Abstract
The literature has consistently reported an association between gambling disorders and various comorbid psychiatric and substance conditions. The majority of studies have been cross-sectional in nature, and therefore fail to describe the temporal sequences between these conditions. To investigate these temporal sequences we conducted a scoping review of empirical longitudinal studies that have explored the relationships between gambling disorders and comorbid psychiatric disorders, including any mood and anxiety disorders, suicidal ideations and attempts, and illicit substance, nicotine and alcohol use and dependence. A search was conducted for peer reviewed and unpublished articles, and government reports published between January 2000 and March 2015, with a main focus on the temporal sequence between these two conditions. Studies were only included if they were in English, prospective in nature, studied treatment and population samples and included any form of gambling. A total of 35 publications were identified and the findings discussed in terms of three populations: (i) specific populations, (ii) children, adolescents, and young adults, and (iii) adults. On the basis of these longitudinal findings it is suggested that psychiatric disorders can represent both a precursor and a consequence of problem gambling, and that there are underlying interactive factors, such as impulsivity that can predict and drive both temporal sequences. Screening for comorbid psychiatric conditions upon entering treatment for problem gambling should form an integral part of clinical assessments. However, the extent to which comorbid conditions contribute causally to the development of gambling disorders remains to be conclusively established.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gambling to excess is considered a public health issue, with past year prevalence estimates of gambling disorders ranging between 0.5 and 7.6 %, depending on populations targeted, assessment instruments used, and methodologies employed (Williams et al. 2012). One of the most consistently reported relationships is that between gambling disorders and various psychiatric disorders, such as depression, anxiety, and substance and alcohol use disorders (Petry 2005). Such relationships have been found both in clinical (Delfabbro 2011; Dowling et al. 2015; Ibáñez et al. 2001; Petry 2005; Soberay et al. 2014; Zimmerman et al. 2006), large scale community (Haw 2009; Nower et al. 2004a) and population studies (Desai and Potenza 2008; Kessler et al. 2008; Petry et al. 2005; Pietrzak et al. 2007). A recent systematic review of population studies conducted over the last 12 years indicated that 57.5 % of problem and pathological gamblers had a comorbid substance use disorder, 60.1 % had nicotine dependence, 37.9 % had any mood disorder, and 37.4 % had any anxiety disorder (Lorains et al. 2011).
The majority of these studies have been cross-sectional in nature, allowing researchers to determine correlational relationships between gambling, putative risk and protective variables, and comorbid conditions. However, in the absence of prospective studies, cross-sectional studies do not permit the temporal direction of these variables to be adequately determined. The question remains not only as to whether a comorbid condition preceded the onset of gambling, but the extent to which it contributed to or mediated the development of a gambling disorder. This has clinical implications related to the identification and subsequent management of the primary disorder. The purpose of this paper was to investigate the temporal sequences between these variables by reviewing empirical longitudinal studies that evaluated the relationship between gambling disorders and comorbid psychiatric and substance disorders.
The Different Temporal Sequences of Problem Gambling
Prospective longitudinal studies have the advantage of mapping the ‘natural history of gambling’, that is, tracking the transition from non-gambling through recreational to problem gambling levels, and subsequently through treatment, and recovery (Abbott and Clarke 2007). Additionally, employing this type of methodology makes it possible to determine the temporal sequence of variables and from that, increased confidence in interpreting the presence of putative causal attributions.
As conceptualized by Blaszczynski and Nower (2002), the temporal sequence between problem gambling and comorbid disorders could develop through three different interactive processes: comorbid psychiatric and substance conditions as a vulnerability factor predisposing impaired control; the consequence of gambling-related stressors; or a third independent factor. Where comorbid disorder/s are present before the onset of gambling problems, gambling can be conceptualised as the manifestation of poor coping strategies; that is, gambling is used as an emotional escape. An individual suffering anxiety and in a heightened state of arousal may select low skill gambling activities such as electronic gaming machines in an attempt to distract their attention through dissociative states. Similarly, an individual suffering depression, and thus in a low arousal state, might choose to play high skill games such as casino table games or sports betting, to overcome states of dysphoria and increase arousal. DSM-5 alludes to these motivations in its criterion item, ‘Often gambles when feeling distressed’ (e.g., helpless, guilty, anxious, depressed; American Psychiatric Association 2013).
Alternatively, gambling disorders can commence before the onset of a comorbid psychiatric or substance condition and can be considered a response to adverse outcomes, such as financial crises, social isolation and feelings of guilt. Finally, it is possible that there could be a common underlying interactive factor (or factors) that is responsible for contributing to both the comorbid disorder/s and the problems with gambling. For example, underlying personality traits such as impulsivity may be associated with comorbid conditions (e.g., anti-social disorders) and excessive gambling (Blaszczynski and Nower 2002). Indeed, impulsivity has been identified by several studies as having a predictive role in the development of gambling problems during adolescence and young adulthood (Clarke 2006; Haw 2009; Slutske et al. 2005; Vitaro et al. 2004).
Current Review
The primary objective of this scoping review was to examine findings from empirical longitudinal studies that considered the relationships between these two variables. The focus was on comorbid disorders identified by numerous cross-sectional studies to be significantly associated with problem gambling; including any mood disorder and anxiety disorders, suicidal ideations and attempts, substance use and dependence, alcohol use and dependence, and nicotine dependence. As some cross sectional studies have found impulsivity to play a predictive role in the development of gambling problems, studies that examined impulsivity were also included in this review (Lightsey and Duncan 2002; Nower et al. 2004b; Petry 2001; Turner et al. 2008). Due to the limit research in this area to date, this review was broad and included studies that considered gambling behaviour or gambling disorders as their variable for inclusion.
Method
Search Strategy
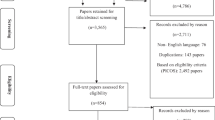
The following electronic literature databases were comprehensively searched: Google Scholar, MEDLINE, PsycINFO, and Web of Science. The search terms used were (gambl* OR problem gambl* OR pathological gambl*) AND either (mental health disorder* OR psychiatric disorder* OR depression OR anxiety OR substance disorder* OR alcohol OR alcohol dependence OR nicotine dependence OR suicid* OR suicid* ideations OR suicid* attempt* OR impulsive*). The search was limited to articles published between January 2000 and March 2015. This date range was chosen to ensure a representative coverage of research conducted post-liberalisation of gambling legislation. After removal of duplicate articles, the search returned 234 unique published articles. Given the varied terminology used to describe problem gambling, for the purpose of this study; ‘pathological gambling’ refers to the most severe form; ‘problem gambling’ to the wider form; and gambling disorder encapsulates all forms of this disorder (at-risk, problem and pathological).
