Abstract
Diabetic nephropathy (DN) is one of the major microvascular complications in diabetes. Podocyte injury such as slit diaphragm effacement is regarded as a determinant in the occurrence and development of albuminuria in DN. In this study, we examined the effect of hyperoside, an active flavonoid glycoside, on proteinuria and renal damage in a streptozotocin-induced DN mouse model at the early stage. The results showed that oral administration of hyperoside (30 mg/kg/day for 4 weeks could significantly decrease urinary microalbumin excretion and glomerular hyperfiltration in DN mice, but did not affect the glucose and lipid metabolism. Periodic acid−Schiff staining and transmission electron microscopy showed that glomerular mesangial matrix expansion and podocyte process effacement in DN mice were significantly improved by hyperoside. Further investigations via immunofluorescence staining, real-time reverse transcription polymerase chain reaction and Western blot analysis showed that the decreased slit diaphragm protein nephrin and podocin mRNA expression and protein levels in DN mice were restored by hyperoside treatment. Collectively, these findings demonstrated that hyperoside could decrease albuminuria at the early stage of DN by ameliorating renal damage and podocyte injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic nephropathy (DN) occurs in 20–40 % of diabetes patients and is the leading cause of end-stage renal disease [1]. Persistent albuminuria in the range of 30–299 mg/24 h (microalbuminuria) is regarded as a marker for the onset of DN and can contribute to the development of DN [2]. Moreover, the level of microalbuminuria is also a well-established risk factor of cardiovascular disease in diabetes patients [3]. It is important to screen and treat the disease at the early stage. At the current time, despite intensive blood glucose control and the widespread use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, progression in the level of albuminuria in some DN patients is unavoidable [4, 5].
Accumulated studies suggest that podocyte injury plays a pivotal role in the occurrence of albuminuria and the pathogenesis of DN [6, 7]. Damage to the podocyte slit diaphragm results in the loss of maintaining the size-selective barrier in proteinuria disease [8]. The major slit diaphragm-associated proteins, nephrin and podocin, have been identified to be important determinants of glomerular permeability and play a significant role in the pathology of glomerular proteinuria [9, 10]. The low expression of nephrin and podocin mRNA and protein are an early event in DN patients and are closely linked to the development of proteinuria in both DN patients and animal models [11, 12]. A recent study demonstrated that maintenance of podocyte slit diaphragm proteins could improve podocyte injury and ameliorate proteinuria [13].
Hyperoside is a major active flavonoid glycoside in many medicinal plants which are commonly used in clinical practice in Traditional Chinese Medicine. Hyperoside has a therapeutic effect on several diseases such as cerebral ischemic reperfusion injury, neurotoxicity and hepatitis [14–17]. Recent studies suggested that hyperoside showed a therapeutic effect on inflammation in mice [18] and renal fibrosis in rats with unilateral ureteral obstruction [19]. Notably, hyperoside could downregulate the expression of receptor for advanced glycation end-products (RAGE) which plays an important role in the initiation of DN [20]. In addition, hyperoside could inhibit high glucose-induced vascular inflammation in vitro and in vivo [21]. Accumulated evidence suggests hyperoside could improve some diabetic vascular injury and complications.
In the present study, we aimed to investigate the possible therapeutic effect of hyperoside on proteinuria in a streptozotocin (STZ)-induced DN mice model. Furthermore, its effect on renal damage and podocyte injury was also explored to elucidate the underlying molecular mechanism.
Materials and methods
Reagents
Hyperoside (Fig. 4a) was purchased from Zelang Biological Technology Company (Nanjing, China) and was suspended in 1 % carboxymethyl cellulose (CMC) solution at different concentrations for the animal experiments.
