Abstract
Among residents living close to agricultural fields who are potentially exposed to pesticides, pregnant women and their fetuses are of particular concern for their vulnerability to environmental chemicals. In this collaborative multicenter study, we covered a wide distribution of participants in the most important fruit production zone of north Patagonia (Argentina) to investigate whether maternal residential proximity to fruit croplands with intense pesticide applications (rural group –RG-) is associated with pregnancy complications and alterations in their newborn parameters compared to the urban population (urban group –UG-). A total of 776 pregnant women met the inclusion criteria. The percentage of threatened miscarriage was significantly higher in the RG than in the UG. The percentage of miscarriage, threat of premature labor, intrauterine fetal death, preterm premature rupture of membranes, and intrauterine growth retardation were similar in both groups. Newborn anthropometric parameters were corrected by sex and gestational age prior to statistical analysis. Length at birth and head circumference were lower in the RG than in the UG. Birth weight was similar in both groups. The percentage of head circumference less than the 5th percentile and the ponderal index were greater in the RG than in the UG. Our results suggest that proximity to pesticide applications may increase the risk of pregnancy complications and altered newborn parameters.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Many non-farmworker residents living within a short distance of agricultural fields may be exposed to spray drift emissions from pesticides designed to target field pests, both during and after applications (Rowe et al. 2016). Due to the intrinsic toxicity of pesticides, it is important to evaluate the potential health consequences in this specific population. However, to date, this issue has been little studied. Pesticides are transported mainly by wind and rain from their points of application to neighboring crops and land, and from the soil to surface and subsurface waters (Matthews and Hamey 2003; Fenik et al. 2011). Some of these pesticides, including organophosphates (OPs) and carbamates (CBMs), share at least one mode of action, the inhibition of cholinesterases, and there is in vitro evidence that the exposure to certain pesticide mixtures may have additive inhibitory effects (Mwila et al. 2013). Pesticide residues in house dust (Coronado et al. 2006; Lu et al. 2000) and pesticide metabolites in children (Babina et al. 2012; Bradman et al. 2011; Fenske et al. 2005; Muñoz Quezada et al. 2019) have been found in populations residing close to agricultural areas. Although pesticide biomarkers such as dialkyl phosphate metabolites are important tools to assess exposures to pesticides, several challenges limit their utility in epidemiological analyses. For example, many pesticides have a short half-life in the body, and biomarkers reflect only very recent exposures (in the order of hours to days) (Bradman et al. 2013).
Among residents living close to agricultural fields potentially exposed to pesticides, pregnant women and their fetuses are of particular concern for their vulnerability to environmental chemicals (Stillerman et al. 2008). One reason for this is that, during fetal development, which is a process characterized by marked cellular proliferation and development of numerous changing metabolic capabilities in the organism, there are critical windows of susceptibility during which exposures to environmental contaminants may result in adverse, permanent, and irreversible effects that can have lifelong and even intergenerational impacts on health (Woodruff et al. 2008). Therefore, during critical periods of development, exposure to pesticides can result in increased risk for pregnancy complications (Magnarelli et al. 2011) and adverse health outcomes (Béranger et al. 2020; Koureas et al. 2012; Weselak et al. 2007). In fact, decreased fetal growth (Eskenazi et al. 2004; Whyatt et al. 2004; Petit et al. 2010), decreased birth weight (BW) and length at birth (LB) (Perera et al. 2003; Rauch et al. 2012; Wohlfahrt-Veje et al. 2011), shortened gestation (Eskenazi et al. 2004; Harley et al. 2011; Jaacks et al. 2019; Parvez et al. 2018; Rauch et al. 2012; Whyatt et al. 2004), and increased risk of in utero growth restriction (Levario-Carrillo et al. 2004) and birth defects (Carmichael et al. 2014; Winchester et al. 2009) have been associated with exposure to pesticides. In addition, delayed conception, miscarriage, and stillbirths have been related to exposure to OPs (Arbuckle et al. 2001; Hanke and Jurewicz 2004; Pastore et al. 1997). Other studies have also shown that prenatal exposure to OPs may impact the neurodevelopment of newborns (Woskie et al. 2017) and pre-school children (Wang et al. 2017) and has also been associated with cognitive abilities in school-age children (Bouchard et al. 2011; Friedman et al. 2020; Rauh et al. 2011). Moreover, epidemiological studies have shown that higher nearby agricultural pesticide use (Shelton et al. 2014) and prenatal exposure to OPs (Sagiv et al. 2018) are associated with autism.
The Alto Valle del Río Negro (High Valley of Negro River), in Argentine Patagonia, is a fruit-growing zone where two periods of the year are clearly differentiated: one in which pesticides, mainly OPs, are intensively applied, known as the spraying period, and another period in which no pesticides are applied, known as the non-spraying period. To evaluate the effects of pesticides, at our lab, we have studied mothers and children residing in this area for more than fifteen years by sampling blood of pregnant women (Souza et al. 2005; Cecchi et al. 2012; Santa- Cruz et al. 2020; Vera et al. 2012). It is remarkable that, in every sampling of pregnant women’s blood, we reported plasma cholinesterase inhibition (18–23%) in the spraying period, which indicates that the population is exposed to OPs. We also studied umbilical cord blood (Quintana et al. 2017), term placentas (Bulgaroni et al. 2013; Chiapella et al. 2014; Rivero - Osimani et al. 2016; Sánchez et al. 2015; Vera et al. 2012), and saliva (Bulgaroni et al. 2012). In addition, we have recorded pregnancy complications (Santa- Cruz et al. 2020) and anthropometric parameters of newborns (Cecchi et al. 2012; Quintana et al. 2017; Rivero - Osimani et al. 2016; Santa- Cruz et al. 2020; Souza et al. 2005) in two rural localities of the area. Data for these studies were obtained both from the rural population during the spraying and non-spraying periods and from the urban population. We also conducted personal interview surveys and found that people had risk behaviors and little knowledge about pesticide applications in the area (Rovedatti et al. 2006). Additionaly, we found alterations in the antioxidant defense and immune response, as well as DNA damage and endocrine disruption (Bulgaroni et al. 2013; Cecchi et al. 2012; Quintana et al. 2017).
In this work, we conducted a collaborative multicenter study with the objective to expand the sampling covering of the Alto Valle del Río Negro in order to investigate whether maternal residential proximity to fruit croplands with intense pesticide applications is associated with pregnancy complications and alterations in their newborn parameters. This is the first study in Argentine Patagonia that compares pregnancy complications and newborn parameters between the rural and urban population by including data from most of the localities of this important fruit production zone.
Materials and methods
Characteristics of the study area
The Alto Valle del Río Negro (Fig. 1) is an artificially irrigated valley which is the Argentine region with the largest agricultural fruit production. Approximately 50,000 ha produce 1,800,000 tons of pears and apples, with 1,368,000 tons being exported (Ministry of Public Finance, Presidency of Argentina 2016). This area includes two Argentine provinces: Río Negro and Neuquén, in northern Patagonia (39° 01′1S and 67° 40′W), and comprises Neuquén city, with a population of ≅231,000 inhabitants, other localities which have between 5000 and 80,000 inhabitants, and other rural areas and small towns surrounded by farms. The soils have scarce organic matter (< 1%). The climate is continental, temperate, and arid, with annual rainfall totals of about 200 mm and frequent spring freezes. The strongest winds, which come from the west and south-west, occur in spring.
Croplands with higher productivity are small agricultural properties of 5.1–50 ha in size, where 500 tons of pesticides are applied every year for fruit pest control (FunBaPa 2010). The insecticide families mostly used in this region are OPs (such as chlorpyrifos and azinphos-methyl) and CBMs (such as carbofuran and pirimicarb). In addition, neonicotinoids (NNTs), such as tiacloprid and acetamiprid, are currently being introduced in the market. Pesticides are applied at the average fruit tree height by ground-based spraying equipment every 15 days for three/four consecutive months (October- December/January) during the dry seasons. In addition, artificial irrigation is performed by periodic flooding of the fruit orchards, which have a flat topography that would enable the transport of pesticides from the soil to surface and subsurface waters. Although an integrated pest management based on selective insecticides, biopesticides, and sexual confusion technique is also implemented in the area, several studies have reported the presence of pesticide residues in the soil (Kirs 2002), water compartments (Loewy et al. 2011; Tosi et al. 2009), and drainage channels (Macchi et al. 2018).