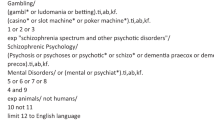
Inclusion and Exclusion Criteria
Studies were included in this review if they were in (i) English, (ii) prospective longitudinal, (iii) studied treatment or population samples, (iv) included any form of gambling such as casino games, electronic gaming machines, betting on sports or dog/harness racing, lotteries, bingo and internet gambling, and (v) considered gambling or problem gambling as their variable. Studies were excluded if they were literature reviews, qualitative in nature, or longitudinal but failed to consider comorbidity. Duplicate articles reporting on the same data set were retained only if they provided additional unique information. The title and abstract of the 234 retrieved articles were scanned for inclusion by two of the authors. Based on the title and abstract, 206 articles were excluded and 28 studies met inclusion criteria. Full texts were only downloaded for these 28 articles.
Additional Searches
In addition, the bibliography of all articles was searched, resulting in a further two articles. A Google search for relevant grey literature such as government and industry reports, and doctoral theses lead to an additional five papers being identified and included. A total of 35 publications formed the basis for this review. Figure 1 summarises the review process.
Data Extraction
The investigators extracted the following relevant information from each included study: (i) country of origin and age range of participants; (ii) sample size at each data collection point; (iii) sampling type; (iv) study design; (v) gambling and psychiatric disorder measures; (vi) prevalence of pathological or problem gambling in the study sample, and (vii) relevant study findings on the temporal sequence between gambling/gambling disorders and the comorbid conditions of interest. Table 1 summarises data for points (i) through to (vi), while (vii) is summarised in text.
Results
General Characteristics of the Included Studies
The majority of the included studies were conducted in Canada (13) and the United States (14). The remaining studies were conducted in Australia (5), New Zealand (1), Sweden (1), and South Africa (1). Most studies were conducted with Western samples, with six focusing on specific populations (e.g., employees, twins, veterans, older adults), 18 on children, adolescents and young adult populations, and 11 on adult populations. Only one study was conducted in a non-western country, South Africa (Hofmeyr et al. 2011). Some epidemiological and naturalistic surveys were conducted with representative samples that included multiple ethnic groups (Chou and Afifi 2011; Parhami et al. 2014; Pilver et al. 2013a, b). Based on these studies, the temporal relationships between gambling and comorbid disorders will be discussed in terms of the following three populations: (a) specific populations; (b) children, adolescents, and young adults; and (c) adults.
Specific Population Findings
Six of the 35 studies considered longitudinal relationships between gambling and comorbid disorders in very specific populations, such as electronic gaming machine (EGM) players (Dickerson et al. 2003); casino employees (Shaffer and Hall 2002); pathological gamblers who had recently quit gambling (Hodgins and el-Guebaly 2010); male monozygotic and dizygotic Vietnam Era Twins (Scherrer et al. 2007); and older adult gamblers (Pilver et al. 2013b; Vander Bilt et al. 2004).
Overall, these studies suggested that in some populations, depression (Scherrer et al. 2007), specific anxiety and mood disorders (Scherrer et al. 2007), drug dependence (Scherrer et al. 2007), alcohol dependence (Scherrer et al. 2007; Vander Bilt et al. 2004), and nicotine dependence (Scherrer et al. 2007) are all significant predictors of problem and pathological gambling up to 10 years later. Similarly, in a study with Australian EGM players, impulsivity and depression were found to be significant predictors of current and later control over gambling behaviours (e.g., how often one visited the venue to gamble) (Dickerson et al. 2003).
When considering treatment outcomes, Hodgins and el-Guebaly (2010), found that past mood disorders and substance use, and problematic alcohol use increased the chance of relapse, and decreased abstinence times. These findings were consistent with previous research by Winters and Kushner (2003) which found that comorbid psychiatric conditions could play a part in compliance rates in treatment. On the other hand, one study with a population based cohort of male monozygotic and dizygotic Vietnam Era Twins, suggested that not having a comorbid disorder was a protective factor against developing pathological gambling at 10-year follow-up (Scherrer et al. 2007). The reverse predictive relationship between the two variables of interest was also found. In older adults, past year problem gambling was found to predict depression disorders, anxiety disorders, any substance use disorder, drug use/dependence, alcohol use/dependence, and nicotine dependence at three-year follow-up (Pilver et al. 2013b).
In contrast, one study involving casino employees, found that staff who developed disordered gambling did not differ in depression, drinking or smoking rates when compared to those who did not develop problem or pathological gambling 2 years later (Shaffer and Hall 2002). However, employees with pre-existing pathological gambling, but not non- and low- risk gamblers, were more likely to develop or experience increases in current psychiatric disorders. This is contradictory to previous findings that suggested that psychiatric and substance use disorders can predict disordered gambling (Pilver et al. 2013b; Vander Bilt et al. 2004), and proposes that there are inconsistencies around psychiatric and substance use variables predicting problem gambling. However, this study used a very specific sample (casino employees) and the authors point out that high attrition rates and response biases may have affected their results.
Limitations
When drawing conclusions from these studies, it is relevant to take into account that all studies focused on very specific sub-groups of the population, thereby limiting their generalisability. However, it does give an insight into the possible longitudinal links between problematic gambling and comorbid psychiatric disorders for populations of interest, such as older adult gamblers and problematic gamblers who are attempting to quit.
Children, Adolescents and Young Adults
Eighteen studies explored longitudinal links between gambling disorders and comorbid psychiatric and substance conditions in children, adolescents and young adult populations. The majority of studies followed large samples, with participant ages ranging from 4 to 26 years.
Gambling and Comorbidity
Six out of the 18 studies considered the longitudinal relationships between comorbid psychiatric conditions and substance use/disorders, and gambling participation. In one study, results indicated that adolescent cigarette and alcohol use, and impulsivity were predictive of increased gambling participation in young adulthood (McComb 2010). The relationship between impulsivity and later self-reported gambling participation was also found in a study with 6th graders (Pagani et al. 2009). Greater impulsivity scores in kindergarten predicted greater gambling involvement when children where in 5th and 6th grade, over other confounds such as parental gambling. Conversely, Breyer et al. (2009) found no relationship between Attention Deficit Hyperactivity Disorder (ADHD; which often includes symptoms that reflect impulsivity) and later gambling participation. However, this could be due to the difference in the study measures used; one considered impulsivity directly, and the other ADHD.