Diabetic nephropathy model
Type 1 diabetes was induced by low-dose STZ injection as detailed by the Animal Models of Diabetic Complications Consortium protocol in National Institute of Diabetes and Digestive and Kidney Diseases [22]. Female C57BL6 mice aged 7–8 weeks received three intraperitoneal injections of STZ (Sigma, St Louis, MO, USA; 100 mg/kg body weight) dissolved in 10 mM sodium citrate (pH 5.5) every 48 h. Those with high blood glucose (13.9–22.2 mmol/l) were regarded as diabetic mice and their ratio of urinary microalbumin to creatinine (mAlb/Cr) was assayed every 2 weeks. Approximately 12 weeks after STZ treatment, the diabetic mice showed significant elevation of urinary mAlb/Cr compared with the non-diabetic mice. Mice that received the same volume of citrate buffer served as non-diabetic normal mice (control group). The diabetic mice with urinary mAlb/Cr (30–300 mg/g) were considered as DN mice. Immediately after the establishment of DN models, the mice were randomly divided into three groups—DN mice orally treated with CMC solution (DN group), and those receiving either a low or high dose of hyperoside (10 or 30 mg/kg once every day, respectively) for 4 weeks. Each of the groups, including the control group, comprised 10 mice. All mice were fed a standard laboratory diet and were provided with water ad libitum.
Experimental protocols
The experimental protocol was approved by the Animal Ethics Committee of Qingdao University. Blood glucose levels of the diabetic mice were monitored twice every week using the Bayer glucose monitor (Bayer, Bergkamen, Germany) and their urine was tested for ketone bodies. When necessary, the diabetic mice were given insulin treatment (Ultratard; Novo Nordisk, Denmark) at a dose of 1 IU/kg body weight (twice a week) to maintain blood glucose in the range of 13.9–22.2 mmol/l for preventing apparent exhaustion or ketosis during the experiment. Every 2 weeks after drug administration, individual 24-h urine sample collections were performed using metabolic cages.
Blood glucose was measured in tail vein blood and serum and urinary creatinine levels were measured by the enzymatic colorimetric method. Urinary albumin concentration was measured by Exocell kits using anti-mouse albumin antibody. Data were normalized to the urinary creatinine levels and expressed as urinary mAlb/Cr. Creatinine clearance (CCr) was calculated and expressed as ml/min/100 g body weight. Kidney weight was measured immediately after the animals were killed. Fresh kidney cortices were excised and stored at −80 °C until further analysis.
ELISA
The characterized AGE carboxymethyl-lysine (CML) (USCN Life Science Inc., Double Lake, MO, USA) in serum was measured by ELISA as in our previous study [23]. The intra-assay and the inter-assay coefficient of variation was 4.8–3.5 %, respectively (range 4.5–128.5 ng/ml). Serum angiotensin II and aldosterone were also measured by commercial ELISA kits (R&D, Wiesbaden, Germany) according to the manufacturer’s instructions.
Light and electron microscopic examination
Half of the rat kidney was fixed in 10 % formalin buffer and then embedded in paraffin for light microscopic observation. Three sections of 5 μm thickness (an interval of 100 μm) for every animal were chosen using an unbiased sampling method and stained by periodic acid−Schiff (PAS) reagent. Mesangial matrix expansion was determined by assessing PAS-positive material in the mesangial region excluding cellular elements [24, 25]. A percentage of the PAS-positive area was analyzed using Image-Pro Plus (Media Cybernetics, Silver Spring, MD, USA) and Leica Q500MC image analysis software. Semi-quantitative analysis was performed with 50 glomeruli randomly selected fields for each subject (at least five mice in each group) and evaluations were made by a blinded investigator.
For ultrastructural evaluation, the renal cortex was cut into small pieces and prefixed with 2.5 % glutaraldehyde (pH 7.4) for 4 h, then postfixed in 1 % buffered sodium tetroxide for 1 h and embedded in Epon 812. Ultra-thin sections were stained with lead citrate/uranyl acetate and examined under a JEM-1010 EX transmission electron microscope. Three samples were selected from every kidney and each with five electron micrographs at ×25,000 magnification. Five glomeruli in every electron micrograph were randomly selected for further measurement. Image-Pro Plus software was utilized to measure the mean glomerular basement membrane (GBM) thickness at three different cross section sites.
