Abstract
Little is known on the potential impact of temperature on respiratory morbidity, especially for children whose respiratory system can be more vulnerable to climate changes. In this time-series study, Poisson generalized additive models combined with distributed lag nonlinear models were used to assess the associations between ambient temperature and childhood respiratory morbidity. The impacts of extreme cold and hot temperatures were calculated as cumulative relative risks (cum.RRs) at the 1st and 99th temperature percentiles relative to the minimum morbidity temperature percentile. Attributable fractions of respiratory morbidity due to cold or heat were calculated for temperatures below or above the minimum morbidity temperature. Effect modifications by air pollution, age, and sex were assessed in stratified analyses. A total of 877,793 respiratory hospital visits of children under 14 years old between 2013 and 2017 were collected from Beijing Children’s Hospital. Overall, we observed J-shaped associations with greater respiratory morbidity risks for exposure to lower temperatures, and higher fraction of all-cause respiratory hospital visits was caused by cold (33.1%) than by heat (0.9%). Relative to the minimum morbidity temperature (25 °C, except for rhinitis, which is 31 °C), the cum.RRs for extreme cold temperature (-6 °C) were 2.64 (95%CI: 1.51–4.61) for all-cause respiratory hospital visits, 2.73 (95%CI: 1.44–5.18) for upper respiratory infection, 2.76 (95%CI: 1.56–4.89) for bronchitis, 2.12 (95%CI: 1.30–3.47) for pneumonia, 2.06 (95%CI: 1.27–3.34) for rhinitis, and 4.02 (95%CI: 2.14–7.55) for asthma, whereas the associations between extreme hot temperature (29 °C) and respiratory hospital visits were not significant. The impacts of extreme cold temperature on asthma hospital visits were greater at higher levels of ozone (O3) exposure (> 50th percentile). Our findings suggest significantly increased childhood respiratory morbidity risks at extreme cold temperature, and the impact of extreme cold temperature on asthma hospital visits can be enhanced under higher level exposure to O3.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Climate change has become a global public health challenge with increasing concern on the adverse health effects, including respiratory diseases (Patz et al. 2014). Several studies have also used the attributable fraction (AF), defined as the fraction of cases that would not have occurred in the absence of a specific risk factor in the exposed population, to assess the disease burden (Li et al. 2020; Wang et al. 2020). In China, the AF due to non-optimum temperature was 10.57% for respiratory mortality in recent years (Chen et al. 2018b). The optimum temperatures that correspond to minimum morbidity refer to the minimum morbidity temperature and the temperatures higher or lower than “optimum temperature” can be an airway stimulus to the airway to induce bronchoconstriction (Chen et al. 2018b; Deng et al. 2020).
For respiratory diseases, both extreme cold and hot temperatures can likely activate transient receptor potential proteins (TRPs) in upper and lower respiratory tract and cause airway inflammation and hyper-responsiveness (Deng et al. 2020). Population studies have reported J- or U-shaped relationships between daily mean temperature and respiratory mortality, with increasing mortality risks from minimum mortality temperature to lowest and highest temperatures (Ma et al. 2014; Xu et al. 2012). Studies also reported that the impacts of extreme cold temperature were stronger than those of extreme hot temperature, because general population tend to be more adapted to warm weather than cold weather even under the context of global warming (Lam et al. 2016; Li et al. 2020). Compared with adults and the elderly, children and adolescents appeared to be more susceptible to temperature changes (Ma et al. 2019; Chai et al. 2020), who might be more vulnerable respiratory and immune systems under development (Strosnider et al. 2019). However, epidemiological study on respiratory morbidity among children has been limited and warrants more research.
Little is known about whether air pollution can modify the respiratory effects of ambient temperature to some extents. Several studies have assessed the impact of environmental risk factors on respiratory morbidity, such as ambient temperature and air pollutants (Karakatsani et al. 2017; Lam et al. 2016; Li et al. 2015; Sun et al. 2018). Few studies of mortality have found that ozone (O3) significantly modified the impacts of temperature on total and cardiovascular mortality, but the modification effect on respiratory health has been barely investigated (Breitner et al. 2014; Chen et al. 2018a).
In this study, we aimed to examine the associations between ambient temperature and respiratory hospital visits for all-cause, URI, bronchitis, pneumonia, rhinitis, and asthma in children under 14 years old in Beijing, China, as well as to quantify the burdens of corresponding respiratory disease burden attributable to both cold and heat. We also explored the potential effect modifications by air pollution and other risk factors, such as age and sex, on ambient temperature and children respiratory morbidity.
