Abstract
The main goal of this preliminary study was to quantify airborne particles and characterize the dominant cultivable bacterial species as well as some Gram-positive species, and their antibiotic resistance pattern, from environmental samples taken inside and outside of a dairy milking parlour. Sampling was performed over 2 days, in different seasons. The small viable particulate matter < 10 μm (bioaerosols) and cultivable bacteria reached their highest concentrations in the milking parlour. The majority of airborne bacteria in the milking parlour belonged to the genera Staphylococcus (41.9%) and Bacillus (20.9%). A total of 32 different bacterial species of Staphylococcus, Aerococcus, Bacillus, Pseudomonas, Serratia and Acinetobacter were identified. Many of these bacteria may be opportunistic pathogens, causing disease in humans or animals. We found low levels of acquired resistance to the antibiotics commonly used in human or animal infections caused by these opportunistic bacteria. More specifically, resistance to tetracyclines (13.4%), penicillin G (13.4%) and macrolides (7.5%) was identified in Staphylococcus sp. as was a methicillin-resistant S. hominis and resistance to spiramycin (n = 1), lincomycin (n = 1) and streptomycin (n = 2) in Aerococcus sp. An assessment of the occupational risk run by dairy farmers for contracting infections after long- or short-term exposure to micro-organisms requires further studies on the concentration of opportunistic pathogenic bacteria in dairy farm environments.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
France is the second-most important milk producer in Europe, after Germany. Nationwide, 61,733 dairy farms deliver cow’s milk. On dairy farms, cows are milked twice a day, and farmers therefore work for more than 3 h a day in a milking parlour. Inhalation of micro-organisms found in bioaerosols or airborne organic dust may be a health concern for workers in this confined environment, particularly in milking parlours where organic dusts are generated from faecal matter and animal skin (Roque et al. 2016) and suspended in the air by animal movements. In addition, airborne contamination in a milking facility is not only hazardous to workers and animals but is also a source of milk contamination (Piessens et al. 2011; Vacheyrou et al. 2011). Particulate matter (PM) can be inhaled and accumulate in the respiratory system. The link between PM10 and respiratory and other disease has been established (Mukherjee and Agrawal 2017). Dust particles ranging from 2.0 to 3.3 μm are associated with an increased incidence of cattle pneumonia (Wilson et al. 2002a). Bioaerosols from bacteria are typically smaller than 10 μm in diameter (Li et al. 2011; Millner 2009). Previous studies have reported that airborne bacteria from cow barns are often opportunistic pathogens (Dutkiewicz et al. 1994; Vacheyrou et al. 2011; Wilson et al. 2002b; Zucker et al. 2000). These bacteria are not associated with severe infections, but they can become pathogenic under certain conditions (e.g. disease, wound, medication, prior infection, immunodeficiency or advanced age). One recent study conducted in France illustrated that Curtobacterium, Bacillus, Corynebacterium, Aerococcus, Staphylococcus and Pseudomonas were the most predominant bacterial genera identified in the aerial environment of milking parlours (Vacheyrou et al. 2011).
The growing prevalence of antibiotic-resistant micro-organisms in this environment makes for an additional increasing health concern. Antibiotic resistance can be intrinsic (natural) or acquired through acquisition of resistance genes or bacterial mutation. The main risk involves the spread of acquired antibiotic resistance to pathogenic bacteria. In particular, multidrug-resistant (MDR) bacteria, including Escherichia coli resistant to extended-spectrum cephalosporins and methicillin-resistant Staphylococcus aureus (MRSA), are considered a major public health issue. The spread of antibiotic resistance genes to previously susceptible bacteria via PM has recently been reported in beef cattle feed yards (McEachran et al. 2015). Characterization of the airborne bacterial species in milking parlours can therefore provide important information for human and animal health. The main goal of this study was a preliminary study presenting the characteristics of the airborne flora over 2 days in different seasons by quantifying the PM from a dairy milking parlour. This study focused on the characterization of the dominant cultivable species and some Gram-positive species to screen for acquired antibiotic resistance phenotypes. The comprehensive airborne bacterial microflora was not quantified here. Bacterial species and PM concentrations inside and outside the milking parlour were compared on two sampling dates.
