Abstract
While mitochondria are susceptible to environmental detriments, little is known about potential associations between arsenic metabolites and mitochondria DNA copy number (mtDNAcn). We attempted to examine whether maternal urinary arsenic metabolite levels in different trimesters were related to neonatal cord blood mtDNAcn. We included 819 mother-newborn pairs embedded in an in-progress birth cohort survey performed from April 2014 to October 2016 in Wuhan, China. We determined maternal urinary arsenic species concentrations in different trimesters. We determined cord blood mtDNAcn using quantitative real-time polymerase chain reaction. In covariate-adjusted models, each one-unit increment of dimethylated arsenic (DMA) and total arsenic (TAs) in the third trimester was related to 8.43% (95% CI 1.13%, 16.26%) and 12.15% (95% CI 4.35%, 20.53%) increases in mtDNAcn, respectively. The dose–response trend with statistical significance was observed across tertiles of DMA and TAs in the third trimester with mtDNAcn (DMA percent changes (%Δ) = 25.60 (95% CI 6.73, 47.82), for the highest vs the lowest tertile (P = 0.02); TAs %Δ = 40.31 (95% CI 19.25, 65.10), for the highest vs the lowest tertile (P = 0.0002)). These findings may prove the relationships between prenatal arsenic species levels and neonatal mitochondrial dysfunction.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arsenic widely occurs in nature, existing in organic and inorganic forms. Inorganic arsenic (iAs) is generally considered more toxic than organic forms. The World Health Organization has reported that iAs in the groundwater exists at high concentrations (> 10 µg/L) in many countries, including Bangladesh, some areas of China (such as Datong and Yuncheng basins in Shanxi, Hetao basin in Inner Mongolia, and Guitun area in Xinjiang), India, Chile, and Mexico (Ravenscroft et al. 2009). Dietary intake has become an essential source of arsenic exposure because of its accumulation in rice, fish, and dairy products (Chain EPoCitF 2009). People from the USA and some European countries have been reported to be exposed to arsenic at levels up to 300 µg/day via food and beverages (European Food Safety 2014; Kurzius-Spencer et al. 2014). iAs could be methylated to organic forms recognized as monomethylated arsenic (MMA) and dimethylated arsenic (DMA). More highly methylated arsenicals could be excreted more readily through the urine, decreasing retention and decreased biological exposure and toxicity (Vahter 2002). The urinary arsenic levels could reflect the recently individual iAs absorbed dose, and iAs methylation indices, which could be pretty stable for 810 months, were considered valuable markers for ongoing ingestion iAs (Steinmaus et al. 2005). Nevertheless, the idea has received a challenge considering that methylated trivalent arsenic showed more toxicity than the inorganic form (Stýblo et al. 2002). Arsenic species could cross the placenta (Concha et al. 1998; Hall et al. 2007), resulting in newborns’ susceptibility to arsenic exposure (Farzan et al. 2013). Existing epidemiologic research has revealed that earlylife exposure to arsenic species was linked to unfavorable birth consequences [(e.g., low birth weight (LBW), preterm birth (PTB) (Gilbert-Diamond et al. 2016; Laine Jessica et al. 2015), poorer neurobehavioral performance and development of newborns (Chen et al. 2023; Liang et al. 2020; Soler-Blasco et al. 2022)]) and disease later in life (Chen et al. 2019; Steinmaus et al. 2016). Toxicological evidence demonstrates that exposure to inorganic (Huang et al. 2018; Rodriguez Karina et al. 2016; Rodriguez et al. 2020) and methylated arsenicals (Negro Silva Luis et al. 2017, 2021) could lead to adverse offspring health.
Mitochondria, an essential ingredient of eukaryotic cells, plays a prominent role in many biological processes, like reactive oxygen species (ROS) production, apoptosis, and lipid metabolism (Shadel and Horvath 2015, Wai and Langer 2016). Mitochondria’s vulnerability to environmental toxicants might be partially ascribed to its proximity to ROS (Dan Dunn et al. 2015), inadequate repair capacity, deficiency in noncoding introns, and lack of defensive histones (Malik and Czajka 2013). Nevertheless, mitochondria could compensate for genomic insults by modifying their abundance, ultimately altering mitochondrial DNA copy number (mtDNAcn) (Lee and Wei 2000). Generally, mtDNAcn, reflecting the number of copies of the mitochondrial genome per nucleated cell, is a hopeful marker of mitochondrial malfunction (Malik and Czajka 2013). Despite the variation in mtDNAcn among various cell types, mtDNAcn in specific tissues/cells could remain unchangeable due to its rigorous modulation. Accumulating epidemiological studies have associated unexpected mtDNAcn variation from oxidative stress or inflammation with chronic diseases (Hägg et al. 2021). Moreover, studies have demonstrated that mtDNAcn is related to both birth weight and gestational age and is even one of the putative links between poor fetal growth and cardiovascular complications in later life (Gemma et al. 2006; Pejznochová et al. 2008). Recently, mtDNAcn has been proposed as a potential mechanism linking environmental pollutant exposure and reduced birth weight (Barrett Julia 2016). Therefore, identifying the determinants of mtDNAcn may provide more insights into poor fetal growth and aging-related disease. Recent epidemiological studies have elucidated if arsenic exposure alters mtDNAcn in individuals with different arsenic metabolizing capacity (Ameer et al. 2016; De Loma et al. 2022), which reported that arsenic exposure was associated with increased mtDNAcn, particularly in individuals with less-efficient arsenic metabolism. However, the previous research focused on cross-sectional associations of relatively high levels of arsenic exposure with mtDNAcn among occupational workers and residents of arsenic-contaminated areas, with relatively small samples. Owing to the cross-sectional study design, the critical window of susceptibility to arsenic metabolites is still unknown.
Accordingly, we conducted this study to reveal the relationship between maternal arsenic metabolites concentrations based on repeated measurements and cord blood mtDNAcn in the Chinese population and to identify the critical window of heightened susceptibility to prenatal arsenic metabolite exposure.
Methods
Study population
The analysis population is a subset of the Wuhan Healthy Baby Cohort that has enrolled pregnancies at the first prenatal examination (gestational week less than 16) from 2012 to 2019. Eligibility criteria included fluency in Chinese, singleton pregnancy, and intent to reside in Wuhan throughout gestation. Participants were included in the present analysis if they had available data on (1) maternal urinary arsenic metabolites concentrations and (2) neonatal cord blood mtDNAcn. The present analysis was restricted to 828 mothers recruited between April 2014 and October 2016. We further excluded four women with outliers or missing data on urinary arsenic metabolites concentrations and five women without demographic or clinic information data, leaving 819 pregnant women for this analysis.
Informed written consent was acquired from all participators at recruitment. The Huazhong University of Science Institutional review boards have authorized the research procedures.
