Abstract
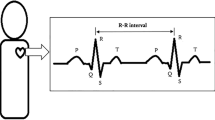
As an indicator of cardiac autonomic function, heart rate variability (HRV) has been proven to decrease after short-term exposure to particulate matters (PM) based on controlled animal studies. In this study, we conducted a systematic review to investigate short-term effects of exposure with different particle sizes on HRV in humans. Both crossover and controlled studies of human which were published prior to February 2020 were searched on four electronic databases. The HRV parameters included standard deviation of normal-to-normal intervals (SDNN), root mean square of successive normal-to-normal intervals (RMSSD), percent of normal-to-normal intervals that differ by more than 50 milliseconds (PNN50), low frequency (LF), high frequency (HF), and LF/HF. This review included 14 studies with 300 participants. The short-term effects of PM exposure on HRV in humans are inconclusive. For time-domain parameters, one study showed higher SDNN values with 2-h exposure to PM, whereas another one showed lower SDNN values. One study found RMSSD increased after PM exposure. One study found PNN50 decreased after PM exposure. For frequency-domain parameters, two studies showed LF increased with 2-h exposure to PM, and two studies showed an increase of LF/HF after PM exposure. Four studies showed lower HF values after PM exposure, whereas two studies showed higher HF values. Five studies did not find statistically significant results for any HRV parameters. We could not conclude that short-term exposure to PM can influence autonomic nervous function. The inconsistent changes of HRV in response to PM exposure may have complex mechanisms, which remains to be elucidated.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is a common disease that seriously impairs human health. The cases were estimated at 422 million worldwide and as the first leading cause of death, leading to one-third of all deaths in 2015 (Roth et al. 2017). In recent years, the level of air pollution has increased gradually (Bai et al. 2018). The public began to pay close attention to the relationship between air pollution and human health. Numerous studies have shown that both long-term and short-term exposure to particulate matters (PM) were associated with increased risk of CVD and its mortality (Cesaroni et al. 2014; Huang et al. 2016; Liu et al. 2018; Orellano et al. 2020). According to the estimate of World Health Organization (WHO), PM pollution caused approximately 3 million deaths around the world (World Health Organization 2016), and CVD was responsible for more than two-thirds of the deaths (Lelieveld et al. 2019).
Animal experiments are often used to investigate the mechanism of PM exposure on the cardiovascular system. Our previous meta-analysis of controlled animal experiments showed that PM exposure can lead to a decrease in heart rate variability (HRV) parameters, including standard deviation of normal-to-normal intervals (SDNN) and ratio of low frequency and high frequency (LF/HF), in rodents (Huang et al. 2020). As a reliable indicator of cardiac autonomic nervous regulation, reduced HRV has been suggested to be related to immune dysfunction and systematic inflammation, as well as an elevated risk of CVD (Chen et al. 2015; Kemp and Quintana 2013; Thayer et al. 2010). The animal experiments suggest that PM exposure may impact the course of CVD development via reducing HRV (Huang et al. 2020).
Meanwhile, epidemiological studies have been used to investigate associations of PM pollution and HRV in humans (Pieters et al. 2012; Buteau and Goldberg 2016). A review of cross-sectional and longitudinal studies concluded that there was evidence of a negative correlation between short-term exposure to PM and HRV, including LF, HF, SDNN, and root mean square of successive normal-to-normal intervals (RMSSD) (Pieters et al. 2012). However, a recent review of panel studies with repeated measurements of outcomes found limited evidence of the association, although negative associations of several HRV parameters and fine particles were found in older CVD patients (Buteau and Goldberg 2016).
Experimental studies with crossover design are also used to investigate effects of PM exposure on HRV indices in humans. Randomized crossover design can improve the quality of studies and provide more accurate evidence of the associations than observational studies. Several crossover studies have found short-term exposure to PM can lead to the decrease of HRV parameters, such as SDNN and HF (Brook et al. 2014; Graff et al. 2009; Vora et al. 2014). However, the results were inconsistent since some other studies found opposite or no statistically significant results (Byrd et al. 2016; Fakhri et al. 2009; Samet et al. 2009). At present, a systematic review of crossover studies is lacking. One previous review of crossover and prospective studies only included three crossover studies for ultrafine particles (UFPs) (Weichenthal 2012). Therefore, a systematic review designed to investigate effects of PM exposure with different particle sizes based on crossover studies for human is needed.