Methods
Participants
We collected daily data on hospital utilization, including outpatient visits and emergency room visits (ERVs), for respiratory diseases between October 2013 and November 2017 from Beijing Children`s Hospital. Outpatient data was unscheduled and first-come first-served in China; thus, the analytical database by including both outpatient visits and ERVs was likely to provide reliable morbidity information for a geographically defined population in our study (Tian et al. 2017; Xu et al. 1995). The database also included information on the date of hospital visits, identification number, sex, age, residential address, and discharge diagnoses with corresponding International Classification of Diseases codes (the 10th Revision, ICD-10). Participants with residential addresses outside metropolitan Beijing area were excluded. The outcomes included hospital visits on all-cause respiratory diseases (J00–J99), upper respiratory infection (URI) (J00–J06), bronchitis (J21), pneumonia (J12–J18, J69), rhinitis (J31), and asthma (J45–46). Participants were classified into three age groups, including those younger than 2 years old (infants), between 2 and 5 years old (preschool children), and between 6 and 14 years old (school-age children) (Lee et al. 2019). This study was approved by the Institutional Review Board of Beijing Children’s Hospital, Capital Medical University (IEC-C-028-A10-V.05). The influenza weekly of reports from October 2013 to November 2017 were obtained from the Chinese National Influenza Center (http://www.chinaivdc.cn/); we assigned 1 to influenza epidemics when reports wrote that influenza activities were at intra-seasonal levels in northern China, or 0 otherwise.
Environmental data
Daily 24-h ambient temperature and relative humidity (RH) from October 2013 to November 2017 were obtained from the Chinese Meteorological Bureau (http://data.cma.cn/). Concurrently, hourly particulate matter with aerodynamic diameter less than 2.5 μm (PM2.5), nitrogen dioxide (NO2), sulfur dioxide (SO2), and O3 measurements were obtained from the Beijing Environmental Protection Bureau (http://beijingair.sinaapp.com/). We computed 24-h averages for PM2.5, NO2, and SO2 and calculated the 8-h daily maximum from 8-h running averages for ozone (O3-8h max) (Wu et al. 2018).
Statistical analysis
Ambient temperature and air pollution data were processed following procedures described earlier (Wu et al. 2019). We then applied Poisson generalized additive models (GAMs) and distributed lag nonlinear models (DLNMs) to provide flexibility for modelling the potentially nonlinear and lagged association between ambient temperature and childhood respiratory hospital visits, with adjustment for influenza epidemic, RH, time trend, public holidays, and day of the week (DOW) (Wu et al. 2018).
First, we built basic models without including ambient temperature and air pollutant variables. A smooth function for time trend with 7 degrees of freedom (DF) per year was chosen to control for seasonality and long-term trends according to previous studies (Lam et al. 2016). We included a smooth function for RH on the same day of hospital visits (lag day 0) with the 6 DF determined by minimizing Akaike’s information criterion (AIC) (Rich et al. 2012). Public holidays and DOW were classified as categorical variables. After defining the basic models, we introduced the cross basis function of daily temperature built by the DLNM, which included a cubic B-spline to model the nonlinear temperature effects and a natural cubic spline with 4 DF to examine the lagged effects (Breitner et al. 2014; Lam et al. 2016). A maximum lag of 14 days was used to model the effects of temperature, because the effects of high temperature were usually within 1–3 days and the effects of low temperatures could last about 2–3 weeks (Chen et al. 2018b). The minimum morbidity temperature, which was defined as the temperature that had minimum impact on morbidity risk, was derived from the lowest point of overall cumulative exposure-response curve between temperature and respiratory morbidity (Li et al. 2020; Tobías et al. 2017; Zhao et al. 2019). We then used minimum morbidity temperature as the reference value to calculate the relative risks (RRs) and calculated the impacts of extreme cold and hot temperatures as cumulative morbidity risks at the 1st and 99th percentile relative to the minimum morbidity temperature percentile. The minimum morbidity temperature was also used as the reference for calculating the AFs during the present day and 7 lagged days. For all-cause and cause-specific respiratory hospital visits, we calculated 95% empirical CIs (95% eCIs) of AFs associated with cold or heat by summing the subsets of days with temperatures below or above than the minimum morbidity temperature (Chen et al. 2018b; Gasparrini and Leone 2014; Wang et al. 2020).
We further introduced air pollutant variables (PM2.5, NO2, SO2, and O3) separately into the models and used single- and multiple-day lags to estimate the associations between air pollution and respiratory hospital visits in both single- and two-pollutant models. The multiple-day exposure lags were calculated as the average levels of current day and several prior days (e.g., lag days 0–3) (Wu et al. 2018). To examine potential effect modifications by air pollution, we divided the levels of air pollutants into two categories: high (> median value) and low (≤ median value). We further introduced the interaction terms between temperature and categorized air pollutants into the main models (Chen et al. 2018a). The statistical significance of difference in effect estimates across strata of air pollutants was tested by Z-test (Xu et al. 2019). Subgroup analyses by age and sex were also performed to identify the most susceptible subpopulation.