Two studies considered gender differences, and found that for males alcohol misuse was predictive of high or increased gambling over time, even when controlling for other factors (Barnes et al. 2002, 2005). This was also true for females but only when other factors such as high impulsivity or low parental monitoring were also present (Barnes et al. 2002).
One out of the six studies considered both the comorbid variables of interest and the influence the age of onset of comorbid psychiatric conditions may have on gambling disorders. Hayatbakhsch et al. (2006) found that a child’s cigarette smoking and alcohol use, but not depression or anxiety at 5 or 14 years old predicted gambling expenditure at 21 years old. When considering age of onset, smoking, alcohol consumption and cannabis use before the age of 15 years predicting greater gambling participation and higher gambling expenditure in young adulthood.
Gambling Disorders and Mood and Anxiety Disorders
The remaining 12 studies all considered the temporal relationships between comorbid psychiatric and substance disorders and gambling disorders. Longitudinal relationships for problem gambling and mood and anxiety disorders were mixed. Even though cross-sectional studies had previously found a positive relationship between mood disorders and problem gambling, only two longitudinal studies found this to be true, with greater early adolescent depression in males weakly associated with problem gambling in late adolescence (Feigelman et al. 2006; Lee et al. 2011). The majority of studies reported no significant relationship between child or adolescent depression (Edgerton et al. 2014; Hayatbakhsch et al. 2006; Shenassa et al. 2011) or internalizing symptoms (Scholes-Balog et al. 2015) and later problem gambling severity. This is despite two studies finding an initial positive cross-sectional relationship between these two variables (Edgerton et al. 2014; Scholes-Balog et al. 2015). This was also true when anxiety was considered, with all three studies that included anxiety as a measure, finding no significant longitudinal relationship between anxiety and problem gambling (Edgerton et al. 2014; Hayatbakhsch et al. 2006; Scholes-Balog et al. 2014).
Gambling Disorders and Suicidality
One study explored the relationship between suicidality in adolescence and disordered gambling 7 years later, and found differing results for males and females (Feigelman et al. 2006). Male problem gamblers were no more likely than non-gamblers to have suicidal thoughts or attempts in adolescence. In contrast, young adult female problem gamblers had significantly more suicidal thinking and attempts throughout adolescence than female non-gamblers, suggesting a gender difference between suicidality and problem gambling for adolescents and young adults.
Gambling Disorders and Substance Use/Disorders
Significant associations were found between adolescent substance use (Winters et al. 2002), hazardous alcohol consumption (Hayatbakhsch et al. 2006; Scholes-Balog et al. 2014) and heavy smoking (Hayatbakhsch et al. 2006; Scholes-Balog et al. 2014), and disordered gambling in young adulthood. Furthermore, when considering other relevant predictive variables, Scholes-Balog et al. (2014) found that adolescent alcohol drinkers who had low levels of rewards for pro-social involvement had an increased probability of problem gambling as young adults when compared to non-drinkers. Nevertheless, two of the included studies reported no longitudinal links between adolescent substance use (Wanner et al. 2009), substance dependence, and alcohol dependence (Edgerton et al. 2014) and later problem gambling.
Gambling Disorders and Impulsivity
One of the variables most often assessed and found to be associated with problem gambling in this population appears to be impulsivity. Four studies reported that higher levels of impulsivity in childhood and adolescence predicted later problem gambling (Martins et al. 2008; Shenassa et al. 2011; Vitaro et al. 2001, 2004). Similarly, individuals with sustained ADHD throughout childhood and young adulthood had a greater chance of subsequent problem gambling severity (Breyer et al. 2009). One study considered the relationship between impulsivity and stability of problem gambling between adolescence and adulthood (Wanner et al. 2009). They found that individuals high in impulsivity had moderately stable gambling problems between adolescence and adulthood, whereas individuals low in impulsivity had unstable problem gambling patterns. This suggests that impulsivity has a role in sustaining problem gambling and that previous findings, which have shown problem gambling to be transitory, unstable and multidirectional in their course (LaPlante et al. 2008), might only be applicable to individuals low on impulsivity.
Similarly, Edgerton et al. (2014) found that impulsiveness was the only variable to affect change of problem gambling severity over time, but not in the expected direction; higher initial impulsiveness predicted slightly faster rates of declining problem gambling severity. This is different to the majority of other findings that found impulsivity to be positively associated with problem gambling (Clarke 2006; Haw 2009; Vitaro et al. 2004). However, Edgerton et al. (2014) note that this relationship might not be true due to the way that impulsivity was measured at only two time points during a very transitional period in life. They suggest that the relationship might look different if impulsivity had been measured as a time variant variable.
Two studies considered the interactive effects of impulsivity and depression on problem gambling. First, Dussault et al. (2011) found that early impulsivity at age 14 predicted both depression and problem gambling at age 17 and problem gambling at age 23. Interestingly, both gambling problems and depression at age 17 predicted depression and problem gambling at age 23 respectively. This suggests that even though, impulsivity predicted both the development of depression and gambling, once they had both developed, their escalation was better explained by a mutual interactive influence on each other. On the other hand, in Lee et al.’s (2011) study, early adolescent depression and not impulsivity was related (weakly) to late adolescent gambling in males. Unlike, the previous study, the combined effect of early impulsivity and depression was divisive and not synergistic on later problem gambling. For example in this study, an individual with high depression who started exhibiting greater impulsivity would have decreased odds of problem gambling later on.
This divisive effect of two comorbid conditions on later problem gambling is not consistent with most research on comorbidy, that suggests that the presence of a comorbid disorder is linked to greater gambling problems and worse outcomes (Ibáñez et al. 2001; Ladd and Petry 2003; Petry 2005). Lee et al. (2011) proposes one explanation, that is, that those individuals with comorbid depression and high impulsivity might direct their disinhibition inwards in the form of self-destructive behaviours, instead of outwards to gambling, which is an external form of escapism. However, this does not explain the findings of Dussault et al. (2011) who found that impulsivity and depression had a mutual interactive effect on problem gambling. Instead, it might be that Lee et al.’s (2011) findings are limited in their generalisability beyond their study sample as it primarily included African-American youths from inner city suburbs.