In this article, we conducted a systematic review of crossover and controlled studies to investigate short-term effects of exposure to PM with different particle sizes on HRV parameters in humans. HRV measurements included SDNN, RMSSD, LF, HF, LF/HF, and percent of normal-to-normal intervals that differ by more than 50 milliseconds (PNN50), which represents the changes of different nervous systems (Dong 2016).
Methods
Eligibility criteria
The aim of this systematic review was to examine short-term effects of exposure to PM on HRV in humans from crossover or controlled studies. The eligible study objects in this research were healthy participants or patients with a certain disease; PM exposures include UFPs, fine particles (particles that is 2.5 μm or less in diameter, PM2.5), or coarse particles (particles that is 10 μm or less in diameter, PM10), and at least one HRV parameter has been measured including SDNN, RMSSD, PNN50, LF, HF, and LF/HF. Studies targeted at multiple pollutants exposure or used other interventions simultaneously were excluded as these factors could be confounders in evaluating the effects of PM. We also excluded theses, dissertations, and research reports since they were not peer-reviewed.
Information sources and search strategy
Two English electronic databases (PubMed and EMBASE), and two Chinese electronic databases (CNKI and WanFang) were searched for related articles published before October 2020. The following search strategy was used in both English and Chinese articles: (“air pollution” OR “air pollutant*” OR “particulate matter*” OR PM OR PM10 OR PM2.5 OR particle*) AND (“heart rate variability” OR HRV OR “heart period variability” OR “cycle length variability” OR “RR variability” OR “respiratory sinus arrhythmia” OR RSA OR “autonomic nervous system”). We did not use “study design” to search articles because this strategy was originally made to search all exposure studies, including controlled animal studies (Huang et al. 2020). We also identified studies by hand-checking reference lists of included studies and related reviews.
Study selection
Two independent researchers (FH and YZ) screened all articles searched. Firstly, titles and abstracts were reviewed to exclude irrelevant papers. We then read full texts of relevant papers and determined whether they should be included in the review according to the inclusion and exclusion criteria. Disagreements were resolved through discussion along with a third colleague (YL). Data was merged when it comes from the same population but different articles.
Data collection and items
Two independent researchers (FH and YZ) extracted the data from all studies included. Extracted information included study design (randomization, blinding method, wash out between exposure), participants information (health condition, age, gender, body mass index), exposure methods (particle size, concentration, way and duration of exposure, state during exposure), control methods, measurements (HRV indices, assessment time), and statistical methods.
Risk of bias
We assessed the risk of bias in the included studies from five aspects, which are allocation concealment (selection bias), blinding of participants (performance bias), blinding of assessment (detection bias), incomplete outcome data (attrition bias), and wash out between exposure (a typical bias for crossover study). Risk of bias was rated as high, low, or unclear. The appraisal of the risk helps us better understand the quality of included studies.
Data analyses
Our initial goal was to conduct a meta-analysis. However, after reviewing the papers, we found the studies were different to a large extent in exposure (especially particle size and concentration) and participants (especially age and disease condition), which can lead to heterogeneity across studies. Furthermore, the measurement time, statistical method, and results expression of included studies varied dramatically, which makes it difficult to synthesize an overall effect. Therefore, we adopted a descriptive method to summarize the results.
Results
Characteristics of included studies
A total of 12 articles that represent 14 independent studies with 300 participants were included (Fig. 1) (Brook et al. 2014; Byrd et al. 2016; Devlin et al. 2014a, 2003b; Fakhri et al. 2009; Graff et al. 2009; Heusser et al. 2019; Huang et al. 2012; Samet et al. 2009; Tobaldini et al. 2018; Vora et al. 2014; Zareba et al. 2009).
