat coexisting mental disorders may lead to enhanced QOL and HRQL in veteran populations.
The importance of psychological health was finally reinforced by the SEM analysis which identified psychological health as the biggest contributor to QOL, with social support and physical health contributing less. The correlations between physical health, psychological health and social support were all moderate to high, indicating that these constructs vary to some extent together. However, their associations with QOL reveal that some were stronger factors than others. For example, although psychological and physical health were quite strongly correlated in this study, psychological health had a much stronger association with QOL compared with physical health. Even though comorbidity between physical and psychological health is common in both the general population (Teesson et al. 2009; Sareen et al. 2007) and in veterans (Wolfe et al. 1999; Engel Jr et al. 2000), psychological health may be a more important factor for QOL than physical health. This is consistent with other research that has also found that in terms of evaluations of QOL or HRQL, psychological issues are stronger predictors than physical health (Pirkola et al. 2009).
These results demonstrate that in a veteran population, psychological health and social support are two important factors that contribute to QOL. QOL may therefore be a useful outcome for evaluating the impact of psychological and social health and monitoring the impact of interventions to improve these in veteran populations. The associations between both physical and psychological health with social support have been reported previously (Holahan and Moos 1981; Golden et al. 2009; Gallant 2003); and in addition to these, our results show that having a supportive social network or being involved in community activities may be important for QOL, this finding is consistent with results from other populations (Bennett et al. 2001).
The strengths of this study include the use of several measures spanning a range of domains of both QOL and HRQL. The use of longitudinal data has allowed an evaluation of the role of psychiatric health over time, which has not been thoroughly assessed in the QOL literature. However, whilst the longitudinal data provides insight into the importance of recency and persistence of psychiatric diagnosis, it is possible that during the ten year interval, there were intermittent symptoms that were not captured by the current data. Furthermore, for those with a current psychiatric diagnosis, perceptions caused by psychiatric morbidity (such as those associated with depression) may interact with subjective wellbeing evaluations. However, the use of longitudinal data provides insight into the role of recency of psychiatric diagnoses in QOL and HRQL. However, due to the use of cross-sectional data in the modelling analysis, the direction of associations cannot be determined. As the sample analysed in this paper were male veterans, it is not known if these findings are generalizable to female veterans.
Overall, the results indicated that psychological health should be considered a major factor in determining QOL and although Gulf War veterans reported poorer QOL and HRQL, the patterns do not vary across study group. Both QOL and HRQL are important outcomes for veterans that need to be recognised even decades after deployment. The current study has highlighted not only the relevance of the previously under-investigated QOL in veterans, but also the crucial role of psychological health in contributing to QOL.
References
Andrews, F., & Withey, S. (1976). Social indicators of well-being: Americans' perceptions of life quality. New York: Plenum.
Andrews, G., Slade, T., & Issakidis, C. (2002). Deconstructing current comorbidity: data from the Australian national survey of mental health and well-being. The British Journal of Psychiatry, 181(4), 306–314.
Bennett, S., Perkins, S., Lane, K., Deer, M., Brater, D., & Murray, M. (2001). Social support and health-related quality of life in chronic heart failure patients. Quality of Life Research, 10(8), 671–682.
Britton, P. C., Ouimette, P. C., & Bossarte, R. M. (2012). The effect of depression on the association between military service and life satisfaction. Quality of Life Research, 21(10), 1857–1862.
Chan, Y.-F., Huang, H., Bradley, K., & Unützer, J. (2014). Referral for substance abuse treatment and depression improvement among patients with co-occurring disorders seeking behavioral health services in primary care. Journal of Substance Abuse Treatment, 46, 106–112. https://doi.org/10.1016/j.jsat.2013.08.016.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale: Erlbaum.
Cubo, E., Rojo, A., Ramos, S., Quintana, S., Gonzalez, M., Kompoliti, K., et al. (2002). The importance of educational and psychological factors in Parkinson's disease quality of life. European Journal of Neurology, 9(6), 589–593.
Der-Martirosian, C., Cordasco, K. M., & Washington, D. L. (2013). Health-related quality of life and comorbidity among older women veterans in the United States. Quality of Life Research, 22(10), 2749–2756.