Urine acquisition and arsenic metabolite quantification
The periods of maternal urine sample collection at each trimester were at 12–16, 22–26, and 32–36 gestational weeks, respectively. Each participant was required to provide their spot urine sample when they received prenatal care service. The urine samples from the participants were gathered into metal-free polypropylene containers and stored at − 20 °C until further analysis. The average gestational ages (mean ± standard deviation [SD]) of urine collection for the first, second, and third trimesters were 13.0, 24.0, and 33.3 weeks, respectively. The sample size for each trimester was 815, 812, and 816, respectively. Details of urinary arsenic metabolite quantification are depicted elsewhere (Wang et al. 2021). In short, midstream spot urine samples were gathered during scheduled antenatal visits and stored at − 20 °C. Arsenic species were quantified by isotope dilution high-performance liquid chromatography coupled with quadrupole inductively coupled plasma mass spectrometer (HPLC–ICPMS), including arsenobetaine (AsB), arsenite (As3+), arsenate (As5+), MMA, and DMA. Information about quality assurance, including limits of detections (LODs), limits of quantifications (LOQs), and intra-day and inter-day coefficients of variation, is the same as that published by Wang et al. (2021). Specific gravity (SG) was determined to standardize the urinary arsenic species levels.
Relative mtDNAcn measurement
Venous umbilical cord blood was collected in vacutainer tubes containing EDTA immediately after delivery. Before analysis, blood samples were reserved at − 80 °C. Relative mtDNAcn measurement was carried out according to a prior described method (Janssen Bram et al. 2012). Information about detailed procedures of quantitative real-time polymerase chain reaction (PCR) is presented in the supporting materials.
Covariates
Maternal demographic data (e.g., maternal age, family annual income, education levels, passive smoking, and folic acid intake) were collected by trained personnel via semi-structured questionnaires. In addition, data on pregnancy (e.g., parity, neonate gender, and pregnancy complications) was retrieved from the medical records. Information about the classification of pre-pregnancy body mass index (BMI) is shown in Supplementary Methods. Secondhand smoke exposure throughout gestation was defined as passive smoke.
Statistical analysis
Continuous variables were expressed as mean ± SD, whereas categorical variables were expressed as counts (percentage). Arsenic metabolite levels lower than the LOD were replaced with LOD/√2. We used SG to adjust for the dilution to correct urine dilution, which might potentially affect the association of arsenic metabolites with mtDNAcn. The formula of SG normalization is exhibited in the Supplementary Methods.
Urinary arsenic metabolite levels and relative mtDNAcn were log2-transformed to alleviate the skewed distribution. Reproducibility of urinary arsenic metabolite concentrations across three pregnancy trimesters as well as any two trimesters was evaluated by the intraclass correlation coefficient (ICC), which was defined as a ratio of the between-person variance to the sum of within- and between-person variances (Rosner 2011). We averaged the SG-adjusted arsenic metabolite levels in different trimesters to generate individual-specific averages throughout gestation—arsenic metabolites. Details about arsenic exposure indices are shown in the Supplementary Methods.
Potential nonlinear associations between arsenic species and cord blood mtDNAcn were examined using 3-knot restricted cubic splines. Except for iAs and mtDNAcn (P = 0.008), linear relationships were observed between DMA, MMA, TAs, and mtDNAcn (P > 0.05). Thus, a general linear model was performed to examine the potential connection of individual-specific arsenic metabolite averages (continuous and in tertiles) across three trimesters with cord blood mtDNAcn. Also, generalized estimating equations (GEEs) were performed to assess the relationships of trimester-specific exposures (both continuous and in tertiles) with mtDNAcn (Sánchez Brisa et al. 2011). Tertile cut-points originated from trimester-specific determination, and we defined the lowest tertile as the reference. In addition, we modeled the median value of every tertile to determine the linear trends of these relationships. We converted beta (β) into percent change (%Δ) of exposures to make the statistical models more interpretable (Barrera-Gómez and Basagaña, 2015). Covariates considered for inclusion were those changed estimates (≥ 10%) in the relationships or those observed to be linked to mtDNAcn in previous studies were based on previous studies. The following variables were included as covariables: maternal age at enrollment, gestational age (weeks), pre-pregnancy BMI (< 18.5, 18.5–23.9, ≥ 24 kg/m2), parity history (nulliparous or not), infant sex (male or not), education level (< 9, 9–12, ≥ 12 years), passive smoking during pregnancy (yes or no), gestational diabetes mellitus (yes or not), and gestational hypertension disorders (yes or not).
To test the robustness of our results, we completed additional analyses by excluding participants with PTB, LBW, gestational diabetes, or hypertensive disorders. Software SAS (version 9.4, Institute Inc., USA) was used.
Results
Characteristics
Table 1 exhibits the characteristics of the mother-newborn pairs. The mean maternal age at enrollment was 28.94 years. Approximately 68.74% of participating women had a normal pre-pregnancy weight, with an average pre-pregnancy BMI of 20.99 kg/m2. Of the mothers in the analysis sample, 27.11% of women reported exposure to secondhand smoke, 88.03% acquired a college education or above, and 80.59% were primiparous. The proportion of gestational diabetes and hypertension disorders was 8.06% and 2.93%, respectively. For newborns, 53.60% were male, and 3.42% were born preterm.
Distribution of maternal urinary arsenic parameters
Supplementary Table 1 exhibits the concentration profiles of the targets. The target analytes were detected with detection frequencies ranging from 64.2 to 98.7%. The median concentrations of maternal SG-normalized urinary DMA were 8.21, 7.72, and 7.93 µg/L, MMA were 1.10, 1.07, and 1.06 µg/L, iAs were 3.18, 3.66, and 3.82 µg/L, and the TAs were 13.58, 13.59, 13.49 µg/L in the first, second and third trimester, respectively. Throughout the pregnancy, the ICCs of SG-normalized arsenic metabolites varied from 0.17 to 0.39, indicating poor reproducibility of urinary arsenic species across pregnancy (Supplementary Table 2).
Relationships of maternal arsenic exposure with cord blood mtDNAcn
Figure 1 lists the relationships of average levels of individual arsenic metabolites across three trimesters with the cord blood mtDNAcn alternation (Supplementary Table 3). In crude models, one double increase in DMA and TA levels was related to an 8.56% (95% CI 0.60, 17.16) and 15.94% (95% CI 5.72, 27.14) increase in cord blood mtDNAcn, respectively. In adjusted models, the relationships of maternal DMA and TA levels with cord blood mtDNAcn were still statistically significant (percent difference 9.22%, 95% CI 1.11, 17.98; percent difference 17.21%, 95% CI 6.70, 28.76). Additionally, the highest tertile of DMA concentrations was significantly linked to an approximately 23.97% (95% CI 5.35, 45.89) increment in mtDNAcn compared with the lowest tertile. Moreover, a 35.14% increase of cord blood mtDNAcn was found in the highest tertile of TAs concentration, compared with the lowest tertile (percent difference 35.14%, 95% CI 14.80, 59.10). In the dose–response trend analysis, the positive association between TA level and mtDNAcn remained significant (p trend = 0.0423), yet there was not a remarkable relationship between DMA and mtDNAcn (p trend = 0.0854). Sensitivity analyses did not markedly alter our results (Supplementary Table 4).