Population and study design
In this prospective study, healthy pregnant women between 17 and 35 years old were recruited in public hospitals of the localities of Allen, Cinco Saltos, Cipolletti, and General Roca, located in the province of Río Negro, and in public hospitals of San Patricio del Chañar and Neuquén cities, and San Lucas Clinic, located in the province of Neuquén. Pregnant women were consecutively recruited by biochemists during routine laboratory prenatal care visits from July 2009 to May 2011. They were informed about the objectives and modalities of the study and asked to sign a written informed consent in accordance with procedures approved by the Bioethics Committee of the local Advisory Committee of Biomedical Research in Humans. The study desing did not require pregnant women to attend beyond the normal prenatal care protocol. They were followed during pregnancy until delivery. At the moment of recruitment, a prenatal questionnaire designed for this study was orally administered to obtain information on the permanent residential address, sociodemographic characteristics, and lifestyle habits such as smoking, consumption of groundwater, alcohol and medicines, previous history of pesticide exposure, and domestic pesticide spraying. This last item referred to pesticide use at home, garden, or workplace and concerned the application of pesticides with a fumigation device and not the use of household aerosols.
Distance between the women’s home and the nearest cropland was estimated locating their addresses in Google Maps. Based on the above, participants were divided into two groups: the rural population group (RG) and the urban population group (UG). The RG included women living in the proximity to areas of intensive pesticide application (< 5000 m). This distance reflects a potential spray drift range likely to occur during pesticide applications (Bukasala et al. 2018; Copes 2012; van den Berg et al. 1999). The UG consisted of women residing in Neuquén city without previous history of pesticide exposure.
Women were eligible to participate in the study if they were healthy, self-reported ethnicity was Hispanic, were not involved in agricultural work, had been living in the same residential address for more than 4 years, and planned to continue receiving prenatal care at the participating health centers. Women with a multiple pregnancy, thyroidopathy, arterial hypertension, gestational diabetes, and/or cholestasis of pregnancy, as well as those exposed to X rays, on medication (except those included in Group A according to the U.S. FDA), consuming alcohol or drugs, positive for Chagas disease, HIV and/or Toxoplasmosis, and/or serious pregnancy complications such as eclampsia or preeclampsia were excluded from the study. The unit of analysis was the pregnant woman and her newborn delivered by vaginal or cesarean delivery. For sample size calculation, the percentage of women with pathological pregnancies in Neuquén province during 2006 and 2007 was obtained from the Perinatal Information System, Department of Statistics, Secretary of Health, Neuquén province, Argentina. Gynecologists and obstetricians participated by providing information about gestational length based on the last menstrual period and obstetrical adjustment by first ultrasound at 24 weeks of gestation, and about complications during pregnancy. They also provided information about weight gain during pregnancy, complications of labor and delivery, method of delivery, placental characteristics, and newborn anthropometric parameters. Incomplete data were completed revising participants’ medical charts, following the delivery of their babies.
Indicators of pregnancy alterations
Pregnancy alterations considered were threatened miscarriage, miscarriage, threat of premature labor, fetal death, preterm premature rupture of membranes (membrane rupture < 37 weeks of gestation), and intrauterine growth retardation (estimated fetal weight by ultrasound examination of < 10th percentile or birth weight of < 10th percentile for gestational age).
Fetal growth indicators
Information on birth outcomes, including BW, LB, head circumference (HC) (which is a cranial growth indicator) and neonatal sex, was retrieved. The ponderal index at birth (PI), known to be a good indicator of fetal nutrition and a measure of proportionality to reflect adiposity in infants, was calculated as the ratio of BW in grams to BL in cubic centimeters (g/cm3). Immediately after birth, the newborn’s weight (in grams) to the nearest 10 g on a calibrated pediatric scale, and length (in centimeters) were recorded. HC (in centimeters) was recorded 24–48 h after delivery. Measurements were performed using standardized procedures by trained study staff. Preterm birth was defined as delivery at < 37 weeks’ gestation. Low birth weight was defined as birth weight < 2500 g. Small for gestational age was defined as weight-for-gestational age percentile < 10 based on the INTERGROWTH-21st standards (Cheikh Ismail et al. 2013).
Statistical analysis
BW, LB, and HC were corrected by sex and gestational age by using z scores. The Z-score was estimated with a transformation of data that indicates how far and in what direction (positive vs. negative) a measured value deviates from the population 50 percentil (p50), expressed in units of the population standard deviation (SD). It is a dimensionless quantity derived from dividing the difference between individual value (x) and p50 by the population SD (σ): \( z=\frac{x-{p}_{50}}{\sigma } \) (Lejarraga and Fustiñana 1986; Wang and Chen 2012). Percentages were calculated for categorical variables, and mean and SD for quantitative variables. The normality of continuous variables was verified by the modified Shapiro-Wilks test (Mahibbur and Govindarajulu 1997). Statistical analyses of categorical variables were compared using Pearson’s chi-squared test. The Student t-test was used to compare differences in the study populations between the two study groups in variables with normal distribution. The Infostat® software was used and statistical significance was assumed as p < 0.05.
Ethics
The study was conducted in accordance with the Declaration of Helsinki of the 59th WMA General Assembly guidelines for the protection of human subjects. The study protocol was approved by the ethical committee of the local Advisory Committee of Biomedical Research in Humans.
Results
A total of 804 women met the inclusion criteria and responded the questionnaire; 21 of them were excluded from the protocol after developing preeclampsia and 7 were lost to follow-up for different reasons (mainly failure to attend programmed visits or moving before delivery). Therefore, results were based on 776 pregnant women (RG, n = 418; UG, n = 358).
Table 1 shows the description of the sociodemographic characteristics of the women enroled in the study. The average age of mothers at the time of recruitment was 25.6 years (range 17–35) in the UG and 24.6 (range 17–35) in the RG. About 60 % of the women had complete high school education background. In the UG, about 10% of women had an education background greater than high school and in the RG, about 6%. The percentage of women with only complete elementary education was twice as high in the RG as in the UG. In both groups, parity was similar, and about 12–13% of women were malnourished according to Rosso-Mardones chart used during the pre-natal control (Mardones and Rosso 1997). Alcohol intake during pregnancy was occasional, and active and passive smoking during pregnancy, groundwater consumption, and domestic pesticide spraying were greater in the RG. Within the RG, 36% of the mothers were passive smokers during pregnancy compared to 5% in the UG; 6% of women in the RG consumed alcohol once or twice a week compared to 0.6% of women in the UG.
Because recognized confounders such as malnutrition (Wigle 2008), smoking (Salihu and Wilson 2007), and alcohol consumption (Ortega-García et al. 2012) differed between the UG and the RG, we analyzed pregnancy complications and newborn’s parameters, first including and then excluding pairs of mother-babies with those characteristics (Fig. 2 and 3).
Figure 2 shows the pregnancy complications recorded. The percentage of threatened miscarriage was significantly higher in the RG than in the UG (03 vs. 3, p < 0.05). This result was still significantly higher in the RG when smokers, alcohol consumers, and malnourished women were not considered in the analysis (0 vs. 2.2, p < 0.05). The percentage of intrauterine growth retardation, preterm premature rupture of membranes, intrauterine fetal death, fetal death, threat of premature labor, and miscarriage were similar in both groups.
The placental characteristics were analyzed only in a subgroup of patients (UG, n = 42; RG, n = 83). The UG presented no abnormalities, whereas in the RG, 27% presented placental calcifications. When smokers, alcohol consumers, and malnourished women were not considered in the analysis, placental calcification represented 17% of the cases in the RG.
