Abstract
The presented study investigates the effects of morin against toxicity induced by acrylamide (ACR) in the brains of Sprague Dawley rats. In this study, neurotoxicity was induced by orally administering 38.27 mg/kg/b.w ACR to rats through gastric gavage for 10 days. Morin was administered at the same time and at different doses (50 and 100 mg/kg/b.w) with ACR. Biochemical and Western blot analyses showed that ACR increased malondialdehyde (MDA), p38α mitogen-activated protein kinase (p38α MAPK), nuclear factor kappa-B (NF-κB), tumor necrosis factor alpha (TNF-α), interleukin-1 beta (IL-1β), interleukin-6 (IL-6), cyclooxygenase-2 (COX-2), p53, caspase-3, bcl-2 associated X protein (Bax), Beclin-1, light chain 3A (LC3A), and light chain 3B (LC3B) levels and decreased those of superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), glutathione (GSH), b-cell lymphoma-2 (Bcl-2), mammalian target of rapamycin (mTOR), phosphoinositide 3-kinase (PI3K), and protein kinase B (Akt) in brain tissue and therefore induced neurotoxicity by causing oxidative stress, inflammation, apoptosis, and autophagy. On the other hand, it was determined that morin positively affected the levels of these markers by displaying antioxidant, anti-inflammatory, anti-apoptotic, and anti-autophagic properties and had a protective effect on ACR-induced neurotoxicity. As a result, morin is an effective substance against brain damage caused by ACR, yet further studies are needed to use it effectively.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Industrial activities lead to the release of new chemicals into the environment. With the increasing frequency of use of these chemicals in daily life, the rate of chemical poisoning in the general population increases over time (Santhanasabapathy et al. 2015). Some chemicals found in products of general use act as potent neurotoxins causing neurological disorders Grandjean and Landrigan (2014). One of these chemicals is acrylamide (ACR) (acrylic amide, IUPAC name 2-propenamide), which occurs in the water treatment process and in the production of many cosmetic products (Erkekoglu and Baydar 2014; Lakshmi et al. 2012). ACR is also used frequently in many laboratories for gel electrophoresis (Erkekoglu and Baydar 2014). One of the issues that cause worldwide concern about ACR is the occurrence of the Maillard reaction while cooking carbohydrate-rich foods such as French fries at temperatures above 120 °C (Kucukler et al. 2020b; Uthra et al. 2017). In this reaction, amino acids can form ACR by interacting with reducing sugars. The active vinyl group of the ACR interacts with the nitrogen of nucleic acids and the –SH and –NH2 groups of proteins and thus leads to neurotoxicity, genotoxicity, and reproductive toxicity (Abdel-Daim et al. 2015). Moreover, most of the ACR is metabolized by cytochrome P450 2E1 (CYP2E1) mediated epoxidation to glycidamide, which is reported to be more toxic (Erkekoglu and Baydar 2014). Subsequently, it can be metabolized by the glycidamide epoxide hydrolase or conjugated with GSH (Abdel-Daim et al. 2015; Erkekoglu and Baydar 2014; Uthra et al. 2017). Previous studies have shown that ACR triggers oxidative stress due to the formation of reactive oxygen species (ROS) and plays a significant role in ACR toxicity (Cao et al. 2008; Oliveira et al. 2009; Zhao et al. 2015). It has been reported that exogenous antioxidants have the ability to inhibit the formation of glycidiamine and glycidamide-DNA inserts and reduce ACR toxicity by effectively alleviating oxidative stress (Abdel-Daim et al. 2015; Zhao et al. 2015). Therefore, the use of phytochemicals against ACR-induced toxicity has received great attention recently (Zhao et al. 2015).
Flavonoids are phenolic compounds found naturally in many fruits, vegetables, and herbal products (Bai et al. 2020; Kandemir et al. 2020; Kucukler et al. 2020a). Previous studies have indicated that flavonoids can be used as a protective agent against various toxic substances due to their antioxidant, anti-inflammatory, anti-autophagic, and anti-apoptotic properties (Aksu et al. 2018; Al-Numair et al. 2012; Celik et al. 2020a; Çağlayan et al. 2019; Yeung et al. 2019). Morin (2 ′, 3,4 ′, 5,7-pentahydroxyflavone) is an important flavonoid with antioxidant properties derived from onions, almonds, apples, and other Moraceae family members (Celik et al. 2020b; Özdemir et al. 2020; Sang et al. 2017). These natural compounds have also been reported to suppress microglial activation, exert anti-amyloidogenic effects, and improve memory and learning ability (Uddin et al. 2020b; c). Morin provides protection against damage caused by ROS due to its antioxidant properties. Moreover, increasing evidence has been reported that morin regulates CYP450 activity and protects many tissues from oxidative damage (Al-Numair et al. 2012). Morin is also known to have anti-inflammatory, anti-apoptotic, anti-autophagic, anti-bacterial, and chemo-protective effects (Hussein et al. 2019). Although previous studies examining the protective effects of morin on nerve damage have obtained positive results, they have not fully elucidated the underlying mechanism (Zhang et al. 2010). A group working on the Parkinson’s model in mice suggested that in 1-methyl-4-phenyl-1,2,3,6 tetrahydropyridine-induced Parkinson’s disease, morin exerts a neuroprotective effect by suppressing ROS production and NF-κB expression (Lee et al. 2016). In another study, it has been reported that morin attenuates the neurotoxicity induced by an environmental pollutant by reducing the Bax/Bcl-2 ratio (Thangarajan et al. 2018). In addition to these properties, morin has been shown to have no toxic effect even at high doses in experimental animals (Hussein et al. 2019).
There are deficiencies in the literature regarding the mechanisms underlying neurotoxicity caused by ACR. In addition, the protective properties of morin against this toxicity have not been clarified. In the presented study, some inflammatory, apoptotic, and autophagic pathways of ACR that play a role in the development of peripheral neurotoxicity were investigated. In addition, it was aimed to reveal the protective properties of morin against ACR neurotoxicity through these pathways.
Materials and methods
Chemicals
Morin hydrate (CAS No: 654055-01-3, molecular weight: 302.24 g/mol), ACR (CAS Number 79-06-1, molecular weight: 71.08 g/mol), and all other chemicals (thiobarbituric acid (TBA), reduced nicotinamide adenine dinucleotide phosphate (NADP), ethylenediamine tetra acetic acid (EDTA), hydrogen peroxide (H2O2), sodium potassium tartrate, bovine serum albumin, copper(II) chloride, sodium hydroxide, reduced glutathione, 5,5-dithio-bis-(2-nitrobenzoic acid), perchloric acid, xanthine, folin-Ciocalteu reagent, ethanol and hydrochloric acid) were purchased from Sigma Chemical Company (St. Louis, MO).