Immunofluorescence
Immunofluorescence staining for nephrin and podocin was performed using frozen kidney sections. Sections (5 μm) were fixed in acetone and blocked with 10 % bovine serum albumin (BSA) before overnight incubation with polyclonal rabbit anti-mouse nephrin or podocin antibody (Abcam Ltd, Cambridge, MA, USA) at a concentration of 1:1000. After washing in PBS (5 min × 3 times), the sections were stained with fluorescein isothiocyanate conjugated anti-rabbit IgG secondary antibodies for 60 min at room temperature. After washing in PBS (5 min × 3 times), sections were observed by a fluorescence microscope (LSM-510, Carl Zeiss, Germany). The immunoreactivity of nephrin and podocin was quantified by the color images obtained as TIF files. The brightness of each image file was inverted to gray-scale mode by Photoshop software (Adobe Systems, San Jose, CA, USA) and analyzed by National Institute of Health (NIH) Image software. The nephrin and podocin indexes were calculated using the following formula: [X (density) × positive area (μm2)]/glomerular total area (μm2), where the staining density is indicated by a number from 0−256 in gray-scale.
Real-time reverse transcriptase polymerase chain reaction (RT-PCR)
Total RNA was isolated from kidney cortices or cultured cells using Trizol reagent according to the manufacturer’s directions (Qiagen, San Diego, CA, USA). RNA (1 μg) was reverse transcribed into cDNA using Oligo-dT priming and superscript reverse transcriptase (Promega Corporation, Madison, WI). Target gene expression was quantified by real-time PCR using SYBR® Green Supermix and the ABI Real-Time PCR Reaction System (Bio-Rad Laboratories). PCR conditions were as follows—denaturation at 95 °C for 3 min, followed by 40 cycles of 95 °C for 15 s, 57 °C for 30 s, and 72 °C for 30 s and finally elongation at 72 °C for 10 min. Mouse nephrin primers: 5′-TCACTACCCCAGGTCTCCAC-3′ (forward) and 5′-CCCTGCCTCTGTCTTCTCTG-3′ (reverse). Mouse podocin primers: 5′-GAAAGGAAGAG ATTGCCCAAG-3′ (forward) and 5′-TGTGGACAGCGACTGAAGAGTGTG-3′ (reverse). Expression of the housekeeping gene β-actin was used to quantify nephrin and podocin expression by the delta–delta cycle time (Ct) method. Mouse housekeeping gene β-actin primers: 5′-AGTGTGACGTTGACATCCGTA-3′ (forward) and 5′-GCCAGAGCAGTAATCTCCTTCT-3′ (reverse). Four independent experiments were performed.
Western blot
The mouse kidney cortices were homogenized in radioimmunoprecipitation assay buffer at 4 °C. After centrifugation at 15,000 rpm for 30 min at 4 °C, supernatant was collected and stored at −80 °C until measurement. Total protein concentration was determined using the Pierce BCA Protein Assay Kit (Thermo Scientific, Rockford, IL, USA) using BSA as the standard. Samples were processed for SDS-PAGE and 30 μg protein obtained from kidney cortex was loaded in each lane. Proteins were electrotransferred onto nitrocellulose membrane (Hybond ECL, Amersham). The membranes were blocked with 5 % defatted milk powder in 1× TBS (0.1 % Tween-20) for 30 min and incubated overnight with polyclonal rabbit anti-mouse nephrin or podocin antibody (Abcam) at a dilution of 1:2,000 at 4 °C. After incubation with horseradish peroxidase labeled secondary antibodies for 60 min, signals were detected with an enhanced chemiluminescence (ECL) kit (Promega). Membranes were incubated with rabbit polyclonal anti-β-actin antibodies (Cell Signaling Technology, USA) to serve as controls for equal loading. The density of nephrin or podocin in each band was determined using NIH Image software and expressed as a relative value to the density of the corresponding band β-actin immunoblot.