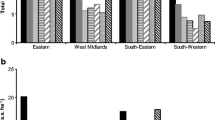
The gestational age for the UG newborns ranged from 28 to 41.5 weeks (mean 38.7 weeks, SD = 1.9 weeks) whereas that for the RG newborns ranged from 31 to 42 weeks (mean 38.0 weeks, SD = 1.5 weeks). Figure 3 shows anthropometric parameters and indexes. The PI was higher in the RG than in the UG, both when considering and not considering all participants with the criterion explained above. The ratio between HC and BW were similar in both groups. Newborn BW, LB, and HC were corrected by sex and gestational age prior to statistical analysis using Z-scores. BW did not differ between groups but LB and HC were lower in the RG than in the UG (Table 2).
Newborn anthropometric measures. Results are expressed as means ± SD. UG: urban group; RG: rural group; §: data after excluding pregnant women with malnutrition, active and passive smokers, and alcohol consumers; missing values < 5%. T- test, *p < 0.05 UG (n = 358) and RG (n = 418), xp < 0.05 §UG (n = 269) and §RG (n = 139)
Figure 4 shows that the percentage of newborns delivered by cesarean section was higher in the RG than in the UG, considering and not considering all participants. The percentage of post-term and preterm birth, the percentage of babies who were small and large for gestational age were similar in both groups. In the RG, without considering smokers, alcohol consumers, and malnourished women, the percentage of HC less than the 5th percentile was greater than that of the UG.
Mode of delivery and newborn parameters. UG: urban group; RG: rural group; §: data after excluding pregnant women with malnutrition, active and passive smokers, and alcohol consumers; HC: head circumference; missing values < 5%. χ2, *p < 0.05 UG (n = 358) and RG (n = 418), xp < 0.05 §UG (n = 269) and §RG (n = 139)
Discussion
Residential proximity to agricultural pesticide applications may be an important source of environmental exposure. The magnitude of exposure of populations living in the proximity to agricultural fields can be substantially larger than that of populations who are not (Ryberg et al. 2018). People living in agricultural communities are exposed to a complex mixture of many individual pesticide active ingredients as well as to potentially toxic adjuvants included in the formulation. In the present study, we investigated the potential association of maternal residential proximity to fruit croplands with intense pesticide applications during pregnancy on pregnancy complications and alterations in their newborn parameters in Argentine North Patagonia. As the variability in fetal growth parameters at birth is known to be associated with the sex of the baby, gestational age at birth, multiplicity, and ethnicity (Janssen et al. 2007), women with similar parity and ethnicity were included in the study, and results were corrected by sex and gestational age. We observed increased pregnancy complications and altered fetal growth parameters in the population with maternal permanent residence closer than 5000 m from fruit croplands (RG), where OPs are the principal pesticides applied.
Among pregnancy complications, the percentage of threatened miscarriage, which, as defined by the World Health Organization, is a pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilation, was three times greater in the RG than in the UG (group of pregnant women who lived in Neuquén city), without previous history of pesticide exposure. Interestingly, when malnourished women, active and passive smokers, and alcohol consumers were excluded from the analysis for being considered confounding factors, the percentage of threatened miscarriage was still significantly greater in the RG, being two-fold greater than in the UG, suggesting that rural mothers experienced greater complications in their pregnancies for living close to areas where OPs are applied. Although threatened miscarriage has been associated with occupational exposure to pesticides and other contaminants (Park et al. 2017; Zhang et al. 1992), the relationship between threatened miscarriage and environmental pesticide exposure is understudied. Threatened miscarriage could be possibly related to underlying placental dysfunction (Davari-Tanha et al. 2008). Since in most cases of threatened miscarriage, bleeding originates from the placenta, we hypothesized that pregnancies complicated by a first-trimester threatened miscarriage could be at increased risk for other placenta-related complications. In this context, it is of interest that, although placental calcification is a physiological phenomenon, in our study, placental calcifications were found only in the RG and not in the UG. There is currently a lack of consistent evidence on the clinical significance of placental calcification and its relationship with pregnancy outcome. Jamal et al. (2017) found that passive smoking was a predictor of placental calcification and concluded that it could be an alarm sign for placental dysfunction. However, in the present study, when we excluded the active and passive smokers from the analysis, the percentage of women with placental calcifications in the RG still remained at 17%. The potential association of pregnancy complications with placental parameters in this population is reinforced by our previous studies in the Alto Valle del Río Negro. In these studies, in term placentas collected in a rural population during the spraying period, we found alterations in steroidogenic function, lipid profiles, frequency of the expression of anti-inflammatory cytokines, and activities of enzymes related to detoxification and oxidative stress defense compared with placentas collected during the non-spraying period (Bulgaroni et al. 2013; Chiapella et al. 2014; Rivero - Osimani et al. 2016; Vera et al. 2012). In addition, in our previous studies performed in women residing in two rural localities of the Alto Valle del Río Negro, we recorded pregnancy complications in the third trimester (Santa- Cruz et al. 2020), being preterm premature rupture of membranes the pregnancy complication found in highest percentage in this rural population during the spraying period. In the present study, as we recorded pregnancy complications along the three trimesters in women living in most of the localities of the Valley, we managed to identify threatened miscarriage as a pregnancy complication associated with rural residence. Many investigators have reported increased incidence of preterm birth and low birth weight following threatened miscarriage. Similarly, it has been reported that the incidence of premature rupture of membranes is higher among patients with threatened miscarriage than among pregnant women without this complication (Buchmayer et al. 2004), and only few reports have found normal development following threatened miscarriage. However, in our study, premature rupture of the membranes was similar between the RG and the UG.
The exact cause of threatened miscarriage is debatable, although it is possible that more than one process is involved in the pathogenesis of this condition (Roshdy Ahmed et al. 2012). Our finding has important public health implications for successful pregnancies and the interpretation of adverse impacts of environmental chemical exposures on pregnancy. Deeper investigations are needed to understand the mechanism underlying the association between pesticide exposures and threatened miscarriage in this area.
Regarding miscarriage, it has been linked to serum levels of organochlorine pesticides (Longnecker et al. 2005; Venners et al. 2005) and pesticide exposure history data (Arbuckle et al. 2001). In areas with distinct exposure to pesticides, prevalence rates per 100,000 inhabitants for miscarriage have been found to be significantly greater than in those with low exposure (García et al. 2017). The association between miscarriage and exposure to pesticides may suggest that exposure to specific pesticides tends to damage the fetus or the fetus–placenta complex or cause chromosomal anomalies (Arbuckle et al. 2001; Harris et al. 2020). However, a study performed in Mexico in women chronically exposed to OPs (Blanco-Muñoz et al. 2013) found no association between maternal paroxonase (an enzyme involved in detoxification from OPs) polymorphisms and the risk of miscarriage. In our study, although the percentage of miscarriage was greater in the RG than in the UG, when pregnant women with malnutrition, active and passive smokers, and alcohol consumers were excluded from the analysis, no cases of miscarriage were observed in either group.
Regarding intrauterine fetal death, in contrast to that found by Bell et al. (2001), who found a slight association between residential proximity to agricultural OP applications and fetal death, our results showed no intrauterine fetal death in the pregnancies studied in both the RG and the UG.
