Abstract
This study aimed to investigate the seasonal variation of gonorrhea in China, and to analyze the relationship between the incidence of gonorrhea and meteorological factors. Data from gonorrhea cases were obtained from the Disease Prevention and Control Bureau and the Data-Center for China Public Health Science, Chinese Center for Disease Control and Prevention, and the incidence of gonorrhea in China from 1 January 2006 to 31 December 2019 was analyzed. Meteorological data from the same period were obtained from the South China Meteorological Data Sharing Center, including the average monthly temperature, relative humidity, atmospheric pressure, sunshine hours, number of rainy days, and precipitation. The ratio-to-moving average method and seasonal subseries plots were used to analyze the seasonality of gonorrhea cases. The distributed lag non-linear model and attribution risks were used to investigate the effects of meteorological indexes on gonorrhea cases. The number of gonorrhea cases showed seasonal variation, with a peak in the third quarter and a decline in the first quarter. The Spearman assay showed that the reported number of patients with gonorrhea was positively correlated with the monthly temperature, relative humidity, precipitation, and number of rainy days. The risk of gonorrhea onset was highest at 6–11 °C, and the highest risk occurred when the average monthly temperature was 7 °C (resulting in an increase of 14.5% compared with 13 °C); a similar result was found regarding the cumulative risk of gonorrhea onset in relation to temperature. The attribution score of temperature to the onset of gonorrhea was 5.02% (95% confidence interval: − 3.84%, 13.88%). The study findings suggest that increased emphasis should be placed on screening for gonorrhea during summer and autumn, and that education on safe sexual behavior should be promoted during these times.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Seasonal variation is a well-known phenomenon in life and health sciences, even for sexually transmitted diseases (STDs) such as gonorrhea (Kakran et al. 2015). The seasonality of gonorrhea was first reported in the USA in 1971 (Cornelius 1971) and then from 1999 to 2003 (Shah et al. 2007), with peak rates of gonorrhea in summer and early autumn (Cornelius 1971; Schroeder et al. 2001; Wright & Judson 1978). Two studies performed in the UK from 1972 to 1976 and 1984 to 1989 have shown a two-peak seasonal distribution in gonorrhea incidence, with peaks in both the first and third quarters of the year (Ross & Scott 1992; Wellings et al. 1999). A study of gonorrhea and urethritis rates in Burkina Faso, West Africa, also reported seasonal differences, with the highest rates occurring from January to May (Damiba et al. 1990).
Since the first case of gonorrhea was reported in Changsha City in 1977, gonorrhea has become prevalent in China. The reported incidence of gonorrhea increased from 10.09 cases per 100,000 population in 1991 to 18.57 cases per 100,000 population in 2001 (Gong et al. 2002), followed by a decline from 22.92 cases per 100,000 population in 2000 to 7.61 cases per 100,000 population in 2013 (Gong et al. 2015). The gonorrhea incidence then increased to reach 9.59 cases per 100,000 population in 2018, which is a 36.03% increase compared with the incidence in 2014 (Yue et al. 2019). Thus, gonorrhea is now an important public health issue in China. To develop effective strategies for gonorrhea prevention and control, there is a need to evaluate the seasonality and potential main determinants of seasonal fluctuations in disease patterns. However, no study has evaluated the seasonal trends of gonorrhea in China. Therefore, we performed the present study with the following aims: (1) to determine if there were any seasonal trends in gonorrhea incidence in China from 2006 to 2019; (2) to investigate the potential relationship between meteorological factors and gonorrhea infection.
Material and methods
Data sources
The gonorrhea case data were obtained from the Disease Prevention and Control Bureau (http://www.nhc.gov.cn/jkj/new_index.shtml) and the Data-Center for China Public Health Science, Chinese Center for Disease Control and Prevention (https://www.phsciencedata.cn/Share/), and the incidence of gonorrhea in China from 1 January 2006 to 31 December 2019 was analyzed.