Table 1 shows basic information about the included studies and participants. Thirteen studies adopted a randomized crossover design, and one adopted a randomized control design. Eleven studies were double-blind and the other three were single-blind. To eliminate the effects of previous exposure, washing out is needed in crossover study. All the crossover studies reported the use of washing out except one. The characteristics of participants varied considerably across studies. Participants in 11 studies were healthy, whereas the others were patients with specific diseases, including diabetes, metabolic syndrome, and asthma. Current nonsmokers were reported in thirteen studies. Male participants accounted for 60.3% in total and the mean age of the participants ranged from 24.9 to 66.9 years old.
Table 2 shows exposure and measurement information. Participants in 6 studies were exposed to UFPs, with mean concentration ranging from 10.0 to 98.0 μg/m3; participants in three studies were exposed to coarse concentrated ambient particles (CAPs), with mean concentration ranging from 76.2 to 164.2 μg/m3; participants in 4 studies were exposed to fine CAPs, with mean concentration ranging from 40.5 to 127.03 μg/m3; participants in the remaining study were exposed to the mixture of fine and coarse particles. In terms of exposure way, one study adopted mouthpiece exposure, while all the others adopted whole body exposure. The duration of exposure was 2 h for most studies except two (one used 1-h exposure and the other one used 3-h exposure). Participants in 9 studies were at rest during exposure while participants in the other 5 studies were doing intermittent exercise. All studies used filtered or clean air as control.
Effects of short-term exposure to PM on HRV parameters
Table 3 exhibits the statistical methods and main findings of included studies. The results of time-domain measurements were not consistent across studies. Twelve studies assessed the short-term effects of PM exposure on SDNN. Among these studies, one showed higher SDNN values with exposure to UFPs when considered multiple time points. However, another study showed lower SDNN values 20 h after exposure to coarse CAPs. For RMSSD, 6 studies assessed the effects and one found RMSSD increased during, immediately, and 3 h after UFPs exposure. For PNN50, 8 studies assessed the effects and only one found PNN50 decreased immediately after fine CAPs exposure.
The short-term effects of PM exposure on LF and HF were assessed by all of the 14 studies. Two studies showed LF increased after UFPs exposure at 20-h and 18-h post-exposure time point. The results were not consistent for HF. Four studies showed lower HF values after PM exposure, including UFPs, coarse and fine CAPs. Two studies showed higher HF values after UFPs and fine CAPs exposure. Thirteen studies assessed LF/HF and two studies showed an increase at the time points of 0-h and 20-h post-exposure. Five studies did not find statistically significant results for any HRV parameters.
The statistical methods differed considerably across studies. Most studies collected and analyzed data at two or more time points while one study analyzed the data only at the time point of 1.5-h post-exposure. Paired t-tests were used to compare the observed outcomes at two time points in three studies, and analysis of variance and mixed model were used to compare the observed outcomes at multiple time points in 11 studies. Point values or the changes of HRV in form of difference and ratio of post-exposure to pre-exposure were exhibited in different studies.
Risk of bias
Figure 2 shows the risk of bias of included studies. The risk of selection bias qualified by allocation concealment and detection bias qualified by blinding of assessment were at a level of low for all studies. The risk of performance bias qualified by blinding of participants was high in three studies and low in the other studies. Attrition bias was serious for most studies since incomplete outcome data existed in eight studies. For the other bias, one crossover study did not report the use of washing out.