Strengths and Limitations
Strengths of the studies included their prospective designs, corroboration of self-reports by teachers and parents (e.g., Hayatbakhsch et al. 2006; Lee et al. 2011; Martins et al. 2008; Vitaro et al. 2004) and long follow-up periods (range = 3 to 30 years). This is especially important for this cohort as adolescence and young adulthood are marked by frequent developmental transitions and changes. On the other hand, one of the main limitations of several studies was that gambling/gambling disorders and comorbid psychiatric and substance measures were not always measured at all time points (such as in Edgerton et al. 2014; Feigelman et al. 2006; Wanner et al. 2009), greatly limiting temporal conclusions that could be drawn from the data. Further, many samples were specific to certain population sub-groups. For example, Dussault et al. (2011), Vitaro et al. (2001), Vitaro et al. (2004), and Wanner et al. (2009), all followed a sample of boys attending schools in low socio-economic areas, Pagani et al. (2009) children from disadvantaged areas, and Lee et al. (2011) only included inner city African-American male adolescents. Therefore large-scale, nationally representative longitudinal studies with children, adolescents and young adults are still required to examine if the above findings are generalisable to the wider adolescent subpopulation.
Adults
A total of 11 longitudinal studies examined the temporal relationships of interest in adult populations. One study considered Internet gambling and comorbid psychiatric and substance conditions finding that depression and anxiety symptomology, or alcohol and smoking were all predictive factors for gambling on the Internet one year later (Svensson and Romild 2011). The remaining studies all considered gambling disorders as their dependent variable.
Findings from Large-Scale Population Studies
Four studies assessed samples from two large representative studies: US-National Epidemiological Survey on Alcohol and Related Conditions [NESARC]; and The Victorian Gambling Study (Billi et al. 2014). In the Victorian Gambling Study, depression and anxiety disorders, alcohol use/dependence, and nicotine dependence were all predictors of future problem gambling (Billi et al. 2014).
On the other hand, disordered gambling was also found to precede the onset of comorbid conditions. Chou and Afifi (2011) assessed data from the NESARC and found that disordered gambling was a predictor of later new onset comorbid psychiatric disorders, such as mood and anxiety disorders, substance use/disorders, and alcohol use/disorders (Chou and Afifi 2011). Pilver et al. (2013a) considered gender differences in the NESARC data, and found that over the course of 3 years, at-risk or problem female gamblers were more likely to develop nicotine dependence when compared to non-gambling females, while at-risk and problem male gamblers were more at-risk of developing an alcohol use disorder than non- or low frequency male gamblers. These authors suggest that this is in line with previous research, which has shown that women are more likely than men to smoke for stress relief, and that men are more likely than women to consume alcohol in response to stress and emotional arousal.
Parhami et al. (2014) used data from the NESARC to consider the longitudinal relationship between different gambling problem levels and comorbid psychiatric conditions. Compared to non-gamblers, individuals who reported any gambling behaviour at the start of the study (gambling disorder, sub-threshold gambling disorder, low frequency gambling) had an increased risk for the onset of a comorbid mood, anxiety or substance use disorder 3 years later. This relationship was graded in that those with a gambling disorder were at the highest risk for the new onset of a comorbid psychiatric disorder and those with recreational gambling were at the lowest risk.
A graded relationship was also found for some specific disorders, such as phobias, PTSD, alcohol disorders, and any non-nicotine or non-alcohol substance use disorders. Further, sub threshold gambling disorder and gambling disorders were associated with the onset of multiple psychiatric disorders, suggesting that not only is problem gambling a risk factor for developing psychiatric disorders but some gambling disorders may also affect the onset of multiple comorbid conditions. However, temporal conclusions are limited for three of these studies (Chou and Afifi 2011; Parhami et al. 2014; Pilver et al. 2013a) as gambling was only assessed initially and not at time two. Therefore the reciprocal nature of these relationships could not be explored.
Findings from Community and Convenience Samples
Studies that examined community or convenience samples also found similar longitudinal links between various comorbid conditions and gambling disorders. The only New Zealand longitudinal study reported that individuals with problematic or hazardous use of alcohol at the beginning of the study were much more likely to be problematic gamblers 7 years later (Abbott et al. 2004). Interestingly, more of the problem and pathological gamblers at the beginning of the study continued to engage in hazardous or problematic drinking 7 years later than continued to experience gambling problems. This may suggest that gambling problems, as opposed to alcohol problems are more transitory in nature. These findings point out the importance of examining comorbidities with problem gambling. Even though individuals might recover from problem gambling, they could still have problems with their other co-occurring disorders. However, findings from this study need to be replicated with a large sample size, as the sample size in the study was very small, and there were high attrition rates between the first and second assessments.
Two recent longitudinal studies in Canada and the United States implemented similar study designs in their data collection, allowing them to conducted parallel analysis in order to identify more robust and comprehensive findings (el-Guebaly, N et al. 2015; Williams et al. 2015). Findings from both suggested that no single variable was singly present in people who subsequently became problem gamblers but that many different variables each increased the risk of future problem gambling. el-Guebaly, N et al. (2015) recruited adult participants through random digital dialling, and identified impulsivity as one of the strongest predictors of later problem gambling, while depression and anxiety predicted problem gambling but not gambling involvement. On the other hand, drug abuse and alcohol use disorder were not associated with either. Individuals with more than one comorbid psychiatric condition were more likely to develop gambling problems but not more likely to be involved in gambling, suggesting that comorbid conditions were more involved in problematic gambling development.
Similarly, Williams et al. (2015) recruited individuals from the community through random digital dialling, and found that impulsivity was one of the strongest predictors of future problem gambling. Likewise, depression was the strongest predictor within the mental health variables, with anxiety-disorders, substance use and lifetime histories of drug and alcohol addictions and mental health problems as other important predictors of future problem gambling. Multivariate analysis suggested that impulsivity, lifetime history of addiction to drugs or alcohol, and a family history of mental health problems were important predictors of future problem gambling. Williams et al. (2015) also explored possible predictors of first onset problem gambling and problem gambling continuation and relapse. They found that impulsivity, depression and tobacco use were all related to first onset problem gambling, while the presence of any comorbid mental health disorder, a life time history of mental health or substance use problems made it more difficult for problem gamblers to recover and/or more susceptible to relapse once they had recovered.
Three studies investigated how comorbid conditions were affecting progression between problem gambling groups (e.g., from at-risk to problem gambling). Currie et al. (2011) study indicated that gamblers who were low-risk at time one but subsequently shifted into the high-risk gambling behaviour group by time two were more likely to be male, older, play electronic gaming machines, and were tobacco users. Surprisingly, even though cross-sectional studies have suggested otherwise, depression, substance dependence and impulsivity did not predict shifting from low to high gambling behaviour. The authors suggested that maybe these factors were more effective in identifying people who were vulnerable in progressing from high-risk to pathological gambling only. However, in an Australian study, showing signs of alcohol dependence, being a current smoker and anxiety were all associated with progressing to higher risk problem gambling categories (e.g., from non-problem gambler to at-risk gambler (Billi et al. 2014). Anxiety however was the only health condition that independently predicted an individual’s progression through gambling statuses.
