Abstract
A multitude of epidemiological studies have demonstrated that both ambient temperatures and air pollution are closely related to health outcomes. However, whether temperature has modification effects on the association between ozone and health outcomes is still debated. In this study, three parallel time-series Poisson generalized additive models (GAMs) were used to examine the effects of modifying ambient temperatures on the association between ozone and mortality (including non-accidental, respiratory, and cardiovascular mortality) in Chengdu, China, from 2014 to 2016. The results confirmed that the ambient high temperatures strongly amplified the adverse effects of ozone on human mortality; specifically, the ozone effects were most pronounced at > 28 °C. Without temperature stratification conditions, a 10-μg/m3 increase in the maximum 8-h average ozone (O3–8hmax) level at lag01 was associated with increases of 0.40% (95% confidence interval [CI] 0.15%, 0.65%), 0.61% (95% CI 0.27%, 0.95%), and 0.69% (95% CI 0.34%, 1.04%) in non-accidental, respiratory, and cardiovascular mortality, respectively. On days during which the temperature exceeded 28 °C, a 10-μg/m3 increase in O3–8hmax led to increases of 2.22% (95% CI 1.21%, 3.23%), 2.67% (95% CI 0.57%, 4.76%), and 4.13% (95% CI 2.34%, 5.92%) in non-accidental, respiratory, and cardiovascular mortality, respectively. Our findings validated that high temperature could further aggravate the health risks of O3–8hmax; thus, mitigating ozone exposure will be brought into the limelight especially under the context of changing climate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is universally acknowledged that air pollution has adverse effects on human health; among all air pollutants, particles with aerodynamic diameters less than 2.5 μm (PM2.5) and ground-level ozone are considered to be most extraordinarily associated with morbidity and mortality (Dimakopoulou et al. 2017; Vicedo-Cabrera et al. 2020; Zhang et al. 2019a, 2020b; Cohen et al. 2015). China, the largest developing country, is currently facing a serious situation regarding air pollution, and PM2.5 and ozone are the first and second major pollutants, respectively (Kan et al. 2012; Wang 2021). Over the past decades, most studies have focused on the health risks of PM2.5; subsequently, a series of corresponding policies regarding PM2.5 control and intervention measures have been implemented based on these research results, leading to the PM2.5 level being effectively controlled in China (Lu et al. 2019; Maji et al. 2020). However, evidence concerning the adverse effects of ozone on health outcomes has been limited due to a lack of ozone data availability. No data were published concerning ozone before 2008. The Ministry of Ecology and Environment of the People’s Republic of China set the subsequent ozone air quality standards, and ground-level ozone data have been available online since 2013 (https://www.mee.gov.cn/). Compared with other countries, it is difficult to evaluate ozone standards in China due to the lack of sufficient evidence regarding the health effects of ozone. Recently, environmental monitoring observations have indicated that the concentration of PM2.5 in the Sichuan Basin of China is decreasing yearly, whereas the concentration of surface ozone is increasing (Ning et al. 2017); these results aroused our concern regarding the health risks caused by ozone in this area.
The ambient temperature is another important health risk factor. Substantial epidemiological and toxicological literature has been published showing a clear and consistent association between exposure to adverse ambient temperature, especially in cases of hypothermia and hyperpyrexia, both of which can cause a series of acute health effects, including respiratory tract injury, chronic cardiovascular conditions, systemic inflammation, and premature mortality (Wang 2021; Dimakopoulou et al. 2017; Qian et al. 2020). At the same time, the spatiotemporal distribution of ambient pollutants is affected by meteorological conditions, especially the ambient temperature (Zhang et al. 2019b); hence, ambient temperature and air pollution are generally highly correlated in many places and may symmetrically interact to affect health outcomes (Bae et al. 2020; Chen et al. 2017). Nonetheless, related studies about the modification effects of the ambient temperature on ozone-mortality relationships are rare, and published results have been inconsistent: some researchers have claimed a strong enhancement of ozone risks on health outcomes only under high temperature levels, whereas others have found outstandingly increases only under low temperature conditions, and some have validated relatively high ozone risks for both high and low temperatures (Iny et al. 2014; Chen et al. 2018b, a; Ren et al. 2007). These inconsistencies may correspond to the different climate and topographic conditions, ozone distribution characteristics, demographic compositions, people’s lifestyles, and education levels of diverse areas (Li et al. 2018). As the capital city of Sichuan province, the population of Chengdu exceeded 16.04 million as of June 2018, and the city suffers serious ozone pollution, especially in summer (Yang et al. 2021). The modulatory effects of ambient temperatures on ozone-mortality relationships in this area are still unclear.
