Abstract
Air pollution has become a global concern and may be hazardous to human reproductive capacity, but the impact of exposure to air pollutants on semen quality remains controversial. We performed the meta-analysis to examine the association between air pollution exposure and semen quality. We searched PubMed, Web of Science Core Collection, and Cochrane Library databases (before December 2019). We selected original epidemiological studies on humans, written and published in English, that provided quantitative information to determine the associations between air pollution and sperm parameters. A random-effects model was used when the pooled effect estimates were found to be heterogeneous (I2 > 50% or P < 0.05), otherwise, a fixed-effects model was applied. Publication bias was not evaluated for less than 10 included articles. Our meta-analysis showed that the standardised mean differences (SMDs) (95% confidence interval, 95% CI) of sperm concentration, sperm count, and sperm total motility were −0.17 (−0.20, −0.13), −0.05 (−0.08, −0.02), and −0.33 (−0.54, −0.11), respectively. However, exposure to air pollution was not related to sperm progressive motility (SMD = 0.00, 95% CI: −0.13, 0.12). The results indicated that exposure to air pollutants at a higher level was associated with impaired semen quality, including declined sperm concentration, reduced sperm count, and declined total motility. The results suggested that high level of air pollution exposure had a negative effect on semen quality. Improvement of air quality is important for enhancing semen quality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent decades, infertility has become a major clinical concern and a threat to public health (Salas-Huetos et al. 2017), affecting about 15% of reproductive age couples across the world (Inhorn and Patrizio 2015; Salas-Huetos et al. 2021). Male factors are responsible for approximately 40% of infertility cases (Legare et al. 2014). In the case of male infertility, a gradual decrease in sperm parameters, particularly of sperm count, had been reported (Organisation 1999; Salas-Huetos et al. 2018; World Health Organization 2010). Epidemiological evidence revealed that a remarkable decreasing trend was observed in the semen quality over the past decades (John Aitken 2013; Sengupta et al. 2018), including the declined sperm count (Jensen et al. 2002), poor sperm motility, and low sperm concentration (Almeida et al. 2017). These data suggested that there was a significant decrease in male fertility rates and reproductive health associating with impaired semen quality (Skakkebaek et al. 2006; Travison et al. 2007).
Currently, the causes of suboptimal semen quality are unclear, and a variety of physiological, environmental, and genetic factors may have a negative effect on male infertility by contributing to the deterioration of semen quality (Bonde 2013; Jungwirth et al. 2012; Jurewicz et al. 2014). Air pollution, environmental endocrine-disrupting chemicals, smoking cigarettes, alcohol intake, illicit drugs, obesity, and stress have been considered risk factors for the decrease in semen quality (Durairajanayagam 2018; Hammoud et al. 2010; Mendiola et al. 2014; Salas-Huetos et al. 2021). Air pollution has gained more interest owing to its deleterious health effects in humans (Beelen et al. 2014; Fathi Najafi et al. 2015; Jurewicz et al. 2018). Accumulating evidence indicated that ambient air pollutants played a pivotal role in impairing male reproductive system, including hormonal level changes, testosterone disturbances, and semen quality alteration (Huang et al. 2020; Tian et al. 2017).