Finally, the last of these three studies found that depression and illicit drug use was associated with greater problem gambling severity at the start of the study, and a faster rate of decline in problem gambling over time (Wiebe et al. 2009). Problematic alcohol use on the other hand was only associated with initial levels of problem gambling and only had one third of the rate of decrease in problem gambling over time. These authors proposed that perhaps alcohol and problem gambling were associated behaviours but that illicit drug use and problem gambling were incompatible over long periods of time. Greater participation in one activity might necessitate the decrease in participation in the other. While these individuals might appear to have recovered from their problem gambling disorder, they may still suffer from an associated comorbid disorder or problem.
The only study conducted with a non-western sample (South African) found similar results to the other adult studies included in this review (Hofmeyr et al. 2011). The authors recruited individuals via two pathways: newspaper advertisements and a subsample from a previous study of 3,000 individuals. Changes over time in depression, anxiety, and impulsivity were significantly associated with accompanying changes in problem gambling severity over time. However, due to the study’s design the authors could not make any further conclusions, including causal inferences, between these four variables. As western countries become increasingly multicultural, and research has shown that culture, values and beliefs all influence gambling participation, patterns and attitudes towards seeking treatment (Raylu and Oei 2004), it is important that future research is conducted with large-scale representative samples, or studies examine problem gambling in different cultural contexts and among different racial/ethnic groups.
Limitations
Even though many of the adult studies either included large representative community or large-scale population samples, several limitations remained. Many studies suffered either high dropout rates, resulting in the final sample no longer being representative of the target population (e.g., Billi et al. 2014), or did not include sufficient numbers of problem gamblers to conduct planned analyses, without the necessity of including moderate or at-risk gamblers (e.g., Wiebe et al. 2009). Furthermore, three out of the 11 studies were based on one longitudinal study conducted in the U.S.: the NESARC. Outcomes from these studies were limited by the design of the NESARC survey as, even though the NESARC was conducted over two time points, it only measured problem gambling at the first time point limiting the analysis and outcomes the authors could measure.
Discussion
Overall the longitudinal findings in this scoping review give us an insight into what the temporal sequences between gambling and/or gambling disorders and comorbid psychiatric and substance conditions may be. Longitudinal links between gambling disorders and comorbid conditions appear to be bidirectional for mood and anxiety disorders, substance use/dependence, alcohol use/dependence, and nicotine dependence in child, adolescent, young adult and adult populations. On the other hand, impulsivity appears to be a strong predictor of later problem gambling and an underlying interactive factor that can drive both the development of gambling disorders and depression. Substance and nicotine use, impulsivity, and depression were found to be associated with the onset of problem gambling, while the presence of nicotine use, substance and alcohol dependence, anxiety, depression and impulsivity seem to affect the progression to more problematic gambling categories (e.g., from at-risk to problem gambling). While, not having a psychiatric disorder was also identified as a protective factor against later problem gambling.
These longitudinal associations broadly fit the pathway model (Blaszczynski and Nower 2002) described previously, which theorizes that temporal relationships between problem gambling and comorbid disorders occurs through three different interactive processes; comorbid psychiatric conditions or substance and alcohol disorders as a vulnerability factor predisposing impaired control over one’s gambling, the consequence of gambling-related stressors, or in the case of impulsivity, as a third independent factor. However, after reviewing the literature, the question remains to what extent comorbid conditions contribute to the development of gambling disorders and vice versa, the extent gambling disorders contribute to the development of comorbid disorders.
Perhaps the presence of comorbid conditions increases one’s general risk of developing a gambling disorder, and vice versa, gambling disorders increase one’s general risk of developing comorbid psychiatric conditions but other factors such as individual and environmental characteristics are also involved. This is evident from studies finding that, although there are significant longitudinal links between psychiatric conditions and problem gambling, the predictive power of comorbid psychiatric conditions on later problem gambling is generally weak (Dussault et al. 2011; Feigelman et al. 2006; Hayatbakhsch et al. 2006; Lee et al. 2011). For example, a recent study by Williams et al. (2015) was able to account for between 69 and 90 % of the variance for future problem gambling by taking other relevant variables in to account. The authors identified several other variables that were significant in predicting future problem gambling, including being an at-risk or problem gambler, participating in continuous forms of gambling, past big gambling wins, family members who are regular gamblers and family/friends who have gambling problems. This suggests that there are no single variables, such as comorbid psychiatric conditions, that are overwhelmingly predictive of disordered gambling but that many variables combine to contribute small but significant effects.
Future Directions
Although 35 studies were identified that had considered the temporal relationships between gambling/gambling disorders and comorbid psychiatric disorders and substance and alcohol disorders, many of them had limitations, such as very specific target groups, small sample sizes, high attrition rates, and limitations in study designs and subsequently data analysis and outcomes. Future studies in this area could improve on these methodological limitations to enable more accurate tracking of the longitudinal relationships between gambling and comorbid conditions, and the ability to determine the extent these variables contribute to the development of each other.
Another important area for future research may be the relationships between gambling, comorbid psychiatric and substance conditions and different gambling forms. There has been some evidence in the literature that problem and moderate risk gambling are more likely to be associated with continuous forms of gambling such as electronic gaming machines (EGM) and racing, and that ‘safer forms’ of gambling such as lotto and scratchcards cause fewer problems (Delfabbro 2011; Productivity Commission 2010). However, as far as the authors could find, no previous longitudinal studies had specifically examined the relationships between disordered gambling, comorbid conditions and different gambling forms.
It should be noted that one of the studies in this review surveyed only EGM players in an Australian gaming venue and found that impulsivity and depression predicted current and future control over gambling behaviours (Dickerson et al. 2003). However, this study did not ask participants about their other gambling activities, or control for these when testing for the above relationships. Similarly, even though some of the studies in this review measured gambling activities and participation rates in different gambling activities, none examined the specific relationships between comorbid psychiatric disorders and disordered gambling on different gambling forms. Instead, the majority of the studies only considered general gambling behaviour or problem gambling measures as the dependent variable in their research.