In the present study, we assessed ozone mortality risks on non-accidental, respiratory, and cardiovascular mortality in Chengdu, China, from 2014 to 2016. In addition, we explored whether the associations between ozone and non-accidental mortality as well as cause-specific mortality were modified by ambient temperature. To achieve this aim, three parallel time-series Poisson generalized additive models (GAMs) were used to estimate how the air temperature modulates the health risks of ozone on the three analyzed kinds of mortality.
Data and methods
Data collection
The daily cause-specific mortality count data for each district/county of Chengdu (including Jinjiang District, Qingyang District, Jinniu District, Wuhou District, Chenghua District, Longquanyi District, Qingbaijiang District, Xindu District, Wenjiang District, Shuangliu District, and Xinjin County) during 2014 to 2016 were obtained from the National Center for Chronic and Non-communicable Disease Control and Prevention (NCNCD) of the Chinese Centers for Disease Control and Prevention (China CDC). The death data come from 421 hospitals with different grades in Chengdu. According to the 10th version of the International Classification of Diseases (ICD-10), data on three types of deaths were collected: non-accidental causes (ICD-10 codes A00-R99), cardiovascular diseases (ICD-10 codes I00–I99), and respiratory diseases (ICD-10 codes J00–J99). The total number of non-accidental, respiratory, and cardiovascular cases was 243,135, 76,721, and 59,676, respectively.
The air pollution data were retrieved from the Chengdu Environmental Monitoring Center. There are six monitoring stations in Chengdu including three urban environmental monitoring stations (Jinquan Lianghe, Sanwayao, and Shahepu), two traffic pollution monitoring stations (Shilidian, Liangjiaxiang), and one suburban environmental monitoring station (Lingyansi). Previous studies have indicated that the daily maximum 8-h average ozone (O3–8hmax) concentration is more strongly associated with health outcomes than other metrics, such as the 1-h maximum ozone concentration or the daily average ozone concentration (Yang et al. 2012). Consistent with the preceding studies, we therefore chose the daily O3–8hmax as the ozone concentration indicator. We collected the daily 24-h mean concentrations of PM10, PM2.5, SO2, and NO2 in Chengdu. To calculate the daily concentrations of the different pollutants at a single station, at least 75% of the hourly values had to be available on a particular day for each pollutant. Moreover, to calculate the 8-h maximum ozone concentration, an extra restrictive condition was that at least 6 h of data had to be available in each 8-h period within a day. The daily concentrations were the mean value of the data from the available monitoring results of six monitoring stations.
Daily meteorological data recorded during the same time period were retrieved from the China Meteorological Data Sharing Service System (http://data.cma.cn/). The daily surface meteorological data of Chengdu were obtained through station averages, mainly including the daily average temperature (°C), daily average relative humidity (RH) (%), and daily average wind speed (m/s).
Statistical methods
We utilized three GAMs to assess how the air temperature modulates the health risks of O3–8hmax on health outcomes: an independent model, a nonparametric bivariate response surface model, and a stratification parametric model (Zhang et al. 2020b). First, we used an independent GAM to investigate the adverse health effects of O3–8hmax on non-accidental mortality, as well as cause-specific (respiratory and cardiovascular) mortality at different lag days. Model 1 can be expressed as follows:
where subscript t is the day of the observation; E(Yt|X) indicates the expected death counts on day t; and \(NS(\bullet )\) denotes the natural cubic spline function. According to the preceding study (Yang et al. 2012), the Time variable was controlled with 7 degrees of freedom (df) per year to express a long-term trend. At the same time, (df = 3) was also used to control the current day’s average relative humidity (RH) and mean wind speed (Wind), as well as the moving average daily mean temperature of the current and the previous day (lag01) (Zhang et al. 2020b). DOW and Holiday are two categorical variables that represent the day of the week and the presence of a public holiday, respectively. The subscript i represents different lag days. We explored the adverse health effects of O3–8hmax on three types of mortality at different lag days which include both a single-day lag (from lag0 to lag4) and cumulative lags (using moving averages of the current day and the previous 1, 2, 3, or 4 days [lag01 to lag04]).\(\alpha\) represents the intercept. In addition, COVs is all other covariates.