Gonorrhea is diagnosed based on the following three aspects: epidemiological history, clinical manifestations, and laboratory findings. A positive epidemiological history includes: a history of unsafe sex, multiple sexual partners or sexual partners with infections, or a history of close contact with a person with gonorrhea; children with a history of sexual abuse; newborns whose mothers have a history of gonorrhea. Clinical manifestations include urethritis for males, and cervicitis, urethritis, vestibular adenitis, and perianal inflammation for females. Positive laboratory findings include: (1) gram-positive diplococcus on microscopic examination; (2) positive Neisseria gonorrhoeae culture; (3) positive nucleic acid test for N. gonorrhoeae. Gonorrhea is suspected in patients with a positive epidemiological history and clinical manifestations, and is definitively diagnosed when a suspected case has one of the positive laboratory findings (Wang et al. 2020).
Meteorological data from the same period were obtained from the South China Meteorological Data Sharing Center, including the monthly average temperature, relative humidity, atmospheric pressure, sunshine hours, rainy days, and precipitation.
Study design
This was an ecological study in epidemiology that analyzed aggregate gonorrhea, meteorological, and socioeconomic data from 1 January 2006 to 31 December 2019 in Chinese mainland. Gonorrhea time-series data were analyzed and the seasonality of gonorrhea was analyzed by the ratio-to-moving average method (Kakran et al. 2015) and seasonal subseries plots.
A secondary analysis was performed to correlate the number of patients with gonorrhea and meteorological factors using the Spearman assay, and the attributable risks of meteorological indexes on gonorrhea cases was analyzed using the distributed lag non-linear model (DLNLM).
Ratio-to-moving average method
Seasonal indices were calculated quarterly using standard methods (Croxton 1944). The first to fourth quarters were defined as January to March, April to June, July to September, and October to December, respectively.
The basis of the moving average ratio method is the multiplication model Y = T × S × C × E, where T is the long-term change trend, S is the seasonal change trend, C is the periodic change trend, and E is the irregular random change. The following calculation steps were used:
-
(1)
The four-quarter moving average was used to eliminate seasonal changes and irregular changes, and the T × C value was calculated.
-
(2)
Y / (T × C) was calculated to obtain the estimated value (S × E) of seasonal and irregular changes (the moving average ratio).
The seasonal index of the moving average of each season was calculated and corrected by averaging the moving average ratio of the same season in previous years, remove the influence of the irregular change E from S × E, and obtaining the estimated value of the seasonal change S, which is the seasonal index.
Seasonal subseries plots
Seasonal subseries plots are a specialized graphical technique that detects seasonality in a time series. This technique was used to detect the seasonality of gonorrhea cases. Excel was used to make a cycle plot; the Excel functions “sum of”, “average”, “offset”, and “trend offset” were used to calculate and plot the averages and trends for different quarters (Kyd 2008).
Analysis of the effect of meteorological factors on gonorrhea cases using the distributed lag non-linear model
The general Poisson distribution was used as the connection function of the DLNM to fit the time series of gonorrhea onset and meteorological factors. Other potential risk factors (including time, season, relative humidity, air pressure, sunshine hours, rainy days, and precipitation) were also incorporated into the model.
Yt is the number of new onset gonorrhea cases in the t-th month; α is the intercept; Tt, l is obtained by the cross basis function in the DLNM matrix of monthly average temperature (l is the number of months of temperature lag); β is the coefficient vector of the matrix Tt, l; ns represent natural cubic spline function, which used to generate the B-spline basis matrix for a natural cubic spline; time is the sequence of months in the study period (1, 2, …, 156); RH is the average monthly relative humidity; Rainday is the average monthly number of rainy days; Rainfall is the average monthly rainfall.
In accordance with the principle of minimizing partial autocorrelation function, the degree of freedom (df) of time was set to 1 df/year (i.e., df = 1 × 13 = 13) to control the long-term and seasonal trends. The temperature df = 3, relative humidity df = 7, pressure df = 6, sunshine hours df = 3, monthly rainy days df = 4, and precipitation df = 6. In the cross-basis function, the distribution functions of temperature (t) and lagging months (l) were set to ns, df = 6, the number of knots nodes was 5 (temperature distribution was uniformly set); the maximum number of lagging months was set to 6, df = 4, and the number of knots nodes was set uniformly using the log knots function. The effect value was estimated with the median level of the monthly mean temperature as a reference.