Duffy, S. A., Terrell, J. E., Valenstein, M., Ronis, D. L., Copeland, L. A., & Connors, M. (2002). Effect of smoking, alcohol, and depression on the quality of life of head and neck cancer patients. General Hospital Psychiatry, 24(3), 140–147.
Engel Jr., C. C., Liu, X., McCarthy, B. D., Miller, R. F., & Ursano, R. (2000). Relationship of physical symptoms to posttraumatic stress disorder among veterans seeking care for Gulf War-related health concerns. Psychosomatic Medicine, 62(6), 739–745.
Forman-Hoffman, V. L., Carney, C. P., Sampson, T. R., Peloso, P. M., Woolson, R. F., Black, D. W., et al. (2005). Mental health comorbidity patterns and impact on quality of life among veterans serving during the first Gulf War. Quality of Life Research: an International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 14(10), 2303–2314.
Foster, J., Powell, J., Marshall, E., & Peters, T. (1999). Quality of life in alcohol-dependent subjects – a review. Quality of Life Research, 8(3), 255–261.
Gallant, M. P. (2003). The influence of social support on chronic illness self-management: a review and directions for research. Health Education & Behavior, 30(2), 170–195.
Gill, T. M., & Feinstein, A. R. (1994). A critical appraisal of the quality of quality-of-life measurements. JAMA: the Journal of the American Medical Association, 272(8), 619–626.
Golden, J., Conroy, R. M., & Lawlor, B. A. (2009). Social support network structure in older people: underlying dimensions and association with psychological and physical health. Psychology, Health & Medicine, 14(3), 280–290. https://doi.org/10.1080/13548500902730135.
Guyatt, G. (1997). Insights and limitations from health-related quality of life research. Journal of General Internal Medicine, 12(11), 720–721.
Hawthorne, G., Herrman, H., & Murphy, B. (2006). Interpreting the WHOQOL-BREF: preliminary population norms and effect sizes. Social Indicators Research, 77(1), 37–59.
Holahan, C. J., & Moos, R. H. (1981). Social support and psychological distress: a longitudinal analysis. Journal of Abnormal Psychology, 90(4), 365.
Hu, L. t., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling: a Multidisciplinary Journal, 6(1), 1–55.
Ikin, J. F., Sim, M., Creamer, M., Forbes, A., McKenzie, D., Kelsall, H., et al. (2004). War-related psychological stressors and risk of psychological disorders in Australian veterans of the 1991 Gulf War. British Journal of Psychiatry, 185(2), 116–126.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. (Research Support, Non-U.S. Gov't Validation Studies). Journal of General Internal Medicine, 16(9), 606–613.
McKenzie, D. P., Ikin, J. F., McFarlane, A. C., Creamer, M., Forbes, A. B., Kelsall, H. L., et al. (2004). Psychological health of Australian veterans of the 1991 Gulf War: an assessment using the SF-12, GHQ-12 and PCL-S. Psychological Medicine, 34(08), 1419–1430.
Mendlowicz, M. V., & Stein, M. B. (2000). Quality of life in individuals with anxiety disorders. American Journal of Psychiatry, 157(5), 669–682.
Muldoon, M. F., Barger, S. D., Flory, J. D., & Manuck, S. B. (1998). What are quality of life measurements measuring? British Medical Journal, 316, 542–544.
Pirkola, S., Saarni, S., Suvisaari, J., Elovainio, M., Partonen, T., Aalto, A.-M., et al. (2009). General health and quality-of-life measures in active, recent, and comorbid mental disorders: a population-based health 2000 study. Comprehensive Psychiatry, 50(2), 108–114.
Proctor, S. P., Harley, R., Wolfe, J., Heeren, T., & White, R. F. (2001). Health-related quality of life in Persian Gulf War veterans. Military Medicine, 166(6), 510–519.
Sareen, J., Cox, B. J., Stein, M. B., Afifi, T. O., Fleet, C., & Asmundson, G. J. (2007). Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosomatic Medicine, 69(3), 242–248.
Schwarz, N., & Clore, G. L. (1983). Mood, misattribution, and judgments of well-being: informative and directive functions of affective States. Journal of Personality and Social Psychology, 45(3), 513.