Second, a nonparametric bivariate response surface model was adopted to visually examine the combing effects of both the ambient average temperature and O3–8hmax on three types of mortality. The model is described as follows:
where \(ST\left(\bullet \right)\) indicates the thin-plate spline functions. Statistics revealed that the adverse health risks of O3–8hmax on three types of mortality were strongest between the current and previous day (lag01) (as is described later in this study). Therefore, the daily O3–8hmax at lag01 was used in the follow-up research to effectively capture the overall effects. The COVs are the same as those used in model 1.
Finally, we adopted a temperature-stratified parametric model to examine the heterogeneity of O3–8hmax risks across different temperature ambient temperature strata. Temperatures were categorized into high and low temperature levels and then to determine whether the O3–8hmax risks varied across different temperature strata. However, there is by no means uniform standard for choosing temperature cutoff points so far (Zhang et al. 2020b). According to previous research results, people feel more comfortable when the daily average temperature is near approximately 24℃ and begin to feel uncomfortable due to heat when the daily average is > 28 °C (Ssl et al., 2019). Therefore, we chosen temperature cutoff points corresponding to the transition from comfort to discomfort with increasing heat (i.e., 24 °C, 26 °C, and 28 °C), as outlined by Zhang et al. (2020b). Finally, we divided the temperature data into two strata, including high temperatures (above the cutoffs) and low temperatures (below the cutoffs). Then, we assessed how the O3–8hmax mortality risks varied among the different temperature levels using varied temperature cutoff points. Model 3 is given as follows:
where \({Temp}_{k}\) is the k-th temperature strata; \({\beta }_{1}\) and \({\beta }_{2}\) denote the main independent effects of O3–8hmax levels and daily average temperature, respectively; and \({\beta }_{3}\) refers to a vector of coefficients reflecting the conjunction effects between O3–8hmax and daily average temperatures; this vector was also adjusted for temperature (\({Temp}_{k}\)) within each temperature strata. The COVs are the same as those used in model 1.
To test the robustness of the models, we performed several sensitivity analyses. First, we changed the df of time from 4 to 10 per year. Second, we changed the df of Temp, RH, and Wind from 3 to 5, respectively. Third, we applied different maximum lags for temperature (1, 3, 5, and 7 days, respectively). Moreover, we used co-pollutant models of other pollutants, such as PM2.5, PM10, SO2, NO2, and CO to account for potential confounding effects from multiple exposures. All of the above analyses were conducted when the temperature levels were stratified by using 24℃.
All statistical analyses were conducted with R 4.1.2. The estimated modulating effects and corresponding 95% confidence interval (CI) were showed as percentage changes in health outcomes with each 10-μg/m3 increment in the O3–8hmax mass concentration.
Results
Table 1 summarizes the distributions of three types of mortality, meteorological factors, and O3–8hmax concentrations during the study period. There were considerable variations in the three mortality types, ranging from 144 to 430 non-accidental mortalities, 35 to 136 cardiovascular mortalities, and 23 to 121 respiratory mortalities. During the study period, the daily mean temperature range between − 1.9 and 29.8℃ and there were no any heat waves (Fig S1). According to statistical analysis, the average temperature in Chengdu was 16.6 ± 7.2 °C, the average RH was 81.7 ± 8.2%, and the average wind speed was 1.3 ± 0.5 m/s. Notably, the average daily O3–8hmax concentration was 119.9 µg/m3 that quite higher than those reported in some developed countries (Tao et al. 2016; Nyssanbayeva et al. 2019; Winiewski et al. 2021) and in other Chinese cities (Sui, et al. 2021; Zhang et al. 2006). According to the National Ambient Air Quality Standard (GB3095-2012), the O3–8hmax concentrations exceeded the primary (100 µg/m3) and secondary (160 µg/m3) standard limits in 611 days and 280 days, respectively, and the corresponding over standard rates were 55.75% and 25.55%, respectively.
Figure 1 illustrates the effects of percentage changes in O3–8hmax on three types of mortality at different lags. The most significant effects of O3–8hmax on the three types of mortality all appeared at a cumulative lag of one day (lag01). Therefore, lag01 O3–8hmax was used as the research object in subsequent studies. After the calculations, a 10-μg/m3 increase in O3–8hmax was found to lead to 0.40% (95% CI 0.15%, 0.65%), 0.61% (95% CI 0.27%, 0.95%), and 0.69% (95% CI 0.34%, 1.04%) increases in non-accidental, respiratory, and cardiovascular mortality, respectively.