Treatment Implications
This scoping review provides several implications for the prevention of gambling disorders. Firstly, the results from this review support the need for problem gambling initiatives to have a more holistic approach by targeting both gambling disorders and the wide range of psychiatric conditions that are associated with gambling disorders. Those gambling disorders treatment services that are currently not routinely screening for comorbid psychiatric conditions should strongly consider implementing this as part of their intake procedures. Similarly, other treatment services for the various comorbid conditions should consider routine screening for gambling-related problems. Doing so might help reduce the future incidence of gambling disorders and assist with relapse and recovery rates. Relevant training in treating comorbid conditions should also be on offer to gambling treatment providers, as well as gambling treatment training for relevant mental health professionals. In services were this is not a possibility, greater inter-agency collaboration and referrals could be encouraged.
Furthermore as noted by Dowling et al. (2016) and Winters and Kushner (2003), there are few studies that have attempted to clarify how comorbid psychiatric and substance conditions affect treatment outcomes from well-known problem gambling treatments, and whether gambling disorders and comorbid conditions should be treated together or sequentially. A recent systematic review by Dowling et al. (2016) identified only 21 studies which considered the influence of comorbid conditions on problem gambling treatment outcomes. Even though they found that overall comorbid conditions don’t seem to contradict the affects of established problem gambling treatments such as CBT, the responses from different sub groups of psychiatric conditions varied widely.
Similarly, it remains uncler whether with comorbidies it is more effective to treat each condition according to the severity of the disorder, or treat the condition that appeared first in the temporal relationship (Toneatto and Miller 2004; Winters and Kushner 2003). Further research that considers treatment outcomes from gambling disorders with comorbidities, and studies which compare treating gambling disorders and comorbidies either sequentially or according to their temporal nature are required before best practices in this area can be determined.
However, with all these recommendations caution needs to be taken around potentially stigmatising problem gamblers as mentally ill. This might have a counter productive effect, with stigmatisation resulting in less problem gamblers seeking treatment. Instead, the aim for both treatment providers and gambling policy should be education on which comorbidities are most likely to present, and best practices for treating both.
References
Abbott, M. W., & Clarke, D. (2007). Prospective problem gambling research: contribution and potential. International Gambling Studies, 7(1), 123–144.
Abbott, M. W., Williams, M. M., & Volberg, R. A. (2004). A prospective study of problem and regular nonproblem gamblers living in the community. Substance Use & Misuse, 39(6), 855–884.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. Fifth Edition. American Psychiatric Association. Available from: http://psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596. Accessed 5 Jan 2015.
Barnes, G. M., Welte, J. W., Hoffman, J. H., et al. (2002). Effects of alcohol misuse on gambling patterns in youth. Journal of Studies on Alcohol, 63(6), 767–775.
Barnes, G. M., Welte, J. W., Hoffman, J. H., et al. (2005). Shared predictors of youthful gambling, substance use, and delinquency. Psychology of Addictive Behaviors, 19(2), 165–174.
Billi R, Stone CA, Marden P, et al. (2014) The Victorian gambling study a longitudinal study of gambling and health in Victoria 2008–2012. North Melbourne: Victorian Responsible Gambling Foundation. Available from: http://www.responsiblegambling.vic.gov.au/__data/assets/pdf_file/0008/10016/A-LONGITUDINAL-STUDY-OF-GAMBLING-AND-HEALTH-IN-VICTORIA-20082012.pdf (5 January 2015).
Blaszczynski, A., & Nower, L. (2002). A pathways model of problem and pathological gambling. Addiction, 97(5), 487–499.
Breyer, J. L., Botzet, A. M., Winters, K. C., et al. (2009). Young adult gambling behaviors and their relationship with the persistence of ADHD. Journal of Gambling Studies, 25(2), 227–238.
Chou, K.-L., & Afifi, T. O. (2011). Disordered (pathologic or problem) gambling and axis I psychiatric disorders: results from the national epidemiologic survey on alcohol and related conditions. American Journal of Epidemiology, 173(11), 1289–1297.
Clarke, D. (2006). Impulsivity as a mediator in the relationship between depression and problem gambling. Personality and Individual Differences, 40(1), 5–15.
Currie, S. R., Hodgins, D. C., Casey, D. M., et al. (2011). Examining the predictive validity of low-risk gambling limits with longitudinal data: Predictive validity of low-risk gambling limits. Addiction, 107(2), 400–406.
Delfabbro, P. H. (2011). Australasian gambling review. South Australia: Independent Gambling Authority.
Desai, R. A., & Potenza, M. N. (2008). Gender differences in the associations between past-year gambling problems and psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology, 43(3), 173–183.
Dickerson M, Haw J and Shepherd L (2003) The psychological causes of problem gambling: A longitudinal study of at risk recreational EGM players. Thesis, University of Western Sydney. Available from: http://www.olgr.nsw.gov.au/rr_pcpg.asp.
Dowling, N. A., Cowlishaw, S., Jackson, A. C., Merkouris, S. S., Francis, K. L., & Christensen, D. R. (2015). Prevalence of psychiatric comorbidity in treatment-seeking problem gamblers: A systematic review and meta-analysis. Australian and New Zealand Journal of Psychiatry, 49(6), 519–539. doi:10.1177/0004867415575774.
Dowling, N. A., Merkouris, S. S., & Lorains, F. K. (2016). Interventions for comorbid problem gambling and psychiatric disorders: Advancing a developing field of research. Addictive Behaviors, 58, 21–30. doi:10.1016/j.addbeh.2016.02.012.
Dussault, F., Brendgen, M., Vitaro, F., et al. (2011). Longitudinal links between impulsivity, gambling problems and depressive symptoms: a transactional model from adolescence to early adulthood: Impulsivity, gambling problems and depressive symptoms. Journal of Child Psychology and Psychiatry, 52(2), 130–138.
Edgerton, J. D., Melnyk, T. S., & Roberts, L. W. (2014). Problem gambling and the youth-to-adulthood transition: assessing problem gambling severity trajectories in a sample of young adults. Journal of Gambling Studies, 31(4), 1463–1485.
el-Guebaly, N., Casey, D. M., Currie, S. R., et al. (2015) The leisure, lifestyle, & lifecycle project (LLLP): A longitudinal study of gambling in Alberta. Alberta: Alberta Gambling Research Institute. Available from: http://www.abgamblinginstitute.ualberta.ca/Research/StrategicPartnershipsCollabora/LeisureLifestyleLifecycleProje.aspx.
Feigelman, W., Gorman, B. S., & Lesieur, H. (2006). Examining the relationship between at-risk gambling and suicidality in a national representative sample of young adults. Suicide & Life-Threatening Behavior, 36(4), 396–408.
Haw, J. (2009). Impulsivity partially mediates the relationship between depression and problem gambling. Gambling Research, 21(2), 12.