Recent studies investigated the association between ambient air pollutant exposure and semen quality. Sun, S. et al. 2020 assessed the exposure to ambient particulate matter <10 micrometres (μm) in aerodynamic diameter (PM10), nitrogen dioxide (NO2), sulphur dioxide (SO2), and ozone (O3) (Sun et al. 2020) and identified that exposure to PM10 was associated with declined sperm concentration, sperm count, total motility, and progressive motility during spermatocytogenesis period in China. A study conducted in Salt Lake City showed that exposure to ambient particulate matter having a median diameter of 2.5 μm or less (PM2.5) for 2 months was negatively correlated to sperm motility (Hammoud et al. 2010). On the contrary, Hansen, C. et al. 2010 performed a cohort study and indicated that no statistically significant decrement in sperm outcomes was observed in fertile men under exposure to PM2.5 (Hansen et al. 2010). Among the results of previous studies examining the relationship between nitrogen oxide (NOx) exposure and semen quality, a negative association of NOX with sperm count was observed (Cannarella et al. 2019). However, a study conducted in the Czech Republic suggested that exposure to NOX was not related to sperm concentration, motility, or sperm count except sperm morphology (Selevan et al. 2000). These controversial associations are commonly attributed to limitations of human studies, such as specific populations and confounding factors. In addition, exposure to air pollution had detrimental effects on semen quality in animal models (Yang et al. 2019; Zhou et al. 2019), suggesting damage to male fertility. For example, high concentration of PM2.5 exposure impaired mice sperm concentration, motility, and morphology, and the decline in testosterone concentration and alteration of testosterone biosynthesis process mediated the results (Yang et al. 2019). Human and animal studies highlight the necessity of new, updated meta-analysis to provide a wide-ranging vision of the field and create a consensus on the topic.
In this meta-analysis, we aimed to summarise the high-quality evidence from published human observational studies of the effect of ambient air pollution on semen quality parameters, including sperm concentration, sperm count, total motility, and progressive motility.
Material and methods
Search strategy
We conducted a systematic search of the literature concerning exposure to air pollution and semen quality. We searched PubMed, Web of Science Core Collection, and Cochrane Library databases (before December 2019).
The following search terms were used to retrieve relevant articles:
#1: (air pollution) OR (particulate matter) OR (air pollutants) OR (suspended particulates) OR (fine particles) OR (ambient fine particulate matter) OR PM2.5 OR PM10 OR (particle concentration) OR (gaseous pollutants) OR (sulfur dioxide) OR (nitrogen dioxide) OR ozone OR (carbon monoxide) OR smog
#2: (semen quality) OR (sperm quality) OR (sperm count) OR (sperm motility) OR (sperm morphology) OR (normal morphology) OR (sperm volume) OR (sperm concentration) OR (semen concentration) OR (total sperm number) OR (sperm viability) OR (sperm vigour) OR (sperm progressive motility) OR (total motility)
#3: #1 and #2
Two independent reviewers examined the titles and abstracts identified by electronic searches to select potentially relevant studies.
Inclusion and exclusion criteria
Only articles written in English were included. Articles were considered for inclusion in the current meta-analysis if (1) they were epidemiological studies on humans providing the quantitative information to determine the associations between the air pollution and sperm parameters and if (2) they presented the mean and standard deviation (SD) of the sperm parameters.
The exclusion criteria were as follows: (1) studies that did not investigate the association between air pollution and semen quality were excluded after the preliminarily prescreening. (2) When the articles focused on the animal assays or concentrated on mechanism research, they would be excluded. (3) If the study was not an original one, such as a review, a report, or a comment, it would be excluded.
Data extraction
All data were extracted by two independent investigators. For the eligible articles, the recorded date included a full description of study characteristics: the first author, publication year, location studied, design of studies, sample size, age of the population studied, the air pollutants, effect size, and the main conclusion. We also extracted the mean and SD of the sperm parameters exposed by the highest and the lowest levels of air pollution in the included articles.
Quality assessment
The quality of the included studies was evaluated by the Newcastle–Ottawa Scale for cohort studies, while the adapted form of the Newcastle–Ottawa Scale for cross-sectional studies (He et al. 2017; Herzog et al. 2013). We considered the following items: the selection, the comparability, and the outcome of the study.
Statistical analysis
The analysis was conducted by Stata software 16.0, and P-value < 0.05 was considered statistically significant. Standard mean differences (SMDs) and their corresponding 95% confidence intervals (95% CIs) were used to assess the influence of air pollutants on sperm parameters. The heterogeneity of included studies was estimated by I2 statistics tests. A random-effects model was selected when the effect estimates were found to be heterogeneous (I2 > 50% or P < 0.05), otherwise, a fixed-effects model was applied. A sensitivity analysis was conducted after sequentially excluding each study to assess the stability of the results. Publication bias was not assessed for the less than 10 included studies (Nasser 2020).