Associations of average maternal arsenic concentrations with cord blood mtDNAcn (data correspond to Supplementary Table 3). Models were adjusted for maternal age at enrollment, gestational age, pre-pregnancy BMI, parity history, infant sex, education level, passive smoking during pregnancy, hypertensive disorders in pregnancy, and gestational diabetes mellitus. Abbreviations: CI, confidence interval; DMA, dimethylarsinic acid; MMA, monomethylarsonic acid; iAs, inorganic As, sum of As3 + , As5 + ; TAs, Total As, sum of DMA, MMA, and iAs; %DMA, percentage of dimethylarsinic acid; %MMA, percentage of monomethylarsonic acid; %iAs, percentage of inorganic As; PMI, primary methylation index (MMA/iAs); SMI, secondary methylation index (DMA/MMA); TMI, total methylation index, (MMA + DMA)/iAs. The percentages of each metabolite were calculated: levels of the metabolite/(DMA + MMA + iAs) × 100
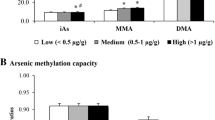
Figure 2 (Supplementary Table 5) exhibits the relationships of trimester-specific arsenic metabolite concentrations with cord blood mtDNAcn. In adjusted models, each twofold increment of DMA, iAs, and TAs in the third trimester was associated with 8.43% (95% CI 1.13%, 16.26%), 3.94% (95% CI 0.10%, 7.94%), and 12.15% (95% CI 4.35%, 20.53%) increases in mtDNAcn, respectively. Cord blood mtDNAcn increased across increasing tertiles of urinary DMA, iAs, and TAs levels in the third trimester. The observed associations in sensitivity analyses did not change compared with the primary study results (Supplementary Table 6).
Trimester-specific associations between prenatal arsenic exposure and cord blood mtDNAcn (data correspond to Supplementary Table 5). Models were adjusted for maternal age at enrollment, gestational age, pre-pregnancy BMI, parity history, infant sex, education level, passive smoking during pregnancy, hypertensive disorders in pregnancy, and gestational diabetes mellitus. Abbreviations: CI, confidence interval; DMA, dimethylarsinic acid; MMA, monomethylarsonic acid; iAs, inorganic As, sum of As3+, As.5+; TAs, Total As, sum of DMA, MMA, and iAs; %DMA, percentage of dimethylarsinic acid; %MMA, percentage of monomethylarsonic acid; %iAs, percentage of inorganic As; PMI, primary methylation index (MMA/iAs); SMI, secondary methylation index (DMA/MMA); TMI, total methylation index, (MMA + DMA)/iAs. The percentages of each metabolite were calculated: levels of the metabolite / (DMA + MMA + iAs) × 100
Discussion
In this birth cohort study, we demonstrated that prenatal exposure to DMA and TAs during the third trimester, rather than during the first or second trimesters, was positively associated with cord blood leukocyte mtDNAcn. This association persisted even after adjustment for potential confounders.
Arsenic widely exists on the earth, leading to the risk of environmental exposure. It can be converted to MMA and DMA in humans, and urinary arsenic species are acknowledged as a marker of arsenic exposure (Hayakawa et al. 2005). The urinary arsenic speciation levels in this study were lower than those in Mexico (median of DMA, MMA, and TAs were 20.6, 1.4, and 23.3 µg/L, respectively) (Laine Jessica et al. 2015) and Pabna (medians of DMA, MMA, and TAs were 50.2, 3.4, and 63.2 µg/L) pregnant women (Gao et al. 2019). Additionally, the urinary arsenic speciation levels in this study were higher than those of pregnant women in the INMA Project (geometric means [GM] of DMA, MMA, and iAs were 5.54, 0.28, and 0.27 µg/L, respectively) (Soler-Blasco et al. 2021), Oklahoma City (GM of DMA, MMA, iAs, and TAs were 3.93, < LOD, 1.36, and 4.46 µg/L, respectively) (Chen et al. 2021), the PHIME-CROME project (GM of DMA, MMA, and TAs were 2.67, 0.17, and 3.23 μg/L, respectively) (Stajnko et al. 2019), and the MADRES study (medians of DMA, MMA, iAs, and TAs were 4.4, 0.4, 0.5, and 5.4 µg/L, respectively) (Farzan et al. 2021). Different urinary arsenic speciation levels in other regions might result from variations in research participants, living environments, lifestyle behaviors, dietary intakes, and individual methylation efficiency. Urinary iAs reflect recently personal iAs absorbed dose, and unique iAs methylation patterns remain stable for 8–10 months (Steinmaus et al. 2005). Urinary arsenic concentration could be a surrogate for exogenous multiple exposure sources (Hughes Michael 2006; Kile Molly et al. 2009). Our reported ICCs (0.17–0.39) for repeated urinary arsenic speciation measurements were low, revealing high variability over the three trimesters. The low ICCs might be partly due to the alteration in external exposure level of arsenic speciation or the woman’s physiology attributed to the progression of pregnancy (Abduljalil et al. 2012). Given the poor reproducibility in this study, multiple or consecutive measurements along the pregnancy are desired to characterize arsenic speciation exposure during the whole pregnancy accurately.