Finally, sensitivity analyses were conducted to examine the robustness of associations for extreme temperatures on all-cause and cause-specific respiratory hospital visits reported in main models by (1) applying alternative DF (6–10 per year) for time trend in the models (Ma et al. 2019) and (2) adjusting for the impacts of PM2.5, NO2, SO2, and O3. All models were implemented using R version 3.5.3, and a two-sided P < 0.05 was considered statistically significant. The effect estimates were presented as RRs and 95% confidence interval (95%CIs).
Results
Data characterization
A total of 877,793 respiratory hospital visits over 1521 days of study period were included in this analysis, including 678,934 outpatient visits and 198,859 ERVs (Table 1). The major causes were URI, bronchitis, pneumonia, rhinitis, and asthma, accounted for 383,459 (43.7%), 189,180 (21.6%), 173,036 (19.7%), 60,670 (6.9%), and 22,169 (2.5%) of total hospital visits, respectively. A mean daily number of respiratory hospital visits were 577, 151, 306, and 120 for all age combined, infants, preschool children, and school-age children, 336 for male and 241 for female children, respectively. The average temperature and RH during study period were 12.6 °C and 54.0%, ranging from -15.5 to 31.2 °C and from 9.6 to 95.3%, respectively (Table 2). The mean temperatures were -1.5 °C, 15.0 °C, 25.4 °C, and 11.6 °C for winter, spring, summer, and fall, respectively. Average daily concentrations were 75.5 μg/m3 for PM2.5, 45.7 μg/m3 for NO2, 11.2 μg/m3 for SO2, and 101.4 μg/m3 for O3, and the interquartile range (IQR) of PM2.5, NO2, SO2, and O3 were 69.3, 25.2, 10.6, and 88.6 μg/m3, respectively. Figure S1 presents the variations in annual averages of daily levels for temperature and RH, and daily concentrations for PM2.5, NO2, SO2 and O3 with decreasing trend of PM2.5, NO2, and SO2 levels over time. Table S1 shows the Spearman correlation coefficients for the environmental variables, with positive correlations observed between temperature and O3 concentrations (r = 0.82, P < 0.05) and inversely weak correlations between temperature and PM2.5 (r = -0.10, P < 0.05). NO2 and SO2 were negatively correlated with temperature (r = -0.34 and -0.54, respectively).
Ambient temperature and respiratory morbidity
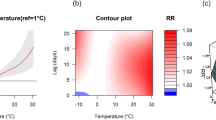
Figure S2 showed that the RRs of extreme cold temperature (25 °C) were the strongest on the present day, attenuated drastically to lag day 7, and followed by a significant morbidity displacement (i.e., RRs below 1) on the subsequent days for all-cause respiratory hospital visits. Figure 1 illustrated the cumulative exposure-response curves for the associations between temperature and all-cause and cause-specific respiratory hospital visits (including URI, bronchitis, pneumonia, rhinitis, and asthma) prior to 0–7 days. For all-cause, URI, bronchitis, pneumonia, and asthma hospital visits, the curves were consistently inversely J-shaped, and the cum.RRs increased sharply when the mean temperature decreased from 25 °C to about 6 °C, and then plateaued for a temperature lower than 6 °C. The cum.RRs for temperature higher than 25 °C suggested that the associations were not significant in this temperature range, possibly because of the small number of days with mean temperature higher than 25 °C during the study period (Fig. S3). For rhinitis hospital visits, the cum.RRs increased sharply when the mean temperature decreased from 31 °C to about 10 °C, and then plateaued for a temperature lower than 10 °C.
Cumulative exposure-response curves for associations between temperature and all-cause and major cause-specific childhood respiratory hospital visits prior 0–7 days in Beijing, 2013-2017. Cumulative exposure-response relationships between temperature and all-cause and major cause-specific childhood respiratory hospital visits, including URI, bronchitis, pneumonia, rhinitis, and asthma. The effect estimate is shown by the dotted line, and the red areas represent the 95% confidence intervals. URI upper respiratory infection
Table 3 summarized cumulative associations between temperature and daily respiratory hospital visits prior to 0–7 days. The minimum morbidity temperatures were all 25 °C (except for rhinitis, which was 31 °C), corresponding to the 80th centile of temperature distribution. For all-cause respiratory hospital visits, the cum.RR for extreme cold temperature was 2.64 (95%CI: 1.51–4.61) and for extreme hot temperature was 1.13 (95%CI: 0.92–1.38). The results were similar for outpatient visits and ERVs. We only calculated the cum.RR for extreme cold temperature on rhinitis hospital visits, because the minimum morbidity temperature (31 °C) was larger than the 99th percentile of temperature (29 °C). Exposure to extreme cold temperature was also associated with increased risk of URI (2.73; 95%CI: 1.44–5.18), bronchitis (2.76; 95%CI: 1.56–4.89), pneumonia (2.12; 95%CI: 1.30–3.47), rhinitis (2.06; 95%CI: 1.27–3.34), and asthma (4.02; 95%CI: 2.14–7.55). However, the cum.RRs for extreme hot temperature were not significant. For all-cause respiratory hospital visits, the cum.RRs for extreme cold temperature varied in magnitude by age and sex groups. The cum.RRs of extreme cold temperature were highest in infants (4.52; 95%CI: 2.54–8.03) and in male children (3.15; 95%CI: 1.75–5.64), but the differences in effect estimates examined by using Z-test were not significant (P > 0.05). Table S3 shows the cum.RRs for respiratory morbidity in association with daily mean temperature exposure at different percentiles during lag days 0–7.