Results
Literature retrieval and study characteristics
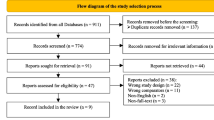
In total, we obtained 5136 articles from electronic bibliographic databases: PubMed (4154 articles), Web of Science Core Collection (966 articles), and Cochrane Library databases (16 articles). Duplicated articles were removed automatically and 4731 articles remained. Among them, 247 studies were removed for not being published in English. By reviewing the titles and/or abstracts, we excluded 4139 studies that were not related to the research subject. A total of 171 studies were animal studies, and 90 articles were reviews, so we excluded them. Eighty-four articles were considered potentially eligible. Fifty-eight of them were excluded from the exposures, and outcomes were not entirely consistent with the subject. Eventually, 6 of the remaining studies providing the mean and SD of sperm parameters were included in the final analysis (Fig. 1).
The characteristics of the included 6 studies are presented in Table 1. Of these, 4 studies used cross-sectional design and 2 were cohort studies. The total participants included ranged from 48 to 1759. These studies were conducted in China, Czech, and Italy. Four studies assessed the exposure of PM10, SO2, and NOx; while 2 studies evaluated carbon monoxide (CO). One of the studies covered PM2.5, O3, and polycyclic aromatic hydrocarbons (PAH). The sperm parameters in the included studies were analysed according to the World Health Organization laboratory manual guidelines published in 1999 and 2010 (Organisation 1999; World Health Organization 2010). According to the reported sperm parameters, the number of papers included in each meta-analysis was different: 6 provided data on sperm count, 5 on sperm concentration, 4 on sperm total motility, and 3 on sperm progressive motility.
In each study, we collected the original mean and SD of sperm parameters from the highest and lowest levels of exposure groups. The criteria of the high or low levels were not completely consistent in the meta-analysis.
Quality evaluated
Newcastle–Ottawa Scale and the adapted form of the Newcastle-Ottawa Scale were used for the evaluation of included studies. Studies with more than a score of 5 were classified as good quality studies. The six studies meet the criterion.
Sperm concentration
In the present analysis, a total of 3206 samples were used in exploring the association between exposure to air pollution and sperm concentration. The fixed-effects model was used to analyse the overall result; the I2 statistic was 48.0% and the P-value was 0.061. The overall SMD for sperm concentration was −0.17 (95% CI: −0.20, −0.13) (Fig. 2). The results showed that exposure to air pollution had a link with decreased sperm concentration. The random-effects model showed a similar result that air pollution was statistically significantly associated with sperm concentration. A sensitivity analysis was carried out by sequentially excluding each study, and similar results were presented in Table S1. There was a large overlap in the confidence intervals. The effect estimates supported the negative association between air pollution exposure and sperm concentration consistently.
Sperm count
A total of 4465 participants, including 3370 samples, were analysed for sperm count (Table 1). The mean sperm count ranged from 34.33 to 278.1 million/ml. For the I2 was 45.9%, we applied the fixed-effects model to analyse the effect. As shown in Fig. 3, the overall SMD for sperm count was −0.05 (95%CI: −0.08, −0.02). The result showed that high levels of air pollution exposure were statistically significantly associated with the reduced sperm count. We conducted the subgroup analysis of air pollution exposure by location. The SMD of studies conducted in Italy and Czech were −0.21(95% CI: −0.49, 0.08) and 0.01 (95% CI: −0.26, 0.27), respectively, which showed no relationship between air pollution exposure and the risk of decreasing sperm count. After omitting each study in sequence, we obtained similar results (Table S2). The sensitivity analysis indicated that the results in the present analysis were robust.
Sperm total motility
Four of the included studies provided information on sperm total motility. For high heterogeneity (I2 was 97.0%), the random-effects model was applied to assess the relationship between air pollution exposure and sperm total motility. According to the overall SMD −0.33 (95% CI: −0.54, −0.11) (Fig. 4), we suggested that exposure to air pollution at a higher level was significantly related to the deteriorating tendency of sperm total motility.