Figure 2 graphically depicts the combined effects of the daily average temperature and O3–8hmax on non-accidental, cardiovascular, and respiratory mortality using three-dimensional visualization graphs. It is apparent that the combined effects were extremely complex. It is interesting to note that the non-accidental, cardiovascular, and respiratory mortality all reached their maxima when high-temperature and high-concentration O3–8hmax coexisted, thus indicating that the high temperature exacerbated/amplified the mortality risks of O3–8hmax.
Table 2 summarizes the modulating effects of low/high temperatures on O3–8hmax-mortality relationships using varied temperature cutoff points. It should also be noted that the modulation effects of temperature on O3–8hmax-mortality were more pronounced in the high-temperature section than in the low-temperature section, and these effects were stronger than those obtained in the independent effect model. Furthermore, the higher the temperature cutoff points were, the greater the health risks of O3–8hmax were on the same kind of mortality at a high temperature level, indicating that high temperatures significantly aggravated the health risk of O3–8hmax on mortality compared to low temperatures.
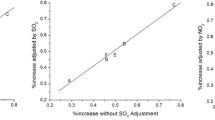
The sensitivity analyses turned out that the O3–8hmax-mortality risks kept robust to changing the df of the temporal smoothness per year (Fig. 3). The percentage changes derived per 10-μg/m3 increment in O3–8hmax significantly increased from 0.35 (95% CI 0.24%, 0.46%) to 0.40% (95% CI 0.27%, 0.53%) for non-accidental mortality, 0.48 (95% CI 0.26%, 0.70%) to 0.61% (95% CI 0.35%, 0.87%) for respiratory mortality, and 0.62 (95% CI 0.39%, 0.85%) to 0.69% (95% CI 0.46%, 0.92%) for cardiovascular mortality when the df was changed from 4 to 10 per year. The changes of df for Temp, RH, and Wind, and the maximum lag days of mean temperature did not substantially affect the magnitude of the estimates (see Table S1, S2), and the same patterns were found in the co-pollutant models with the inclusion of PM2.5, PM10, SO2, NO2, and CO (see Table S3), suggesting that the ozone-mortality relationship was not confounded by other pollutants.
Discussion
Ground-level ozone has become a compelling environmental problem that has drawn substantial attention worldwide (Stocker et al. 2013). Assessing ground-level ozone health effects could provide additional evidences for policymaking on the topic of ozone control measures, particularly under the background of climate change (Madaniyazi et al., 2016). Our findings proved that exposure to ground-level O3–8hmax were positively associated with non-accidental mortality as well as cardiovascular and respiratory mortality in Chengdu, China, during the study period. Furthermore, our study further validated that high temperature significantly amplified O3–8hmax-mortality risks on the three analyzed mortality types. In particular, there existed a consistent pattern of increasing O3–8hmax-mortality risks as we progressively adopted higher cutoffs for high-temperature category.
It is worth noting that the average daily O3–8hmax concentration was 119.9 µg/m3 and has a high ozone exceeding standard rate in Chengdu during the study period. From the perspective of air-pollution meteorology, there exist two key factors leading to air pollution: one is the excessive emission of air pollutants and secondary transformation, and the other is the dilution and diffusion of air pollutants by the unfavorable meteorological conditions (Cai et al., 2017). As we all known, ozone, as a secondary pollutant, is widespread in the atmospheric troposphere and mainly produced by photochemical reactions of precursors (nitrogen oxides and volatile organic compounds (VOCs)); the concentration of ground-level ozone are influenced by anthropogenic and natural emissions and by chemical, physical, and biological processes. The anthropogenic VOCs mainly come from incomplete combustion in motor vehicle exhaust, the volatilization of oil and gas coatings, and industrial emissions (Dang et al. 2021). As of June 2018, motor vehicle ownership had exceeded 3.89 million in Chengdu, and these vehicles produce plenty of nitrogen oxides and VOCs, which are conducive to the formation of ozone. On the other hand, Chengdu is located in the Sichuan Basin and is thus affected by the topography of the Qinghai-Tibetan Plateau; the average wind speed in the Sichuan Basin is low year-round, and the frequency of static and stable weather is high. These conditions are unfavorable to the diffusion or dilution of ground-level ozone (Zhang et al. 2019b). These high precursor concentrations and poor air diffusion conditions ultimately synergistically lead to high ozone pollution concentrations in Chengdu. Therefore, Chengdu should strengthen its air quality control, reduce its emission of ozone precursors, and formulate corresponding motor vehicle control and dispatching policies according to the changing meteorological conditions.