Hayatbakhsch MR, Najman JM, Aird R, et al. (2006) Early life course determinants of young adults’ gambling behaviour. Reported prepared for the Office of Gaming regulation, Queensland Treasury. Available from: http://www.researchgate.net/profile/Michelle_Heron-Delaney/publication/37629964_Early_life_course_determinants_of_young_adults’_gambling_behaviour._An_Australian_Longitudinal_Study/links/0912f507ddf1e49cc5000000.pdf. Accessed 6 Jan 2015.
Hodgins, D. C., & el-Guebaly, N. (2010). The influence of substance dependence and mood disorders on outcome from pathological gambling: five-year follow-up. Journal of Gambling Studies, 26(1), 117–127.
Hofmeyr, A., Dellis, A., Kincaid, H., et al. (2011) Report on the national longitudinal study of gambling behaviour (NLSGB) in South Africa. September. Available from: http://www.responsiblegambling.co.za/media/user/documents/NLSGB%20report%20-%20September%202011.pdf. Accessed 6 Jan 2015.
Ibáñez, A., Blanco, C., Donahue, E., et al. (2001). Psychiatric comorbidity in pathological gamblers seeking treatment. American Journal of Psychiatry, 158(10), 1733–1735.
Kessler, R. C., Hwang, I., LaBrie, R., et al. (2008). DSM-IV pathological gambling in the national comorbidity survey replication. Psychological Medicine, 38(09), 1351–1360.
Ladd, G. T., & Petry, N. M. (2003). A comparison of pathological gamblers with and without substance abuse treatment histories. Experimental and Clinical Psychopharmacology, 11(3), 202–209.
LaPlante, D. A., Nelson, S. E., LaBrie, R. A., et al. (2008). Stability and progression of disordered gambling: lessons from longitudinal studies. The Canadian Journal of Psychiatry/La Revue Canadienne de Psychiatrie, 53(1), 52–60.
Lee, G. P., Storr, C. L., Ialongo, N. S., et al. (2011). Compounded effect of early adolescence depressive symptoms and impulsivity on late adolescence gambling: a longitudinal study. Journal of Adolescent Health, 48(2), 164–169.
Lightsey, O. R., Jr., & Duncan, C. (2002). Impulsivity, coping, stress, and problem gambling among university students. Journal of Counseling Psychology, 49(2), 202–211.
Lorains, F. K., Cowlishaw, S., & Thomas, S. A. (2011). Prevalence of comorbid disorders in problem and pathological gambling: systematic review and meta-analysis of population surveys: comorbid disorders in pathological gambling. Addiction, 106(3), 490–498.
Martins, S. S., Storr, C. L., Ialongo, N. S., et al. (2008). Gender differences in mental health characteristics and gambling among African-American adolescent gamblers. American Journal on Addictions, 17(2), 126–134.
McComb JL (2010) A longitudinal study of family influences on gambling behavior in early adulthood. PhD Thesis, Purdue University, Indiana. Available from: http://docs.lib.purdue.edu/dissertations/AAI3444721.
Nower, L., Gupta, R., Blaszczynski, A., et al. (2004a). Suicidality and depression among youth gamblers: a preliminary examination of three studies. International Gambling Studies, 4(1), 69–80.
Nower, L., Derevensky, J. L., & Gupta, R. (2004b). The relationship of impulsivity, sensation seeking, coping, and substance use in youth gamblers. Psychology of Addictive Behaviors, 18(1), 49–55.
Pagani, L., Japel, C., & Derevensky, J. (2009). Predicting gambling behavior in sixth grade from kindergarten impulsivity: a tale of developmental continuity. Archives of Pediatrics & Adolescent Medicine, 163(3), 238–243.
Parhami, I., Mojtabai, R., Rosenthal, R. J., et al. (2014). Gambling and the onset of comorbid mental disorders: a longitudinal study evaluating severity and specific symptoms. Journal of Psychiatric Practice, 20(3), 207–219.
Petry, N. M. (2001). Substance abuse, pathological gambling, and impulsiveness. Drug and Alcohol Dependence, 63(1), 29–38.
Petry, N. M. (2005). Comorbidity of disordered gambling and other psychiatric disorders. In: Pathological gambling: Etiology, comorbidity, and treatment, Washington, DC, US: American Psychological Association, pp. 85–115.
Petry, N. M., Stinson, F. S., & Grant, B. F. (2005). Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: results from the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry, 66(5), 564–574.
Pietrzak, R. H., Morasco, B. J., Blanco, C., et al. (2007). Gambling level and psychiatric and medical disorders in older adults: results from the national epidemiologic survey on alcohol and related conditions. The American Journal of Geriatric Psychiatry, 15(4), 301–313.
Pilver, C. E., Libby, D. J., Hoff, R. A., et al. (2013a). Gender differences in the relationship between gambling problems and the incidence of substance-use disorders in a nationally representative population sample. Drug and Alcohol Dependence, 133(1), 204–211.
Pilver, C. E., Libby, D. J., Hoff, R. A., et al. (2013b). Problem gambling severity and the incidence of axis I psychopathology among older adults in the general population. Journal of Psychiatric Research, 47(4), 534–541.
Productivity Commission (2010) Gambling. Canberra. Available from: http://www.pc.gov.au/projects/inquiry/gambling-2009/report. Accessed 16 Dec 2015.
Raylu, N., & Oei, T. P. (2004). Role of culture in gambling and problem gambling. Clinical Psychology Review, 23(8), 1087–1114.
Scherrer, J. F., Slutske, W. S., Xian, H., et al. (2007). Factors associated with pathological gambling at 10-year follow-up in a national sample of middle-aged men. Addiction, 102(6), 970–978.
Scholes-Balog, K. E., Hemphill, S. A., Dowling, N. A., et al. (2014). A prospective study of adolescent risk and protective factors for problem gambling among young adults. Journal of Adolescence, 37(2), 215–224.
Scholes-Balog, K. E., Hemphill, S. A., Toumbourou, J. W., et al. (2015). Problem gambling and internalising symptoms: a longitudinal analysis of common and specific social environmental protective factors. Addictive Behaviors, 46, 86–93.
Shaffer, H. J., & Hall, M. N. (2002). The natural history of gambling and drinking problems among casino employees. The Journal of Social Psychology, 142(4), 405–424.
Shenassa, E. D., Paradis, A. D., Dolan, S. L., et al. (2011). Childhood impulsive behavior and problem gambling by adulthood: a 30-year prospective community-based study. Addiction, 107(1), 160–168.