To explore the reasons for high heterogeneity, we performed a subgroup analysis according to the design of relevant studies. In two cohort studies, the value of I2 was reduced to 33.6%, while the heterogeneity estimate was not materially affected in cross-sectional studies. The results in sensitivity analysis after one-by-one elimination were not significantly different (Table S3), indicating the funding of the original analysis was reliable.
Sperm progressive motility
Three of the included studies providing 6 sets of data studying the relationship between air pollution and sperm progressive motility. Because the I2 was 91.0%, the random-effects model was applied to the meta-analysis. No association between air pollution and progressive motility was observed with a pooled SMD 0.00 (95% CI: −0.13, 0.12) (Fig. 5). After the omission of a single article one by one (Table S4), we obtained statistically steady results and the analysis was robust.
Discussion
In the present study, 6 studies out of a total of 5136 articles were included to explore the association between air pollution and semen quality. We found that air pollution had a deleterious effect on sperm concentration (SMD: −0.17, 95%CI: −0.20, −0.13), sperm count (SMD: −0.05, 95%CI: −0.08, −0.02), and sperm total motility (SMD: −0.33, 95% CI: −0.54, −0.11). No evidence showed that air pollution exposure reduced sperm progressive motility (SMD: 0.00, 95% CI: −0.13, 0.12). The consistent direction of SMD was verified by sensitivity analysis after one-by-one elimination, which adds confidence to the findings.
In humans, the whole process of spermatogenesis is estimated to be 90 days (Zhang et al. 2019). Therefore, the data of air pollutants exposure for the 90-day period preceding sampling were considered relevant. In previous studies, Wu et al. 2017 retrospectively assessed the exposures of pollutants during the important 90 days and reported that there were significant associations between particulate matter (PM) exposure and sperm concentration and count during the entire period of sperm development (Wu et al. 2017). Consistent with our results, a negative effect of SO2 exposure on the sperm concentration and count was observed by Liu et al. in Wuhan, China (Liu et al. 2017). However, the same results were not replicated in Rube et al. (Rubes et al. 2005). No significant association between air pollution exposure and sperm concentration or count was found (Selevan et al. 2000). The difference in characteristics of the study population, study areas, air pollution mix, and sources in multiple geographic locations and approaches of exposure assessment might be an explanation as to the inconsistent findings (Dionisio et al. 2016; Hammoud et al. 2010; Lao et al. 2018; Zhou et al. 2019). Cannarella et al. (2019) did not indicate the time of exposure time and analysed the environmental concentrations of SO2, NO2, NOx, CO, and O3 according to the Regional Agency for Environmental Protection (ARPA) in Italy, no association between air pollution exposure and semen quality was found except sperm count. Boggia et al. only collected data of NO2 exposure continuous for 30 days (Boggia et al. 2009), and a significant decline of sperm total motility was observed in workers who were occupationally exposed to NO2. In our meta-analysis, the declined sperm total motility was also found at a high exposure level.
Although considerable evidence supported the health effects of air pollution on semen quality (Hansen et al. 2010; Yang et al. 2019), the direct etiological mechanisms between air pollution and the impaired semen quality need to be determined. PM2.5 has gained more interest for the large surface areas and the capacity of carrying various toxic stuff and multiple trace elements (Jurewicz et al. 2018; Xing et al. 2016). Spermatogenesis is sensitive to oxidative stress particularly (Aitken et al. 2015; Du Plessis et al. 2015), and PM2.5 could cause oxidative stress to damage semen quality (Weichenthal et al. 2013). PM2.5 exposure could also induce apparent DNA damages and histopathologic changes in the testes, resulting in abnormal semen parameters in mice (Zhou et al. 2019). The exposure to diesel exhaust PM2.5 (DEP) probably targeting the spermatogenetic meiosis disturbed spermatogenesis thus semen quality (Yang et al. 2019). Meanwhile, the implication of the hypothalamic-pituitary-gonadal (HPG) axis might be a crucial mediator for adverse effects of PM2.5 exposure on decreased semen quality. It influenced the levels of hormones which is critical to the development of spermatogenesis (Fathi Najafi et al. 2015). Further studies are needed to explore potential biological mechanisms between PM exposure and decreased semen quality, which might explain the potential reasons for male infertility.