The mtDNAcn, quantifying mitochondrial genome abundance, is a marker of mitochondrial function and oxidative stress (Castellani et al. 2020a, Malik and Czajka 2013). Mitochondria is the dominant cellular site of oxidative phosphorylation and ROS generation (Meyer et al. 2017). mtDNA is a prime victim of oxidative stress (Yakes and Houten 1997). MtDNAcn in most somatic cells ranges from 100 to 10,000 (Castellani et al. 2020b; Rausser et al. 2021). Mitochondria undergo fusion to complement mtDNA lesions via the transfer of nucleoids (Chen et al. 2010). Generally, the quantity of mtDNAcn within a cell is strictly governed to keep the cell in good condition (Attardi and Schatz 1988). Emerging epidemiology evidence has linked variation in mtDNAcn, either elevated or lower levels, to age-related disease (Castellani et al. 2020b; Hägg et al. 2021). Several epidemiological surveys have revealed that toxic exposures during early life were linked to changes in cord blood mtDNAcn. Increased cord blood mtDNAcn was found to be related to prenatal exposure to β-hexachlorocyclohexane (Vriens et al. 2017), aluminum (Liu et al. 2019), manganese (Kupsco et al. 2019), lead, and rare earth elements (gadolinium, dysprosium, erbium, and praseodymium) (Liu et al. 2020). Other surveys have shown that declined mtDNAcn was related to maternal smoking (Janssen et al. 2017), maternal lifetime stress (Brunst et al. 2017), prenatal exposure to thallium (Wu et al. 2019), arsenic (Song et al. 2020), magnesium (Smith Anna et al. 2021), air pollutants (PM2.5, PM10, and NO2) (Brunst et al. 2018; Clemente Diana et al. 2016; Hu et al. 2020; Janssen Bram et al. 2012), and benzotriazoles (Chen et al. 2020). It is comprehensible that the tendency of mtDNAcn changes varies from various pollutants. Additionally, findings for one exposure were not consistent. Therefore, current epidemiological surveys about the relationships of prenatal exposures with alterations in child mtDNAcn could not draw firm agreements. This discordance in effects might be partly ascribed to the discrepancies in the characteristics of the study participants, types and levels of exposures, different tissues used to determine mtDNAcn (cord blood vs. placenta tissue), and duration of exposure. Limited research has examined the relationships of maternal arsenic metabolite concentrations with cord blood mtDNAcn.
In this study, we observed positive (urinary DMA and TAs) associations with cord blood mtDNAcn. Prior surveys have shown that people in arsenic-exposed areas have higher mtDNAcn (Ameer et al. 2016; Lou et al. 2022; Sanyal et al. 2018). To our knowledge, only one study in Belgium has shown that cord blood TAs were linked to an elevated placental mtDNAcn (Vriens et al. 2017). Increased mtDNAcn manifests enhanced mitochondrial biogenesis resulting in cell aberrant proliferation (Lee et al. 2011, Malik and Czajka 2013, Wei and Lee 2002). Previous experimental surveys have displayed that low-level arsenic exposure enhanced mitochondrial biogenesis (Lee et al. 2011; Lou et al. 2022). Lee et al. found that primary keratinocytes treated with arsenic at concentrations lower than 1.0 µmol/L exhibited increased cell proliferation and mitochondrial biogenesis (Lee et al. 2011). Luo et al. found mtDNAcn in human hepatocyte L-02 cells treated with a low dose of iAs3+ (0.2 µmol/L) increased by more than 50% (Lou et al. 2022). Some surveys have reported that mtDNAcn increases with ROS to compensate for mtDNA lesions (Lee et al. 2000a; Liu et al. 2006; Wei et al. 2001). As a noted ROS stimulus, arsenic induces several types of ROS production, like peroxyl radicals, superoxide anion radicals, hydroxyl radicals, and hydrogen peroxide (Banerjee et al. 2011; Lynn et al. 2000). Little research has documented arsenite’s capability to promote mitochondrial ROS generation (Liu et al. 2005; Partridge et al. 2007). When ROS damaged mtDNA, reinforced mitochondrial biogenesis could increase mtDNAcn to make amends for mitochondrial malfunction (Giordano et al. 2014; Lee et al. 2000b). Nevertheless, excessive ROS might bring about declined mtDNA synthesis (Hou et al. 2010). Maintaining mtDNAcn in response to ROS induced by different pollutants remains unclear. Further surveys based on prospective cohorts and ingeniously designed toxicological surveys are needed to elucidate the toxic mechanism for arsenic species. Our findings also showed a possibly enhanced susceptibility to arsenic species exposure in the third trimester. Probable explanations might be variations in arsenic metabolite concentrations across pregnancy or chronic arsenic toxicity in mitochondria (Partridge et al. 2007). More studies are warranted to determine possible windows of prenatal exposure to arsenic species.
So far, this is the first report on connections between maternal arsenic species and cord blood mtDNAcn, using repeated measurements. Notwithstanding, some disadvantages could not be ignored. First, it was not possible to eliminate the residual confounding by other unmeasured factors, like the lack of cell-type data for cord blood mtDNAcn. Blood samples used to quantify mtDNAcn consist of different cell types, and mtDNAcn in diverse immune cells vary (Hurtado-Roca et al. 2016). Equally, mtDNAcn is estimated according to genomic DNA originating from the buffy coat, which is confounded by both cell type distributions and contaminating platelets (Rausser et al. 2021). The lack of data on platelet count in the cord blood samples might result in the overestimation of leukocyte mtDNAcn quantification in consideration of high levels of mtDNA, not nuclear DNA, in platelets (Hurtado-Roca et al. 2016; Urata et al. 2008). Second, oxidative stress biomarkers in cord blood samples were not determined, which were associated with mitochondrial function (Liu et al. 2003). Finally, all participants in this survey were Chinese, which limited external generalizability to other populations. Further surveys of different people are suggested to confirm our findings.