Statistical analysis
All results were expressed as mean ± standard error (SE) and analyzed by Graphpad Prism 6.0 software (San Diego, CA, USA). One-way ANOVA with a one-tailed Student’s t test was used to identify significant differences in multiple comparisons. The post hoc comparisons using the Student−Newman–Keuls test were used for inter-group comparisons of multiple variables. A probability of P < 0.05 was considered to be statistically significant.
Results
Hyperoside treatment could ameliorate albuminuria and kidney function in DN mice
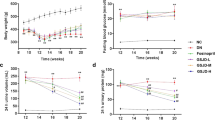
To evaluate the effect of hyperoside on albuminuria and hyperfiltration status in STZ-induced DN mice, we measured urinary mAlb/Cr, 24-h urinary total protein (24 h-UTP) and CCr. Compared with the control group, treatment with hyperoside at a higher dose (30 mg/kg/day) for 4 weeks resulted in a significant suppression of increased urinary mAlb/Cr, 24 h-UTP and CCr in DN mice (Fig. 1a–c). DN mice exhibited a significant increase in kidney/body weight ratio compared with non-diabetic mice. Unexpectedly there was no difference in kidney/body weight ratio between hyperoside- and vehicle-treated DN mice (Fig. 1d). Moreover, blood pressure, plasma glucose and lipid metabolic parameters, CML-AGE, plasma angiotensin II and aldosterone were also measured and analyzed in the four groups. The data showed that hyperoside (10 or 30 mg/kg/day) administration for 4 weeks had no significant effect on blood pressure and blood biochemical indexes in DN mice (Table 1).
Hyperoside ameliorated proteinuria and impairment of kidney function in DN mice (n = 10). a–c Urinary mAlb/Cr, 24 h-UTP and creatinine clearance (CCr) were measured 4 weeks after hyperoside treatment. d Kidney/body weight ratio was determined before termination of the experiments. Control non-diabetic normal mice; DN diabetic nephropathy (mice were treated with vehicle CMC solution); LHPS and HHPS DN mice treated with 10 or 30 mg/kg/day of hyperoside, respectively. Data are presented as mean ± SE. P < 0.05 is statistically significant. aIndicates significant vs control, bIndicates significant vs DN
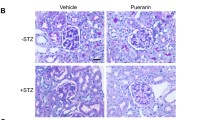
Hyperoside treatment could improve renal morphological abnormalities in DN mice
PAS staining was used to represent renal expanded mesangial regions in light microscopic appearance. Hyperoside treatment (30 mg/kg/day) for 4 weeks could significantly inhibit renal mesangial expansion and extracellular matrix accumulation observed in DN mice (Fig. 2a, b). Glomerular ultrastructural changes were assessed by transmission electron microscopy. In contrast with non-diabetic mice, decreased podocyte foot processes and widely fused podocytes (Fig. 2c, d) were observed in DN mice. Treatment with hyperoside (30 mg/kg/day) for 4 weeks could significantly improve those renal morphological abnormalities in DN mice.
Hyperoside attenuated renal mesangial expansion and foot process effacement in DN mice (n = 6). a Light microscopy of renal mesangial regions stained by PAS. b Quantification of PAS staining was shown by PAS staining score. c Widely fused podocytes and decreased foot process number were observed by transmission electron microscopy (×25,000 magnification). d Semiquantitative analysis of foot process number on GBM was assessed in subtus columns. Data are presented as mean ± SE. P < 0.05 is statistically significant. aIndicates significant vs control, bIndicates significant vs DN
Hyperoside treatment could restore decreased nephrin and podocin immunoreactivity in DN mice
The immunoreactivity of podocyte slit diagram proteins, nephrin and podocin, was mainly distributed in a linear pattern along the glomerular capillaries of the glomerular basement membrane in DN mice. The amount of glomerular nephrin and podocin positive area was decreased in the DN group in comparison with non-diabetic mice in the control group (P < 0.05). Hyperoside (30 mg/kg/day) showed a significant protective effect on decreased glomerular nephrin and podocin immunoreactivity in DN mice compared with the vehicle solution after 4 weeks of treatment (Fig. 3a, b).