There are several strengths of this study. Firstly, our study had well-defined inclusion and exclusion criteria. Secondly, the low heterogeneity in sperm concentration and count raised the reliability of the results. We conducted a subgroup analysis of study designs, which could explain the high heterogeneity in sperm total motility. Our study supported the conclusion that air pollution might have an adverse effect on semen quality. However, the limitations of the study should be considered. The available data did not consider confounding factors affecting semen quality, such as age and smoking status. In addition, only 6 articles were included according to the criterion, which may lead to some bias. Thus, more studies related to the subject of effects of air pollution on semen quality are still required.
Conclusion
In conclusion, this meta-analysis of epidemiological studies indicated that a higher level of air pollution exposure was associated with lower semen quality, especially sperm concentration, sperm count, and sperm total motility. However, no statistical difference was observed on sperm progressive motility. The results suggested that air quality should be considered a significant factor for semen quality. Observational studies can prove associations but not demonstrate causation, and more attention should be paid to confirm the associations summarised in the present meta-analysis. Longitudinal studies and randomised controlled trials of high quality will then be required to evaluate the causal relationship between air pollution and semen quality.
Data availability
Not applicable.
References
Aitken RJ, Baker MA, Nixon B (2015) Are sperm capacitation and apoptosis the opposite ends of a continuum driven by oxidative stress? Asian J Androl 17:633–639. https://doi.org/10.4103/1008-682X.153850
Almeida S, Rato L, Sousa M, Alves MG, Oliveira PF (2017) Fertility and sperm quality in the aging male. Curr Pharm Des 23:4429–4437. https://doi.org/10.2174/1381612823666170503150313
Beelen R, Stafoggia M, Raaschou-Nielsen O, Andersen ZJ, Xun WW, Katsouyanni K, Dimakopoulou K, Brunekreef B, Weinmayr G, Hoffmann B, Wolf K, Samoli E, Houthuijs D, Nieuwenhuijsen M, Oudin A, Forsberg B, Olsson D, Salomaa V, Lanki T, Yli-Tuomi T, Oftedal B, Aamodt G, Nafstad P, de Faire U, Pedersen NL, Östenson CG, Fratiglioni L, Penell J, Korek M, Pyko A, Eriksen KT, Tjønneland A, Becker T, Eeftens M, Bots M, Meliefste K, Wang M, Bueno-de-Mesquita B, Sugiri D, Krämer U, Heinrich J, de Hoogh K, Key T, Peters A, Cyrys J, Concin H, Nagel G, Ineichen A, Schaffner E, Probst-Hensch N, Dratva J, Ducret-Stich R, Vilier A, Clavel-Chapelon F, Stempfelet M, Grioni S, Krogh V, Tsai MY, Marcon A, Ricceri F, Sacerdote C, Galassi C, Migliore E, Ranzi A, Cesaroni G, Badaloni C, Forastiere F, Tamayo I, Amiano P, Dorronsoro M, Katsoulis M, Trichopoulou A, Vineis P, Hoek G (2014) Long-term exposure to air pollution and cardiovascular mortality: an analysis of 22 European cohorts. Epidemiology 25:368–378. https://doi.org/10.1097/EDE.0000000000000076
Boggia B, Carbone U, Farinaro E, Zarrilli S, Lombardi G, Colao A, De Rosa N, De Rosa MJJoei (2009): Effects of working posture and exposure to traffic pollutants on sperm quality. 32, 430-434
Bonde JP (2013) Occupational causes of male infertility. Current opinion in endocrinology, diabetes, and obesity 20, 234-239.doi: https://doi.org/10.1097/MED.0b013e32835f3d4b