Materials and methods
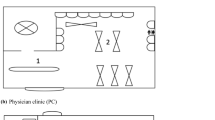
The experiment was conducted on a typical dairy cow farm located in the Rhône-Alpes region of France, housing approximately 20 Montbéliarde cows aged from 3 to 10 years of age. The cows on this farm are milked twice daily in a 70-m2 milking facility containing six automatic milk samplers. Manually opening of windows and doors in this milking parlour maintained the ventilation. Pipeline milkers transport the milk directly from the cow’s udder to the milk cooler and milk tank. Aerial samples were taken twice, once on 24 July (C1) and once on 2 October 2018 (C2). Outdoor air samples taken downstream wind milking parlour within a distance of 100 m away, in the early morning before milking, have been used for comparison with indoor aerial samples. These outdoor samples might be contaminated by the milking parlour source. The indoor air samples were collected during milking from 7:00 AM to 8:00 AM and just after milking. The outdoor air temperatures and relative humidity (%) during these two sampling sessions were extracted from data provided by the French weather observation association (https://asso.infoclimat.fr) (Table S1). The indoor relative humidity and temperature were monitored using the Testo 174H data logger only during C2, for which the mean values ± standard deviation (SD) were 14.3 ± 0.9 °C and 63 ± 3%, respectively. Indoor humidity remains relatively stable over time, because the floor is systematically hosed down before milking.
Particulate matter (PM) with sizes ranging from 0.5 to 25 μm was monitored using the BioTrak 9510-BD particle counter (TSI Incorporated, ville, pays). This counter uses laser-induced fluorescence, which is based on the detection of the fluorescence of the NADH, flavin and tryptophan molecules to determine whether a particle is viable or non-viable (micro-organism or inert). Our results were based on counts of particles ranging from 0.5 to 10 μm (PM10), which are typical of the aerodynamic diameters of bioaerosols (Li et al. 2016).
For bacterial counts, air samples were collected at 2 m above the ground using a STREAM Air sampler (AC-SPerhi, Saint Laurent des Arbres, France), containing a Petri dish filled with culture media and operating at a flow rate of 0.2 m3/min. The sampling volume was 0.4 m3 of air for the non-selective media and 1 m3 for selective media.
Aerobic bacteria were plated in Petri dishes on different non-selective and selective culture media. Non-selective media consisted of Columbia agar with 5% sheep blood (COS). Selective media were used to detect resistant bacteria: ChromID ESBL for the selective growth of extended-spectrum beta-lactamase-producing bacteria, Chapman2 for the detection of coagulase-positive staphylococci and ChromID Granada for Group B Streptococcus (bioMérieux, ville, France). A total of 86 aerial samples were collected. All Petri dishes were incubated at 37 °C for 18 h. After incubation, to determine the quantitative bacterial count (CFU/m3), the countable numbers of colonies (10–400 colonies) on COS plates were scored. From all Petri dishes, one to five colonies with different morphology, shape or colour were individually re-isolated on COS plates and identified using matrix-assisted desorption ionization time-of-flight (MALDI-TOF) mass spectrometry (Vitek®MS, ville, pays).
Antimicrobial susceptibility was tested using the disk diffusion method on Mueller-Hinton agar (Bio-Rad, Marne-la-Coquette, France). The antibiotic disks (Mast Diagnostics, Amiens, France) tested in this study are listed in Supplementary Table S2, and results were interpreted according to the zone diameter breakpoints recommended by the French committee on antimicrobial susceptibility testing (Comité de l’antibiogramme de la Société Française de microbiologie; CA-SFM 2019). The isolates presenting intermediate resistance were classified as resistant. For all staphylococci presenting a resistance phenotype to cefoxitin, the mecA gene was specifically screened for using a previously described method (Klingenberg et al. 2001).
Results
The sizes of both outdoor and indoor airborne particles were mostly (99.8–100%) equal to or less than 10 μm (PM10). The outdoor and indoor mean PM10 concentrations were significantly lower during the second air sampling date (Table 1). Indoor PM10 levels were 1.4–1.5 times higher than outdoor PM10 levels, during both sampling dates, C1 and C2 (Table 1). The variability of viable particles was higher in C2 (indoor SD = 48%, outdoor SD = 46%) than in C1 (indoor SD = 28%, outdoor SD = 13%) (Fig. 1). The mean proportion of viable PM10 particles smaller than or equal to 10 μm ranged from 0.08 (outdoors) to 0.49% (indoors). For both sampling dates, the concentration of airborne cultivable bacteria in the milking parlour ranged from 360 CFU/m3 to higher than 2 × 103 CFU/m3 of air. The proportion of viable particles in the cultivable airborne bacteria ranged from 0.8 to higher than 19%. PM10 and viable particles were significantly higher in the milking parlour during milking hours (Table 1, Fig. 1).