Table 3 also illustrated the AFs of all-cause and cause-specific respiratory visits associated with different components of non-optimum temperatures. The overall AFs of non-optimum temperatures were 33.1% for all-cause respiratory hospital visits, 26.2% for URI, 36.5% for bronchitis, 23.1% for pneumonia, 44.0% for rhinitis, and 39.7% for asthma. Cold was responsible for most of the burden, due to the right shifted minimum morbidity temperature in the temperature distribution leading to more cold days and higher effects at lower temperatures. In addition, the cold-related burdens in subgroups of infants and male children were also higher than in other groups.
Air pollution and respiratory morbidity
We observed statistically significant positive associations between O3 and respiratory hospital visits (Table 4). The RRs per IQR increase in O3 (lag day 1) for all-cause, URI, bronchitis, pneumonia, and asthma hospital visits in single-pollutant models were 1.10 (95%CI: 1.06–1.15), 1.13 (95%CI: 1.08–1.19), 1.10 (95%CI: 1.05–1.15), 1.09 (95%CI: 1.05–1.13), and 1.05 (95%CI: 1.00–1.11), respectively, and the RRs remained positive and significant after adjusting for PM2.5, NO2, and SO2 in two-pollutant models. The association between O3 and rhinitis hospital visits in single-pollutant model was not significant, but became significant after adjusting for NO2. However, no significant and consistent associations were observed for PM2.5, NO2, and SO2 (Table S3).
Modification effects and sensitivity analyses
Table 5 reported the cum.RRs of all-cause and cause-specific respiratory hospital visits in associations with extreme cold temperature stratified by O3 levels. For rhinitis hospital visits, the cum.RRs for extreme cold temperature were 0.99 (95%CI: 0.68–1.44) at low O3 level and 1.92 (95%CI: 1.32–2.78) at high O3 level, with significant difference between low and high O3 levels. For asthma hospital visits, the cum.RRs for extreme cold temperature were 2.50 (95%CI: 1.38–4.53) at low O3 level and 15.89 (95%CI: 8.77–28.80) at high O3 level, with significant difference between low and high O3 levels. However, for all-cause, URI, bronchitis, and pneumonia hospital visits, the cum.RRs for extreme cold temperature were generally stronger at high O3 level than at low O3 level without significant difference between low and high O3 levels.
In the sensitivity analyses, for all-cause respiratory hospital visits, the models with alternative DF (6–10 per year) for time trend were comparable to the base model (Fig. S4). For all-cause and cause-specific respiratory hospital visits, the cum.RRs for extreme cold temperature were slightly attenuated but did not change substantially after adjusting for PM2.5, but moderately increased after adjusting for NO2, SO2, or O3 (Table S4).
Discussion
This study took advantage of a comparatively large sample of database to assess environmental factor associated respiratory morbidity in children under 14 years old in Beijing, China, and found inversely J-shaped associations between temperature exposure and all-cause and cause-specific respiratory hospital visits. The fraction of all-cause respiratory hospital visits caused by cold was 33.1%, and by heat was 0.9%. The cum.RRs for extreme cold temperature were 2.73 (95%CI: 1.44–5.18), 2.76 (95%CI: 1.56–4.89), 2.12 (95%CI: 1.30–3.47), 2.06 (95%CI: 1.27–3.34), and 4.02 (95%CI: 2.14–7.55) for URI, bronchitis, pneumonia, rhinitis, and asthma. We also observed significant positive association between O3 exposure and all-cause and cause-specific respiratory hospital visits. The cum.RRs for extreme cold temperature on all-cause and cause-specific respiratory hospital visits were generally stronger at high O3 level than at low O3 level. Our results supported continuing efforts to mitigate air pollution exposure under the context of climate change.