Animals
Ethics committee approval required to conduct the study was obtained from the Local Ethics Council of Animal Experiments (Approval no: 2017-13 / 161). A total of 35 male Sprague Dawley male rats which are 8–10 weeks old were used in the experiment. The weight of the animals at the beginning of the experiment was 250 ± 20 g. Experimental applications of rats obtained from Experimental Research and Application Center, Ataturk University (Erzurum, Turkey), were carried out in this center. The rats were adapted to the environment for a period of 1 week before the administration. The ambient conditions had 24 ± 1 °C and 45 ± 5% humidity. In addition, it was ensured that the environment the rats were in had a 12 h light/dark cycle. The rats were fed with standard pellet feed and tap water provided ad libitum.
Experimental design
The rats were divided into 5 different groups, and there were 7 animals in each group. 1/3 (38.27 mg/kg /b.w) ACR of the LD50 dose determined by Uthra et al. (2017) was administered in order to cause moderate neurotoxicity in animals. Morin was given according to the doses determined by Celik et al. (2020b). Experimental groups are designed as follows:
-
Control: Rats were given physiological saline orally by gastric gavage for 10 days.
-
Morin-100: Rats were given 100 mg/kg/b.w morin hydrate orally by gastric gavage for 10 days.
-
ACR: The rats were given 38.27 mg/kg/b.w ACR orally by gastric gavage for 10 days.
-
ACR + Morin-50: Both 38.27 mg/kg/b.w ACR and 50 mg/kg/b.w morin hydrate were administered orally to rats by gastric gavage for 10 days.
-
ACR + Morin-10: Both 38.27 mg/kg/b.w ACR and 100 mg/kg/b.w morin hydrate were administered orally to rats by gastric gavage for 10 days.
The rats were decapitated under mild sevoflurane (Sevorane, Abbott Laboratories, Istanbul-Turkey) anesthesia 24 h after the last drug administration (11th day). After decapitation, the cortex brain tissues of the animals were taken and stored at −80 °C until biochemical analysis.
Determination of lipid peroxidation degrees in brain tissue
Brain tissue was pulverized in liquid nitrogen by means of a homogenizer (Tissue Lyser II, Qiagen, Netherlands), and the pulverized tissues were used in all analyses. Then, with this device, tissues were homogenized by diluting with 1.15% potassium chloride at a ratio of 1:10 (w/v). The homogenates obtained were centrifuged at 3500 rpm for 15 min. Malondialdehyde (MDA) levels were measured in the homogenates obtained to determine the degree of lipid peroxidation. MDA analyses were performed according to the method of Placer et al. (1966). This method is based on measuring the color formed as a result of the reaction of MDA with TBA at a wavelength of 532 nm. Results were determined as nmol/g tissue.
Determination of enzymatic (SOD, CAT, and GPx) and non-enzymatic (GSH) antioxidant levels in brain tissue
Enzymatic [superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx)] and non-enzymatic [glutathione (GSH)] antioxidant levels were measured in homogenates obtained from brain tissue. Homogenates were centrifuged at 3500 rpm for 15 min for SOD and CAT activities, while they were centrifuged at 10,000 rpm for 20 min for measurement of GPx activity and GSH amount. In all analyses, centrifugation of homogenates was carried out at +4 °C. The method of Sun et al. (1988) was used for SOD activity. This method is based on the nitroblue tetrazolium (NBT) degradation of the superoxide radical produced by the xanthinoxanthine oxidase system and formazan. The activity level was determined as U/g protein. The method by Aebi (1984) was used for CAT activity, and the results were expressed as catal/g protein. In this method, catalase activity was determined by spectrophotometric measurement of the amount of hydrogen peroxide consumed per unit time. GPx activity and GSH amount were determined according to the methods of Lawrence and Burk (1976) and Sedlak and Lindsay (1968), respectively. The level of GPx activity was given as U/g protein, while the amount of GSH was expressed as nmol/g tissue.
Analysis of total protein levels in brain tissue
Total protein content of the brain tissue was made by using the homogenates obtained with the method by Lowry et al. (1951). Total protein levels of the samples were calculated by comparing the absorbance values from different concentrations of albumin.
Determination of the levels of inflammatory markers in brain tissue
To measure the level of inflammation in the brain tissue, the activities of p38α mitogen-activated protein kinase (p38α MAPK) and cyclooxygenase-2 (COX-2) and the levels of nuclear factor kappa B (NF-κB), tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), and interleukin-6 (IL-6) were measured. In this way, homogenates were prepared from the brain tissue diluted with phosphate buffer saline (PBS) at a ratio of 1:20 (w/v) by means of a homogenizer. Supernatants obtained by centrifuging homogenates at 3500 rpm for 15 min and 4 °C were used for analysis. Analyses of all inflammatory markers were performed with commercial kits purchased from YL Biont (Shanghai, China), according to the procedure specified by the manufacturer.
Determination of the levels of autophagic markers in brain tissue
The levels of Beclin-1, light chain 3A (LC3A), and light chain 3B (LC3B) were measured in previously prepared supernatants to determine the degree of autophagy in brain tissue. Commercial kits (YL Biont, Shanghai, China) were used for measurements. After the analyses were performed according to the procedure specified by the manufacturer, the absorbance values were obtained by reading the plate at 450 nm wavelength by means of enzyme-linked immunosorbent assay (ELISA) microplate reader (Bio-Tek, Winooski, VT, USA). The amount of autophagic markers in the samples was determined by comparing the absorbance values obtained with the absorbance values of the standards.
Western blot analysis of brain tissue
Brain tissues taken from rats were homogenized after diluting 1: 5 (w/v) with Mammalian Cell Extraction Kit (ab65399, Abcam, UK). The homogenates were then centrifuged at 14,000 rpm for 3 min. Tissue proteins were prepared by denaturing using Laemmli buffer (Bromophenol blue, Tris-HCl pH 6.8, glycerol, 2-mercaptoethanol, SDS). Afterwards, equal volumes of protein samples were taken, and the run was performed in 15% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE), and proteins were separated from each other. After electrophoresis, the proteins from the gel were transferred to nitrocellulose membranes (0.2 μm pore size). The membrane was blocked for 1 h after 2 washes in TBS-0.05% Tween 20 (TBS-T). This was done in 5% skim milk powder. At the end of this period, the membranes were left to incubate in a shaker at 4 °C for 1 night with primary antibodies β-actin (sc-47778), Bax (sc-20067), Bcl-2 (sc-7382), procaspase-3 (sc-271759), and cytochrome c (sc-13156). The next day, membranes treated with primers were washed 5 times with TBS-T for 5 min. After washing, it was incubated with anti-mouse secondary antibody (goat anti mouse IgG, sc-2005) for 1 and a half hours at 37 °C. Protein levels were analyzed with a photo analysis system (GelDoc EZ and Image Lab. 5.2.1 software, Bio-Rad, USA).