Statistical methods
The statistical analysis was performed using R software (version 3.6.1). The DLNLM was implemented using the “DLNM” package. The statistical tests were two-sided, with the mean value set at 0.05.
Patient and public involvement
Patients or the public WERE NOT involved in the design, or conduct, or reporting, or dissemination plans of our research.
Results
Overview of gonorrhea infection from January 2006 to December 2019
The overall number of gonorrhea cases showed a U-shaped trend, with a significant decrease from 2006 (156,679) to 2012 (69,365) and rebound reaching 140,655 in 2017 (Fig. 1). The baseline characteristics of the aggregate gonorrhea cases are showed in Fig. 1 (age distribution) and Fig. 1 (regional distribution). Most patients with gonorrhea were in the sexually active age group of 16–49 years and lived in East and South China, which are economically developed areas.
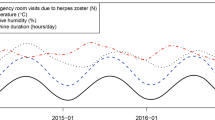
The national monthly average temperature, relative humidity, air pressure, sunshine hours, rainy days, and rainfall showed significant seasonal cyclic changes (Supplementary Fig. 1).
Seasonal variation of gonorrhea cases from January 2006 to December 2019
Similar to the seasonality seen with the ratio-to-moving average method, the seasonal subseries plots showed that the number of gonorrhea cases peaked in the third quarter and declined in the first quarter. The average number of gonorrhea cases was highest (32,541.07) in the third quarter and lowest (26,437.64) in the first quarter (Fig. 2).
Table 1 shows the overall seasonal indices after seasonal adjustment of the data from 2006 to 2019. A decrease in gonorrhea cases occurred in the first quarter of each year. The seasonally adjusted average ratio of gonorrhea cases was highest in the third quarter (108.78%) followed by the fourth quarter (105.07%), while a trough was observed in the second quarter (99.11%) and first quarter (87.03%).
Correlation between gonorrhea infection and meteorological factors
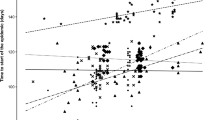
The results of the Spearman assay showed that the reported number of patients with gonorrhea was positively correlated with temperature, relative humidity, precipitation, and number of rainy days, all of which were simultaneously included in the model (Fig. 3).
Lag effects evaluated by the distributed lag non-linear model
Lag effects of monthly mean temperature on the risk of gonorrhea onset
In the model with a lag time of 0 month, the risk of gonorrhea onset was high at 6–11 °C, with a significant difference compared with the annual average temperature of 13 °C. The risk of gonorrhea onset was highest at 7 °C (relative risk [RR]: 1.145; 95% confidence interval [CI]: 1.028–1.274); that is, compared with the risk of gonorrhea onset at an average monthly temperature of 13 °C, the risk of gonorrhea onset was increased by 14.5% at an average monthly temperature of 7 °C. The risk of gonorrhea onset was the second highest at an average monthly temperature of 6 °C (RR: 1.135; 95% CI: 1.005–1.282) (Fig. 4A).
In the model with a lag time of 1 month, the risk of gonorrhea onset was high at 7–11 °C, and significantly differed at various temperatures. The risk of gonorrhea onset was highest at an average monthly temperature of 7 °C (RR: 1.108; 95% CI: 1.006–1.219), followed by an average monthly temperature of 8 °C (RR: 1.097; 95% CI: 1.015–1.186) (Fig. 4B).
The risk of gonorrhea onset did not significantly differ in accordance with the average monthly temperature in other lag time models (Fig. 4C–G).
Lag effects of monthly mean temperature on the cumulative risk of gonorrhea onset
The cumulative risk of gonorrhea onset was high at 6–11 °C, and the RR at 7 °C with a lag time of 2 months was 1.362 (95% CI: 1.025–1.809). The difference was statistically significant compared with the annual average temperature of 13 °C, and the effect lasted for up to 2 months (Supplementary Fig. 2A–C).