Most studies so far performed to quantify in utero exposures have relied upon maternal urinary or blood concentration as a proxy. While these measurements are critical to quantify maternal exposure, they do not provide a direct measure of fetal exposure. Exposure to insecticides during pregnancy may increase the risk of adverse birth outcomes (Jaacks et al. 2019). In our study, newborn anthropometric parameters were adjusted by sex and gestational age prior to statistical comparisons in both groups. Our results showed that the newborns of women of the RG had a smaller BL, smaller HC and higher PI at birth than those of women of the UG, and that the percentage of newborns with HC below the 5th percentile was higher in the RG than in the UG after excluding pregnant women with malnutrition, active and passive smokers, and alcohol consumers from the analysis. The exclusion of cases of pregnant women that presented these features is supported by the literature. Studies have shown that mild to moderate alcohol consumption diminishes the at-birth HC of theoretically healthy newborns in a linear form (Ortega-García et al. 2012). A decrease in HC has been used as a biomarker of the effect of neurotoxicants and constitutes diagnostic criteria in fetal alcohol syndrome (Ervalahti et al. 2007). It is also well-acknowledged that a reduction in BW, LB, and HC is associated with smoking habits in pregnancy (Ortega-García et al. 2012; Vardavas et al. 2010; Raatikainen et al. 2007). Consistent with our results, a significant decrease in HC in infants of women exposed to pesticides has been associated with a low activity of the detoxifying enzyme paraoxonase 1 (Berkowitz et al. 2004), although Whyatt et al. (2004) observed no significant decrease in HC at birth related to OP concentrations in cord plasma samples. Additionally, a decreasing trend of HC and an increased risk of HC below the 5th percentile have been observed in infants of mothers residing in crop areas in France, where OPs are used (Petit et al. 2010). However, in another agricultural area of OPs applications, Eskenazi et al. (2004) found that HC at birth was positively correlated with the level of dialkyl phosphate metabolites in maternal urine in early pregnancy. Béranger et al. (2020) observed associations between maternal hair concentrations of various pesticides or metabolites, including OPs, CBMs, and NNTs, with BW, LB, and HC and suggested that prenatal exposure to pesticides belonging to distinct chemical families may influence birth outcomes. In contrast, Wang et al. (2012) found no associations for BW and LB with maternal OPs in urine, although, similarly to that found by Eskenazi et al. (2004), they showed decreased gestational duration for female fetuses.
Although BW, BL, and HC are not specific for a dysfunction or disease, these parameters are conventionally used to evaluate and predict intrauterine development and possible alterations in growth. It is noteworthy that HC at birth may be considered a predictor of the IQ and cognitive abilities (Lindley et al. 1999; Petit et al. 2010). Considerable evidence suggests that prenatal exposure to OPs contributes to child neurodevelopmental disorders (Sapbamrer and Hongsibsong 2019). Moreover, relationships between maternal residential proximity to agricultural use of neurotoxic pesticides and poorer neurodevelopment in children have been identified (Gunier et al. 2017) and close residential proximity to greenhouse floricultural crops has been associated with adverse neurobehavioral performance among children (Friedman et al. 2020).
In our study, the rural population studied (RG) consisted of pregnant women living close (within less than 5000 m) to intense use of pesticides. Although OPs are the principal type of pesticides used in this region, combined toxicity due to other pesticide groups such as CBMs and NNTs could contribute to our results. Rappazzo et al. (2016) provided evidences of associations between residential exposure to agricultural pesticides and birth defects such as structural defects of several organs. In addition, Rull et al. (2006) found that maternal residential proximity within 1000 m of pesticide applications and exposure to OPs increased the risks of neural tube defects and anencephaly or bifid spine subtypes. In a retrospective study, Ling et al. (2018) found an increase in the risk of preterm birth among women living within 2000 m of agricultural application of pesticides (OPs, pyrethroids, and CBMs) during pregnancy, and their assessment revealed that exposure to pesticides was associated with preterm delivery but was rarely linked with term low BW. In addition, a meta-analysis of published data from the USA showed that pesticides were detected in house dust samples at a distance of 1000 m from treated agricultural fields (Deziel et al. 2017). However, the findings from the USA, where aerial spraying is common, may not be directly transferable to the situation in the Alto Valle del Río Negro, where ground-based spraying equipment is used in the season where the strongest winds occur, thus increasing the risk of exposure.
Fetal growth restriction, the main reason for low BW other than preterm birth, might result from transplacental oxygen and nutrient transport, hypoxia, oxidative stress, placental inflammation, and inhibition of placental growth hormones; these mechanisms may be influenced by toxic exposure to OPs and CBMs (Ling et al. 2018). Although in the present study we did not find much evidence for associations between term low BW and rural residence, we have previously reported altered placental oxidative stress parameters in this population (Chiapella et al. 2014). Thus, plausible mechanisms involving maternal, fetal, or placental units have yet to be identified to characterize the risk of the population of the Alto Valle del Río Negro.
We also found a significant association of the rural residence with the PI, which was increased in the RG. In this index, BW and LB are related. Newborns can be symmetrical or asymmetrical according to the PI. Symmetrical fetal development includes an appropriate relationship between BW and LB. Asymmetrical newborns with high PI have a relative greater weight than length, which is frequently taken as a measurement of obesity. Thus, the value of the PI is supplementary to the data of BW and LB. The PI at birth also predicts the body mass index and several diseases (Roje et al. 2004). In the present study, we corrected our data by sex and gestational age, important factors for the PI. Our results indicate that newborns of RG mothers were shorter relative to their weight at birth. Although BW did not differ between newborns of RG and UG mothers, an increased PI suggests fetal altered growth and organ maturation in those of RG mothers respect to those of UG mothers. The PI has been found to be a predictor of intrauterine growth restriction, but babies from RG mothers were not significantly smaller than those of UG mothers. The use of the PI curve for gestational age, together with other growth curves, improves the nutritional assessment of newborns (Fayyaz 2005).
It cannot be ruled out that the cause of the higher percentage of newborns delivered by cesarean section in RG with respect to UG, considering and not considering all participants, could be due to different characteristics and medical standards between the two areas.
This is the first multicenter study to identify the relationship between rural residence and pregnancy and newborn parameters covering a wide distribution of participants along the Alto Valle del Río Negro. An important strength of this study is the prospective design, as pregnant women were followed during pregnancy until delivery and their newborn’s parameters were registered. This strengthens the interpretation of the findings, as we are sure that birth addresses reflect the residence of mothers over the entirety of pregnancy. Another strength of the present study is that estimating the exposure during the prenatal period, when individuals are highly vulnerable to environmental insults, allows early implementation of health controls for rural children. Additionally, this study complements other previous studies of our group, in which rural participants were examined comparing the spraying and non-spraying periods. Taken together, these studies may be applicable to other fruit production areas.
One limitation of this study is that women exposure to pesticides was estimated in the prenatal stage by residential proximity to fruit crops. Currently, there is no a standard to determine exposure to pesticides in utero. However, since exposure assessment by biomonitoring or environmental monitoring is often not feasible in large population studies, we did not rely on distance only, but took into account the results of our previous studies in the Alto Valle del Río Negro in the design of the study. Although there is some literature where other authors conducted exposure assessment by collecting urine multiple times, the design of our study attempted to be included in the normal pregnancy control protocol, without additional participation of the women beyond being recruited and the first interview, in order to avoid unintended impacts on participant’s pregnancies. Another potential limitation of this study is that, when recording threatened miscarriage, the severity of vaginal bleeding was based on a subjective description by the patient. In addition, we did not collect information on potential routes of exposure to pesticides apart from whether or not the women lived in the rural communities, such as dietary intake. Despite these limitations, this study was undertaken based on a hospital-based study, with reliable information provided by the health personnel and also obtained from the medical record, and suggests that the risk of pregnancy complications and altered measures of birth outcomes could be associated with the pregnant women’s residential pesticide exposure estimated by proximity to fruit crops in the Alto Valle del Río Negro.