Sherbourne, C. D., & Stewart, A. L. (1991). The MOS social support survey. Social Science and Medicine, 32, 705–714.
Singh, J., Mattoo, S. K., Sharan, P., & Basu, D. (2005). Quality of life and its correlates in patients with dual diagnosis of bipolar affective disorder and substance dependence. Bipolar Disorders, 7(2), 187–191.
Slade, T., Johnston, A., Oakley Browne, M. A., Andrews, G., & Whiteford, H. (2009). 2007 national survey of mental health and wellbeing: methods and key findings. Australasian Psychiatry, 43(7), 594–605.
Smith, K. W., Avis, N. E., & Assmann, S. F. (1999). Distinguishing between quality of life and health status in quality of life research: a meta-analysis. Quality of Life Research, 8(5), 447–459.
Surìs, A., Lind, L., Kashner, T. M., & Borman, P. D. (2007). Mental health, quality of life, and health functioning in women veterans differential outcomes associated with military and civilian sexual assault. Journal of Interpersonal Violence, 22(2), 179–197.
Teesson, M., Slade, T., & Mills, K. (2009). Comorbidity in Australia: findings of the 2007 national survey of mental health and wellbeing. Australian and New Zealand Journal of Psychiatry, 43(7), 606–614.
The WHOQOL Group. (1998). Development of the World Health Organization WHOQOL-bref quality of life assessment. Psychological Medicine, 28, 551–558.
Toomey, R., Kang, H. K., Karlinsky, J., Baker, D. G., Vasterling, J. J., Alpern, R., et al. (2007). Mental health of US Gulf War veterans 10 years after the war. The British Journal of Psychiatry, 190(5), 385–393.
Voelker, M. D., Saag, K. G., Schwartz, D. A., Chrischilles, E., Clarke, W. R., Woolson, R. F., et al. (2002). Health-related quality of life in Gulf War era military personnel. American Journal of Epidemiology, 155(10), 899–907.
Volk, R. J., Cantor, S. B., Steinbauer, J. R., & Cass, A. R. (1997). Alcohol use disorders, consumption patterns, and health-related quality of life of primary care patients. Alcoholism: Clinical and Experimental Research, 21(5), 899–905.
Von Korff, M., Ormel, J., Keefe, F. J., & Dworkin, S. F. (1992). Grading the severity of chronic pain. Pain, 50, 133–149.
Wang, P. S., Berglund, P., Olfson, M., Pincus, H. A., Wells, K. B., & Kessler, R. C. (2005). Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 603–613.
Ware Jr., J. E., Kosinski, M., & Keller, S. D. (1996). A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220–233.
Weathers, F. W., Litz, B. T., Herman, D. S., Huska, J. A., & Keane, T. M. (1993). The PTSD checklist (PCL): reliability, validity, and diagnostic utility. Paper presented at the 9th Annual Conference of the International Society for Traumatic Stress Studies. San Antonio.
Wittchen, H. (1994). Reliability and validity studies of the WHO-composite international diagnostic interview (CIDI): a critical review. Journal of Psychiatric Research, 28(1), 57–84.
Wolfe, J., Proctor, S. P., Erickson, D. J., Heeren, T., Friedman, M. J., Huang, M. T., et al. (1999). Relationship of psychiatric status to Gulf War Veterans' health problems. Psychosomatic Medicine, 61(4), 532–540.
World Health Organisation. (1997). Composite international diagnostic interview CIDI auto 2.1 administrator's guide and reference. Geneva: World Health Organisation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest.
Disclaimer
The article has been produced using funding provided by the Australian Department of Veterans’ Affairs. However, the views expressed in the article do not necessarily represent the views of the Minister for Veterans’ Affairs or the Department of Veterans’ Affairs. The Commonwealth does not give any warranty nor accept any liability in relation to the contents of this work.
Rights and permissions
About this article
Cite this article
Wright, B.K., Kelsall, H.L., Sim, M.R. et al. Quality of Life in Gulf War Veterans: the Influence of Recency and Persistence of Psychiatric Morbidity. Applied Research Quality Life 14, 23–38 (2019). https://doi.org/10.1007/s11482-017-9579-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-017-9579-7