Conclusion
In this prospective pre-birth cohort from Wuhan, China, DMA and TA exposure in the third trimester was linked to elevated cord blood mtDNAcn. Our findings provided epidemiological data on mtDNA as a target of metals and emphasized a possible complicated part of arsenic specie in pathways of disease. Additional surveys are demanded to shed light on the molecular pathways involved in cord blood mtDNA damage induced by maternal methylated arsenic exposure.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Abduljalil K, Furness P, Johnson TN, Rostami-Hodjegan A, Soltani H (2012) Anatomical, physiological and metabolic changes with gestational age during normal pregnancy. Clin Pharmacokinet 51:365–396. https://doi.org/10.2165/11597440-000000000-00000
Ameer SS, Xu Y, Engström K, Li H, Tallving P, Nermell B, Boemo A, Parada LA, Peñaloza LG, Concha G, Harari F, Vahter M, Broberg K (2016) Exposure to inorganic arsenic is associated with increased mitochondrial DNA copy number and longer telomere length in peripheral blood. Front Cell Dev Biol 4:87. https://doi.org/10.3389/fcell.2016.00087
Attardi G, Schatz G (1988) Biogenesis of mitochondria. Annu Rev Cell Biol 4:289–331. https://doi.org/10.1146/annurev.cb.04.110188.001445
Banerjee M, Bhattacharjee P, Giri AK (2011) Arsenic-induced cancers: a review with special reference to gene, environment and their interaction. Genes Environ 33:128–140
Barrera-Gómez J, Basagaña X (2015) Models with transformed variables: interpretation and software. Epidemiology 26:e16–e17. https://doi.org/10.1097/EDE.0000000000000247
Barrett JR (2016) Prenatal air pollution and reduced birth weight: decline in placental mitochondria as a potential mechanism. Environ Health Perspect 124:A98–A98. https://doi.org/10.1289/ehp.124-A98
Brunst KJ, Sanchez-Guerra M, Chiu Y-HM, Wilson A, Coull BA, Kloog I, Schwartz J, Brennan KJ, Bosquet Enlow M, Wright RO, Baccarelli AA, Wright RJ (2018) Prenatal particulate matter exposure and mitochondrial dysfunction at the maternal-fetal interface: effect modification by maternal lifetime trauma and child sex. Environ Int 112:49–58. https://doi.org/10.1016/j.envint.2017.12.020
Brunst KJ, Sanchez Guerra M, Gennings C, Hacker M, Jara C, Bosquet Enlow M, Wright RO, Baccarelli A, Wright RJ (2017) Maternal lifetime stress and prenatal psychological functioning and decreased placental mitochondrial DNA copy number in the PRISM study. Am J Epidemiol 186:1227–1236. https://doi.org/10.1093/aje/kwx183
Castellani CA et al (2020a) Mitochondrial DNA copy number can influence mortality and cardiovascular disease via methylation of nuclear DNA CpGs. Genome Med 12:84. https://doi.org/10.1186/s13073-020-00778-7
Castellani CA, Longchamps RJ, Sun J, Guallar E, Arking DE (2020b) Thinking outside the nucleus: Mitochondrial DNA copy number in health and disease. Mitochondrion 53:214–223. https://doi.org/10.1016/j.mito.2020.06.004
Chain EPoCitF (2009) Scientific opinion on arsenic in food. EFSA J 7:1351
Chen H, Vermulst M, Wang YE, Chomyn A, Prolla TA, McCaffery JM, Chan DC (2010) Mitochondrial fusion is required for mtDNA stability in skeletal muscle and tolerance of mtDNA mutations. Cell 141:280–289. https://doi.org/10.1016/j.cell.2010.02.026
Chen H, Zhang H, Wang X, Wu Y, Zhang Y, Chen S, Zhang W, Sun X, Zheng T, Xia W, Xu S, Li Y (2023) Prenatal arsenic exposure, arsenic metabolism and neurocognitive development of 2-year-old children in low-arsenic areas. Environ Int 174:107918. https://doi.org/10.1016/j.envint.2023.107918
Chen Y, Wu F, Liu X, Parvez F, LoIacono NJ, Gibson EA, Kioumourtzoglou M-A, Levy D, Shahriar H, Uddin MN, Islam T, Lomax A, Saxena R, Sanchez T, Santiago D, Ellis T, Ahsan H, Wasserman GA, Graziano JH (2019) Early life and adolescent arsenic exposure from drinking water and blood pressure in adolescence. Environ Res 178:108681. https://doi.org/10.1016/j.envres.2019.108681
Chen X, Zhou Y, Hu C, Xia W, Xu S, Cai Z, Li Y (2020) Prenatal exposure to benzotriazoles and benzothiazoles and cord blood mitochondrial DNA copy number: a prospective investigation. Environ Int 143:105920. https://doi.org/10.1016/j.envint.2020.105920
Chen W-J, Davis EM, Stoner JA, Robledo C, Goodman JR, Garwe T, Janitz AE, Xu C, Hwang J, Peck JD (2021) Urinary total arsenic and arsenic methylation capacity in pregnancy and gestational diabetes mellitus: a case-control study. Chemosphere 271:129828. https://doi.org/10.1016/j.chemosphere.2021.129828
Clemente DB, Casas M, Vilahur N, Begiristain H, Bustamante M, Carsin AE, Fernández MF, Fierens F, Gyselaers W, Iñiguez C, Janssen BG, Lefebvre W, Llop S, Olea N, Pedersen M, Pieters N, Santa Marina L, Souto A, Tardón A et al (2016) Prenatal ambient air pollution, placental mitochondrial DNA content, and birth weight in the INMA (Spain) and ENVIRONAGE (Belgium) birth Cohorts. Environ Health Perspect 124:659–665. https://doi.org/10.1289/ehp.1408981
Concha G, Vogler G, Lezcano D, Nermell B, Vahter M (1998) Exposure to inorganic arsenic metabolites during early human development. Toxicol Sci 44:185–190. https://doi.org/10.1006/toxs.1998.2486
De Loma J, Krais AM, Lindh CH, Mamani J, Tirado N, Gardon J, Broberg K (2022) Arsenic exposure and biomarkers for oxidative stress and telomere length in indigenous populations in Bolivia. Ecotoxicol Environ Saf 231:113194. https://doi.org/10.1016/j.ecoenv.2022.113194
Dunn JD, Alvarez LAJ, Zhang X, Soldati T (2015) Reactive oxygen species and mitochondria: a nexus of cellular homeostasis. Redox Biol 6:472–485. https://doi.org/10.1016/j.redox.2015.09.005
European Food Safety A (2014) Dietary exposure to inorganic arsenic in the European population. EFSA J 12:3597
Farzan SF, Howe CG, Chavez TA, Hodes TL, Johnston JE, Habre R, Dunton G, Bastain TM, Breton CV (2021) Demographic predictors of urinary arsenic in a low-income predominantly Hispanic pregnancy cohort in Los Angeles. J Expo Sci Environ Epidemiol 31:94–107. https://doi.org/10.1038/s41370-020-0251-1