Conclusion
Our results suggest that OPs applications may increase the risk of pregnancy complications and altered newborn parameters. Certainly, the magnitude of these associations should be interpreted cautiously and such associations need to be verified by means of further studies. While our results cannot prove a causal link between proximity to agrochemicals and pregnancy complications and birth outcomes, an association might provide clues to common factors shared by these variables. There is a clear need to understand this association to develop and optimize prevention strategies. Additionally, there is a need for studies regarding other associated biological effects to determine the extent of potential pregnancy and fetal alterations as well as possible long-term effects. Our results accentuate the need to establish monitorings in areas where there is residential proximity to fruit crops, recording biomarkers of exposure and effects obtained from different noninvasive matrices, as well as anthropometric data. The lack of a continuous follow-up on exposure and effects might lead to unfavorable decision-making concerning how to reduce the risk of pesticide drifting and runoff to nearby homes of vulnerable population groups.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BW:
-
Birth weight
- CBMs:
-
Carbamates
- HC:
-
Head circumference
- LB:
-
Length at birth
- NNTs:
-
Neonicotinoids
- OPs:
-
Organophosphates
- PI:
-
Ponderal index at birth
- RG:
-
Rural group
- UG:
-
Urban group
References
Arbuckle TE, Lin Z, Mery LS (2001) An exploratory analysis of the effect of pesticide exposure on the risk of spontaneous abortion in an Ontario farm population. Environ Health Perspect 109:851–857. https://doi.org/10.1289/ehp.01109851
Babina K, Dollard M, Pilotto L, Edwards JW (2012) Environmental exposure to organophosphorus and pyrethroid pesticides in South Australian preschool children: a cross sectional study. Environ Int 48:109–120. https://doi.org/10.1016/j.envint.2012.07.007
Bell EM, Hertz-Picciotto I, Beaumont JJ (2001) Case-cohort analysis of agricultural pesticide applications near maternal residence and selected causes of fetal death. Am J Epidemiol 154:702–710. https://doi.org/10.1093/aje/154.8.702
Béranger R, Hardy EM, Binter AC, Charles MA, Cécile Zaros C, Appenzeller BMR, Chevrier C (2020) Multiple pesticides in mothers’ hair samples and children’s measurements at birth: results from the French national birth cohort (ELFE). Int J Hyg Environ Health 223:22–33. https://doi.org/10.1016/j.ijheh.2019.10.010
Berkowitz GS, Wetmur JG, Birman-Deych E, Obel J, Lapinski RH, Godbold JH, Holzman IR, Wolff MS (2004) In utero pesticide exposure, maternal paraoxonase activity, and head circumference. Environ Health Perspect 112:388–391. https://doi.org/10.1289/ehp.6414
Blanco-Muñoz J, Aguilar-Garduño C, Gamboa-Avila R, Rodríguez-Barranco M, Pérez-Méndez O, Huesca-Gómez C, González-Alzaga B, Lacasaña M (2013) Association between PON1 genetic polymorphisms and miscarriage in Mexican women exposed to pesticides. Sci Total Environ 449:302–308. https://doi.org/10.1016/j.scitotenv.2013.01.034
Bouchard MF, Chevrier J, Harley KG, Kogut K, Vedar M, Calderon N, Trujillo C, Johnson C, Bradman A, Barr DB, Eskenazi B (2011) Prenatal exposure to organophosphate pesticides and IQ in 7-year-old children. Environ Health Perspect 119(8):1189–1195. https://doi.org/10.1289/ehp.1003185
Bradman A, Castorina R, Barr DB, Chevrier J, Harnly ME, Eisen EA, McKone TE, Harley K, Holland N, Eskenazi B (2011) Determinants of organophosphorus pesticide urinary metabolite levels in young children living in an agricultural community. Int. J. Environ. Res. Public Health 8:1061–1083. https://doi.org/10.3390/ijerph8041061
Bradman A, Kogut K, Eisen EA, Jewell NP, Quirós-Alcalá L, Castorina R, Chevrier J, Holland NT, Barr DB, Kavanagh-Baird G, Eskenazi B (2013) Variability of organophosphorous pesticide metabolite levels in spot and 24-hr urine samples collected from young children during 1 week. Environ Health Perspect 121(1):118–124. https://doi.org/10.1289/ehp.1104808
Buchmayer SM, Sparén P, Cnattingius S (2004) Previous pregnancy loss: risks related to severity of preterm delivery. Am J Obstet Gynecol 191(4):1225–1231. https://doi.org/10.1016/j.ajog.2004.02.066
Bukasala JS, Brunekreef B, Brouwer M, Koppelman GH, Wijga AH, Huss A, Gehring U (2018) Associations of residential exposure to agricultural pesticides with asthma prevalence in adolescence: the PIAMA birth cohort. Environ Int 121:435–442. https://doi.org/10.1016/j.envint.2018.09.029
Bulgaroni V, Rovedatti MG, Sabino G, Magnarelli G (2012) Organophosphate pesticide environmental exposure: analysis of salivary cholinesterase and carboxilesterase activities in preschool children and their mothers. Environ Monit Assess 184(5):3307–3314. https://doi.org/10.1007/s10661-011-2190-8
Bulgaroni V, Lombardo P, Rivero-Osimani V, Vera B, Dulgerian L, Cerbán F, Guiñazú N (2013) Environmental pesticide exposure modulates cytokines, arginase and ornithine decarboxylase expression in human placenta. Reprod Toxicol 39:23–32. https://doi.org/10.1016/j.reprotox.2013.03.010
Carmichael SL, Yang W, Roberts E, Kegley SE, Padula AM, English PB, Lammer EJ, Shaw GM (2014) Residential agricultural pesticide exposures and risk of selected congenital heart defects among offspring in the San Joaquin Valley of California. Environ Res 135:133–138. https://doi.org/10.1016/j.envres.2014.08.030
Cecchi A, Rovedatti MG, Sabino G, Magnarelli GG (2012) Environmental exposure to organophosphate pesticides: assessment of endocrine disruption and hepatotoxicity in pregnant women. Ecotox Environ Safe 80:280–287. https://doi.org/10.1016/j.ecoenv.2012.03.008
Cheikh Ismail L, Knight HE, Bhutta Z, Chumlea WC, International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st) (2013) Anthropometric protocols for the construction of new international fetal and newborn growth standards: the INTERGROWTH-21st Project. BJOG 120(2):42–47. https://doi.org/10.1111/1471-0528.12125
Chiapella G, Genti-Raimondi S, Magnarelli G (2014) Placental oxidative status in rural residents environmentally exposed to organophosphates. Environ Toxicol Pharmacol 38:220–229. https://doi.org/10.1016/j.etap.2014.06.001
Copes WJ (2012) Evaluation of plant barriers to mitigate spray drift. Thesis, Master of Environmental Engineering, Faculty of Engeneering, National University of Comahue [in Spanish]. https://inta.gob.ar/documentos/evaluacion-de-barreras-vegetales-para-mitigar-la-deriva-de-pulverizaciones
Coronado GD, Vigoren EM, Thompson B, Griffith WC, Faustman EM (2006) Organophosphate pesticide exposure and work in pome fruit: evidence for the take-home pesticide pathway. Environ Health Perspect 114(7):999–1006. https://doi.org/10.1289/ehp.8620
Davari-Tanha F, Shariat M, Kaveh M, Ebrahimi M, Jalalvand S (2008) Threatened abortion: a risk factor for poor pregnancy outcome. Acta Med Iran 46(4):314–320. https://doi.org/10.1016/j.ajog.2003.09.023
Deziel NC, Freeman LE, Graubard BI, Jones RR, Hoppin JA, Thomas K, Hines CJ, Blair A, Sandler DP, Chen H, Lubin JH, Andreotti G, Alavanja MCR, Friesen MC (2017) Relative contributions of agricultural drift, para-occupational, and residential use exposure pathways to house dust pesticide concentrations: meta-regression of published data. Environ Health Perspect 125:296–305. https://doi.org/10.1289/EHP426