Determination of the levels of apoptotic markers in brain tissue
The level of apoptosis in brain tissue was determined by the analysis of p53, caspase-3, bcl-2 associated X protein (Bax), and b-cell lymphoma-2 (Bcl-2) markers in supernatants. P53, Bax, and Bcl-2 levels were YL Biont (Shanghai, China), and caspase-3 levels were made according to the procedure determined by the companies with commercial kits obtained from Sunred Biological Technology (Shanghai, China).
Determination of PI3K, mTOR, and Akt activities in brain tissue
Measurement of mammalian target of rapamycin (mTOR) levels and phosphoinositide 3-kinase (PI3K) and protein kinase B (Akt) activities in brain tissue were determined with kits purchased from YL Biont (Shanghai, China). PI3K, mTOR, and Akt levels were calculated by comparing the absorbance values obtained from the ELISA reader with the absorbents of the standards.
Statistical analysis
Statistical analysis of the data obtained by biochemical methods was performed by one-way analysis of variance (one-way ANOVA). Whether there is a difference between the groups was determined by Tukey’s multiple comparison test. Results were given as mean ± standard error (S.E.M). Values from Western blot analysis were taken after at least three replicates. GraphPad Prism 5 program was used for statistical analysis. One-way ANOVA and Newman-Keuls post hoc tests were performed on the data.
Results
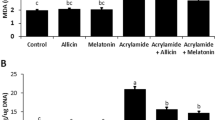
Effects of morin against lipid peroxidation caused by ACR in brain tissue
The effects of morin on MDA levels, the lipid peroxidation marker, in the brain tissue induced by ACR are presented in Table 1. Analysis results showed that ACR increased MDA levels about 2 times compared to control group (p <0.001) and thus caused significant oxidative damage in brain tissue. On the other hand, it was determined that there was a decrease in MDA levels (p <0.001) in the groups given ACR and morin compared to the ACR application alone, and this decrease was higher in the ACR + MH-100 group compared to the low dose group (p <0.05).
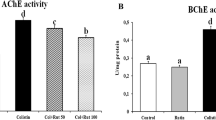
Effects of morin on enzymatic and non-enzymatic antioxidant levels in ACR-induced brain tissue
It was determined that the activities of antioxidant enzymes (SOD, CAT, and GPx) were significantly suppressed in the brain tissues of the rats treated with ACR compared to the control group (p < 0.001). In addition, the decrease in GSH levels is another indicator that ACR triggers oxidative stress in brain tissue. Morin, on the other hand, was found to significantly restore SOD, CAT, and GPx activities suppressed by ACR (p < 0.001). In addition, it was found that morin administration increased GSH levels compared to the ACR group. According to the results, it was determined that MH-100 group was more effective against oxidative stress induced by ACR. Enzymatic and non-enzymatic antioxidant levels are summarized in Table 1.
Effects of morin against ACR-induced neuroinflammation
The levels of inflammation markers belonging to the brain tissue are presented in Fig. 1. Accordingly, it was found that ACR caused p38α MAPK and COX-2 activation, while morin decreased these enzyme activities compared to the ACR group (p <0.001). It was also determined that the levels of NF-κB, TNF-α, IL-1β, and IL-6, which are important markers of inflammation, increased with ACR administration. The decrease in NF-κB, TNF-α, IL-1β, and IL-6 levels in brain tissue with morin administration shows that morin alleviates the inflammation caused by ACR (p <0.001). However, it was observed that morin did not alter TNF-α, IL-1β, and IL-6 levels between doses.
a Effects of ACR and morin administration on p38α MAPK activity in brain tissue of rats. b Effects of ACR and morin administration on NF-κB levels in brain tissue of rats. c Effects of ACR and morin administration on TNF-α levels in brain tissue of rats. d Effects of ACR and morin administration on IL-1β levels in brain tissue of rats. e Effects of ACR and morin administration on IL-6 levels in brain tissue of rats. f Effects of ACR and morin administration on COX-2 activity in brain tissue of rats. Data were presented as mean ± SEM. ***p < 0.001 control vs others, **p < 0.01 control vs others, *p < 0.05 control vs others; ###p < 0.001 ACR vs others, ##p < 0.01 ACR vs others, #p < 0.05 ACR vs others; ns not significant
Effects of morin on ACR-induced autophagy in brain tissue
In the present study, it was determined that ACR significantly increased the autophagic markers beclin-1, LC3A, and LC3B levels compared to the control group (p <0.001) (Fig. 2). However, it was detected that morin decreased beclin-1, LC3A, and LC3B levels compared to the group treated with ACR alone (p <0.001) (Fig. 2) and provided protection against ACR-induced autophagy.
a Effects of ACR and morin administration on Beclin-1 levels in brain tissue of rats. b Effects of ACR and morin administration on LC3A levels in brain tissue of rats. c Effects of ACR and morin administration on LC3B levels in brain tissue of rats. Data were presented as mean ± SEM. ***p < 0.001 control vs others, **p < 0.01 control vs others, *p < 0.05 control vs others; ###p < 0.001 ACR vs others, ##p < 0.01 ACR vs others, #p < 0.05 ACR vs others; ns not significant
Effects of morin against ACR-induced apoptosis in brain tissue
To further investigate the molecular mechanisms of the anti-apoptotic effects of morin against ACR-induced apoptosis, we focused on the expression of pro-apoptotic Bax, cytochrome C, and anti-apoptotic Bcl-2 and procaspase-3 proteins in brain tissues. At the same time, the ratios of Bax/Bcl-2 expression levels in these tissues were analyzed because the calculation of the Bax/Bcl-2 ratio is important for understanding the induction of apoptosis. According to the Bax/Bcl-2 expression ratio, it was observed that protein levels increased significantly in ACR-treated group and decreased in morin-treated groups (Fig. 3B-III). At the end of the study, it was observed that the cytochrome C protein level increased significantly in the ACR-treated groups and the protein expression level decreased significantly in the ACR + Morin 50 and ACR + Morin 100 groups (Fig. 3B-IV). Additionally, in ACR-induced samples, the levels of pro-caspase-3 protein decreased (increase in active caspase-3), while there was either no change or an increase in the level of procaspase-3 in the ACR + Morin 50 and ACR + Morin 100 groups (Fig. 3B-V).