The temperature stratification results showed that the health risks of O3–8hmax were more prominent at high-temperature levels than at low-temperature levels. For instance, 1 day where temperatures exceeded 24 °C, a 10-μg/m3 increment in O3–8hmax increased mortality risks of non-accidental, respiratory, and cardiovascular by 0.52%, 0.65%, and 1.15%, respectively. The corresponding risks were 0.17%, 0.18%, and 0.22%, respectively, under low-temperature conditions (< 24 °C). These results keep consistent with some previous findings that O3–8hmax-mortality risks were more prominent in warm season (or summer half year) than in cold season (or winter half year) (Gryparis et al. 2004; Sun et al. 2018). Nevertheless, several previous studies (Cheng and Kan 2012) suggested that the most pronounced health risks of ozone on mortality were always observed in the cold season in southern coastal cities of China, which were distinctly opposite from our results. There are several reasons for the inconsistency between previous studies and our findings. First, the exposure pattern is an important factor affecting the results (Bell and Michelle 2004). In southern coastal cities of China, it is hot during summer and people prefer to stay indoors and mild in winter and people prefer to stay outdoors (Cheng and Kan 2012). Chengdu city is located in southwestern China and has a subtropical climate. In Chengdu, the warm season is relatively mild, and few extreme weather events occur. For instance, the average warm-season temperature is 20.93 °C. People therefore have passion for staying outdoors and open windows in these mild temperatures, which might increase the exposure of the population to ambient ozone (Wong et al. 2001). In contrast, people prefer to stay at home rather than go out in cold season, especially in winter, due to the bitter cold outdoor temperatures and poor air quality, ultimately reducing human exposure to ambient ozone in this season. Second, difference in the adjustment of the daily mean temperature might be possible reasons underlying these differences (Chen et al. 2018b, a). In the temperature-mortality association, the effect of a high temperature was immediate, while the effects of cold remained significant over long time lags (Zhang et al. 2020a). Previous studies have chosen different temperature lags of one day to a maximum lag of 21 days (Chen et al. 2018b, a; Jhun et al. 2014). Different from previous studies, considering the characteristics of ozone (short-lived gas), we pay more attention to the short-term temperature modification effects on ozone-mortality in this study. This discrepancy could cause inconsistent modification patterns.
Although the independent health risks of adverse temperatures or O3–8hmax on human health have been studied extensively and expounded in numerous studies, the interactions between temperature and O3–8hmax have been explored only in fragments, and the results remain controversial (Ren et al. 2007; Shi et al. 2020; Rainham and Smoyer-Tomic 2003). Only some studies have found interactive effects, while others have not. These discrepancies mainly result from environmental and climatic conditions, acclimatization, education attainment, infrastructures, etc. (Zhang et al. 2020b). Furthermore, the analytical methods used in various studies would lead to the inconsistency of results. Compared with previous studies, we divided temperatures into two levels (low and high temperatures) by using different temperature thresholds corresponding to comfort and discomfort. Our findings further support the notion that high-concentration ozone and high temperatures mutually interact to affect public health. The evidence from our study indicated the higher the temperature cutoff points were, the greater the health risks of O3–8hmax were on the same kind of mortality at a high-temperature level. Therefore, heat exposure may exacerbate physiological responses to short-term ozone exposure. For instance, each 10-μg/m3 increase in O3–8hmax concentration increased mortality risks by 0.74%, 0.81%, and 1.30% in non-accidental, respiratory, and cardiovascular mortality under high-temperature (> 26 °C) conditions; the corresponding risks were 2.22%, 2.67%, and 4.13% when chosen 28℃ as the temperature cutoff, as a warmer climate will likely increase individual susceptibility to ambient ozone exposure. As a result, it will become even more important to mitigate ozone exposure in the future (Tao et al. 2021; Vicedo-Cabrera et al. 2020).