Farzan SF, Karagas MR, Chen Y (2013) In utero and early life arsenic exposure in relation to long-term health and disease. Toxicol Appl Pharmacol 272:384–390. https://doi.org/10.1016/j.taap.2013.06.030
Gao S, Lin P-I, Mostofa G, Quamruzzaman Q, Rahman M, Rahman ML, Su L, Hsueh Y-m, Weisskopf M, Coull B, Christiani DC (2019) Determinants of arsenic methylation efficiency and urinary arsenic level in pregnant women in Bangladesh. Environ Health 18:94. https://doi.org/10.1186/s12940-019-0530-2
Gemma C, Sookoian S, Alvariñas J, García SI, Quintana L, Kanevsky D, González CD, Pirola CJ (2006) Mitochondrial DNA depletion in small- and large-for-gestational-age newborns. Obesity (Silver Spring) 14:2193–2199. https://doi.org/10.1038/oby.2006.257
Gilbert-Diamond D, Emond Jennifer A, Baker Emily R, Korrick Susan A, Karagas Margaret R (2016) Relation between in utero arsenic exposure and birth outcomes in a cohort of mothers and their newborns from New Hampshire. Environ Health Perspect 124:1299–1307. https://doi.org/10.1289/ehp.1510065
Giordano C, Iommarini L, Giordano L, Maresca A, Pisano A, Valentino ML, Caporali L, Liguori R, Deceglie S, Roberti M, Fanelli F, Fracasso F, Ross-Cisneros FN, D'Adamo P, Hudson G, Pyle A, Yu-Wai-Man P, Chinnery PF, Zeviani M et al (2014) Efficient mitochondrial biogenesis drives incomplete penetrance in Leber's hereditary optic neuropathy. Brain 137:335–353. https://doi.org/10.1093/brain/awt343
Hägg S, Jylhävä J, Wang Y, Czene K, Grassmann F (2021) Deciphering the genetic and epidemiological landscape of mitochondrial DNA abundance. Hum Genet 140:849–861. https://doi.org/10.1007/s00439-020-02249-w
Hall M, Gamble M, Slavkovich V, Liu X, Levy D, Cheng Z, van Geen A, Yunus M, Rahman M, Pilsner JR, Graziano J (2007) Determinants of arsenic metabolism: blood arsenic metabolites, plasma folate, cobalamin, and homocysteine concentrations in maternal–newborn pairs. Environ Health Perspect 115:1503–1509. https://doi.org/10.1289/ehp.9906
Hayakawa T, Kobayashi Y, Cui X, Hirano S (2005) A new metabolic pathway of arsenite: arsenic–glutathione complexes are substrates for human arsenic methyltransferase Cyt19. Arch Toxicol 79:183–191. https://doi.org/10.1007/s00204-004-0620-x
Hou L, Zhu Z-Z, Zhang X, Nordio F, Bonzini M, Schwartz J, Hoxha M, Dioni L, Marinelli B, Pegoraro V, Apostoli P, Bertazzi PA, Baccarelli A (2010) Airborne particulate matter and mitochondrial damage: a cross-sectional study. Environ Health 9:48. https://doi.org/10.1186/1476-069X-9-48
Hu C, Sheng X, Li Y, Xia W, Zhang B, Chen X, Xing Y, Li X, Liu H, Sun X, Xu S (2020) Effects of prenatal exposure to particulate air pollution on newborn mitochondrial DNA copy number. Chemosphere 253:126592. https://doi.org/10.1016/j.chemosphere.2020.126592
Huang MC, Douillet C, Dover EN, Stýblo M (2018) Prenatal arsenic exposure and dietary folate and methylcobalamin supplementation alter the metabolic phenotype of C57BL/6J mice in a sex-specific manner. Arch Toxicol 92:1925–1937. https://doi.org/10.1007/s00204-018-2206-z
Hughes MF (2006) Biomarkers of exposure: a case study with inorganic arsenic. Environ Health Perspect 114:1790–1796. https://doi.org/10.1289/ehp.9058
Hurtado-Roca Y, Ledesma M, Gonzalez-Lazaro M, Moreno-Loshuertos R, Fernandez-Silva P, Enriquez JA, Laclaustra M (2016) Adjusting MtDNA quantification in whole blood for peripheral blood platelet and leukocyte counts. PLoS ONE 11:e0163770. https://doi.org/10.1371/journal.pone.0163770
Janssen BG, Gyselaers W, Byun H-M, Roels HA, Cuypers A, Baccarelli AA, Nawrot TS (2017) Placental mitochondrial DNA and CYP1A1 gene methylation as molecular signatures for tobacco smoke exposure in pregnant women and the relevance for birth weight. J Transl Med 15:5. https://doi.org/10.1186/s12967-016-1113-4
Janssen BG, Munters E, Pieters N, Smeets K, Cox B, Cuypers A, Fierens F, Penders J, Vangronsveld J, Gyselaers W, Nawrot Tim S (2012) Placental mitochondrial DNA content and particulate air pollution during in utero life. Environ Health Perspect 120:1346–1352. https://doi.org/10.1289/ehp.1104458
Kile ML, Hoffman E, Hsueh Y-M, Afroz S, Quamruzzaman Q, Rahman M, Mahiuddin G, Ryan L, Christiani David C (2009) Variability in biomarkers of arsenic exposure and metabolism in adults over time. Environ Health Perspect 117:455–460. https://doi.org/10.1289/ehp.11251
Kupsco A, Sanchez-Guerra M, Amarasiriwardena C, Brennan KJM, Estrada-Gutierrez G, Svensson K, Schnaas L, Pantic I, Téllez-Rojo MM, Baccarelli AA, Wright RO (2019) Prenatal manganese and cord blood mitochondrial DNA copy number: effect modification by maternal anemic status. Environ Int 126:484–493. https://doi.org/10.1016/j.envint.2019.02.029
Kurzius-Spencer M, Burgess JL, Harris RB, Hartz V, Roberge J, Huang S, Hsu C-H, O’Rourke MK (2014) Contribution of diet to aggregate arsenic exposures—an analysis across populations. J Expo Sci Environ Epidemiol 24:156–162. https://doi.org/10.1038/jes.2013.37
Laine JE, Bailey KA, Rubio-Andrade M, Olshan AF, Smeester L, Drobná Z, Herring AH, Stýblo M, García-Vargas GG, Fry RC (2015) Maternal arsenic exposure, arsenic methylation efficiency, and birth outcomes in the Biomarkers of Exposure to ARsenic (BEAR) pregnancy cohort in Mexico. Environ Health Perspect 123:186–192. https://doi.org/10.1289/ehp.1307476
Lee H-C, Wei Y-H (2000) Mitochondrial role in life and death of the cell. J Biomed Sci 7:2–15. https://doi.org/10.1007/BF02255913
Lee H-C, Yin P-H, Lu C-Y, Chi C-W, Wei Y-H (2000a) Increase of mitochondria and mitochondrial DNA in response to oxidative stress in human cells. Biochem J 348 Pt 2(Pt 2):425–432
Lee H-C, Yin P-H, Lu C-Y, Chi C-W, Wei Y-H (2000b) Increase of mitochondria and mitochondrial DNA in response to oxidative stress in human cells. Biochem J 348:425–432
Lee C-H, Wu S-B, Hong C-H, Liao W-T, Wu C-Y, Chen G-S, Wei Y-H, Yu H-S (2011) Aberrant cell proliferation by enhanced mitochondrial biogenesis via mtTFA in arsenical skin cancers. Am J Pathol 178:2066–2076. https://doi.org/10.1016/j.ajpath.2011.01.056