In the context of global climate change, extreme weather events become more frequent and intense, and prior studies have found that both extreme cold and hot temperatures were associated with increased respiratory morbidity (Chai et al. 2020; Gasparrini et al. 2015; Lam et al. 2016; Ma et al. 2019; Qiu et al. 2016; Scovronick et al. 2018; Zhang et al. 2020a). In the present analysis, we found inversely J-shaped associations between ambient temperature and respiratory morbidity, and most of the respiratory disease burden was attributable to the coldness (35.7%). A multicity time-series study conducted in Jiangsu Province, China, reported that cold was responsible for 18.10% of respiratory mortality, larger than the fraction attributable to heat (4.93%) (Ma et al. 2020). Human experiments in environmental chambers found that when exercising in conditions of coldness, the subjects with asthma had significant decreases in forced expiratory volume in 1 s (FEV1) (20–21%) and increases in specific airway resistance (SRaw) (72–96%) (Eschenbacher et al. 1992). Xing et al. found that inhalation of cold air may cause autonomic respiratory responses such as airway constriction and mucosal secretion through the autonomic nerve reflex (Xing et al. 2008).
The minimum morbidity temperatures for the associations between temperature and childhood respiratory hospital visits for all-cause, URI, bronchitis, pneumonia, and asthma were all 25 °C. Song et al. reported that the minimum morbidity temperature was 21.5 °C for respiratory ERVs and the cum.RR for extreme cold temperature (12 °C vs 25 °C) was 1.81 (95%CI: 1.26–2.76) (Song et al. 2018). Lam et al. reported that the minimum morbidity temperature was 25 °C for asthma hospitalizations during the cold season and the cum.RR for extreme cold temperature was 1.33 (95%CI: 1.13–1.58) (Lam et al. 2016). The minimum morbidity temperature and cold relative RRs for rhinitis were higher than those for other respiratory diseases, which can be partly explained by the fact that the nose serves as the portal of entry to the respiratory tract and is more vulnerable to ambient temperature (Shusterman 2016). The cum.RRs for all-cause and cause-specific respiratory hospital visits plateaued and even slightly decreased for a temperature lower than 10 °C, which might be explained by a longer duration of central heating in Beijing in winter and increased adaptive capability against cold exposure (Chen et al. 2018b; Ma et al. 2019). In addition, we observed stronger associations between extreme cold temperature and all-cause respiratory morbidity in infants (< 2 years old) and in male children, although the differences examined by using Z-test were not significant. Compared with older children (2–14 years old), infants have a more undeveloped respiratory system which make them suffer more from extreme cold temperature (Xu et al. 2012). Sex differences might be dependent on breathing patterns and immunologic responses, and Muenchhoff et al. observed stronger Th1 immune responses in females and higher susceptibility in males for many pathogens (Muenchhoff and Goulder 2014).
Among pollutants, we observed the significant positive associations between O3 and all-cause, URI, bronchitis, pneumonia, and asthma respiratory hospital visits, and the associations remained significantly positive after adjusting for PM2.5, NO2, and SO2. Previous studies have also reported that exposure to O3 was positively associated with URI, pneumonia, and asthma morbidity (Lam et al. 2016; Strosnider et al. 2019). O3 is a reactive gaseous pollutants and powerful oxidant and can react with proteins or lipids in the lung surface. The secondary oxidation products can induce respiratory tract inflammation and epithelial cell injury, which results in a range of respiratory symptoms (Zu et al. 2018). Karakatsani et al. conducted a panel study among school-age children and showed that an increase of 10 μg/m3 in weekly O3 concentration was associated with a 11.10% (95%CI: 4.23–18.43%) increase in the fractional concentration of nitric oxide in exhaled air (FeNO), a marker of airway inflammation (Karakatsani et al. 2017). However, we found that the association between O3 and rhinitis respiratory hospital visits was not consistent, which has been barely investigated and needs further investigation. In addition, we did not find evidence of significant positive associations between PM2.5 and respiratory morbidity as reported in other studies (Lam et al. 2016; Peel et al. 2005; Strosnider et al. 2019; Szyszkowicz et al. 2018; Zhang et al. 2020b), which was likely due to the extensive use of personal-level protection device outdoors during high pollution episodes (Langrish et al. 2009; Shi et al. 2017).
Only a few studies have investigated the effect modification by O3 on ambient temperature-mortality relationships (Breitner et al.2014; Burkart et al. 2013; Chen et al.2018a). Chen et al. reported that the impacts of both extreme cold and hot temperatures on total and cardiovascular mortality were stronger at high O3 level (Chen et al.2018a). Breitner et al. reported that the impact of extreme hot temperatures on non-accidental and cardiovascular mortality were stronger at high O3 level (Breitner et al.2014). However, the effect modification by O3 on ambient temperature and respiratory health has been barely investigated. In this analysis, we observed significantly impacts at extreme cold temperature on childhood respiratory hospital visits for rhinitis and asthma on days with higher O3 level. Cheng et al. also reported significant interaction between O3 and extreme low temperature for respiratory mortality in Shanghai, China (Cheng and Kan 2012). The underlying mechanisms for the observed temperature effect modification by O3 level were still unclear, but exposure to O3 can increase the stimulus to the hyperreactive airway and aggravate airway inflammation in people with asthma, which may lead to a higher susceptibility to temperature changes (Chen et al. 2018a; Lam et al. 2016). However, we should note several study limitations. Firstly, the use of ambient monitoring measurements might not well represent population environmental exposure levels. We did not consider the amount of time spent indoors and outdoors, as well as the use of air conditioning and heating, which tend to bias the effect estimates towards null. Secondly, though we observed increased RRs of respiratory morbidity at higher temperature, the number of days with daily mean temperature higher than 25 °C was small during the study period, which limited our ability to examine the potential impact of extreme hot temperature on respiratory hospital visits. Further studies are needed to investigate the effect modification of ambient temperature and O3 on respiratory health in hotter areas.