At 8–10 °C, the impact of temperature lasted for 3 months. In the model with a lag time of 3 months (Supplementary Fig. 2A–D), the RRs of the cumulative risks of gonorrhea onset at 8 °C, 9 °C, and 10 °C were 1.377 (95% CI: 1.008–1.881), 1.285 (95% CI: 1.023–1.615), and 1.180 (95% CI: 1.017–1.369), respectively.
The estimation of the cumulative relative risk of gonorrhea onset after a monthly average temperature of 8 °C for 3 months showed that the RR was 1.377, and 95% CI was 1.008–1.881; that is, relative to an average monthly temperature of 13 °C, the cumulative risk of gonorrhea onset after 3 months with an average temperature of 8 °C was increased by 37.7%.
Extreme temperature analysis
The national monthly average temperature was 11.80 ± 9.23 °C (range − 5.61 °C to 24.61 °C) and the median annual temperature was 13 °C. The 2.5 percentile of the annual temperature (− 3 °C) was defined as the extremely low temperature to estimate the effect of low temperature, while the 97.5 percentile of the annual temperature (24 °C) was defined as the extremely high temperature to estimate the effect of high temperature. The results showed that neither an extremely low temperature nor an extremely high temperature had an effect on the incidence of gonorrhea (Supplementary Table 1).
Attributable risks of gonorrhea due to short-term temperature exposure
Using the “backward perspective” method, the monthly average temperature of 13 °C was set as the baseline exposure level, and the cumulative lag was set between 0 and 6 months. The attribute number was 86,518 gonorrhea cases due to exposure to temperatures of 5–12 °C (95% CI: − 71,224 to 244,560), and the attribution score was 5.02% (95% CI: − 3.84%, 13.88%).
Discussion
Gonorrhea is caused by N. gonorrhoeae and is one of the most common STDs worldwide. Gonococcal infections are asymptomatic in 10% of males and most females (Detels et al. 2011), which exacerbates transmission. As antibiotic treatment of gonorrhea is effective, the focus is on prevention and control, which requires good understanding of the mechanism of disease transmission.
Seasonal variation in gonorrhea incidence has been reported in many countries; however, the seasonality varies. Cornelius (1971) first reported that the incidence of gonorrhea in the USA is highest in the third quarter and lowest in the first quarter, which is the same as the present findings in China. In contrast, the number of gonorrhea cases in India is highest in the second quarter and lowest in the fourth quarter (Kakran et al. 2015). Gonorrhea is most prevalent in the summer months in Israel from 1978 to 2008 (Mimouni et al. 2010). Aside from the meteorological factors related to the geographical environment, the differences between countries in the seasonality of gonorrhea may be associated with the sexual behavior and humanities and social habits of local populations. For example, the highest reported gonorrhoea incidence is from January to May in Burkina Faso of West Africa, which correlates with the harvest season and reflects increased sexual contact among young, mobile men (Damiba et al. 1990). India has the highest culture-positive gonorrhea incidence in the second quarter followed by the third quarter, which represent summer vacation periods for schools and colleges, and celebrations and social gatherings after harvesting in April; both factors are associated with increased sexual activity and partner changes (Kakran et al. 2015). Shah et al. (2007) reported significant 3‐month cycles for all STDs (including gonorrhea), with prominent peaks evident in March, May, August, and November from 1999 to 2003 in the USA. The authors proposed that the March and May peaks may be associated with the sexual activities of young adults during spring break, the August peak is representative of summer sexual activity of youths during school recess, and the November peak may be an expression of an endogenous annual rhythm in human biology, characterized by elevated levels of testosterone in young males (Shah et al. 2007). In the UK, an increase in sexual activity and unsafe sex occurs at or around the Christmas period, and a longer but less pronounced subsidiary period of increased sexual activity and unsafe sex coincides with the summer vacation period (Wellings et al. 1999). However, no study has investigated the relationship between the seasonality of gonorrhea numbers and the season itself (i.e., the meteorological factors). Therefore, the current study investigated the effects of meteorological factors (monthly average temperature, relative humidity, atmospheric pressure, sunshine hours, rainy days, and precipitation) on the incidence of gonorrhea.