Distribution of particulate matter less than or equal to 10 μm in diameter (PM10) (a, c) and viable particles (b, d) inside and outside the milking parlour. The boxplot shows the distribution and variability of PM10 and viable particles (≤ 10 μm) recorded during the sampling on 24 July 2018 (C1) and on 2 October 2018 (C2). The box stretches from the first to the third quartile; the median is indicated by the thick black line in the box. The two lines outside the box extend to the highest (95th percentile) and lowest (5th percentile) observations. Circles indicate extreme values
Among the 222 selected colonies, reliable identification was obtained for 157 isolates (70.7%) using MALDI-TOF MS. Staphylococcus and Bacillus were the most frequently identified genera from the non-selective COS medium (41.9% and 20.9%, respectively) and from the selective Chapman medium (67.3% and 25.5%, respectively) (Fig. 2). Aerococcus viridans were detected on the Granada medium at a high frequency (61.1%), and Pseudomonas mendocina, P. putida and P. fluorescens were mainly isolated from the ESBL medium (70.6%). We did not find any Streptococcus on Granada media. For all media and sampling dates, Gram-positive bacteria were the most frequent airborne cultivable bacteria isolated on the growth media tested (Fig. 2). A total of 8 Gram-negative bacteria species and 24 Gram-positive species were identified (Figs. 2 and 3). A total of 12 bacterial species were identified both outdoors and indoors (Fig. 3a). However, 17 species were associated specifically with the milking parlour (Fig. 3a). Only three bacterial species were specifically detected outdoors (Fig. 3a). Interestingly, the most frequently isolated bacterial species (S. haemolyticus, B. altitudinis/pumilus, B. altitudinis/pumilus, A. viridans, A. lwoffii) (Fig. 2) were identified on both sampling dates (Fig. 3b), and the less prevalent species were specifically related to a unique sampling date (Fig. 3b).
The patterns of resistance to the antibiotics commonly used to treat human or animal infections caused by the dominant microflora Aerococcus sp. and Staphylococcus sp. are given in Tables 2 and 3. We also found that 6 of 13 Pseudomonas isolates identified on selective ESBL media were resistant to ticarcillin in combination with clavulanic acid or to fosfomycin. One of five Serratia isolates was resistant to chloramphenicol. Some bacterial species showed a multiple resistance profile, such as one isolate of P. putida resistant to fosfomycin, ticarcillin-clavulanic acid and one A. baumannii isolate resistant to fosfomycin, piperacillin, ceftazidime and aztreonam. One S. hominis isolate was methicillin resistant (MRS) and showed the associated resistance to penicillin G, tetracycline, erythromycin fusidic acid and cefoxitin. Cefoxitin resistance was confirmed by the presence of the mecA gene. All isolates of Bacillus sp. tested here were susceptible to aminoglycosides, vancomycin and tetracyclines. All the other isolates not mentioned here were susceptible to the tested antibiotic.
Discussion
The highest concentrations of PM10, viable particles and cultivable bacteria were reported in the milking parlour. The average concentrations of PM10 and viable particles were about the same level as that reported in previous studies for dairy confinements (Lee et al. 2006).
The higher variability of viable particle number observed in C2 compared to C1 could be linked to dust resuspension processes due to increased air humidity related to seasonal variability (Clements et al. 2018) and binding of dust on walls and floors (Basinas et al. 2014).
The increased number of viable particles among PM10 recorded in the milking parlour during the second sampling date (C2) may be associated with changes observed in meteorological conditions (increased air humidity, reduced air temperature, Table S1). Indeed bioaerosol (bacteria, viruses, pollens) concentrations and morphological characteristics of PM10 may undergo considerable changes according to environmental parameters, such as temperature, relative humidity and wind velocity (Lighthart 2000). However, the most important meteorological factors in the viability of airborne bacteria are temperature and UV radiation (Li et al. 2011).