Conclusion
Our study found nonlinear associations between ambient temperature and respiratory morbidity among children, as well as the corresponding disease burden that is mainly attributable to cold in Beijing, China. The impacts of extreme cold temperature on asthma morbidity can be significantly modified by O3. Our findings support reducing air pollution concentrations to further reduce the health burdens attributable to ambient temperature under the context of climate change.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Breitner S, Wolf K, Devlin RB, Diaz-Sanchez D, Peters A, Schneider A (2014) Short-term effects of air temperature on mortality and effect modification by air pollution in three cities of Bavaria, Germany: a time-series analysis. Sci Total Environ 485-486:49–61. https://doi.org/10.1016/j.scitotenv.2014.03.048
Burkart K, Canário P, Breitner S, Schneider A, Scherber K, Andrade H, Alcoforado MJ, Endlicher W (2013) Interactive short-term effects of equivalent temperature and air pollution on human mortality in Berlin and Lisbon. Environ Pollut 183:54–63. https://doi.org/10.1016/j.envpol.2013.06.002
Chai G, He H, Su Y, Sha Y, Zong S (2020) Lag effect of air temperature on the incidence of respiratory diseases in Lanzhou. China Int J Biometeorol 64:83–93. https://doi.org/10.1007/s00484-019-01795-x
Chen K, Wolf K, Breitner S, Gasparrini A, Stafoggia M, Samoli E, Andersen ZJ, Bero-Bedada G, Bellander T, Hennig F, Jacquemin B, Pekkanen J, Hampel R, Cyrys J, Peters A, Schneider A, UF&HEALTH Study Group (2018a) Two-way effect modifications of air pollution and air temperature on total natural and cardiovascular mortality in eight European urban areas. Environ Int 116:186–196. https://doi.org/10.1016/j.envint.2018.04.021
Chen R, Yin P, Wang L, Liu C, Niu Y, Wang W, Jiang Y, Liu Y, Liu J, Qi J, You J, Kan H, Zhou M (2018b) Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. Bmj 363:k4306. https://doi.org/10.1136/bmj.k4306
Cheng Y, Kan H (2012) Effect of the interaction between outdoor air pollution and extreme temperature on daily mortality in Shanghai. China J Epidemiol 22:28–36. https://doi.org/10.2188/jea.je20110049
Deng L, Ma P, Wu Y, Ma Y, Yang X, Li Y, Deng Q (2020) High and low temperatures aggravate airway inflammation of asthma: evidence in a mouse model. Environ Pollut 256:113433. https://doi.org/10.1016/j.envpol.2019.113433
Eschenbacher WL, Moore TB, Lorenzen TJ, Weg JG, Gross KB (1992) Pulmonary responses of asthmatic and normal subjects to different temperature and humidity conditions in an environmental chamber. Lung 170:51–62. https://doi.org/10.1007/bf00164755
Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, Tobias A, Tong S, Rocklöv J, Forsberg B, Leone M, de Sario M, Bell ML, Guo YLL, Wu CF, Kan H, Yi SM, de Sousa Zanotti Stagliorio Coelho M, Saldiva PHN, Honda Y, Kim H, Armstrong B (2015) Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386:369–375. https://doi.org/10.1016/s0140-6736(14)62114-0
Gasparrini A, Leone M (2014) Attributable risk from distributed lag models. BMC Med Res Methodol 14:55. https://doi.org/10.1186/1471-2288-14-55
Karakatsani A, Samoli E, Rodopoulou S, Dimakopoulou K, Papakosta D, Spyratos D, Grivas G, Tasi S, Angelis N, Thirios A, Tsiotsios A, Katsouyanni K (2017) Weekly personal ozone exposure and respiratory health in a panel of Greek schoolchildren. Environ Health Perspect 125:077016. https://doi.org/10.1289/EHP635
Lam HC, Li AM, Chan EY, Goggins WB 3rd (2016) The short-term association between asthma hospitalisations, ambient temperature, other meteorological factors and air pollutants in Hong Kong: a time-series study. Thorax 71:1097–1109. https://doi.org/10.1136/thoraxjnl-2015-208054
Langrish JP, Mills NL, Chan JKK, Leseman DLAC, Aitken RJ, Fokkens PHB, Cassee FR, Li J, Donaldson K, Newby DE, Jiang L (2009) Beneficial cardiovascular effects of reducing exposure to particulate air pollution with a simple facemask. Part Fibre Toxicol 6:8. https://doi.org/10.1186/1743-8977-6-8
Lee SW et al (2019) Short-term effects of multiple outdoor environmental factors on risk of asthma exacerbations: age-stratified time-series analysis. J Allergy Clin Immunol 144:1542–1550.e1541. https://doi.org/10.1016/j.jaci.2019.08.037