Hyperoside restored decreased glomerular nephrin and podocin expression in DN mice. a–b Immunoreactivity of nephrin and podocin was determined by immunofluorescence staining. The columns quantified the amount of immunoreactive nephrin and podocin determined by NIH Image software in gray-scale mode (n = 6). c–d Expression of nephrin and podocin mRNA detected by real-time RT-PCR; the columns show the amount of nephrin mRNA relative to β-actin. Data are presented as mean ± SE. P < 0.05 is statistically significant. aIndicates significant vs control, bIndicates significant vs DN
Hyperoside treatment could restore decreased nephrin and podocin expression in DN mice
The renal cortex which mainly contains glomerulus was carefully dissected for real-time PCR and Western blotting. The data showed that nephrin and podocin mRNA expression in renal cortex was dramatically decreased compared with the control group (P < 0.05). Hyperoside (30 mg/kg/day) for 4 weeks could restore the decreased nephrin and podocin mRNA levels in DN mice (Fig. 3c, d). Western blot analysis also showed decreased nephrin and podocin protein levels were enhanced with hyperoside treatment in DN mice (Fig. 4b–d), which is inconsistent with the results from immunofluorescence staining and real-time PCR analysis.
a The chemical structural formula of hyperoside. b–d Expression of nephrin and podocin protein expression detected by Western blot analysis; the columns show the amount of nephrin protein levels relative to β-actin. Data are presented as mean ± SE. P < 0.05 is statistically significant. aIndicates significant vs control, bIndicates significant vs DN
Discussion
Proteinuria is the clinical hallmark of the onset and development of DN [1, 26]. The early loss of glomerular permeability selectivity plays a pivotal role in the pathogenesis for microalbuminuria of DN [26]. Podocytes are glomerular inherent cells with high differentiation and limited dividing ability [6]. The central role of the podocyte slit diaphragm in maintaining the size-selective barrier has been verified by accumulating studies on mutiple slit diaphragm-associated proteins such as nephrin, podocin and CD2-associated protein [27]. Mutations in the nephrin gene could result in marked proteinuria in patients with congenital nephrotic syndrome of the Finnish type [28]. The correlation between slit diaphragm protein impairment and proteinuria has been indicated in DN patients and animals [11, 12, 29]. Moreover, nephrin has recently been essential for insulin responsiveness of podocytes [30]. The effacement of podocyte nephrin and podocin in DN was regarded as an early morphologic marker for podocyte injury and potential therapeutic target.
As an active flavonoid glycoside in many medicinal plants, hyperoside is known for its potential anti-inflammatory effect especially on high glucose-induced inflammation [18, 21]. Recent studies suggested that hyperoside might have a therapeutic effect on diabetic vascular injury and diabetic complications [18, 21]. Our present study showed that oral administration of hyperoside (30 mg/kg/day) for 4 weeks could significantly ameliorate urinary albumin excretion (urinary mAlb/Cr and 24 h-UTP) in DN mice at its early stage. Although the increased kidney/body weight ratio was not improved, hyperoside (30 mg/kg/day) for 4 weeks could suppress the elevated CCr of DN mice, suggesting that it could reverse increased glomerular hyperfiltration in DN mice. This therapeutic effect of hyperoside was probably not due to metabolic improvement because the glucose and lipid metabolic factors showed no significant change such as blood glucose, TC, TG, LDL, HbA1c and the characterized CML-AGE. Although blood pressure, serum angiotensin II and aldosterone levels did not show a significant difference, we could not absolutely exclude the possible role of the improvement of hemodynamic factors. PAS staining showed that renal mesangial expansion and extracellular matrix accumulation could be significantly inhibited by hyperoside treatment. Furthermore, the morphologic observations by electron microscopy showed that hyperoside could also improve podocyte foot process effacement in DN mice. Together, our data indicated that hyperoside has a comprehensive protective effect on the renal structural abnormalities of the diabetic kidney.