Liang C, Wu X, Huang K, Yan S, Li Z, Xia X, Pan W, Sheng J, Tao R, Tao Y, Xiang H, Hao J, Wang Q, Tong S, Tao F (2020) Domain- and sex-specific effects of prenatal exposure to low levels of arsenic on children’s development at 6 months of age: findings from the Ma’anshan birth cohort study in China. Environ Int 135:105112. https://doi.org/10.1016/j.envint.2019.105112
Liu C-S, Tsai C-S, Kuo C-L, Chen H-W, Lii C-K, Ma Y-S, Wei Y-H (2003) Oxidative stress-related alteration of the copy number of mitochondrial DNA in human leukocytes. Free Radic Res 37:1307–1317. https://doi.org/10.1080/10715760310001621342
Liu S-X, Davidson MM, Tang X, Walker WF, Athar M, Ivanov V, Hei TK (2005) Mitochondrial damage mediates genotoxicity of arsenic in mammalian cells. Cancer Res 65:3236–3242. https://doi.org/10.1158/0008-5472.CAN-05-0424
Liu CS, Cheng WL, Lee CF, Ma YS, Lin CY, Huang CC, Wei YH (2006) Alteration in the copy number of mitochondrial DNA in leukocytes of patients with mitochondrial encephalomyopathies. Acta Neurol Scand 113:334–341. https://doi.org/10.1111/j.1600-0404.2006.00586.x
Liu B, Song L, Zhang L, Wu M, Wang L, Cao Z, Zhang B, Xu S, Wang Y (2019) Prenatal aluminum exposure is associated with increased newborn mitochondrial DNA copy number. Environ Pollut 252:330–335. https://doi.org/10.1016/j.envpol.2019.05.116
Liu Y, Wu M, Liu B, Song L, Bi J, Wang L, Upadhyaya Khatiwada S, Chen K, Liu Q, Xiong C, Li Y, Xia W, Xu S, Wang Y, Zhou A (2020) Association of prenatal exposure to rare earth elements with newborn mitochondrial DNA content: results from a birth cohort study. Environ Int 143:105863. https://doi.org/10.1016/j.envint.2020.105863
Lou Q, Zhang M, Zhang K, Liu X, Zhang Z, Zhang X, Yang Y, Gao Y (2022) Arsenic exposure elevated ROS promotes energy metabolic reprogramming with enhanced AKT-dependent HK2 expression. Sci Total Environ 836:155691. https://doi.org/10.1016/j.scitotenv.2022.155691
Lynn S, Gurr J-R, Lai H-T, Jan K-Y (2000) NADH oxidase activation is involved in arsenite-induced oxidative DNA damage in human vascular smooth muscle cells. Circ Res 86:514–519. https://doi.org/10.1161/01.res.86.5.514
Malik AN, Czajka A (2013) Is mitochondrial DNA content a potential biomarker of mitochondrial dysfunction? Mitochondrion 13:481–492. https://doi.org/10.1016/j.mito.2012.10.011
Meyer JN, Leuthner TC, Luz AL (2017) Mitochondrial fusion, fission, and mitochondrial toxicity. Toxicology 391:42–53. https://doi.org/10.1016/j.tox.2017.07.019
Negro Silva LF, Lemaire M, Lemarié Catherine A, Plourde D, Bolt Alicia M, Chiavatti C, Bohle DS, Slavkovich V, Graziano Joseph H, Lehoux S, Mann Koren K (2017) Effects of inorganic arsenic, methylated arsenicals, and arsenobetaine on atherosclerosis in the apoE−/− mouse model and the role of As3mt-mediated methylation. Environ Health Perspect 125:077001. https://doi.org/10.1289/EHP806
Negro Silva LF, Makhani K, Lemaire M, Lemarié Catherine A, Plourde D, Bolt Alicia M, Chiavatti C, Bohle DS, Lehoux S, Goldberg Mark S, Mann Koren K (2021) Sex-specific effects of prenatal and early life inorganic and methylated arsenic exposure on atherosclerotic plaque development and composition in adult ApoE−/− mice. Environ Health Perspect 129:057008. https://doi.org/10.1289/EHP8171
Partridge MA, Huang SXL, Hernandez-Rosa E, Davidson MM, Hei TK (2007) Arsenic induced mitochondrial DNA damage and altered mitochondrial oxidative function: implications for genotoxic mechanisms in mammalian cells. Cancer Res 67:5239–5247. https://doi.org/10.1158/0008-5472.CAN-07-0074
Pejznochová M, Tesařová M, Honzík T, Hansíková H, Magner M, Zeman J (2008) The developmental changes in mitochondrial DNA content per cell in human cord blood leukocytes during gestation. Physiol Res 57:947–955. https://doi.org/10.33549/physiolres.931246
Rausser S, Trumpff C, McGill MA, Junker A, Wang W, Ho S-H, Mitchell A, Karan KR, Monk C, Segerstrom SC, Reed RG, Picard M (2021) Mitochondrial phenotypes in purified human immune cell subtypes and cell mixtures. eLife 10:e70899. https://doi.org/10.7554/eLife.70899
Ravenscroft P, Brammer H, Richards K (2009) Arsenic pollution: a global synthesis, vol 28. John Wiley & Sons
Rodriguez KF, Ungewitter Erica K, Crespo-Mejias Y, Liu C, Nicol B, Kissling Grace E, Yao Humphrey H-C (2016) Effects of in utero exposure to arsenic during the second half of gestation on reproductive end points and metabolic parameters in female CD-1 mice. Environ Health Perspect 124:336–343. https://doi.org/10.1289/ehp.1509703
Rodriguez KF, Mellouk N, Ungewitter EK, Nicol B, Liu C, Brown PR, Willson CJ, Yao HHC (2020) In utero exposure to arsenite contributes to metabolic and reproductive dysfunction in male offspring of CD-1 mice. Reprod Toxicol 95:95–103. https://doi.org/10.1016/j.reprotox.2020.05.006
Rosner B (2011) Fundamentals of biostatistics, 7th edn. Cengage Learning, Boston Brooks/Cole
Sánchez BN, Hu H, Litman Heather J, Téllez-Rojo Martha M (2011) Statistical methods to study timing of vulnerability with sparsely sampled data on environmental toxicants. Environ Health Perspect 119:409–415. https://doi.org/10.1289/ehp.1002453
Sanyal T, Bhattacharjee P, Bhattacharjee S, Bhattacharjee P (2018) Hypomethylation of mitochondrial D-loop and ND6 with increased mitochondrial DNA copy number in the arsenic-exposed population. Toxicology 408:54–61. https://doi.org/10.1016/j.tox.2018.06.012
Shadel GS, Horvath TL (2015) Mitochondrial ROS signaling in organismal homeostasis. Cell 163:560–569. https://doi.org/10.1016/j.cell.2015.10.001
Smith AR, Lin Pi ID, Rifas-Shiman Sheryl L, Rahman Mohammad L, Gold Diane R, Baccarelli Andrea A, Claus Henn B, Amarasiriwardena C, Wright Robert O, Coull B, Hivert M-F, Oken E, Cardenas A (2021) Prospective associations of early pregnancy metal mixtures with mitochondria DNA copy number and telomere length in maternal and cord blood. Environ Health Perspect 129:117007. https://doi.org/10.1289/EHP9294