The mechanisms by which the ambient temperature causes modulation effects on the relationships of ozone on human health remain unclear. There are several possible underlying mechanisms that explain this phenomenon. High temperatures are a well-known cause of heat-related mortality and can thus affect the physiological and psychological stress of the human body and aggravate many pre-existing diseases (Rainham and Smoyer-Tomic 2003). Furthermore, high temperatures are a necessary meteorological condition for ozone generation. Extreme high temperatures may further aggravate the generation rate of ozone and subsequently increase the health risks posed by ozone to the population. Ozone is a potent oxidant capable of generating reactive oxygen species/free radicals in lung cells, thus leading to the promotion of oxidative stress, inducing acute airway inflammation and damaging biomolecules (Lodovici et al., 2011; Ahmad et al. 2005). The inflammation of pulmonary tissues could further induce a spectrum of mediators and alter cardiac functions or the irritant receptor-mediated stimulation of parasympathetic pathways (Watkinson et al. 2001), making people more vulnerable to the effects of ozone variability. Therefore, both high-temperature and high-concentration ozone may interact to synergistically affect people health.
The study has several advantages should be acknowledged. First, as far as I am concerned, this is the first time to study the modification effects of temperature on O3–8hmax mortality in Chengdu, China. Second, different from the traditional studies, we divided the temperature data into two strata (including high and low temperatures) by using different temperature cutoff points from the perspective of human comfort, which is more in line with the actual situation. Third, our study further validated that high temperature significantly amplified O3–8hmax-mortality risks on the three analyzed mortality types. This interaction pattern remained consistent when different cutoffs for temperature were applied. All these findings suggest that different environmental governance and disease control strategies should be considered in Chengdu. Within a context of the changing climate, our results suggested that health damage due to ozone pollution may be influenced by the impact of increasing temperatures, and it might become much more important to mitigate ozone exposure in Chengdu of China to further reduce the public health burden.
Some limitations of this study should be acknowledged. First, we utilized mortality data from only a 3-year period, and the statistical power was thus reduced. Second, we had no access to sub-categorical mortality characteristics, such as age, sex, educational background, work status, or the air conditioning utilization rate. Iny et al. (2014) proved that air conditioning can mitigate the mortality risks caused by ozone exposure in 97 US cities, especially during the warm season. Unfortunately, we did not collect the relevant data mentioned above, and this limited our ability to link potentially sensitive subpopulations. Third, similar to most previous time-series studies (Bae et al. 2020; Shin et al. 2020), we only collected available outdoor monitoring data to represent personal exposure to ambient ozone, but not collected ozone concentration information in the indoor environments where people spend more time, and this omission could have biased the assessment accuracy obtained for ozone risks, resulting in a large exposure measurement error (Maji and Namdeo 2021). Fourth, previous studies (Shin et al. 2020; Zhang et al. 2020a) have demonstrated that both PM2.5 and ozone have adverse effects on mortality. It should be noted that we tried to include multiple interaction effects (including temperature and PM2.5, temperature, and O3–8hmax, as well as PM2.5 and O3–8hmax) on mortality in the model at initially. However, taking such complications into account did not significantly improve goodness of fit and lead to huge computation burden. In addition, previous study (Murase et al., 2009) has pointed out that if multiple interactions are considered simultaneously in the model, collinearity effects are inevitable and further lead to overfitting of the model, resulting in a large error. Therefore, we just pay more attention to the temperature modification effects on the relationship between O3–8hmax and mortality. We hope to do further research and overcome these problems in the future.
Conclusions
In conclusion, high temperatures strongly amplified the adverse health risks of O3–8hmax on non-accidental mortality as well as cause-specific mortality (including respiratory and cardiovascular mortality) in Chengdu, China. The results validated that reducing O3–8hmax emissions, especially in hot weather, would benefit public health. These findings improve our cognition for the short-term health risks of ozone and offer substantial reference information for policymaking regarding ground-level ozone control and adaptation strategies with the aim of protecting public health.
References
Ahmad S, Ahmad A, McConville G et al (2005) Lung epithelial cells release ATP during ozone exposure: signaling for cell survival. Free Radic Biol Med 39(2):213–226
Bae S, Lim YH, Hong YC (2020) Causal association between ambient ozone concentration and mortality in Seoul, Korea. Environ Res 182(Mar.):109098.1–109098.5.