The alteration in podocyte slit diaphragm protein expression is an early event in DN. Our study showed podocyte slit diaphragm molecule nephrin and podocin mRNA and protein expression were significantly decreased in DN mice when compared with the control, which is consistent with previous observations [11, 12, 29]. Either immunofluorescence staining or mRNA and protein analysis suggested that the decreased renal nephrin and podocin expression in DN mice was significantly restored by hyperoside at dose of 30 mg/kg/day for 4 weeks. Hyperoside might have a protective effect on podocyte slit diagram dysfunction by upregulating nephrin and podocin expression and/or decreasing their impairment. Due to the importance of nephrin and podocin in podocyte slit diaphragm, their reduction was taken as a determinant of glomerular hyperpermeability in DN status. The preservation of nephrin and podocin expression by hyperoside treatment might be associated with improved urinary microalbumin excretion in the DN model.
A recent pharmacokinetic study suggested that unbound hyperoside existed in rat blood circulation and kidney after oral administration [31], indicating that the effect of hyperoside depends on its original type, not its metabolites. To clarify the protective effect of hyperoside on diabetes-related podocyte injury and decipher the detailed molecular mechanisms, we need to further investigate its effect on nephrin and podocin expression in cultured podocytes under diabetes-related stimulus in future work.
Conclusions
In summary, our study provided the first experimental evidence of the therapeutic effect of hyperoside on albuminuria and renal injury in DN mice at the early stage. Hyperoside could protect podocyte slit diagram effacement by restoring podocyte nephrin and podocin maintenance, which might be involved in its therapeutic mechanisms.
References
Gross JL, de Azevedo MJ, Silveiro SP et al (2005) Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care 28:164–176
Wada T, Shimizu M, Toyama T et al (2012) Clinical impact of albuminuria in diabetic nephropathy. Clin Exp Nephrol 16:96–101
Klausen K, Borch-Johnsen K, Feldt-Rasmussen B et al (2004) Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation 110:32–35
Coca SG, Ismail-Beigi F, Haq N et al (2012) Role of intensive glucose control in development of renal end points in type 2 diabetes mellitus: systematic review and meta-analysis intensive glucose control in type 2 diabetes. Arch Intern Med 172:761–769
Vejakama P, Thakkinstian A, Lertrattananon D et al (2012) Reno-protective effects of renin-angiotensin system blockade in type 2 diabetic patients: a systematic review and network meta-analysis. Diabetologia 55:566–578
Wolf G, Chen S, Ziyadeh FN (2005) From the periphery of the glomerular capillary wall toward the center of disease: podocyte injury comes of age in diabetic nephropathy. Diabetes 54:1626–1634
Cao Z, Cooper ME (2011) Pathogenesis of diabetic nephropathy. J Diabetes Investig 2:243–247
Tryggvason K, Wartiovaara J (2001) Molecular basis of glomerular permselectivity. Curr Opin Nephrol Hypertens 10:543–549
Liu G, Kaw B, Kurfis J et al (2003) Neph1 and nephrin interaction in the slit diaphragm is an important determinant of glomerular permeability. J Clin Investig 112:209–221
Zhang A, Huang S (2012) Progress in pathogenesis of proteinuria. Int J Nephrol 2012:314251. doi:10.1155/2012/314251
Toyoda M, Suzuki D, Umezono T et al (2004) Expression of human nephrin mRNA in diabetic nephropathy. Nephrol Dial Transplant 19:380–385
Doublier S, Salvidio G, Lupia E et al (2003) Nephrin expression is reduced in human diabetic nephropathy: evidence for a distinct role for glycated albumin and angiotensin II. Diabetes 52:1023–1030
Eto N, Wada T, Inagi R et al (2007) Podocyte protection by darbepoetin: preservation of the cytoskeleton and nephrin expression. Kidney Int 72:455–463