Cannarella R, Liuzzo C, Mongioi LM, Condorelli RA, La Vignera S, Bellanca S, Calogero AE (2019) Decreased total sperm counts in habitants of highly polluted areas of Eastern Sicily, Italy. Environmental science and pollution research international 26:31368–31373. https://doi.org/10.1007/s11356-019-06248-x
Dionisio KL, Baxter LK, Burke J, Özkaynak HJAQ, Atmosphere, Health (2016) The importance of the exposure metric in air pollution epidemiology studies: when does it matter, and why? 9, 495-502
Du Plessis SS, Agarwal A, Halabi J, Tvrda E (2015) Contemporary evidence on the physiological role of reactive oxygen species in human sperm function. J Assist Reprod Genet 32:509–520. https://doi.org/10.1007/s10815-014-0425-7
Durairajanayagam D (2018) Lifestyle causes of male infertility. Arab J Urol 16:10–20. https://doi.org/10.1016/j.aju.2017.12.004
Fathi Najafi T, Latifnejad Roudsari R, Namvar F, Ghavami Ghanbarabadi V, Hadizadeh Talasaz Z, Esmaeli M (2015) Air pollution and quality of sperm: a meta-analysis. Iranian Red Crescent medical journal 17:e26930. https://doi.org/10.5812/ircmj.17(4)2015.26930
Hammoud A, Carrell DT, Gibson M, Sanderson M, Parker-Jones K, Peterson CM (2010) Decreased sperm motility is associated with air pollution in Salt Lake City. Fertil Steril 93:1875–1879. https://doi.org/10.1016/j.fertnstert.2008.12.089
Hansen C, Luben TJ, Sacks JD, Olshan A, Jeffay S, Strader L, Perreault SD (2010) The effect of ambient air pollution on sperm quality. Environ Health Perspect 118:203–209. https://doi.org/10.1289/ehp.0901022
He D, Wu S, Zhao H, Qiu H, Fu Y, Li X, He Y (2017) Association between particulate matter 2.5 and diabetes mellitus: a meta-analysis of cohort studies. J Diabetes Investig 8:687–696. https://doi.org/10.1111/jdi.12631
Herzog R, Alvarez-Pasquin MJ, Diaz C, Del Barrio JL, Estrada JM, Gil A (2013) Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 13:154. https://doi.org/10.1186/1471-2458-13-154
Huang G, Zhang Q, Wu H, Wang Q, Chen Y, Guo P, Zhao Q (2020) Sperm quality and ambient air pollution exposure: a retrospective, cohort study in a Southern province of China. Environmental research 188:109756. https://doi.org/10.1016/j.envres.2020.109756
Inhorn MC, Patrizio P (2015) Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update 21:411–426. https://doi.org/10.1093/humupd/dmv016
Jensen TK, Carlsen E, Jorgensen N, Berthelsen JG, Keiding N, Christensen K, Petersen JH, Knudsen LB, Skakkebaek NE (2002) Poor semen quality may contribute to recent decline in fertility rates. Hum Reprod 17:1437–1440. https://doi.org/10.1093/humrep/17.6.1437
John Aitken R (2013) Falling sperm counts twenty years on: where are we now? Asian J Androl 15:204–207. https://doi.org/10.1038/aja.2012.167
Jungwirth A, Giwercman A, Tournaye H, Diemer T, Kopa Z, Dohle G, Krausz C, European Association of Urology Working Group on Male I (2012) European Association of Urology guidelines on male infertility: the 2012 update. Eur Urol 62:324–332. https://doi.org/10.1016/j.eururo.2012.04.048
Jurewicz J, Radwan M, Sobala W, Radwan P, Bochenek M, Hanke W (2014) Effects of occupational exposure - is there a link between exposure based on an occupational questionnaire and semen quality? Syst Biol Reprod Med 60:227–233. https://doi.org/10.3109/19396368.2014.907837
Jurewicz J, Dziewirska E, Radwan M, Hanke W (2018) Air pollution from natural and anthropic sources and male fertility. Reproductive biology and endocrinology : RB&E 16:109. https://doi.org/10.1186/s12958-018-0430-2