Ervalahti N, Korkman M, Fagerlund A, Autti-Rämö I, Loimu L, Hoyme HE (2007) Relationship between dysmorphic features and general cognitive function in children with fetal alcohol spectrum disorders. Am J Med Genet 43:2916–2923. https://doi.org/10.1002/ajmg.a.32009
Eskenazi B, Harley K, Bradman A, Weltzien E, Jewell N, Barr D, Furlong C, Holland N (2004) Association of in utero organophosphate pesticide exposure and fetal growth and length of gestation in an agricultural population. Environ Health Perspect 112(10):1116–1124. https://doi.org/10.1289/ehp.6789
Fayyaz J (2005) Ponderal index. J Pak Med Assoc 55(6):228–229 https://ecommons.aku.edu/pakistan_fhs_mc_emerg_med/196
Fenik J, Tankiewicz M, Biziuk M (2011) Properties and determination of pesticides in fruits and vegetables. Trends Anal Chem 30(6):814–826. https://doi.org/10.1016/j.trac.2011.02.008
Fenske RA, Lu C, Curl CL, Shirai JH, Kissel JC (2005) Biologic monitoring to characterize organophosphorus pesticide exposure among children and workers: an analysis of recent studies in Washington State. Environ Health Perspect 113:1651–1657. https://doi.org/10.1289/ehp.8022
Friedman E, Hazlehurst MF, Loftus C, Karr C, McDonald KN, Suarez-Lopez JR (2020) Residential proximity to greenhouse agriculture and neurobehavioral performance in Ecuadorian children. Int J Hyg Environ Health 223:220–227. https://doi.org/10.1016/j.ijheh.2019.08.009
FunBaPa (2010) Evaluation of the impact of the National Program of Suppression of Carpocapsa on the pome fruit growing in the irrigated valleys of Norpatagonia. FunBaPa Eds., Viedma, 79pp [in Spanish]. http://www.funbapa.org.ar/funbapa/wp-content/uploads/2013/06/impacto-carpocapsa.pdf last. january 2020
García J, Ventura MI, Requena M, Hernández AF, Parrón T, Alarcón R (2017) Association of reproductive disorders and male congenital anomalies with environmental exposure to endocrine active pesticides. Reprod Toxicol 71:95–100. https://doi.org/10.1016/j.reprotox.2017.04.011
Gunier RB, Bradman A, Harley KG, Kogut K, Eskenazi B (2017) Prenatal residential proximity to agricultural pesticide use and IQ in 7-year-old children. Environ Health Perspect 125(5):057002. https://doi.org/10.1289/EHP504
Hanke W, Jurewicz J (2004) The risk of adverse reproductive and developmental disorders due to occupational pesticide exposure: an overview of current epidemiological evidence. Int J Occup Med Environ Health 17(2):223–243
Harley K, Huen K, Aguilar-Schall R, Holland N, Bradman A, Barr DB, Eskenazi B (2011) Association of organophosphate pesticide exposure and paraoxonase with birth outcome in Mexican-American women. PLoS One 6(8):e23923. https://doi.org/10.1371/journal.pone.0023923
Harris SM, Jin Y, Loch-Caruso R, Padilla IY, Meeker JD, Bakulski KM (2020) Identification of environmental chemicals targeting miscarriage genes and pathways using the comparative toxicogenomics database. Environ Res 184:109259. https://doi.org/10.1016/j.envres.2020.109259
Jaacks LM, Diao N, Calafat AM, Ospina M, Mazumdar M, Hasan M, Wright R, Quazi Quamruzzaman Q, Christiani DC (2019) Association of prenatal pesticide exposures with adverse pregnancy outcomes and stunting in rural Bangladesh. Environ Int 133:105243. https://doi.org/10.1016/j.envint.2019.105243
Jamal A, Moshfeghi M, Moshfeghi S, Mohammadi N, Zarean E, Jahangiri N (2017) Is preterm placental calcification related to adverse maternal and foetal outcome? J Obstet Gynaecol 37(5):605–609. https://doi.org/10.1080/01443615.2017.1285871
Janssen PA, Thiessen P, Klein MC, Whitfield MF, MacNab YC, Cullis-Kuhl SC (2007) Standards for the measurement of birth weight, length and head circumference at term in neonates of European, Chinese and South Asian ancestry. Open Med 1(2):e74–e88
Kirs VE (2002) Dynamic and Degradation of Organophosphate Pesticides in High Valley of Negro River Soil. Thesis, Master of Chemical Sciences, Faculty of Engeneering, National University of Comahue [in spanish]. http://opac.uncoma.edu.ar/cgi-bin/koha/opac-detail.pl?biblionumber=81
Koureas M, Tsakalof A, Tsatsakis A, Hadjichristodoulou C (2012) Systematic review of biomonitoring studies to determine the association between exposure to organophosphorus and pyrethroid insecticides and human health outcomes. Toxicol Lett 210:155–168. https://doi.org/10.1016/j.toxlet.2011.10.007
Lejarraga H, Fustiñana C (1986) Weight, body length, and head circumference standards from 26 to 92 weeks of postmenstrual age. Arch Argent Pediatr 84:210–214 [in Spanish]. https://www.sap.org.ar/docs/publicaciones/archivosarg/1986/1986_84_4.pdf
Levario-Carrillo M, Olave ME, Corral D, Alderete JG, Gagioti S, Bevilacqua E (2004) Placental morphology of rats prenatally exposed to methyl parathion. Exp Toxicol Pathol 55(6):489–496. https://doi.org/10.1078/0940-2993-00346
Lindley A, Benson J, Grimes C, Cole T, Herman A (1999) The relationship in neonates between clinically measured head circumference and brain volume estimated from head CT-scans. Early Hum Dev 56(1):17–29. https://doi.org/10.1016/S0378-3782(99)00033-X
Ling C, Liew Z, von Ehrenstein OS, Heck JE, Park AS, Cui X, Cockburn M, Wu J, Ritz B (2018) Prenatal exposure to ambient pesticides and preterm birth and term low birthweight in agricultural regions of California. Toxics 6(3):E41. https://doi.org/10.3390/toxics6030041
Loewy RM, Monza LB, Kirs VE, Savini MC (2011) Pesticide distribution in an agricultural environment in Argentina. J Environ Sci Health A 46:662–670. https://doi.org/10.1080/03601234.2012.592051
Longnecker MP, Klebanoff MA, Dunson DB, Guo X, Chen Z, Zhou H, Brock JW (2005) Maternal serum level of the DDT metabolite DDE in relation to fetal loss in previous pregnancies. Environ Res 97(2):127–133. https://doi.org/10.1016/S0013-9351(03)00108-7
Lu C, Fenske RA, Simcox NJ, Kalman D (2000) Pesticide exposure of children in an agricultural community: evidence of household proximity to farmland and take home exposure pathways. Environ Res 84(3):290–302. https://doi.org/10.1006/enrs.2000.4076
Macchi P, Loewy RM, Lares B, Latini L, Monza L, Guiñazú N, Montagna CM (2018) The impact of pesticides on the macroinvertebrate community in the water channels of the Río Negro and Neuquén Valley, North Patagonia (Argentina). Environ Sci Pollut Res Int 25:1066–10678. https://doi.org/10.1007/s11356-018-1330-x
Magnarelli GG, Rovedatti MG, Pechen de D’Angelo AM (2011) Pesticides and human health. In: Anguiano OL, Montagna CM (eds) Pesticide classification and toxicology. EDUCO, Neuquén, pp 309–340 [in Spanish]. http://www.ctys.com.ar/index.php?idPage=20&idArticulo=1826
Mahibbur RM, Govindarajulu Z (1997) A modification of the test of Shapiro and Wilks for normality. J Appl Stat 24(2):219–235. https://doi.org/10.1080/02664769723828
Mardones F, Rosso P (1997) Design of a weight gain chart for pregnant women. Rev Méd Chile 125:1437–1448
Matthews G, Hamey P (2003) Exposure of bystanders to pesticides. Pestic Outlook 14:210–212. https://doi.org/10.1039/b311469b
Ministry of Public Finance, Presidency of Argentine (2016) Value chain analysis report. Fresh fruits - apples and pears [in Spanish]. https://www.economia.gob.ar/peconomica/docs/Complejo_fruta_pepita.pdf. Accessed 1 Apri 2020