The present study was the first to assess the seasonal variation of gonorrhea in China. We found that the number of patients with gonorrhea was positively correlated with temperature, relative humidity, and precipitation, which provides a better understanding of the seasonal trends of N. gonorrhoeae infection, resulting in better implementation of the optimal control strategies for this STD.
The DLNM not only considers the hysteresis effect of exposure factors, but also considers the nonlinear relationship between exposure and response, which is suitable for the study of health effects of time-series data like temperature (Gasparrini et al. 2015; Gasparrini & Leone 2014; Kim et al. 2019). We established this DLNM and found that compared with the average monthly temperature of 13 °C, the risk of gonorrhea onset was most increased at 7 °C (risk increased by 14.5%), followed by 6 °C, and the cumulative risk of 3 months at 8 °C was increased by 37.7%. Therefore, the risk of gonorrhea infection was highest at the temperature range of 6–11 °C, and more attention should be paid to the temperature exposure in the past 3 months of individuals with unsafe sexual behavior.
The attribution score of temperature to gonorrhea infection was 5.02% for exposure at 5–12 °C. The influence of meteorology on this infectious disease is consistent with that of a previous study that reported an attribution score of less than 18% (Ma et al. 2020). The present study confirmed the effects of temperature on reported gonorrhea cases, which is worthy of more attention because a relatively small percentage (5.02%) of cases attributable to temperature causes a huge actual absolute number of potentially infected persons (more than 85,000).
The present study has the following limitations. First, the incidence data were based on monthly aggregation; incidence data with a higher resolution (such as the daily incidence) obtains much more accurate results. Second, based on the analysis of national data, exposure levels vary widely among regions. Further studies with accurate data from each area and time are necessary. As the meteorological factors contribute to less than 20% of the variation in infection transmission (Ma et al. 2020), a complex model including multiple biomedical environmental and social factors should be considered.
In conclusion, the present study shows that the reported number of gonorrhea cases was positively correlated with temperature and humidity, and reached a peak in July–September, followed by October–December. However, the seasonality of reported gonorrhea cases is not particularly obvious, suggesting that sexual behavior or other social economic factors may interfere or weaken the effect of meteorological factors on the disease. The present findings suggest that increased emphasis should be placed on screening for gonorrhea infection during summer and autumn, and that education on safe sexual behavior should be promoted during these times.
Data availability
The data of gonorrhea cases were obtained from the Disease Control and Prevention Bureau (http://www.nhc.gov.cn/jkj/new_index.shtml) and the Data-Center for China Public Health Science, Chinese Center for Disease Control and Prevention (https://www.phsciencedata.cn/Share/). The meteorological data of the same period were obtained from the South China Meteorological Data Sharing Center. The data that support the findings of this study are available from Dr. Jin Bu (dr.jinbu@gmail.com) upon reasonable request.