Discussion
HRV reflects autonomic nervous function and reduced HRV is considered an unfavorable prognostic biomarker for CVD (Bilchick et al. 2020; Tsuji et al. 1996). Altered cardiac autonomic nervous system control of heart rate could be one of the pathophysiological mechanisms by which PM affects the cardiovascular system. Our previous meta-analysis, based on 23 controlled animal studies, found short-term exposure to PM can lead to decrease of SNDD, LF, and LF/HF in rodents (Huang et al. 2020). Epidemiological evidence for human is inadequate. A meta-analysis of cross-sectional and longitudinal studies showed an inverse relationship between particulate air pollution and HRV parameters, including LF, HF, SDNN, and RMSSD (Pieters et al. 2012). However, a recent review of panel studies showed that the evidence is not enough to support the association (Buteau and Goldberg 2016). Crossover design is another common method to investigate the relationship of PM and HRV. Based on the review of 14 crossover/controlled studies, we did not find short-term exposure to PM had a specific effect on HRV.
For frequency-domain parameters, HF almost exclusively reflects parasympathetic function and variation of respiratory (Hayano et al. 1991; Task Force of the European Society of Cardiology 1996). We found the changes of HF after exposure were not consistent across studies. Four studies found HF decreased significantly during or after 2-h exposure to UFPs (Devlin et al., 2014; Vora et al. 2014), coarse (Brook et al. 2014), and fine CAPs (Devlin et al. 2003). These results support the hypothesis that short-term PM exposure can lead to impairment of parasympathetic autonomic function and reduced vagal tone. However, two other studies showed a statistically significant increase of HF after 2-h exposure to UFPs (Samet et al. 2009) and fine CAPs (Fakhri et al. 2009). The participants were aged 18–35 and 19–48, respectively. In contrast, the age of participants in previous 4 studies was 30–60, 27–70, 18–50, and 60–80. It is believed that HF is particularly sensitive to respiratory variation, and this respiratory influence is known to decrease with age (Hayano et al. 1991; Samet et al. 2009; Task Force of the European Society of Cardiology 1996). Therefore, the dichotomy in HF changes may result from the age difference of the studies.
Time-domain measurements RMSSD and PNN50 are also thought to reflect parasympathetic function (Aubert et al. 2003; Hayano et al. 1991; Rowan 3rd et al. 2007; Task Force of the European Society of Cardiology 1996). Six studies measured RMSSD and one study found RMSSD increased during and after UFPs exposure for healthy adults (Zareba et al. 2009). In contrast, eight studies measured PNN50 and one study found PNN50 decreased immediately following fine CAPs exposure for the elderly (Devlin et al. 2003). Meanwhile, more studies showed non-significant results of HF, RMSSD, and PNN50. Therefore, the association of short-term PM exposure and decreased parasympathetic function is inconclusive and needs to be further studied.
LF has been used as a marker of sympathetic function and LF/HF has been used as an index of sympathetic-vagal balance (Acharya et al. 2006; Rowan 3rd et al. 2007). Fourteen studies measured LF and 13 studies measured LF/HF. Two studies showed an increase in LF after exposure to UFPs (Devlin et al. 2014; Samet et al. 2009). Two studies showed an increase in LF/HF after exposure to coarse CAPs (Brook et al. 2014) and UFPs (Devlin et al. 2014). These results indicate sympathetic activation and/or vagal withdrawal. However, the results of SDNN, which may also have sympathetic influence (Hayano et al. 1991; Task Force of the European Society of Cardiology 1996), were not consistent. One study reported decreased SDNN values after exposure to 89.0 μg/m3 coarse CAPs (Graff et al. 2009). Another study reported increased SDNN values with exposure to 10 μg/m3 but not 25 μg/m3 UFPs (Zareba et al. 2009). The authors argued that the concentration of PM might have an influence on the results. Most studies did not report significant results for LF, LF/HF, and SDNN, indicating that the association of PM exposure and sympathetic function is inconclusive and needs to be further studied.
A note of caution should be taken when interpreting these findings, especially the heterogeneity across studies. Firstly, the characteristics of participants and exposure were different. The participants from all of the fourteen studies include both the healthy and patients with certain diseases, all aged from 18 to 80 years old. PM exposure included ultrafine, fine, and coarse particles, and the concentration ranged from 10 to 127.03 μg/m3. Secondly, the statistical methods varied considerably. Paired t-tests, mixed model, and analysis of variance were used to analyze the results. Different studies used different time points and the results were exhibited by different forms, including point value and changes of HRV calculated by subtracting or dividing the pre-exposure values. The heterogeneity makes it difficult to synthesize the results and draw a general conclusion. Furthermore, the exposure time was quite short (1–3 h). This may also have had an influence on the results.