Effect of morin on apoptotic markers in neurotoxicity caused by ACR. Protein levels (a) Bax (bcl-2 associated X protein) (23 kDa), b-cell lymphoma-2 (Bcl-2) (26 kDa), cytochrome c (15 kDa), and procaspase-3 (34 kDa) were measured by Western blotting. β-Actin was used as reference. b Data were presented as mean ± SEM. ***p < 0.001 control vs others, **p < 0.01 control vs others, *p < 0.05 control vs others; ###p < 0.001 ACR vs others, ##p < 0.01 ACR vs others, #p < 0.05 ACR vs others; ns not significant
Apoptotic p53, caspase-3, Bax, and anti-apoptotic Bcl-2 levels in the brain tissue were investigated by biochemical method, and the results, similar to the Western blot method, showed that ACR triggers apoptosis by increasing p53, caspase-3, and Bax levels and decreasing Bcl-2 levels (p <0.001) (Fig. 4). Morin treatment, on the other hand, was found to reduce these apoptotic markers and increase Bcl-2 levels, thus alleviating ACR-induced apoptosis (Fig. 4). The results reveal that morin may play an anti-apoptotic role in ACR-treated rats.
a Effects of ACR and morin administration on p53 levels in brain tissue of rats. b Effects of ACR and morin administration on caspase-3 activity in brain tissue of rats. c Effects of ACR and morin administration on Bax levels in brain tissue of rats. d Effects of ACR and morin administration on Bcl-2 levels in brain tissue of rats. Data were presented as mean ± SEM. ***p < 0.001 control vs others, **p < 0.01 control vs others, *p < 0.05 control vs others; ###p < 0.001 ACR vs others, ##p < 0.01 ACR vs others, #p < 0.05 ACR vs others; ns not significant
Effects of morin on PI3K, mTOR, and Akt activities in ACR-induced brain tissue
In our study, the PI3K/Akt/mTOR pathway, which has an important role in the regulation of autophagy and apoptosis, was examined in brain tissue, and the results are presented in Fig. 5. The data demonstrate that ACR downregulates the mTOR/PI3K/Akt pathway in brain tissue. Nevertheless, it was determined that the administration of morin significantly increased the mTOR, PI3K (p <0.001), and Akt (p <0.05) levels compared to the ACR group, yet there was no difference between the doses.
a Effects of ACR and morin administration on mTOR levels in brain tissue of rats. b Effects of ACR and morin administration on PI3K activity in brain tissue of rats. c Effects of ACR and morin administration on Akt activity in brain tissue of rats. Data were presented as mean ± SEM. ***p < 0.001 control vs others, **p < 0.01 control vs others, *p < 0.05 control vs others; ###p < 0.001 ACR vs others, ##p < 0.01 ACR vs others, #p < 0.05 ACR vs others; ns not significant
Discussion
ACR, which has been used in various fields since the 1980s, is also formed by cooking carbohydrate-rich foods at high temperatures. Therefore, humans are chronically exposed to this toxic substance at low concentrations, and toxicity occurs in many organs, including the brain (Prasad 2012, Tian et al. 2015). Based on this, researchers have recently been working hard to elucidate the toxicity mechanisms of ACR and to find new therapeutic options against the damage. In the present study, the effects of morin against neurotoxicity caused by ACR were investigated through oxidative stress, inflammation, apoptosis, and autophagy pathways. The results revealed that morin is an important protective agent against ACR-induced neurotoxicity.
Reactive oxygen species (ROS), which are by-products of oxidative metabolism such as superoxide, peroxides, and hydroxyl radical, form the pathogenesis of various diseases by attacking DNA, proteins, and lipids in cells (Abdel-Daim et al. 2015; 2020b; Elhelaly et al. 2019). Enzymatic (SOD, CAT, and GPx) and non-enzymatic (GSH) antioxidant defense system maintains oxidant-antioxidant balance by clearing ROS produced in the body under normal conditions (AlKahtane et al. 2020; Temel et al. 2020). However, since various chemical agents, including ACR, increase ROS production excessively, this balance is disrupted and oxidative stress occurs (Abdel-Daim et al. 2015). The high metabolic rate, low cellular regeneration capacity, and high levels of polyunsaturated fatty acids in the brain tissue cause this tissue to be much more sensitive to ROS than other tissues (Celik et al. 2020c; Dai et al. 2018; Syed et al. 2018). Indeed, there is increasing evidence that oxidative stress can cause neurodegeneration (Syed et al. 2018). Previous studies have reported that ACR also triggers oxidative stress by increasing reactive oxygen species and thus leads to neurotoxicity (Abdel-Daim et al. 2020a; Elhelaly et al. 2019; Goudarzi et al. 2019; Zhao et al. 2017). However, researchers have shown that morin may have a neuroprotective effect by alleviating oxidative stress (Thangarajan et al. 2018). In the current study, it was seen that ACR caused oxidative stress by causing a decrease in antioxidant enzyme activities and an increase in lipid peroxidation. Possible reasons for this are thought to be due to the fact that ACR depletes GSH stores while converting to the non-toxic form [N-Acetyl-S- (2-carbamoylmethyl) cysteine] and inhibits antioxidant enzymes by binding to -SH groups. Furthermore, it was determined that morin decreases lipid peroxidation by increasing enzymatic and non-enzymatic antioxidant levels, thus alleviating oxidative stress triggered by ACR. It is thought that the antioxidant effect of morin is due to the property of scavenging ROS by the hydroxyl groups in its structure.
Inflammation in the central nervous system (CNS) plays a fundamental role in the pathogenesis of a variety of neurodegenerative diseases (Kabir et al. 2021; Uddin et al. 2020a; Yan et al. 2019; Yardım et al. 2020b). NF-κB and MAPK signaling pathways have significant roles in the regulation of inflammation and in neurodegenerative diseases (Dong et al. 2019; Jin et al. 2020). NF-κB is a nuclear transcription factor that contributes significantly to the inflammation process by increasing the transcription of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 and COX-2, which is known to play a role in the inflammatory response (Dong et al. 2019; Ileriturk et al. 2020; Tao et al. 2018). A previous study reported that activation of NF-κB causes neuroinflammation (Yakovleva et al. 2011). Oxidative stress is among the leading causes of inflammation in the CNS. Oxidative stress contributes to this process by activating NF-κB (Çelik et al. 2020; Yan et al. 2019). The MAPK family, consisting of the ERK, JNK, and P38 signaling pathways, is also one of the important factors mediating inflammation. It is known that MAPK activates NF-κB by disrupting the IκB-NF-κB complex (Dong et al. 2019; Yang et al. 2016; Youn et al. 2018). Another study reported that ACR activates NF-κB and that neuroinflammation occurs due to the increase in pro-inflammatory cytokine levels accordingly (Pan et al. 2018). Similarly, our findings revealed that ACR increased TNF-α, IL-1β, and IL-6 levels and COX-2 activity, in addition to the increase in p38α MAPK and NF-κB levels, thereby causing neuroinflammation. Because of the importance of MAPK and NF-κB signaling pathways in inflammation, the use of therapeutics targeting these pathways against inflammatory agents will provide significant advantages in treatment. Previous studies reported that morin attenuates inflammation by suppressing NF-κB activation in various tissues (Jiang et al. 2019; Lee et al. 2016). In our study, it was found that morin can significantly protect against neuroinflammation induced by ACR by decreasing the levels of p38α MAPK and NF-κB.