In this study, the multi-channel instrument use for the monitoring the number of PM10 and viable particles was useful for rapid analysis in the field. However, the variation observed in the number of viable particles was not correlated with the number of cultivable bacteria. We can make the hypothesis that the proportion of cultivable bacteria among the viable particles was too low to allow comparison between these parameters. Moreover, there is not available data allowing comparison between the Biotrack counter technology providing the number of viable bacteria and plate counting showing the number of cultivable bacteria. Therefore, due to the notorious difficulty in isolating some Gram-negative bacteria including E. coli in air samples (Zucker et al. 2000), targeted real-time PCR may be an alternative to detect certain uncultivable pathogenic bacteria in future studies.
In this study, most cultivable bacterial species identified on selective and non-selective media can be human opportunistic pathogens (e.g. S. aureus, S. auricularis, A. lwoffii, B. circulans, E. hirae, S. marcescens, S. maltophilia) (Brooke 2012; O'Gara 2017) or can lead to food poisoning (B. cereus group, B. licheniformis) (Salkinoja-Salonen et al. 1999) and are related to a severe respiratory syndrome (A. viridans), abortion or cow mastitis (S. haemolyticus) in bovines (Roque et al. 2016; Shi et al. 2015) or can be opportunistic pathogen in swine (S. hyicus) (Staphylococcosis 2019). Most of the bacterial species that were detected only in the milking parlour, such as L. lactis, Bacillus sp., S. chromogenes, S. epidermidis and S. equorum, have been regularly isolated from indoor milking parlours and rarely from outdoor environmental samples (Piessens et al. 2011; Vacheyrou et al. 2011). In contrast, bacterial species such as A. viridans, S. haemolyticus, S. sciuri, S. xylosus, B. cereus and B. licheniformis are common in outdoor environmental samples. Other observations confirm that some of these bacterial species are able to survive and persist in environmental air samples taken from animal husbandry buildings (Piessens et al. 2011; Roque et al. 2016). Some opportunistic pathogens isolated during this study, such as B. altitudinis/pumilus, E. hirae or P. putida, S. maltophilia and S. marcescens, have not been described before in the aerial samples taken from cattle buildings.
The most frequently isolated bacterial species were common to C1 and C2; however, the diversity of strains seems to be higher in autumn (C2), while most of the identified bacteria belonged to Staphylococcus spp. during summer (C1). High air temperature may increase the grow of Staphylococcus spp. as was observed previously for S. aureus in a dairy barn (Islam et al. 2019). This seasonal effect on bioaerosol diversity and concentration in milking parlours need to be confirmed in further in depth work.
Information on antibiotic resistance from airborne bacteria in dairy farm is scarce (Navajas-Benito et al. 2017). The moderate percentage of bacteria resistant to antimicrobials found in the present work is in accordance with other studies carried out in cattle farms (Navajas-Benito et al. 2017). The main acquired antibiotic resistances observed in this study were resistances to enrofloxacine or tetracycline among A. viridans and Staphylococcus spp.. These results are in agreement with the patterns of resistance previously reported in dairy cows, probably because bovine mastitis is often treated with tetracycline or erythromycin worldwide (Oliver and Murinda 2012). Nevertheless, in this study, we isolated a coagulase-negative S. hominis opportunistic pathogen carrying the mecA gene from the air sample taken from the milking parlour environment. Methicillin-resistant S. hominis was previously identified in hospital and or in airborne dust at residential level (Lis et al. 2009); this work demonstrated the presence of methicillin-resistant S. hominis in bioaerosols from milking parlour and therefore confirms the spread of methicillin-resistant staphylococci in non-healthcare settings (Xu et al. 2015).
In conclusion, all these results provide new insights on airborne bacterial pathogen and antimicrobial resistance in dairy farm and suggest increased bacterial exposure during milking. The milking parlour air samples showed the presence of cultivable airborne bacteria, reaching high levels of contamination (> 2000 CFU/m3) according to the World Health Organization (WHO) (1988) guidelines (≤ 500 CFU mixture of species/m3) (Organization 1998). The data presented here suggest a possible exposure of farmers to opportunistic bacteria. In rare cases, these bacteria showed an acquired resistance pattern. Further studies on the concentration of opportunistic pathogen bacterial leading to infections after long- or short-term exposure are crucial for risk assessments.
Data availability
Not applicable.