Despite these limitations, the findings have practical implications. To our knowledge, this is the first systematic review of crossover and controlled studies to examine the effects of short-term exposure to PM on cardiac autonomic function, which was measured by HRV parameters in humans. Based on the current evidence, we cannot conclude that short-term exposure (1–3 h) to PM has an influence on autonomic nervous function. The inconsistent changes of HRV in response to PM exposure may have complex mechanisms, which remains to be elucidated.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
Acharya UR, Joseph KP, Kannathal N et al. (2006) Heart rate variability: a review. Medical and Biological Engineering and Computing 44(12): 1031erate
Aubert AE, Seps B, Beckers F (2003) Heart rate variability in athletes. Sports Med 33(12):889–919
Bai L, Wang J, Ma X, Lu H (2018) Air pollution forecasts: an overview. Int J Environ Res Public Health 15(4):780
Bilchick KC, Fetics B, Djoukeng R et al (2020) Prognostic value of heart rate variability in chronic congestive heart failure (Veterans Affairs’ Survival Trial of Antiarrhythmic Therapy in Congestive Heart Failure). Am J Cardiol 90(1):24ay
Brook RD, Bard RL, Morishita M, Dvonch JT, Wang L, Yang HY, Spino C, Mukherjee B, Kaplan MJ, Yalavarthi S, Oral EA, Ajluni N, Sun Q, Brook JR, Harkema J, Rajagopalan S (2014) Hemodynamic, autonomic, and vascular effects of exposure to coarse particulate matter air pollution from a rural location. Environ Health Perspect 122(6):624–630
Buteau S, Goldberg MS (2016) A structured review of panel studies used to investigate associations between ambient air pollution and heart rate variability. Environmental Reasearch 148(207):148
Byrd JB, Morishita M, Bard RL et al (2016) Acute increase in blood pressure during inhalation of coarse particulate matter air pollution from an urban location. Journal of the American Society of Hypertension 10(2):133–139.e4
Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, Caracciolo B, de Faire U, Erbel R, Eriksen KT, Fratiglioni L, Galassi C, Hampel R, Heier M, Hennig F, Hilding A, Hoffmann B, Houthuijs D, Jockel KH, Korek M, Lanki T, Leander K, Magnusson PKE, Migliore E, Ostenson CG, Overvad K, Pedersen NL, P JJ, Penell J, Pershagen G, Pyko A, Raaschou-Nielsen O, Ranzi A, Ricceri F, Sacerdote C, Salomaa V, Swart W, Turunen AW, Vineis P, Weinmayr G, Wolf K, de Hoogh K, Hoek G, Brunekreef B, Peters A (2014) Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ 348:f7412
Chen X, Huang YY, Yun F, Chen TJ, Li J (2015) Effect of changes in sympathovagal balance on the accuracy of heart rate variability obtained from photoplethysmography. Experimental and Therapeutic Medicine 10(6):2311–2318
Devlin RB, Ghio AJ, Kehrl H, Sanders G, Cascio W (2003) Elderly humans exposed to concentrated air pollution particles have decreased heart rate variability. The European Respiratory Journal Supplement 40:–76 sdecr
Devlin RB, Smith CB, Schmitt MT et al (2014) Controlled exposure of humans with metabolic syndrome to concentrated ultrafine ambient particulate matter causes cardiovascular effects. Toxicol Sci 140(1):610
Dong JG (2016) The role of heart rate variability in sports physiology. Experimental and Therapeutic Medicine 11(5):1531–1536
Fakhri AA, Ilic LM, Wellenius GA, Urch B, Silverman F, Gold DR, Mittleman MA (2009) Autonomic effects of controlled fine particulate exposure in young healthy adults: effect modification by ozone. Environ Health Perspect 117(8):1287–1292