Li ZL, Hu J, Li YL et al (2013) The effect of hyperoside on the functional recovery of the ischemic/reperfused isolated rat heart: potential involvement of the extracellular signal-regulated kinase 1/2 signaling pathway. Free Radic Biol Med 57:132–140
Zeng KW, Wang XM, Ko H et al (2011) Hyperoside protects primary rat cortical neurons from neurotoxicity induced by amyloid beta-protein via the PI3 K/Akt/Bad/Bcl(XL)-regulated mitochondrial apoptotic pathway. Eur J Pharmacol 672:45–55
Li ZL, Liu JC, Hu J et al (2012) Protective effects of hyperoside against human umbilical vein endothelial cell damage induced by hydrogen peroxide. J Ethnopharmacol 139:388–394
Wu LL, Yang XB, Huang ZM et al (2007) In vivo and in vitro antiviral activity of hyperoside extracted from Abelmoschus manihot (L) medik. Acta Pharmacol Sin 28:404–409
Ku SK, Zhou W, Lee W, et al. (2014) Anti-Inflammatory effects of hyperoside in human endothelial cells and in mice. Inflammation 38:784–799
Yan Y, Feng Y, Li W et al (2014) Protective effects of quercetin and hyperoside on renal fibrosis in rats with unilateral ureteral obstruction. Exp Ther Med 8:727–730
Zhang Z, Sethiel MS, Shen W et al (2013) Hyperoside downregulates the receptor for advanced glycation end products (RAGE) and promotes proliferation in ECV304 cells via the c-Jun N-terminal kinases (JNK) pathway following stimulation by advanced glycation end-products in vitro. Int J Mol Sci 14:22697–22707
Ku SK, Kwak S, Kwon OJ et al (2014) Hyperoside inhibits high-glucose-induced vascular inflammation in vitro and in vivo. Inflammation 37:1389–1400
Brosius FC 3rd, Alpers CE, Bottinger EP et al (2009) Mouse models of diabetic nephropathy. J Am Soc Nephrol 20:2503–2512
An XF, Zhao Y, Yu JY et al (2010) Plasma sRAGE is independently associated with high sensitivity C-reactive protein in type 2 diabetes without coronary artery disease. Diabetes Res Clin Pract 87:e19–e22
Alsaad KO, Herzenberg AM (2007) Distinguishing diabetic nephropathy from other causes of glomerulosclerosis: an update. J Clin Pathol 60:18–26
Sugimoto H, Grahovac G, Zeisberg M et al (2007) Renal fibrosis and glomerulosclerosis in a new mouse model of diabetic nephropathy and its regression by bone morphogenic protein-7 and advanced glycation end product inhibitors. Diabetes 56:1825–1833
Jefferson JA, Shankland SJ, Pichler RH (2008) Proteinuria in diabetic kidney disease: a mechanistic viewpoint. Kidney Int 74:22–36
Patari-Sampo A, Ihalmo P, Holthofer H (2006) Molecular basis of the glomerular filtration: nephrin and the emerging protein complex at the podocyte slit diaphragm. Ann Med 38:483–492
Lenkkeri U, Mannikko M, McCready P et al (1999) Structure of the gene for congenital nephrotic syndrome of the finnish type (NPHS1) and characterization of mutations. Am J Hum Genet 64:51–61
Aaltonen P, Luimula P, Astrom E et al (2001) Changes in the expression of nephrin gene and protein in experimental diabetic nephropathy. Lab Investig 81:1185–1190
Coward RJ, Welsh GI, Koziell A et al (2007) Nephrin is critical for the action of insulin on human glomerular podocytes. Diabetes 56:1127–1135
Xue C, Guo J, Qian D et al (2011) Identification of the potential active components of Abelmoschus manihot in rat blood and kidney tissue by microdialysis combined with ultra-performance liquid chromatography/quadrupole time-of-flight mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 879:317–325
Acknowledgments
This study is supported by Shandong Province Natural Science Foundation (ZR2014CM040) and Jiangsu Province Natural Science Foundation (BK20141503).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interest
All the authors have no potential conflicts of interest to declare.
Additional information
J. Zhang and H. Fu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, J., Fu, H., Xu, Y. et al. Hyperoside reduces albuminuria in diabetic nephropathy at the early stage through ameliorating renal damage and podocyte injury. J Nat Med 70, 740–748 (2016). https://doi.org/10.1007/s11418-016-1007-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11418-016-1007-z