Li L, Yang J, Guo C, Chen PY, Ou CQ, Guo Y (2015) Particulate matter modifies the magnitude and time course of the non-linear temperature-mortality association. Environ Pollut 196:423–430. https://doi.org/10.1016/j.envpol.2014.11.005
Li H, Yao Y, Duan Y, Liao Y, Yan S, Liu X, Zhao Z, Fu Y, Yin P, Cheng J, Jiang H (2020) Years of life lost and mortality risk attributable to non-optimum temperature in Shenzhen: a time-series study. J Expo Sci Environ Epidemiol. 31:187–196. https://doi.org/10.1038/s41370-020-0202-x
Ma W, Chen R, Kan H (2014) Temperature-related mortality in 17 large Chinese cities: how heat and cold affect mortality in China. Environ Res 134:127–133. https://doi.org/10.1016/j.envres.2014.07.007
Ma Y, Zhou J, Yang S, Yu Z, Wang F, Zhou J (2019) Effects of extreme temperatures on hospital emergency room visits for respiratory diseases in Beijing, China. Environ Sci Pollut Res Int 26:3055–3064. https://doi.org/10.1007/s11356-018-3855-4
Ma Y, Zhou L, Chen K (2020) Burden of cause-specific mortality attributable to heat and cold: a multicity time-series study in Jiangsu Province, China. Environ Int 144:105994. https://doi.org/10.1016/j.envint.2020.105994
Muenchhoff M, Goulder PJ (2014) Sex differences in pediatric infectious diseases. J Infect Dis 209(Suppl 3):S120–S126. https://doi.org/10.1093/infdis/jiu232
Patz JA, Frumkin H, Holloway T, Vimont DJ, Haines A (2014) Climate change: challenges and opportunities for global health. Jama 312:1565–1580. https://doi.org/10.1001/jama.2014.13186
Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, Todd K, Mulholland JA, Ryan PB, Frumkin H (2005) Ambient air pollution and respiratory emergency department visits. Epidemiology 16:164–174. https://doi.org/10.1097/01.ede.0000152905.42113.db
Qiu H, Sun S, Tang R, Chan KP, Tian L (2016) Pneumonia hospitalization risk in the elderly attributable to cold and hot temperatures in Hong Kong. China Am J Epidemiol 184:555–569. https://doi.org/10.1093/aje/kww041
Rich DQ, Kipen HM, Huang W, Wang G, Wang Y, Zhu P, Ohman-Strickland P, Hu M, Philipp C, Diehl SR, Lu SE, Tong J, Gong J, Thomas D, Zhu T, Zhang J(J) (2012) Association between changes in air pollution levels during the Beijing Olympics and biomarkers of inflammation and thrombosis in healthy young adults. Jama 307:2068–2078. https://doi.org/10.1001/jama.2012.3488
Scovronick N, Sera F, Acquaotta F, Garzena D, Fratianni S, Wright CY, Gasparrini A (2018) The association between ambient temperature and mortality in South Africa: a time-series analysis. Environ Res 161:229–235. https://doi.org/10.1016/j.envres.2017.11.001
Shi J et al (2017) Cardiovascular benefits of wearing particulate-filtering respirators: a randomized crossover trial. Environ Health Perspect 125:175–180. https://doi.org/10.1289/ehp73
Shusterman D (2016) Nonallergic rhinitis: environmental determinants. Immunol Allergy Clin North Am 36:379–399. https://doi.org/10.1016/j.iac.2015.12.013
Song X, Wang S, Li T, Tian J, Ding G, Wang J, Wang J, Shang K (2018) The impact of heat waves and cold spells on respiratory emergency department visits in Beijing, China. Sci Total Environ 615:1499–1505. https://doi.org/10.1016/j.scitotenv.2017.09.108
Strosnider HM, Chang HH, Darrow LA, Liu Y, Vaidyanathan A, Strickland MJ (2019) Age-specific associations of ozone and fine particulate matter with respiratory emergency department visits in the United States. Am J Respir Crit Care Med 199:882–890. https://doi.org/10.1164/rccm.201806-1147OC
Sun S et al (2018) Seasonal temperature variability and emergency hospital admissions for respiratory diseases: a population-based cohort study Thorax 73:951-958. https://doi.org/10.1136/thoraxjnl-2017-211333
Szyszkowicz M, Kousha T, Castner J, Dales R (2018) Air pollution and emergency department visits for respiratory diseases: a multi-city case crossover study. Environ Res 163:263–269. https://doi.org/10.1016/j.envres.2018.01.043
Tian Y, Xiang X, Juan J, Sun K, Song J, Cao Y, Hu Y (2017) Fine particulate air pollution and hospital visits for asthma in Beijing. China Environ Pollut 230:227–233. https://doi.org/10.1016/j.envpol.2017.06.029