Slutske, W. S., Caspi, A., Moffitt, T. E., et al. (2005). Personality and problem gambling: a prospective study of a birth cohort of young adults. Archives of General Psychiatry, 62(7), 769–775.
Soberay, A., Faragher, J. M., Barbash, M., et al. (2014). Pathological gambling, co-occurring disorders, clinical presentation, and treatment outcomes at a university-based counseling clinic. Journal of Gambling Studies, 30(1), 61–69.
Svensson, J., & Romild, U. (2011). Incidence of Internet gambling in Sweden: results from the Swedish longitudinal gambling study. International Gambling Studies, 11(3), 357–375.
Toneatto, T., & Miller, G. (2004). Assessing and treating problem gambling: empirical status and promising trends. Canadian Journal of Psychiatry, 49, 517–525. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15453101 .
Turner, N. E., Jain, U., Spence, W., et al. (2008). Pathways to pathological gambling: component analysis of variables related to pathological gambling. International Gambling Studies, 8(3), 281–298.
Vander Bilt, J., Dodge, H. H., Pandav, R., et al. (2004). Gambling participation and social support among older adults: a longitudinal community study. Journal of Gambling Studies, 20(4), 373–389.
Vitaro, F., Brendgen, M., Ladouceur, R., et al. (2001). Gambling, delinquency, and drug use during adolescence: mutual influences and common risk factors. Journal of Gambling Studies, 17(3), 171–190.
Vitaro, F., Wanner, B., Ladouceur, R., et al. (2004). Trajectories of gambling during adolescence. Journal of Gambling Studies, 20(1), 47–69.
Wanner, B., Vitaro, F., Carbonneau, R., et al. (2009). Cross-lagged links among gambling, substance use, and delinquency from midadolescence to young adulthood: additive and moderating effects of common risk factors. Psychology of Addictive Behaviors, 23(1), 91–104.
Wiebe J, Maitland SB, Hodgins D, et al. (2009) Transitions and stability of problem gambling behaviours. Report prepared for the Addictions Foundation of Manitoba. Available from: http://prism.ucalgary.ca//handle/1880/48239. Accessed 6 Jan 2015.
Williams RJ, Volberg RA and Stevens RM (2012) The population prevalence of problem gambling: Methodological influences, standardized rates, jurisdictional differences, and worldwide trends. Report prepared for the Ontario Problem Gambling Research Centre. Available from: https://www.uleth.ca/dspace/handle/10133/3068. Accessed 6 Jan 2015.
Williams, R. J., Hann, R., Schopflocher, D., et al. (2015). Quinte longitudinal study of gambling and problem gambling. Reported for the Ontario Problem Gambling Research Centre. Available from: https://uleth.ca/dspace/handle/10133/3641. Accessed 6 Jan 2015.
Winters, K. C., & Kushner, M. G. (2003). Treatment issues pertaining to pathological gamblers with a comorbid disorder. Journal of Gambling Studies, 19(3), 261–277.
Winters, K. C., Stinchfield, R. D., Botzet, A., et al. (2002). A prospective study of youth gambling behaviors. Psychology of Addictive Behaviors, 16(1), 3–9.
Zimmerman, M., Chelminski, I., & Young, D. (2006). Prevalence and diagnostic correlates of DSM-IV pathological gambling in psychiatric outpatients. Journal of Gambling Studies, 22(2), 255–262.
Acknowledgements
This work was supported by a philanthropic grant provided by The Registered Clubs Association of New South Wales (Clubs NSW), Australia.
Author’s Contributions
All authors contributed substantially to 1) the literature review, including searching for, collating and critically analysing research articles; 2) the drafting and revision of the manuscript; and 3) have read and approved the current version of the manuscript to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Melanie Hartmann has no financial disclosures to declare.
Dr Blaszczynski has had financial professional dealings with the gambling industry and various State and Federal governments directly and indirectly over the last 3 years including research funding, personal fees for professional consultancy, honoraria for grant reviews and theses examination, royalties for published books, and funding and expenses covered to attend and present at conference and government meetings from:
• Gambling industry operators including La Loterie Romande (Switzerland), Svenska Spel (Sweden), Club NSW (Australia), Comelot (UK), La Française des Jeux (France), Loto-Québec (Québec, Canada), Casino Austria, National Lottery (Belgium), Sportsbet, British Columbia Lottery Corporation, Aristocrat Leisure Industries
• Organisations that are funded directly or indirectly from the gambling industry or levies on the gambling industry including the Victorian Responsible Gambling Foundation, Ontario Problem Gambling Research Centre, the Responsible Gambling Trust, Manitoba Gambling Research Program, Ministerial Expert Advisory Group (Federal Government), and honoraria and expense reimbursement for training programs and workshops conducted from government funded problem gambling counselling services
• Government funded agencies including the NSW Office of Liquor, Gaming, & Racing, Australian Institute of Family Studies, Gambling Research Australia, Australian Department Social Services
• Non-industry or government agencies including the National Association for Gambling Studies, National Council on Problem Gambling, Le Comité d’organisation Congrès international sur les troubles addictifs
All professional dealings have been conducted with the aim of enhancing responsible gambling and harm minimisation policies and practices, training counsellors in the treatment interventions, and advancing our understanding of the psychology of gambling.
Competing Interests
The authors declare that there are no competing interests in the preparation of this manuscript.
Declaration
We confirm that this work is original and has not been published elsewhere, nor is it currently under consideration for publication by another journal.
With the submission of this manuscript we declare that:
• All authors of this research paper have directly participated in the planning, execution, or analysis of this study;
• All authors of this paper have read and approved the final version submitted;
• The contents of this manuscript have not been copyrighted or published previously;
• The contents of this manuscript are original and not now under consideration for publication elsewhere;
• The contents of this manuscript will not be copyrighted, submitted, or published elsewhere, while acceptance by the Journal is under consideration;
• There are no directly related manuscripts or abstracts, published or unpublished, by any authors of this paper;
• The manuscript has not been submitted to more than one journal for simultaneous consideration;
• The manuscript has not been published previously (partly or in full);
• No data have been fabricated or manipulated (including images) to support your conclusions;
• No data, text, or theories by others are presented as if they were the author’s own (“plagiarism”);
Rights and permissions
About this article
Cite this article
Hartmann, M., Blaszczynski, A. The Longitudinal Relationships Between Psychiatric Disorders and Gambling Disorders. Int J Ment Health Addiction 16, 16–44 (2018). https://doi.org/10.1007/s11469-016-9705-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-016-9705-z