Graff DW, Cascio WE, Rappold A, Zhou H, Huang YCT, Devlin RB (2009) Exposure to concentrated coarse air pollution particles causes mild cardiopulmonary effects in healthy young adults. Environ Health Perspect 117(7):1089 10
Hayano J, Sakakibara Y, Yamada A et al (1991) Accuracy of assessment of cardiac vagal tone by heart rate variability in normal subjects. Am J Cardiol 90(1):24you
Heusser K, Tank J, Holz O, May M, Brinkmann J, Engeli S, Diedrich A, Framke T, Koch A, Großhennig A, Jan Danser AH, Sweep FCGJ, Schindler C, Schwarz K, Krug N, Jordan J, Hohlfeld JM (2019) Ultrafine particles and ozone perturb norepinephrine clearance rather than centrally generated sympathetic activity in humans. Sci Rep 9(1):3641
Huang YCT, Rappold AG, Graff DW, Ghio AJ, Devlin RB (2012) Synergistic effects of exposure to concentrated ambient fine pollution particles and nitrogen dioxide in humans. Inhal Toxicol 24(12):790–797
Huang F, Luo Y, Guo Y et al (2016) Particulate matter and hospital admissions for stroke in Beijing, China: modification effects by ambient temperature. J Am Heart Assoc 5(7):e003437
Huang F, Wang P, Pan X, Wang Y, Ren S (2020) Effects of short-term exposure to particulate matters on heart rate variability: a systematic review and meta-analysis based on controlled animal studies. Environ Pollut 256:113306
Kemp AH, Quintana DS (2013) The relationship between mental and physical health: insights from the study of heart rate variability. Int J Psychophysiol 89(3):288–296
Lelieveld J, KlingmingmJ K, Pozzer A et al (2019) Cardiovascular disease burden from ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur Heart J 40(20):159024(12)
Liu Z, Wang F, Li W et al (2018) Does utilizing WHO’s interim targets further reduce the riskm ambient air pollution in Europe reassessed using novel hazard ratio functions. Eur Heart J 40(20):159024(12)–790 797ogy 24(1)
Orellano P, Reynoso J, Quaranta N, Bardach A, Ciapponi A (2020) Short-term exposure to particulate matter (PM10 and PM2.5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: systematic review and meta-analysis. Environ Int 142:105876
Pieters N, Plusquin M, Cox B, Kicinski M, Vangronsveld J, Nawrot TS (2012) An epidemiological appraisal of the association between heart rate variability and particulate air pollution: a meta-analysis. Heart 98(15):1127–1135
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, Alla F, Alvis-Guzman N, Amrock S, Ansari H, Ärnlöv J, Asayesh H, Atey TM, Avila-Burgos L, Awasthi A, Banerjee A, Barac A, Bärnighausen T, Barregard L, Bedi N, Belay Ketema E, Bennett D, Berhe G, Bhutta Z, Bitew S, Carapetis J, Carrero JJ, Malta DC, Castañeda-Orjuela CA, Castillo-Rivas J, Catalá-López F, Choi JY, Christensen H, Cirillo M, Cooper L Jr, Criqui M, Cundiff D, Damasceno A, Dandona L, Dandona R, Davletov K, Dharmaratne S, Dorairaj P, Dubey M, Ehrenkranz R, el Sayed Zaki M, Faraon EJA, Esteghamati A, Farid T, Farvid M, Feigin V, Ding EL, Fowkes G, Gebrehiwot T, Gillum R, Gold A, Gona P, Gupta R, Habtewold TD, Hafezi-Nejad N, Hailu T, Hailu GB, Hankey G, Hassen HY, Abate KH, Havmoeller R, Hay SI, Horino M, Hotez PJ, Jacobsen K, James S, Javanbakht M, Jeemon P, John D, Jonas J, Kalkonde Y, Karimkhani C, Kasaeian A, Khader Y, Khan A, Khang YH, Khera S, Khoja AT, Khubchandani J, Kim D, Kolte D, Kosen S, Krohn KJ, Kumar GA, Kwan GF, Lal DK, Larsson A, Linn S, Lopez A, Lotufo PA, el