Tobías A, Armstrong B, Gasparrini A (2017) Brief report: investigating uncertainty in the minimum mortality temperature: methods and application to 52 Spanish cities. Epidemiology 28:72–76. https://doi.org/10.1097/ede.0000000000000567
Wang Y, Liu Y, Ye D, Li N, Bi P, Tong S, Wang Y, Cheng Y, Li Y, Yao X (2020) High temperatures and emergency department visits in 18 sites with different climatic characteristics in China: risk assessment and attributable fraction identification. Environ Int 136:105486. https://doi.org/10.1016/j.envint.2020.105486
Wu R et al (2019) Health benefit of air quality improvement in Guangzhou, China: results from a long time-series analysis (2006-2016). Environ Int 126:552–559. https://doi.org/10.1016/j.envint.2019.02.064
Wu R et al (2018) Temporal variations in ambient particulate matter reduction associated short-term mortality risks in Guangzhou, China: a time-series analysis (2006-2016). Sci Total Environ 645:491–498. https://doi.org/10.1016/j.scitotenv.2018.07.091
Xing H, Ling JX, Chen M, Johnson RD, Tominaga M, Wang CY, Gu J (2008) TRPM8 mechanism of autonomic nerve response to cold in respiratory airway. Mol Pain 4:22. https://doi.org/10.1186/1744-8069-4-22
Xu H et al. (2019) Ambient air pollution is associated with cardiac repolarization abnormalities in healthy adults Environ Res 171:239-246. https://doi.org/10.1016/j.envres.2019.01.023
Xu X, Li B, Huang H (1995) Air pollution and unscheduled hospital outpatient and emergency room visits. Environ Health Perspect 103:286–289. https://doi.org/10.1289/ehp.95103286
Xu Z, Etzel RA, Su H, Huang C, Guo Y, Tong S (2012) Impact of ambient temperature on children's health: a systematic review. Environ Res 117:120–131. https://doi.org/10.1016/j.envres.2012.07.002
Zhang H, Liu S, Chen Z, Zu B, Zhao Y (2020a) Effects of variations in meteorological factors on daily hospital visits for asthma: a time-series study. Environ Res 182:109115. https://doi.org/10.1016/j.envres.2020.109115
Zhang Y, Ding Z, Xiang Q, Wang W, Huang L, Mao F (2020b) Short-term effects of ambient PM1 and PM2.5 air pollution on hospital admission for respiratory diseases: case-crossover evidence from Shenzhen, China. Int J Hyg Environ Health 224:113418. https://doi.org/10.1016/j.ijheh.2019.11.001
Zhao Y, Huang Z, Wang S, Hu J, Xiao J, Li X, Liu T, Zeng W, Guo L, du Q, Ma W (2019) Morbidity burden of respiratory diseases attributable to ambient temperature: a case study in a subtropical city in China. Environ Health 18:89. https://doi.org/10.1186/s12940-019-0529-8
Zu K, Shi L, Prueitt RL, Liu X, Goodman JE (2018) Critical review of long-term ozone exposure and asthma development. Inhal Toxicol 30:99–113. https://doi.org/10.1080/08958378.2018.1455772
Acknowledgments
We thank all those who have helped us.
Funding
This study was supported by grants from National Key Research and Development Project (2017YFC0211701, 2016YFC0901103).
Author information
Authors and Affiliations
Contributions
Concept and design: W Huang, BP Xu, QH Zhang. Acquisition, analysis, or interpretation of data: J Song, RS Wu, HB Xu, YT Zhu, X Xu. Drafting of the manuscript: JK Fang, J Song. Critical revision of the manuscript for important intellectual content: W Huang, BP Xu. Statistical analysis: JK Fang, HB Xu, RS Wu, T Wang, NM Yuan. Obtained funding: W Huang, BP Xu. Administrative, technical, or material support: XM Song, YP Zeng, YF Xie. Supervision: W Huang, BP Xu, QH Zhang. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study did not contain confidential patient data. The Institutional Review Board of Beijing Children’s Hospital, Capital Medical University approved this study (IEC-C-028-A10-V.05). The patient’s consent to participate is not applicable in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 1287 kb)
Rights and permissions
About this article
Cite this article
Fang, J., Song, J., Wu, R. et al. Association between ambient temperature and childhood respiratory hospital visits in Beijing, China: a time-series study (2013–2017). Environ Sci Pollut Res 28, 29445–29454 (2021). https://doi.org/10.1007/s11356-021-12817-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-12817-w