Muñoz Quezada MT, Lucero B, Bradman A, Steenland K, Zúñiga L, Calafat AM, Ospina M, Iglesias V, Muñoz MP, Buralli RJ, Fredes C, Gutiérrez JP (2019) An educational intervention on the risk perception of pesticides exposure and organophosphate metabolites urinary concentrations in rural school children in Maule Region. Chile Environ Res 176:108554. https://doi.org/10.1016/j.envres.2019.108554
Mwila K, Burton MH, Van Dyk JS, Pletschke BI (2013) The effect of mixtures of organophosphate and carbamate pesticides on acetylcholinesterase and application of chemometrics to identify pesticides in mixtures. Environ Monit Assess 185(3):2315–2327. https://doi.org/10.1007/s10661-012-2711-0
Ortega-García JA, Gutierrez-Churango JE, Sánchez-Sauco MF, Martínez-Aroca M, Delgado-Marín JL, Sánchez-Solis M, Parrilla-Paricio JJ, Claudio L, Martínez-Lage JF (2012) Head circumference at birth and exposure to tobacco, alcohol and illegal drugs during early pregnancy. Childs Nerv Syst 28(3):433–439. https://doi.org/10.1007/s00381-011-1607-6
Park C, Kang M-Y, Kim D, Park J, Eom H, Kim E-A (2017) Prevalence of abortion and adverse pregnancy outcomes among working women in Korea: a cross-sectional study. PLoS One 12(8):e0182341. https://doi.org/10.1371/journal.pone.0182341
Parvez S, Gerona RR, Proctor C, Friesen M, Ashby JL, Reiter JL, Lui Z, Winchester PD (2018) Glyphosate exposure in pregnancy and shortened gestational length: a prospective Indiana birth cohort study. Environ Health 17:23. https://doi.org/10.1186/s12940-018-0367-0
Pastore LM, Hertz-Picciotto I, Beaumont JJ (1997) Risk of stillbirth from occupational and residential exposures. Occup Environ Med 54:511–518. https://doi.org/10.1136/oem.54.7.511
Perera FP, Rauh V, Tsai WY, Kinney P, Camann D, Barr D, Bernert T, Garfinkel R, Tu YH, Diaz D, Dietrich J, Whyatt RM (2003) Effects of transplacental exposure to environmental pollutants on birth outcomes in a multiethnic population. Environ Health Perspect 111:201–205. https://doi.org/10.1289/ehp.5742
Petit C, Chevrier C, Durand G, Monfort C, Rouget F, Ronan Garlantezec R, Cordier S (2010) Impact on fetal growth of prenatal exposure to pesticides due to agricultural activities: a prospective cohort study in Brittany. France Environ Health 9:71 http://www.ehjournal.net/content/9/1/71
Quintana MM, Vera B, Magnarelli G, Guiñazú N, Rovedatti MG (2017) Neonate, placental and umbilical cord blood parameters in pregnant women residing in areas with intensive pesticide application. Environ Sci Pollut Res 24:20736–20746. https://doi.org/10.1007/s11356-017-9642-9
Raatikainen K, Huurinainen P, Heinonen S (2007) Smoking in early gestation or through pregnancy: a decision crucial to pregnancy outcome. Prev Med 44(1):59–63. https://doi.org/10.1016/j.ypmed.2006.07.017
Rappazzo KM, Warren JL, Meyer RE, Herring AH, Sanders AP, Brownstein NC, Luben TJ (2016) Maternal residential exposure to agricultural pesticides and birth defects in a 2003 to 2005 North Carolina birth cohort. Birth Defects Res A 106:240–249. https://doi.org/10.1002/bdra.23479
Rauch SA, Braun JM, Barr DB, Calafat AM, Khoury J, Montesano MA, Yolton K, Lanphear BP (2012) Associations of prenatal exposure to organophosphate pesticide metabolites with gestational age and birthweight. Environ Health Perspect 120(7):1055–1060. https://doi.org/10.1289/ehp.1104615
Rauh V, Arunajadai S, Horton M, Perera F, Hoepner L, Barr DB, Whyatt R (2011) Seven-year neurodevelopmental scores and prenatal exposure to chlorpyrifos, a common agricultural pesticide. Environ Health Perspect 119(8):1196–1201. https://doi.org/10.1289/ehp.1003160
Rivero - Osimani VL, Valdez SR, Guiñazú N, Magnarelli G (2016) Alteration of syncytiotrophoblast mitochondria function and endothelial nitric oxide synthase expressionin the placenta of rural residents. Reprod Toxicol 61:47–57. https://doi.org/10.1016/j.reprotox.2016.02.018
Roje D, Ivo B, Ivica T, Mirjana V, Vesna C, Aljosa B, Marko V, Zoran M, Marko M, Tomislav M (2004) Gestational age — the most important factor of neonatal ponderal index. Yonsei Med J 45(2):273–280. https://doi.org/10.3349/ymj.2004.45.2.273
Roshdy Ahmed S, El-Khatem El-Sammani M, Al-Alaziz Al-Sheeha M, Saeed Aitallah A, Jabin Khan F, Roshdy Ahmed S (2012) Pregnancy outcome in women with threatened miscarriage: a year study. Mat Soc Med 24(1):26–28. https://doi.org/10.5455/msm.2012.24.26-28
Rovedatti MG, Trapassi JH, Vela L, López A, Santa Cruz S y Magnarelli G (2006) Environmental health prevention for populations exposed to pesticides: interviews in rural communities and educational workshop for multiplier agents. Acta Toxicol Argent 14 (1): 1-6, [in Spanish]. https://www.toxicologia.org.ar/bibliotecavirtual/acta_toxicologica/vol14-1.pdf
Rowe C, Gunier R, Bradman A, Harley KG, Kogut K, Parra K, Eskenazi B (2016) Residential proximity to organophosphate and carbamate pesticide use during pregnancy, poverty during childhood, and cognitive functioning in 10-year-old children. Environ Res 150:128–137. https://doi.org/10.1016/j.envres.2016.05.048
Rull RP, Ritz B, Shaw GM (2006) Neural tube defects and maternal residential proximity to agricultural pesticide applications. Am J Epidemiol 163(8):743–753. https://doi.org/10.1093/aje/kwj101
Ryberg MW, Rosenbaum RK, Mosqueron L, Fantke P (2018) Addressing bystander exposure to agricultural pesticides in life cycle impact assessment. Chemosphere 197:541–549. https://doi.org/10.1016/j.chemosphere.2018.01.088
Sagiv SK, Harris MH, Gunier RB, Kogut KR, Harley KG, Deardorff J, Bradman A, Holland N, Eskenazi B (2018) Prenatal organophosphate pesticide exposure and traits related to autism spectrum disorders in a population living in proximity to agriculture. Environ Health Perspect 126(4):047012. https://doi.org/10.1289/EHP2580
Salihu HM, Wilson RE (2007) Epidemiology of prenatal smoking and perinatal outcomes. Early Hum Dev 83:713–720. https://doi.org/10.1016/j.earlhumdev.2007.08.002
Sánchez S, Vera B, Montagna C, Magnarelli G (2015) Characterization of placental cholinesterases and activity induction associated to environmental organophosphate exposure. Toxicol Rep 2:437–442. https://doi.org/10.1016/j.toxrep.2014.11.013
Santa- Cruz S, Magnarelli G, Rovedatti MG (2020) Evaluation of endocrine disruption and gestational disorders in women residing in areas with intensive pesticide application: an exploratory study. Environ Toxicol Pharmacol 73:103280. https://doi.org/10.1016/j.etap.2019.103280
Sapbamrer R, Hongsibsong S (2019) Effects of prenatal and postnatal exposure to organophosphate pesticides on child neurodevelopment in different age groups: a systematic review. Environ Sci Pollut Res 26:18267–18290. https://doi.org/10.1007/s11356-019-05126-w
Shelton JF, Geraghty EM, Tancredi DJ, Delwiche LD, Schmidt RJ, Ritz B, Hansen RL, Hertz-Picciotto I (2014) Neurodevelopmental disorders and prenatal residential proximity to agricultural pesticides: the CHARGE study. Environ Health Perspect 122(10):1103–1109. https://doi.org/10.1289/ehp.1307044
Souza MS, Magnarelli GG, Rovedatti MG, Santa-Cruz S, Pechen de D’Angelo AM (2005) Prenatal exposure to pesticides: analysis of human placental acetylcholinesterase, glutathione-S-transferase and catalase as biomarkers of effect. Biomarkers 10(5):376–389. https://doi.org/10.1080/13547500500272614