Bell, Michelle L (2004) Ozone and short-term mortality in 95 US urban communities, 1987–2000. Jama 292(19):2372–2378
Cai W, Li K, Liao H et al (2017) Weather conditions conducive to Beijing severe haze more frequent under climate change. Nat Clim Chang 7(4):257–262
Chen K, Wolf K, Breitner S et al (2018a) A. Two-way effect modifications of air pollution and air temperature on total natural and cardiovascular mortality in eight European urban areas. Environ Int 116:186–196
Chen K, Wolf K, Hampel R et al (2018b) Does temperature-confounding control influence the modifying effect of air temperature in ozone–mortality associations?[J]. Environmental Epidemiology 2(1):1
Chen L, Shi M, Gao S et al (2017) Response to comment on “Assessment of population exposure to PM 2.5 for mortality in China and its public health benefit based on BenMAP”. Environ Pollut 221(FEB):311
Cheng Y, Kan H (2012) Effect of the interaction between outdoor air pollution and extreme temperature on daily mortality in Shanghai. China J Epidemiol 22(1):28–36
Cohen AJ, Brauer, Burnett et al (2017) Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet 389(10082):1907–1918
Dang R, Liao H, Fu Y (2021) Quantifying the anthropogenic and meteorological influences on summertime surface ozone in China over 2012–2017[J]. Sci Total Environ 754:142394
Dimakopoulou K, Grivas G, Samoli E et al (2017) Determinants of personal exposure to ozone in school children. Results from a panel study in Greece. Environ Res 154:66–72
Gryparis A, Forsberg B, Katsouyanni K et al (2004) Acute effects of ozone on mortality from the air pollution and health. Am J Respir Crit Care Med 170(10):1080–1087
Iny, Jhun, Neal et al (2014) Effect modification of ozone-related mortality risks by temperature in 97 US cities - ScienceDirect. Environ Int 73(1):128–134
Jhun I, Fann N, Zanobetti A, Hubbell B (2014) Effect modification of ozone-related mortality risks by temperature in 97 US cities. Environ Int 73:128–134
Kan H, Chen R, Tong S (2012) Ambient air pollution, climate change, and population health in China. Environment International 42(none):10–19
Li Y, Shang Y, Zheng C et al (2018) Estimated acute effects of ozone on mortality in a rural district of Beijing, China, 2005–2013: a time-stratified case-crossover study. Int J Environ Res Public Health 15(11):2460
Lodovici M, Bigagli E, Luceri C et al (2011) Protective effect of resveratrol against oxidation stress induced by 2-nitropropane in rat liver. Pharmacology & Pharmacy 02(3):228–234
Lu X, Lin C, Li W et al (2019) Analysis of the adverse health effects of PM2.5 from 2001 to 2017 in China and the role of urbanization in aggravating the health burden. Sci Total Environ 652(20):683–695
Madaniyazi L, Nagashima T, Guo Y et al (2016) Projecting ozone-related mortality in East China. Environ Int 92–93:165–172
Maji KJ, Namdeo A (2021) Continuous increases of surface ozone and associated premature mortality growth in China during 2015–2019. Environ Pollut 269C:116183
Maji KJ, Dikshit AK, Arora M et al (2020) Estimating premature mortality attributable to PM2.5 exposure and benefit of air pollution control policies in China for. Sci Total Environ 2017:612–683
Murase, Hiroto, Nagashima et al (2009) Application of a generalized additive model (GAM) to reveal relationships between environmental factors and distributions of pelagic fish and krill: a case study in Sendai Bay, Japan. ICES Journal of Marine Science / Journal du Conseil 66(6):1417–1424
Ning G, Wang S, Ma M et al (2017) Characteristics of air pollution in different zones of Sichuan Basin. China Science of the Total Environment 612:975
Nyssanbayeva AS, Cherednichenko AV, Cherednichenko AV et al (2019) Temporal dynamics of ground-level ozone and its impact on morbidity in Almaty city in comparison with Astana city. Kazakhstan Int J Biometeorol 63(17):1381–1392
Qian X, Zbs B, Yan TA et al (2020) Impacts of urbanization on the temperature-cardiovascular mortality relationship in Beijing China. Environ Res 191:110234
Rainham D, Smoyer-Tomic KE (2003) The role of air pollution in the relationship between a heat stress index and human mortality in Toronto. Environ Res 93(1):9–19
Ren C, Williams G, Morawska L et al (2007) Ozone modifies associations between temperature and cardiovascular mortality: analysis of the NMMAPS data. Epidemiology 18(4):255–260
Shi W, Sun Q, Du P et al (2020) Modification effects of temperature on the ozone-mortality relationship: a nationwide multicounty study in China. Environ Sci Technol 54(5):2859–2868
Shin HH, Parajuli RP, Maquiling A et al (2020) Temporal trends in associations between ozone and circulatory mortality in age and sex in Canada during 1984–2012. Sci Total Environ 724:137944
Ssl A, Aha B, Es A (2019) Using simulation methods to investigate the impact of urban form on human comfort Case study: coast of Baltim, North Coast Egypt. Alexandria Engineering Journal 58(1):273–282
Stocker T F, Qin D, Plattner G K, et al. Climate change 2013: the physical science basis. Contribution of Working Group I to the Fifth Assessment Report of IPCC the Intergovernmental Panel on Climate Change. http://www.ipcc.ch/publications_and_data/ publications_ipcc_fourth_assessment_report_wg1_report_the_physical_science_basis.htm, 2014, 18(2):95–123.