Lao XQ, Zhang Z, Lau AKH, Chan TC, Chuang YC, Chan J, Lin C, Guo C, Jiang WK, Tam T, Hoek G, Kan H, Yeoh EK, Chang LY (2018) Exposure to ambient fine particulate matter and semen quality in Taiwan. Occup Environ Med 75:148–154. https://doi.org/10.1136/oemed-2017-104529
Legare C, Droit A, Fournier F, Bourassa S, Force A, Cloutier F, Tremblay R, Sullivan R (2014) Investigation of male infertility using quantitative comparative proteomics. J Proteome Res 13:5403–5414. https://doi.org/10.1021/pr501031x
Liu Y, Zhou Y, Ma J, Bao W, Li J, Zhou T, Cui X, Peng Z, Zhang H, Feng M, Yuan Y, Chen Y, Huang X, Li Y, Duan Y, Shi T, Jin L, Wu L (2017) Inverse association between ambient sulfur dioxide exposure and semen quality in Wuhan, China. Environmental science & technology 51:12806–12814. https://doi.org/10.1021/acs.est.7b03289
Mendiola J, Jorgensen N, Andersson AM, Stahlhut RW, Liu F, Swan SH (2014) Reproductive parameters in young men living in Rochester, New York. Fertil Steril 101:1064–1071. https://doi.org/10.1016/j.fertnstert.2014.01.007
Nasser M (2020) Cochrane Handbook for Systematic Reviews of Interventions. Am J Public Health 110:753–754. https://doi.org/10.2105/Ajph.2020.305609
Organisation WH (1999) WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. Cambridge University Press
Rubes J, Selevan SG, Evenson DP, Zudova D, Vozdova M, Zudova Z, Robbins WA, Perreault SDJHR (2005): Episodic air pollution is associated with increased DNA fragmentation in human sperm without other changes in semen quality. 20:2776-2783
Salas-Huetos A, Bullo M, Salas-Salvado J (2017) Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies. Hum Reprod Update 23:371–389. https://doi.org/10.1093/humupd/dmx006
Salas-Huetos A, Rosique-Esteban N, Becerra-Tomas N, Vizmanos B, Bullo M, Salas-Salvado J (2018) The effect of nutrients and dietary supplements on sperm quality parameters: a systematic review and meta-analysis of randomized clinical trials. Adv Nutr 9:833–848. https://doi.org/10.1093/advances/nmy057
Salas-Huetos A, Maghsoumi-Norouzabad L, James ER, Carrell DT, Aston KI, Jenkins TG, Becerra-Tomas N, Javid AZ, Abed R, Torres PJ, Luque EM, Ramirez ND, Martini AC, Salas-Salvado J (2021) Male adiposity, sperm parameters and reproductive hormones: an updated systematic review and collaborative meta-analysis. Obes Rev 22:e13082. https://doi.org/10.1111/obr.13082
Selevan SG, Borkovec L, Slott VL, Zudova Z, Rubes J, Evenson DP, Perreault SD (2000) Semen quality and reproductive health of young Czech men exposed to seasonal air pollution. Environ Health Perspect 108:887–894. https://doi.org/10.1289/ehp.00108887
Sengupta P, Borges E Jr, Dutta S, Krajewska-Kulak E (2018) Decline in sperm count in European men during the past 50 years. Hum Exp Toxicol 37:247–255. https://doi.org/10.1177/0960327117703690
Skakkebaek NE, Jorgensen N, Main KM, Rajpert-De Meyts E, Leffers H, Andersson AM, Juul A, Carlsen E, Mortensen GK, Jensen TK, Toppari J (2006) Is human fecundity declining? Int J Androl 29:2–11. https://doi.org/10.1111/j.1365-2605.2005.00573.x
Sun S, Zhao J, Cao W, Lu W, Zheng T, Zeng Q (2020) Identifying critical exposure windows for ambient air pollution and semen quality in Chinese men. Environmental research 189:109894. https://doi.org/10.1016/j.envres.2020.109894