Mitochondrial membrane permeability is particularly controlled by the Bcl-2 proto-oncogene family, including anti-apoptotic Bcl-2 and pro-apoptotic Bax proteins (Thangarajan et al. 2018; Yardim et al. 2020). The penetration of Bax into the mitochondria with its activation causes impairment of membrane permeability. This leads to cytochrome c release and activation of caspases, which greatly contribute to the initiation of the apoptotic process (Thangarajan et al. 2018). Normally, apoptosis provides the environmental adaptation of neurons in the nervous system. However, in adverse situations that may occur, apoptosis balance is disturbed. This imbalance plays a crucial role in many neurodegenerative diseases. Apoptosis is also known to be an important factor in ACR-induced neuropathy (Sun et al. 2018). The Bcl-2 protein increases the membrane potential by inactivating Bax and suppresses the apoptotic process (Aksu et al. 2016; Thangarajan et al. 2018). Nonetheless, it contributes to the apoptotic pathway by decreasing Bcl-2 expression of the p53 protein (Yang et al. 2016). An important factor causing the initiation of the apoptotic process is caspase-3 activation (Kandemir et al. 2017; Tabeshpour et al. 2019). Caspase-3 is known to be activated by increasing cytochrome c, Bax, and p38α MAPK and decreased Bcl-2 expressions (Darendelioglu et al. 2016; Sun et al. 2018; Tabeshpour et al. 2020). Previous studies have shown that ACR causes an increase in the ratio of Bax/Bcl-2, triggers cytochrome c release, and activates the apoptotic pathway by activating caspase-9, resulting in neurotoxicity (Chen et al. 2013; Lakshmi et al. 2012). Similarly, in our study, it was detected that ACR increases Bax/Bcl-2 ratio and p53 expression, causes cytochrome c release, and activates caspase-3 accordingly. In addition, the fact that caspase-3 activation occurred in correlation with the increase of p38AP MAPK explains the relationship between these two factors. Morin, on the other hand, was determined to inhibit the Bax/Bcl-2/caspase-3 pathway by attenuating cytochrome c release, thus displaying anti-apoptotic properties.
Although the high occurrence of autophagy causes cellular dysfunction and cell death, this biological process normally has an essential role in clearing and recycling components of aged or damaged cells (Aksu et al. 2020; Yang et al. 2018; Yuntao et al. 2016). Autophagy begins with the formation of double-membrane vesicles called autophagosomes. Autophagosomes form autophagolysosomes by combining with lysosomes, leading to their contents to be decomposed into basic molecules and recycled for reuse (Yuntao et al. 2016). Previous studies have shown that autophagy plays an important role in various neurodegenerative diseases (Anglade et al. 1997; Boland et al. 2008). Beclin-1 is responsible for initiating autophagy. Beclin-1 contains a Bcl-2 homology domain 3 (BH3) domain in its structure. Autophagic activity Beclin-1 is hampered by Bcl-2 family proteins. LC3 is an important precursor for monitoring autophagosome formation (Buyuklu et al. 2015). During the realization of autophagy, the cytoplasmic LC3A is transformed into the autophagosomal membrane-bound LC3B form (McCoy et al. 2010). Previous studies reported that various toxic substances increase Beclin-1 and LC3 expressions and cause neurotoxicity by triggering autophagy (Xu et al. 2018; Yang et al. 2018; Yardım et al. 2020a; Yuntao et al. 2016). On the other hand, mTOR is a negative regulator of autophagic activity in eukaryotic cells (Cao et al. 2016). It was also reported that PI3K-activated Akt positively regulates mTOR (Mohamed et al. 2018) and suppresses the expression and functions of Atg proteins that induce autophagy accordingly. Thus, the PI3K/Akt/mTOR signaling pathway has been reported to play a suppressive role on autophagy (Vucicevic et al. 2011). Manthari et al. (2018) reported that arsenic down-regulated PI3K, Akt, and mTOR expressions in mouse cerebral cortex and hippocampus, thereby increasing autophagy and causing neurotoxicity. In the present study, it was seen that ACR increased Beclin-1, LC3A, and LC3B levels by down-regulating the PI3K/Akt/mTOR signaling pathway, thereby activating autophagy in brain tissue. The fact that ACR increases Beclin-1 levels by decreasing Bcl-2 levels strengthens the evidence for the relationship between these two. It was also determined that morin activates the PI3K/Akt/mTOR signal pathway against ACR by showing anti-autophagic properties and suppresses the Beclin-1/LC3A/LC3B signal pathway.
Conclusion
Taken together, the present study revealed that ACR, which is a highly toxic substance that affects all people globally, causes neurotoxicity by initiating oxidative stress, inflammatory response, autophagy, and apoptotic process in brain tissue. On the other hand, morin, a natural antioxidant, alleviated ACR-induced inflammation, autophagy, and apoptosis by acting on the indicated signaling pathways, thus protecting against the development of neurotoxicity. In conclusion, morin is an effective substance that can be used against neuronal damage caused by ACR. Still, this needs to be supported by further studies.