Soler-Blasco R, Murcia M, Lozano M, Sarzo B, Esplugues A, Vioque J, Lertxundi N, Marina LS, Lertxundi A, Irizar A, Braeuer S, Goesler W, Ballester F, Llop S (2021) Urinary arsenic species and methylation efficiency during pregnancy: concentrations and associated factors in Spanish pregnant women. Environ Res 196:110889. https://doi.org/10.1016/j.envres.2021.110889
Soler-Blasco R, Murcia M, Lozano M, Sarzo B, Esplugues A, Riutort-Mayol G, Vioque J, Lertxundi N, Santa Marina L, Lertxundi A, Irizar A, Braeuer S, Ballester F, Llop S (2022) Prenatal arsenic exposure, arsenic methylation efficiency, and neuropsychological development among preschool children in a Spanish birth cohort. Environ Res 207:112208. https://doi.org/10.1016/j.envres.2021.112208
Song L, Liu B, Wang L, Wu M, Zhang L, Liu Y, Bi J, Yang S, Zhang B, Xia W, Xu S, Chen R, Cao Z, Wang Y (2020) Exposure to arsenic during pregnancy and newborn mitochondrial DNA copy number: a birth cohort study in Wuhan. China. Chemosphere 243:125335. https://doi.org/10.1016/j.chemosphere.2019.125335
Stajnko A, Šlejkovec Z, Mazej D, France-Štiglic A, BriŠKi AS, Prpić I, Špirić Z, Horvat M, Falnoga I (2019) Arsenic metabolites; selenium; and AS3MT, MTHFR, AQP4, AQP9, SELENOP, INMT, and MT2A polymorphisms in Croatian-Slovenian population from PHIME-CROME study. Environ Res 170:301–319. https://doi.org/10.1016/j.envres.2018.11.045
Steinmaus C, Yuan Y, Kalman D, Atallah R, Smith AH (2005) Intraindividual variability in arsenic methylation in a U.S. population. Cancer Epidemiol Biomark Prev 14:919–924. https://doi.org/10.1158/1055-9965.EPI-04-0277
Steinmaus C, Ferreccio C, Acevedo J, Balmes JR, Liaw J, Troncoso P, Dauphiné DC, Nardone A, Smith AH (2016) High risks of lung disease associated with early-life and moderate lifetime arsenic exposure in northern Chile. Toxicol Appl Pharmacol 313:10–15. https://doi.org/10.1016/j.taap.2016.10.006
Stýblo M, Drobná Z, Jaspers I, Lin S, Thomas DJ (2002) The role of biomethylation in toxicity and carcinogenicity of arsenic: a research update. Environ Health Perspect 110:767–771. https://doi.org/10.1289/ehp.110-1241242
Urata M, Koga-Wada Y, Kayamori Y, Kang D (2008) Platelet contamination causes large variation as well as overestimation of mitochondrial DNA content of peripheral blood mononuclear cells. Ann Clin Biochem 45:513–514. https://doi.org/10.1258/acb.2008.008008
Vahter M (2002) Mechanisms of arsenic biotransformation. Toxicology 181–182:211–217
Vriens A, Nawrot TS, Baeyens W, Den Hond E, Bruckers L, Covaci A, Croes K, De Craemer S, Govarts E, Lambrechts N, Loots I, Nelen V, Peusens M, De Henauw S, Schoeters G, Plusquin M (2017) Neonatal exposure to environmental pollutants and placental mitochondrial DNA content: a multi-pollutant approach. Environ Int 106:60–68. https://doi.org/10.1016/j.envint.2017.05.022
Wai T, Langer T (2016) Mitochondrial dynamics and metabolic regulation. Trends Endocrinol Metab 27:105–117. https://doi.org/10.1016/j.tem.2015.12.001
Wang X, Wu Y, Sun X, Guo Q, Xia W, Wu Y, Li J, Xu S, Li Y (2021) Arsenic exposure and metabolism in relation to blood pressure changes in pregnant women. Ecotoxicol Environ Saf 222:112527. https://doi.org/10.1016/j.ecoenv.2021.112527
Wei Y-H, Lee H-C (2002) Oxidative stress, mitochondrial DNA mutation, and impairment of antioxidant enzymes in aging. Exp Biol Med (maywood) 227:671–682. https://doi.org/10.1177/153537020222700901
Wei Y-H, Lee C-F, Lee H-C, Ma Y-S, Wang C-W, Lu C-Y, Pang C-Y (2001) Increases of mitochondrial mass and mitochondrial genome in association with enhanced oxidative stress in human cells harboring 4,977 BP-deleted mitochondrial DNA. Ann N Y Acad Sci 928:97–112. https://doi.org/10.1111/j.1749-6632.2001.tb05640.x
Wu M, Shu Y, Song L, Liu B, Zhang L, Wang L, Liu Y, Bi J, Xiong C, Cao Z, Xu S, Xia W, Li Y, Wang Y (2019) Prenatal exposure to thallium is associated with decreased mitochondrial DNA copy number in newborns: evidence from a birth cohort study. Environ Int 129:470–477. https://doi.org/10.1016/j.envint.2019.05.053
Yakes FM, Van Houten B (1997) Mitochondrial DNA damage is more extensive and persists longer than nuclear DNA damage in human cells following oxidative stress. Proc Natl Acad Sci U S A 94:514–519. https://doi.org/10.1073/pnas.94.2.514
Acknowledgements
The authors would like to acknowledge Shuangshuang Bao and Xiaojie Sun for their support and guidance in this developing this work.
Funding
This work was supported by the National Natural Science Foundation of China (42077398), the Program for HUST Academic Frontier Youth Team (2018QYTD12), and the National Institutes of Health (R01ES029082).
Author information
Authors and Affiliations
Contributions
Feng Qiu: conceptualization, data curation, methodology, software, formal analysis, writing—original draft; Hongling Zhang: data curation, formal analysis; xin Wang: investigation, methodology; Zhenxian Jia: data curation, validation; Yujie He: investigation, methodology, validation; Yi Wu: investigation, methodology; Zhangpeng Li: data curation, investigation; Tongzhang Zheng: data curation, investigation. Wei Xia: project administration, data curation, supervision. Shunqing Xu: conceptualization, project administration, resources; Yuanyuan Li: conceptualization, funding acquisition, project administration, writing—review and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was evaluated and approved by the Huazhong University of Science Institutional review boards.
Consent for publication
All authors revised the manuscript critically for intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qiu, F., Zhang, H., Wang, X. et al. Prenatal arsenic metabolite exposure is associated with increased newborn mitochondrial DNA copy number: evidence from a birth cohort study. Environ Sci Pollut Res 31, 38142–38152 (2024). https://doi.org/10.1007/s11356-024-32933-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-024-32933-7