Razek HMA, Malekzadeh R, Mazidi M, Meier T, Meles KG, Mensah G, Meretoja A, Mezgebe H, Miller T, Mirrakhimov E, Mohammed S, Moran AE, Musa KI, Narula J, Neal B, Ngalesoni F, Nguyen G, Obermeyer CM, Owolabi M, Patton G, Pedro J, Qato D, Qorbani M, Rahimi K, Rai RK, Rawaf S, Ribeiro A, Safiri S, Salomon JA, Santos I, Santric Milicevic M, Sartorius B, Schutte A, Sepanlou S, Shaikh MA, Shin MJ, Shishehbor M, Shore H, Silva DAS, Sobngwi E, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadele Atnafu N, Tesfay F, Thakur JS, Thrift A, Topor-Madry R, Truelsen T, Tyrovolas S, Ukwaja KN, Uthman O, Vasankari T, Vlassov V, Vollset SE, Wakayo T, Watkins D, Weintraub R, Werdecker A, Westerman R, Wiysonge CS, Wolfe C, Workicho A, Xu G, Yano Y, Yip P, Yonemoto N, Younis M, Yu C, Vos T, Naghavi M, Murray C (2017) Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 70(1):1–25
Rowan WH 3rd, Campen MJ, Wichers LB, Watkinson WP (2007) Heart rate variability in rodents: uses and caveats in toxicological studies. Cardiovasc Toxicol 7(1):28: y
Samet JM, Rappold A, Graff D et al (2009) Concentrated ambient ultrafine particle exposure induces cardiac changes in young healthy volunteers. Am J Respir Crit Care Med 179(11):103488–103429
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Circulation 93(5):1043–1065
Thayer JF, Yamamoto SS, Brosschot JF (2010) The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol 141(2):122–131
Tobaldini E, Bollati V, Prado M, Fiorelli EM, Pecis M, Bissolotti G, Albetti B, Cantone L, Favero C, Cogliati C, Carrer P, Baccarelli A, Bertazzi PA, Montano N (2018) Acute particulate matter affects cardiovascular autonomic modulation and IFN-gamma methylation in healthy volunteers. Environ Res 161:97–103
Tsuji H, Mg L, Venditti FJ Jr et al (1996) Impact of reduced heart rate variability on risk for cardiac events. The Framingham Heart Study Circulation 94(11):2850ironm
Vora R, Zareba W, Utell MJ, Pietropaoli AP, Chalupa D, Little EL, Oakes D, Bausch J, Wiltshire J, Frampton MW (2014) Inhalation of ultrafine carbon particles alters heart rate and heart rate variability in people with type 2 diabetes. Particle and Fibre Toxicology 11:31
Weichenthal S (2012) Selected physiological effects of ultrafine particles in acute cardiovascular morbidity. Environ Res 115:26–36
World Health Organization (2016) Ambient air pollution: a global assessment of exposure and burden of disease. World Health Organization, Geneva
Zareba W, Couderc JP, Oberdorster G et al (2009) ECG parameters and exposure to carbon ultrafine particles in young healthy subjects. Inhal Toxicol 21(3):223Heal
Funding
This work was supported by the National Natural Science Foundation of China (grant number 81773512) and the Scientific Research Common Program of Beijing Municipal Commission of Education (grant number KM201810025008).
Author information
Authors and Affiliations
Contributions
HF, YZ, and YL performed the literature search, HF and YL performed the data analysis and drafted the work, PW, YW, and LZ critically revised the work, and YL performed funding acquisition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, F., Zhao, Y., Wang, P. et al. Short-term exposure to particulate matter on heart rate variability in humans: a systematic review of crossover and controlled studies. Environ Sci Pollut Res 28, 35528–35536 (2021). https://doi.org/10.1007/s11356-021-14494-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-14494-1