Data availability
Not applicable
References
Abdel-Daim MM, Abd Eldaim MA, Hassan AG (2015) Trigonella foenum-graecum ameliorates acrylamide-induced toxicity in rats: roles of oxidative stress, proinflammatory cytokines, and DNA damage. Biochem Cell Biol 93:192–198
Abdel-Daim MM, El-Ela FIA, Alshahrani FK, Bin-Jumah M, Al-Zharani M, Almutairi B, Alyousif MS, Bungau S, Aleya L, Alkahtani S (2020a) Protective effects of thymoquinone against acrylamide-induced liver, kidney and brain oxidative damage in rats. Environ Sci Pollut Res 27:37709–37717
Abdel-Daim MM, Mahmoud OM, Al Badawi MH, Alghamdi J, Alkahtani S, Salem NA (2020b) Protective effects of Citrus limonia oil against cisplatin-induced nephrotoxicity. Environ Sci Pollut Res 27:41540–41550
Aebi H (1984) [13] Catalase in vitro, methods in enzymology. Elsevier 121-126
Aksu EH, Ozkaraca M, Kandemir FM, Omur AD, Eldutar E, Kucukler S, Comakli S (2016) Mitigation of paracetamol-induced reproductive damage by chrysin in male rats via reducing oxidative stress. Andrologia 48:1145–1154
Aksu EH, Kandemir FM, Kucukler S, Mahamadu A (2018) Improvement in colistin-induced reproductive damage, apoptosis, and autophagy in testes via reducing oxidative stress by chrysin. J Biochem Mol Toxicol 32:e22201
Aksu EH, Kandemir FM, Küçükler S (2020) The effects of hesperidin on colistin-induced reproductive damage, autophagy, and apoptosis by reducing oxidative stress. Andrologia e13900
AlKahtane AA, Ghanem E, Bungau SG, Alarifi S, Ali D, AlBasher G, Alkahtani S, Aleya L, Abdel-Daim MM (2020) Carnosic acid alleviates chlorpyrifos-induced oxidative stress and inflammation in mice cerebral and ocular tissues. Environ Sci Pollut Res 27:11663–11670
Al-Numair KS, Chandramohan G, Alsaif MA (2012) Pretreatment with morin, a flavonoid, ameliorates adenosine triphosphatases and glycoproteins in isoproterenol-induced myocardial infarction in rats. J Nat Med 66:95–101
Anglade P, Vyas S, Javoy-Agid F, Herrero MT, Michel PP, Marquez J, Mouatt-Prigent A, Ruberg M, Hirsch EC, Agid Y (1997) Apoptosis and autophagy in nigral neurons of patients with Parkinson's disease. Histol Histopathol 12:25–31
Bai J, Li L, Zhao S, Fan X, Zhang J, Hu M, Chen Y, Sun Y, Wang B, Jin J, Wang X, Zhang D, Hu J, Li Y (2020) Heterotropic activation of flavonoids on cytochrome P450 3A4: a case example of alleviating dronedarone-induced cytotoxicity. Toxicol Lett 319:187–196
Boland B, Kumar A, Lee S, Platt FM, Wegiel J, Yu WH, Nixon RA (2008) Autophagy induction and autophagosome clearance in neurons: relationship to autophagic pathology in Alzheimer’s disease. J Neurosci 28:6926–6937
Buyuklu M, Kandemir FM, Ozkaraca M, Set T, Bakirci EM, Topal E, Ileriturk M, Turkmen K (2015) Benefical effects of lycopene against contrast medium-induced oxidative stress, inflammation, autophagy, and apoptosis in rat kidney. Hum Exp Toxicol 34:487–496
Çağlayan C, Taslimi P, Demir Y, Küçükler S, Kandemir FM, Gulçin İ (2019) The effects of zingerone against vancomycin-induced lung, liver, kidney and testis toxicity in rats: the behavior of some metabolic enzymes. J Biochem Mol Toxicol 33:e22381
Cao J, Liu Y, Jia L, Jiang LP, Geng CY, Yao XF, Kong Y, Jiang BN, Zhong LF (2008) Curcumin attenuates acrylamide-induced cytotoxicity and genotoxicity in HepG2 cells by ROS scavenging. J Agric Food Chem 56:12059–12063
Cao L, Walker MP, Vaidya NK, Fu M, Kumar S, Kumar A (2016) Cocaine-mediated autophagy in astrocytes involves sigma 1 receptor, PI3K, mTOR, Atg5/7, Beclin-1 and induces type II programed cell death. Mol Neurobiol 53:4417–4430
Çelik H, Kucukler S, Çomaklı S, Caglayan C, Özdemir S, Yardım A, Karaman M, Kandemir FM (2020) Neuroprotective effect of chrysin on isoniazid-induced neurotoxicity via suppression of oxidative stress, inflammation and apoptosis in rats. Neurotoxicology 81:197–208
Celik H, Kandemir FM, Caglayan C, Ozdemir S, Comakli S, Kucukler S, Yardim A (2020a) Neuroprotective effect of rutin against colistin-induced oxidative stress, inflammation and apoptosis in rat brain associated with the CREB/BDNF expressions. Mol Biol Rep 47:2023–2034
Celik H, Kucukler S, Comakli S, Ozdemir S, Caglayan C, Yardim A, Kandemir FM (2020b) Morin attenuates ifosfamide-induced neurotoxicity in rats via suppression of oxidative stress, neuroinflammation and neuronal apoptosis. Neurotoxicology 76:126–137
Celik H, Kucukler S, Ozdemir S, Comakli S, Gur C, Kandemir FM, Yardim A (2020c) Lycopene protects against central and peripheral neuropathy by inhibiting oxaliplatin-induced ATF-6 pathway, apoptosis, inflammation and oxidative stress in brains and sciatic tissues of rats. Neurotoxicology 80:29–40
Chen J-H, Yang C-H, Wang Y-S, Lee J-G, Cheng C-H, Chou C-C (2013) Acrylamide-induced mitochondria collapse and apoptosis in human astrocytoma cells. Food Chem Toxicol 51:446–452
Dai C, Ciccotosto GD, Cappai R, Tang S, Li D, Xie S, Xiao X, Velkov T (2018) Curcumin attenuates colistin-induced neurotoxicity in N2a cells via anti-inflammatory activity, suppression of oxidative stress, and apoptosis. Mol Neurobiol 55:421–434
Darendelioglu E, Aykutoglu G, Tartik M, Baydas G (2016) Turkish propolis protects human endothelial cells in vitro from homocysteine-induced apoptosis. Acta Histochem 118:369–376
Dong P, Ji X, Han W, Han H (2019) Oxymatrine exhibits anti-neuroinflammatory effects on Aβ1–42-induced primary microglia cells by inhibiting NF-κB and MAPK signaling pathways. Int Immunopharmacol 74:105686
Elhelaly AE, AlBasher G, Alfarraj S, Almeer R, Bahbah EI, Fouda MM, Bungău SG, Aleya L, Abdel-Daim MM (2019) Protective effects of hesperidin and diosmin against acrylamide-induced liver, kidney, and brain oxidative damage in rats. Environ Sci Pollut Res 26:35151–35162
Erkekoglu P, Baydar T (2014) Acrylamide neurotoxicity. Nutr Neurosci 17:49–57
Goudarzi M, Mombeini MA, Fatemi I, Aminzadeh A, Kalantari H, Nesari A, Najafzadehvarzi H, Mehrzadi S (2019) Neuroprotective effects of ellagic acid against acrylamide-induced neurotoxicity in rats. Neurol Res 41:419–428