Sui X, Zhang J, Zhang Q et al (2021) The short-term effect of PM2.5/O3 on daily mortality from 2013 to 2018 in Hefei China. Environ Geochem Health 43(2):153–169
Sun Q, Wang W, Chen C et al (2018) Acute effect of multiple ozone metrics on mortality by season in 34 Chinese counties in 2013–2015. J Intern Med 283(5):481–488
Tao L, Zeng W, Lin H et al (2016) Tempo-spatial variations of ambient ozone-mortality associations in the USA: results from the NMMAPS data. Int J Environ Res Public Health 13(9):851
Tao Y, Huang W, Huang X et al (2021) Estimated acute effects of ambient ozone and nitrogen dioxide on mortality in the Pearl River Delta of southern China. Environ Health Perspect 120(3):393–398
Vicedo-Cabrera A M, Sera F, Liu C et al (2020) Short term association between ozone and mortality: global two stage time series study in 406 locations in 20 countries. BMJ
Wang P (2021) China’s air pollution policies: progress and challenges. Curr Opin Environ Sci Health 19:100227
Watkinson WP, Campen MJ, Nolan JP et al (2001) Cardiovascular and systemic responses to inhaled pollutants in rodents: effects of ozone and particulate matter. Environ Health Perspect 109(Suppl. 4):539–546
Winiewski O, Kozak W, Winiewski M (2021) The ground-level ozone concentration is inversely correlated with the number of COVID-19 cases in Warsaw, Poland. Air Qual Atmos Health 14(8):1169–1173
Wong C, Ma S, Hedley A et al (2001) T.H. Effect of air pollution on daily mortality in Hong Kong. Environ Environ Health Perspec 109(4):335–340
Yang C, Yang H, Guo S et al (2012) Alternative ozone metrics and daily mortality in Suzhou: the China Air Pollution and Health Effects Study (CAPES). Sci Total Environ 426:83–89
Yang X, Wu K, Lu Y et al (2021) Origin of regional springtime ozone episodes in the Sichuan Basin, China: role of synoptic forcing and regional transport. Environ Pollut 278(4):116845
Zhang Y, Huang W, London SJ et al (2006) Ozone and daily mortality in Shanghai, China. Environ Health Perspect 114(8):1227–1232
Zhang J, Qi C, Wang Q et al (2019) The acute health effects of ozone and PM2.5 on daily cardiovascular disease mortality: a multi-center time series study in China. Ecotoxicol Environ Saf 174(15):218–223
Zhang Y, Wang S, Zhang X et al (2020a) Temperature modulation of the adverse consequences on human mortality due to exposure to fine particulates: a study of multiple cities in China. Environ Res 185:109353
Zhang Y, Zhang X, Fan X et al (2020) Modifying effects of temperature on human mortality related to black carbon particulates in Beijing, China. Atmospheric Environment 243(JAN):117845
Zhang Y, Wang S, Fan X et al (2019b) A temperature indicator for heavy air pollution risks (TIP). Sci Total Environ 678
Acknowledgements
We thank Canjun Zheng and Xiaoling Zhang for providing daily death data of Chengdu.
Funding
This study was supported by the National Natural Science Foundation of China (42005136); the China Postdoctoral Science Foundation (2020M670419); the National Natural Science Foundation of China (41775147); the National key Research and Development Program of China (2016YFA0602004); and the Sichuan Science and technology planning project (2020Z076).
Author information
Authors and Affiliations
Contributions
Q.T. and S.W. designed the research; C.Z., W.H., and X.F. collected and analyzed the data; Y.Z., J.X., and P.M. wrote the paper.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Y., Tian, Q., Feng, X. et al. Modification effects of ambient temperature on ozone-mortality relationships in Chengdu, China. Environ Sci Pollut Res 29, 73011–73019 (2022). https://doi.org/10.1007/s11356-022-20843-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-022-20843-5