Tian X, Wang X, Ye B, Li C, Zhang Y, Ma LJZyFyxzz (2017) The effects of exposure to ozone on sperm quality in Wuhan. 51, 197-202
Travison TG, Araujo AB, O'Donnell AB, Kupelian V, McKinlay JB (2007) A population-level decline in serum testosterone levels in American men. J Clin Endocrinol Metab 92:196–202. https://doi.org/10.1210/jc.2006-1375
Weichenthal SA, Godri-Pollitt K, Villeneuve PJ (2013) PM2.5, oxidant defence and cardiorespiratory health: a review. Environ Health 12:40. https://doi.org/10.1186/1476-069X-12-40
World Health Organization. (2010) WHO laboratory manual for the examination and processing of human semen. World Health Organization, Geneva, xiv, 271 p. pp
Wu L, Jin L, Shi T, Zhang B, Zhou Y, Zhou T, Bao W, Xiang H, Zuo Y, Li G, Wang C, Duan Y, Peng Z, Huang X, Zhang H, Xu T, Li Y, Pan X, Xia Y, Gong X, Chen W, Liu Y (2017) Association between ambient particulate matter exposure and semen quality in Wuhan, China. Environment international 98:219–228. https://doi.org/10.1016/j.envint.2016.11.013
Xing YF, Xu YH, Shi MH, Lian YX (2016) The impact of PM2.5 on the human respiratory system. J Thorac Dis 8:E69–E74. https://doi.org/10.3978/j.issn.2072-1439.2016.01.19
Yang Y, Yang T, Liu S, Cao Z, Zhao Y, Su X, Liao Z, Teng X, Hua J (2019) Concentrated ambient PM2.5 exposure affects mice sperm quality and testosterone biosynthesis. PeerJ 7:e8109. https://doi.org/10.7717/peerj.8109
Zhang H-T, Zhang Z, Cao J, Tang W-H, Zhang H-L, Hong K, Lin H-C, Wu H, Chen Q, Jiang HJAJoA (2019) Ambient ozone pollution is associated with decreased semen quality: longitudinal analysis of 8945 semen samples from 2015 to 2018 and during pollution-control period in Beijing, China. 21, 501
Zhou L, Su X, Li B, Chu C, Sun H, Zhang N, Han B, Li C, Zou B, Niu Y, Zhang R (2019) PM2.5 exposure impairs sperm quality through testicular damage dependent on NALP3 inflammasome and miR-183/96/182 cluster targeting FOXO1 in mouse. Ecotoxicol Environ Saf 169:551–563. https://doi.org/10.1016/j.ecoenv.2018.10.108
Acknowledgements
The authors would like to thank the funding support from the National Key R&D Program of China (No. 2019YFC1005106) and the National Natural Science Foundation of China (No. 82071700). We also thank the authors of included studies for the provision of data.
Funding
This work was supported by the National Key R&D Program of China (No. 2019YFC1005106), the National Natural Science Foundation of China (No. 82071700), and the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD).
Author information
Authors and Affiliations
Contributions
Hong Qian: conceptualization, data curation, writing the original draft, and software. Qiaoqiao Xu and Wenkai Yan: data execution, conceptualization, and software. Yun Fan, Zhi Li, and Chengzhe Tao: writing, reviewing, and editing. Chuncheng Lu and Feng Zhang: project administration, funding acquisition, and validation. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Not applicable.Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hong Qian, Qiaoqiao Xu and Wenkai Yan consider that the first three authors should be regarded as joint first authors.
Supplementary Information
ESM 1
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Qian, ., Xu, Q., Yan, W. et al. Association between exposure to ambient air pollution and semen quality in adults: a meta-analysis. Environ Sci Pollut Res 29, 10792–10801 (2022). https://doi.org/10.1007/s11356-021-16484-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-16484-9