Grandjean P, Landrigan PJ (2014) Neurobehavioural effects of developmental toxicity. Lancet Neurol 13:330–338
Hussein MM, Gad E, Ahmed MM, Arisha AH, Mahdy HF, Swelum AA-A, Tukur HA, Saadeldin IM (2019) Amelioration of titanium dioxide nanoparticle reprotoxicity by the antioxidants morin and rutin. Environ Sci Pollut Res 26:29074–29084
Ileriturk M, Benzer F, Aksu EH, Yildirim S, Kandemir FM, Dogan T, Dortbudak MB, Genc A (2020) Chrysin protects against testicular toxicity caused by lead acetate in rats with its antioxidant, anti-inflammatory, and antiapoptotic properties. Journal of Food Biochemistry e13593
Jiang K, Shi J, Shi J (2019) Morin alleviates vincristine-induced neuropathic pain via nerve protective effect and inhibition of NF-κB pathway in rats. Cell Mol Neurobiol 39:799–808
Jin H, Peng X, He Y, Ruganzu JB, Yang W (2020) Tanshinone IIA suppresses lipopolysaccharide-induced neuroinflammatory responses through NF-κB/MAPKs signaling pathways in human U87 astrocytoma cells. Brain Res Bull 164:136–145
Kabir MT, Uddin MS, Zaman S, Rahman MS, Behl T, Ahmad A, Hafeez A, Perveen A, Ashraf GM (2021) Exploring the anti-neuroinflammatory potential of steroid and terpenoid-derived phytochemicals to combat Alzheimer’s Disease. Curr Pharm Des 26
Kandemir FM, Kucukler S, Caglayan C, Gur C, Batil AA, Gülçin İ (2017) Therapeutic effects of silymarin and naringin on methotrexate-induced nephrotoxicity in rats: biochemical evaluation of anti-inflammatory, antiapoptotic, and antiautophagic properties. J Food Biochem 41:e12398
Kandemir FM, Caglayan C, Aksu EH, Yildirim S, Kucukler S, Gur C, Eser G (2020) Protective effect of rutin on mercuric chloride-induced reproductive damage in male rats. Andrologia 52:e13524
Kucukler S, Benzer F, Yildirim S, Gur C, Kandemir FM, Bengu AS, Ayna A, Caglayan C, Dortbudak MB (2020a) Protective effects of chrysin against oxidative stress and inflammation induced by lead acetate in rat kidneys: a biochemical and histopathological approach. Biol Trace Elem Res
Kucukler S, Caglayan C, Darendelioğlu E, Kandemir FM (2020b) Morin attenuates acrylamide-induced testicular toxicity in rats by regulating the NF-κB, Bax/Bcl-2 and PI3K/Akt/mTOR signaling pathways. Life Sci 261:118301
Lakshmi D, Gopinath K, Jayanthy G, Anjum S, Prakash D, Sudhandiran G (2012) Ameliorating effect of fish oil on acrylamide induced oxidative stress and neuronal apoptosis in cerebral cortex. Neurochem Res 37:1859–1867
Lawrence RA, Burk RF (1976) Glutathione peroxidase activity in selenium-deficient rat liver. Biochem Biophys Res Commun 71:952–958
Lee KM, Lee Y, Chun HJ, Kim AH, Kim JY, Lee JY, Ishigami A, Lee J (2016) Neuroprotective and anti-inflammatory effects of morin in a murine model of Parkinson’s disease. J Neurosci Res 94:865–878
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Manthari RK, Tikka C, Ommati MM, Niu R, Sun Z, Wang J, Zhang J, Wang J (2018) Arsenic induces autophagy in developmental mouse cerebral cortex and hippocampus by inhibiting PI3K/Akt/mTOR signaling pathway: involvement of blood-brain barrier's tight junction proteins. Arch Toxicol 92:3255–3275
McCoy F, Hurwitz J, McTavish N, Paul I, Barnes C, O'Hagan B, Odrzywol K, Murray J, Longley D, McKerr G (2010) Obatoclax induces Atg7-dependent autophagy independent of beclin-1 and BAX/BAK. Cell Death Dis 1:e108–e108
Mohamed EA, Ahmed HI, Zaky HS (2018) Protective effect of irbesartan against doxorubicin-induced nephrotoxicity in rats: implication of AMPK, PI3K/Akt, and mTOR signaling pathways. Can J Physiol Pharmacol 96:1209–1217
Oliveira NG, Pingarilho M, Martins C, Fernandes AS, Vaz S, Martins V, Rueff J, Gaspar JF (2009) Cytotoxicity and chromosomal aberrations induced by acrylamide in V79 cells: role of glutathione modulators. Mutat Res 676:87–92
Özdemir S, Kucukler S, Çomaklı S, Kandemir FM (2020) The protective effect of Morin against ifosfamide-induced acute liver injury in rats associated with the inhibition of DNA damage and apoptosis. Drug and Chemical Toxicology 1-10
Pan X, Wu X, Yan D, Peng C, Rao C, Yan H (2018) Acrylamide-induced oxidative stress and inflammatory response are alleviated by N-acetylcysteine in PC12 cells: Involvement of the crosstalk between Nrf2 and NF-kappaB pathways regulated by MAPKs. Toxicol Lett 288:55–64
Placer ZA, Cushman LL, Johnson BC (1966) Estimation of product of lipid peroxidation (malonyl dialdehyde) in biochemical systems. Anal Biochem 16:359–364
Prasad SN (2012) Evidence of acrylamide induced oxidative stress and neurotoxicity in Drosophila melanogaster–its amelioration with spice active enrichment: Relevance to neuropathy. Neurotoxicology 33:1254–1264
Sang L, Wang X-M, Xu D-Y, Sang L-X, Han Y, Jiang L-Y (2017) Morin enhances hepatic Nrf2 expression in a liver fibrosis rat model. World J Gastroenterol 23:8334–8344
Santhanasabapathy R, Vasudevan S, Anupriya K, Pabitha R, Sudhandiran G (2015) Farnesol quells oxidative stress, reactive gliosis and inflammation during acrylamide-induced neurotoxicity: behavioral and biochemical evidence. Neuroscience 308:212–227
Sedlak J, Lindsay RH (1968) Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman’s reagent. Anal Biochem 25:192–205
Sun Y, Oberley LW, Li Y (1988) A simple method for clinical assay of superoxide dismutase. Clin Chem 34:497–500
Sun G, Wang X, Li T, Qu S, Sun J (2018) Taurine attenuates acrylamide-induced apoptosis via a PI3K/AKT-dependent manner. Hum Exp Toxicol 37:1249–1257
Syed F, Awasthi KK, Chandravanshi LP, Verma R, Rajawat NK, Khanna VK, John P, Soni I (2018) Bifenthrin-induced neurotoxicity in rats: involvement of oxidative stress. Toxicology Research 7:48–58
Tabeshpour J, Mehri S, Abnous K, Hosseinzadeh H (2019) Neuroprotective effects of thymoquinone in acrylamide-induced peripheral nervous system toxicity through MAPKinase and apoptosis pathways in rat. Neurochem Res 44:1101–1112
Tabeshpour J, Mehri S, Abnous K, Hosseinzadeh H (2020) Role of oxidative stress, MAPKinase and apoptosis pathways in the protective effects of thymoquinone against acrylamide-induced central nervous system toxicity in rat. Neurochem Res 45:254–267