References
Cornelius CE 3rd (1971) Seasonality of gonorrhea in the United States. HSMHA Health Rep 86:157–160
Croxton FECD (1944) App gen stats. Prentice-Hall Inc, New York
Damiba AE, Vermund SH, Kelley KF (1990) Rising trend of reported gonorrhoea and urethritis incidence in Burkina Faso from 1978 to 1983. Trans R Soc Trop Med Hyg 84:132–135
Detels R, Green AM, Klausner JD, Katzenstein D, Gaydos C, Handsfield H, Pequegnat W, Mayer K, Hartwell TD, Quinn TC (2011) The incidence and correlates of symptomatic and asymptomatic Chlamydia trachomatis and Neisseria gonorrhoeae infections in selected populations in five countries. Sex Transm Dis 38:503–509
Gasparrini A, Leone M (2014) Attributable risk from distributed lag models. BMC Med Res Methodol 14:55
Gasparrini A et al (2015) Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet (london, England) 386:369–375
Gong XD, Ye SZ, Zhang JY, Zhang GC, Shao CG, Liang GJ, Jiang WH, Xia Q, Wang QP (2002) Epidemiological situation of sexually transmitted disease in China: from 1991 to 2001. Chin J Dermatol 35:178–182 ((in Chinese))
Gong XD, Yue XL, Jiang N, Teng F, Men PX, Li J, Wang J (2015) Epidemiological characteristics and trends of gonorrhea in China from 2000 to 2014. Chin J Dermatol 48:301–306 ((in Chinese))
Kakran M, Bala M, Singh V (2015) An analysis of underlying factors for seasonal variation in gonorrhoea in India: a 6-year statistical assessment. Indian J Med Microbiol 33:215–220
Kim Y, Ratnam JV, Doi T, Morioka Y, Behera S, Tsuzuki A, Minakawa N, Sweijd N, Kruger P, Maharaj R, Imai CC, Ng CFS, Chung Y, Hashizume M (2019) Malaria predictions based on seasonal climate forecasts in South Africa: a time series distributed lag nonlinear model. Sci Rep 9:17882
Kyd C (2008). How to Create Cycle Plots in Excel to Chart Seasonal Sales Data. https://exceluser.com/2472/
Ma Y, Zhao Y, Liu J, He X, Wang B, Fu S, Yan J, Niu J, Zhou J, Luo B. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China (2020) Sci Total Environ 724:138226. https://doi.org/10.1016/j.scitotenv.2020.138226
Mimouni D, Bar-Zeev Y, Davidovitch N, Huerta M, Balicer RD, Levine H, Ankol O, Grotto I (2010) Secular trends of gonorrhea in young adults in Israel: three decades of follow-up. Eur J Clin Microbiol Infect Dis 29:1111–1115
Ross JD, Scott GR (1992) Seasonal variation in gonorrhoea. Eur J Epidemiol 8:252–255
Schroeder B, Tetlow P, Sanfilippo JS, Hertweck SP (2001) Is there a seasonal variation in gonorrhea and chlamydia in adolescents? J Pediatr Adolesc Gynecol 14:25–27
Shah AP, Smolensky MH, Burau KD, Cech IM, Lai D (2007) Recent change in the annual pattern of sexually transmitted diseases in the United States. Chronobiol Int 24:947–960
Wang QQ, Zhang RL, Liu QZ, Xu JH, Su XH, Yin YP, Qi SZ, Xu DM, Zhou PY, Li YY, Li XF, Wu MZ, Zou XB, Yang LG, Chen XS, Gong XD, Liang GJ, Jiang L, Cheng H, Ge FQ, National Center for STD Control, Chinese Centers for Disease Control and Prevention; Committee of STD, Branch of Dermatovenereology, Chinese Medical Association; Committee of STD, Chinese Dermatologist Association (2020) National Guidelines on Diagnosis and Treatment of Gonorrhea in China (2020). Int J Dermatol Venereol 3:129–134
Wellings K, Macdowall W, Catchpole M, Goodrich J (1999) Seasonal variations in sexual activity and their implications for sexual health promotion. J R Soc Med 92:60–64
Wright RA, Judson FN (1978) Relative and seasonal incidences of the sexually transmitted diseases. A two-year statistical review. Br J Vener Dis 54:433–440
Yue XL, Gong XD, Li J, Wang YJ, Gu H (2019) Gonorrhea in China, 2018. Int J Dermatol Venereol 2:65–69
Author information
Authors and Affiliations
Contributions
BJ and CJ provided overall guidance and managed the project. LY and ZLJ set up the statistical model of the data and finished the manuscript on the basis of comments from other authors. All other authors provided data, developed models, reviewed results, provided guidance on methods, or reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bu, J., Zhou, LJ., Xiao, X. et al. Epidemiological characteristics of gonorrhea and its influential meteorological factors: a 14-year retrospective assessment in China. Environ Sci Pollut Res 29, 35434–35442 (2022). https://doi.org/10.1007/s11356-021-17823-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-17823-6