Stillerman KP, Mattison DR, Giudice LC, Woodruff TJ (2008) Environmental exposures and adverse pregnancy outcomes: a review of the science. Reprod Sci 15:631–650. https://doi.org/10.1177/1933719108322436
Tosi A, de D’Angelo AM P, Savini MC, Loewy MC (2009) Pesticide risk analysis on surface water of the Northern Argentine Patagonic region. Acta Toxicol Argent 17(1):1–6 [in Spanish]. https://toxicologia.org.ar/bibliotecavirtual/acta_toxicologica/ata17_1.pdf
van den Berg F, Kubiak R, Benjey WG, Majewski MS, Yates SR, Reeves G, Smelt JH, van der Linden AMA (1999) Emission of pesticides into the air. Water Air Soil Pollut 115:195–218. https://doi.org/10.1023/A:1005234329622
Vardavas CI, Plada M, Tzatzarakis M, Marcos A, Warnberg J, Gomez- Martinez S, Breidenassel C, Gonzalez-Gross M, Tsatsakis AM, Saris WH, Moreno LA, Kafatos AG (2010) Passive smoking alters circulating naive/memory lymphocyte T-cell subpopulations in children. Pediatr Allergy Immunol 21:1171–1178. https://doi.org/10.1111/j.1399-3038.2010.01039.x
Venners SA, Korrick S, Xu X, Chen C, Guang W, Huang A, Altshul L, Perry M, Fu L, Wang X (2005) Preconception serum DDT and pregnancy loss: a prospective study using a biomarker of pregnancy. Am J Epidemiol 162(8):709–716. https://doi.org/10.1093/aje/kwi275
Vera B, Santa- Cruz S, Magnarelli G (2012) Plasma cholinesterase and carboxylesterase activities and nuclear and mitochondrial lipid composition of human placenta associatedwith maternal exposure to pesticides. Reprod Toxicol 34(3):402–407. https://doi.org/10.1016/j.reprotox.2012.04.007
Wang Y, Chen HJ (2012) Use of percentiles and Z -Scores in anthropometry. In: Preedy VR (ed) Handbook of anthropometry: physical measures of human form in health and disease. Springer Science+Business Media, New York, LLC, pp 29–48. https://doi.org/10.1007/978-1-4419-1788-1_2
Wang P, Tian Y, Wang XJ, Gao Y, Shi R, Wang GQ, Hu GH, Shen XM (2012) Organophosphate pesticide exposure and perinatal outcomes in Shanghai. China Environ Internat 42:100–104. https://doi.org/10.1016/j.envint.2011.04.015
Wang Y, Zhang Y, Ji L, Hu Y, Zhang J, Wang C, Ding G, Chen L, Kamijima M, Ueyama J, Gao Y, Tian Y (2017) Prenatal and postnatal exposure to organophosphate pesticides and childhood neurodevelopment in Shandong. China Environ Int 108:119–126. https://doi.org/10.1016/j.envint.2017.08.010
Weselak M, Arbuckle TE, Wigle DT, Krewski D (2007) In utero pesticide exposure and childhood morbidity. Environ Res 103(1):79–86. https://doi.org/10.1016/j.envres.2006.09.001
Whyatt RM, Rauh V, Barr DB, Camann DE, Andrews HF, Garfinkel R, Hoepner LA, Diaz D, Dietrich J, Reyes A, Tang D, Kinney PL, Perera FP (2004) Prenatal insecticide exposures and birth weight and length among an urban minority cohort. Environ Health Perspect 112:1125–1132. https://doi.org/10.1289/ehp.6641
Wigle DT, Arbuckle TE, Turner MC, Bérubé A, Yang Q, Liu S, Krewski D (2008) Epidemiologic evidence of relationships between reproductive and child health outcomes and environmental chemical contaminants. J Toxicol Environ Health B Crit Rev 11:373–517. https://doi.org/10.1080/10937400801921320
Winchester PD, Huskins J, Ying J (2009) Agrochemicals in surface water and birth defects in the United States. Acta Paediatr 98(4):664–669. https://doi.org/10.1111/j.1651-2227.2008.01207.x
Wohlfahrt-Veje C, Main KM, Schmidt IM, Boas M, Jensen TK, Grandjean P, Skakkebæk NE, Andersen HR (2011) Lower birth weight and increased body fat at school age in children prenatally exposed to modern pesticides: a prospective study. Environ Health 10:79. https://doi.org/10.1186/1476-069X-10-79
Woodruff TJ, Carlson A, Schwartz JM, Giudice LC (2008) Proceedings of the summit on environmental challenges to reproductive health and fertility: executive summary. Fertil Steril 89(1):e1–e20. https://doi.org/10.1016/j.fertnstert.2008.01.065
Woskie S, Kongtip P, Thanasanpaiboon W, Kiatdamrong N, Charoonrungsirikul N, Nankongnab N, Anu Surach A, Phamonphon A (2017) A pilot study of maternal exposure to organophosphate pesticides and newborn neurodevelopment in Thailand. Int J Occup Environ Health 23(3):193–201. https://doi.org/10.1080/10773525.2018.1450324
Zhang J, Cai WW, Lee DJ (1992) Occupational hazards and pregnancy outcomes. Am J Ind Med 21:397–408. https://doi.org/10.1002/ajim.4700210312
Acknowledgements
We thank all the women participating in this study, as well as the health agents who collaborated, especially Dr. Silvia Santa Cruz, nurse midwife Carina Romero, the staff of the Gynecology Service of the General Roca City Hospital, the Laboratory Staff of the Maternity Service and the Statistical Service of Dr. E. Accame Hospital of Allen City.
Funding
This research was conducted with the support of the Fellowship “Ramón Carrillo - Arturo Oñativia” Institutional Projects, issued by the Argentine National Ministry of Health, through the Argentine National Health Research (ECM 2010), and grants from Universidad Nacional del Comahue (I004/3) and Argentine National Agency for the Promotion of Science and Technology, FONCyT (PICT-Redes 2007-00214).
Author information
Authors and Affiliations
Contributions
AC: Methodology, Investigation, Data Curation, Resources
GA: Methodology, Investigation, Resources
NQ: Investigation, Data Curation
MCB: Investigation, Data Curation
SA: Investigation, Data Curation
GS: Formal analysis
GGM: Conceptualization, Writing - Review & Editing, Visualization, Supervision, Project administration, Funding acquisition
MGR: Conceptualization, Writing - Review & Editing, Visualization, Supervision, Project administration, Funding acquisition
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by the ethical committee of the local Advisory Committee of Biomedical Research in Humans.
Consent to participate
Amalia Cecchi, Gabriel Alvarez, Natalia Quidel, María Cecilia Bertone, Guillermo Sabino, and Gladis G. Magnarelli participated in the design, execution, and analysis of the paper entitled Residential proximity to pesticide applications in Argentine Patagonia: impact on pregnancy and newborn parameter, have seen and approved the final version, and that it has neither been published nor submitted elsewhere.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Higher threatened miscarriage was the pregnancy complication associated to residential proximity to Patagonian fruit croplands with pesticide applications.
• Lower length at birth was associated to residential proximity to the fruit croplands in High Valley of Negro River, in Argentine Patagonia.
• Women living within a short distance of this agricultural field had babies with lower head circumference at birth.
• Higher ponderal index in newborns was associated to residential proximity to this fruit-growing zone.
Rights and permissions
About this article
Cite this article
Cecchi, A., Alvarez, G., Quidel, N. et al. Residential proximity to pesticide applications in Argentine Patagonia: impact on pregnancy and newborn parameters. Environ Sci Pollut Res 28, 56565–56579 (2021). https://doi.org/10.1007/s11356-021-14574-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-14574-2