Tao L, Li D, Liu H, Jiang F, Xu Y, Cao Y, Gao R, Chen G (2018) Neuroprotective effects of metformin on traumatic brain injury in rats associated with NF-κB and MAPK signaling pathway. Brain Res Bull 140:154–161
Temel Y, Çağlayan C, Ahmed BM, Kandemir FM, Çiftci M (2020) The effects of chrysin and naringin on cyclophosphamide-induced erythrocyte damage in rats: biochemical evaluation of some enzyme activities in vivo and in vitro. Naunyn-Schmiedeberg’s Archives of Pharmacology 1-10
Thangarajan S, Vedagiri A, Somasundaram S, Sakthimanogaran R, Murugesan M (2018) Neuroprotective effect of morin on lead acetate-induced apoptosis by preventing cytochrome c translocation via regulation of Bax/Bcl-2 ratio. Neurotoxicol Teratol 66:35–45
Tian SM, Ma YX, Shi J, TY L, SS L, GY L (2015) Acrylamide neurotoxicity on the cerebrum of weaning rats. Neural Regen Res 10:938
Uddin M, Hasana S, Ahmad J, Hossain M, Rahman M, Behl T, Rauf A, Ahmad A, Hafeez A, Perveen A (2020a) Anti-Neuroinflammatory Potential of Polyphenols by Inhibiting NF-κB to Halt Alzheimer’s Disease. Curr Pharm Des
Uddin M, Kabir M, Niaz K, Jeandet P, Clément C, Mathew B, Rauf A, Rengasamy KR, Sobarzo-Sánchez E, Ashraf GM (2020b) Molecular insight into the therapeutic promise of flavonoids against Alzheimer’s disease. Molecules 25:1267
Uddin MS, Kabir MT, Tewari D, Mathew B, Aleya L (2020c) Emerging signal regulating potential of small molecule biflavonoids to combat neuropathological insults of Alzheimer’s disease. Sci Total Environ 700:134836
Uthra C, Shrivastava S, Jaswal A, Sinha N, Reshi MS, Shukla S (2017) Therapeutic potential of quercetin against acrylamide induced toxicity in rats. Biomed Pharmacother 86:705–714
Vucicevic L, Misirkic M, Janjetovic K, Vilimanovich U, Sudar E, Isenovic E, Prica M, Harhaji-Trajkovic L, Kravic-Stevovic T, Bumbasirevic V, Trajkovic V (2011) Compound C induces protective autophagy in cancer cells through AMPK inhibition-independent blockade of Akt/mTOR pathway. Autophagy 7:40–50
Xu L, Shen J, Yu L, Sun J, McQuillan PM, Hu Z, Yan M (2018) Role of autophagy in sevoflurane-induced neurotoxicity in neonatal rat hippocampal cells. Brain Res Bull 140:291–298
Yakovleva T, Bazov I, Watanabe H, Hauser KF, Bakalkin G (2011) Transcriptional control of maladaptive and protective responses in alcoholics: a role of the NF-κB system. Brain Behav Immun 25:S29–S38
Yan D, Pan X, Yao J, Wang D, Wu X, Chen X, Shi N, Yan H (2019) MAPKs and NF-κB-mediated acrylamide-induced neuropathy in rat striatum and human neuroblastoma cells SY5Y. J Cell Biochem 120:3898–3910
Yang D, Tan X, Lv Z, Liu B, Baiyun R, Lu J, Zhang Z (2016) Regulation of Sirt1/Nrf2/TNF-α signaling pathway by luteolin is critical to attenuate acute mercuric chloride exposure induced hepatotoxicity. Sci Rep 6:37157
Yang B, Bai Y, Yin C, Qian H, Xing G, Wang S, Li F, Bian J, Aschner M, Lu R (2018) Activation of autophagic flux and the Nrf2/ARE signaling pathway by hydrogen sulfide protects against acrylonitrile-induced neurotoxicity in primary rat astrocytes. Arch Toxicol 92:2093–2108
Yardim A, Kandemir FM, Ozdemir S, Kucukler S, Comakli S, Gur C, Celik H (2020) Quercetin provides protection against the peripheral nerve damage caused by vincristine in rats by suppressing caspase 3, NF-κB, ATF-6 pathways and activating Nrf2, Akt pathways. Neurotoxicology
Yardım A, Kandemir FM, Çomaklı S, Özdemir S, Caglayan C, Kucukler S, Çelik H (2020a) Protective effects of curcumin against paclitaxel-induced spinal cord and sciatic nerve injuries in rats. Neurochemical Research 1-17
Yardım A, Kucukler S, Özdemir S, Çomaklı S, Caglayan C, Kandemir FM, Çelik H (2020b) Silymarin alleviates docetaxel-induced central and peripheral neurotoxicity by reducing oxidative stress, inflammation and apoptosis in rats. Gene 145239
Yeung AWK, Tzvetkov NT, El-Tawil OS, Bungǎu SG, Abdel-Daim MM, Atanasov AG (2019) Antioxidants: scientific literature landscape analysis. Oxidative Med Cell Longev 2019:1–11
Youn K, Lee S, Jun M (2018) Gamma-linolenic acid ameliorates Aβ-induced neuroinflammation through NF-κB and MAPK signalling pathways. J Funct Foods 42:30–37
Yuntao F, Chenjia G, Panpan Z, Wenjun Z, Suhua W, Guangwei X, Haifeng S, Jian L, Wanxin P, Yun F (2016) Role of autophagy in methylmercury-induced neurotoxicity in rat primary astrocytes. Arch Toxicol 90:333–345
Zhang ZT, XB C, Xiong N, Wang HC, JS H, SG S, Wang T (2010) Morin exerts neuroprotective actions in Parkinson disease models in vitro and in vivo. Acta Pharmacol Sin 31:900–906
Zhao M, Wang P, Zhu Y, Liu X, Hu X, Chen F (2015) Blueberry anthocyanins extract inhibits acrylamide-induced diverse toxicity in mice by preventing oxidative stress and cytochrome P450 2E1 activation. J Funct Foods 14:95–101
Zhao M, Wang FSL, Hu X, Chen F, Chan HM (2017) Acrylamide-induced neurotoxicity in primary astrocytes and microglia: roles of the Nrf2-ARE and NF-κB pathways. Food Chem Toxicol 106:25–35
Author information
Authors and Affiliations
Contributions
CG: Writing – original draft, writing – review and editing, methodology, and formal analysisFMK: Writing – original draft, writing – review and editing, methodology, project administration, formal analysis, and conceptualizationED: Methodology and investigationCC: Methodology and investigationSK: Methodology and data curationOK: Investigation and data curationMI: Methodology and Investigation
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics committee approval required to conduct the study was obtained from the Local Ethics Council of Animal Experiments (Approval no: 2017-13/161).
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Mohamed M. Abdel-Daim
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gur, C., Kandemir, F.M., Darendelioglu, E. et al. Morin protects against acrylamide-induced neurotoxicity in rats: an investigation into different signal pathways. Environ Sci Pollut Res 28, 49808–49819 (2021). https://doi.org/10.1007/s11356-021-14049-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-14049-4