References
Basinas I et al (2014) Exposure-affecting factors of dairy farmers’ exposure to inhalable dust and endotoxin. The Annals of Occupational Hygiene 58:707–723. https://doi.org/10.1093/annhyg/meu024
Brooke JS (2012) Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Microbiol Rev 25:2–41. https://doi.org/10.1128/CMR.00019-11
CA-SFM (2019) Comité de l’antibiogramme de la Société Française de Microbiologie: recommandations vétérinaires. https://www.sfm-microbiologie.org/2019/07/09/casfm-veterinaire-2019/ [Online]
Clements N, Keady P, Emerson JB, Fierer N, Miller SL (2018) Seasonal variability of airborne particulate matter and bacterial concentrations in Colorado homes. Atmosphere 9:133
Dutkiewicz J et al (1994) Airborne microorganisms and endotoxin in animal houses. Grana 33:85–90. https://doi.org/10.1080/00173139409427837
Islam MA, Ikeguchi A, Naide T (2019) Concentrations of aerosol numbers and airborne bacteria, and temperature and relative humidity, and their interrelationships in a tie-stall dairy barn animals. Basel 9:1023. https://doi.org/10.3390/ani9121023
Klingenberg C, Glad GT, Olsvik R, Flaegstad T (2001) Rapid PCR detection of the methicillin resistance gene, mecA, on the hands of medical and non-medical personnel and healthy children and on surfaces in a neonatal intensive care unit. Scand J Infect Dis 33:494–497
Lee S-A, Adhikari A, Grinshpun SA, McKay R, Shukla R, Reponen T (2006) Personal exposure to airborne dust and microorganisms in agricultural environments. J Occup Environ Hyg 3:118–130. https://doi.org/10.1080/15459620500524607
Li M, Qi J, Zhang H, Huang S, Li L, Gao D (2011) Concentration and size distribution of bioaerosols in an outdoor environment in the Qingdao coastal region. Sci Total Environ 409:3812–3819. https://doi.org/10.1016/j.scitotenv.2011.06.001
Li J, Zhou L, Zhang X, Xu C, Dong L, Yao M (2016) Bioaerosol emissions and detection of airborne antibiotic resistance genes from a wastewater treatment plant. Atmos Environ 124:404–412. https://doi.org/10.1016/j.atmosenv.2015.06.030
Lighthart B (2000) Mini-review of the concentration variations found in the alfresco atmospheric bacterial populations. Aerobiologia 16:7–16. https://doi.org/10.1023/a:1007694618888
Lis DO, Pacha JZ, Idzik D (2009) Methicillin resistance of airborne coagulase-negative staphylococci in homes of persons having contact with a hospital environment. Am J Infect Control 37:177–182. https://doi.org/10.1016/j.ajic.2008.09.013
McEachran AD, Blackwell BR, Hanson JD, Wooten KJ, Mayer GD, Cox SB, Smith PN (2015) Antibiotics, bacteria, and antibiotic resistance genes: aerial transport from cattle feed yards via particulate matter. Environ Health Perspect 123:337–343. https://doi.org/10.1289/ehp.1408555
Millner PD (2009) Bioaerosols associated with animal production operations. Bioresour Technol 100:5379–5385. https://doi.org/10.1016/j.biortech.2009.03.026
Mukherjee A, Agrawal M (2017) World air particulate matter: sources, distribution and health effects. Environ Chem Lett 15:283–309. https://doi.org/10.1007/s10311-017-0611-9
Navajas-Benito EV et al (2017) Molecular characterization of antibiotic resistance in Escherichia coli strains from a dairy cattle farm and its surroundings. J Sci Food Agric 97:362–365. https://doi.org/10.1002/jsfa.7709
O'Gara JP (2017) Into the storm: chasing the opportunistic pathogen Staphylococcus aureus from skin colonisation to life-threatening infections. Environ Microbiol 19:3823–3833. https://doi.org/10.1111/1462-2920.13833
Oliver SP, Murinda SE (2012) Antimicrobial resistance of mastitis pathogens. The Veterinary clinics of North America Food animal practice 28:165–185. https://doi.org/10.1016/j.cvfa.2012.03.005
Organization WH (1998) Indoor air quality: biological contaminants: report on a WHO meeting. Rautavaara, 29 August −2 September 1988
Piessens V et al (2011) Distribution of coagulase-negative Staphylococcus species from milk and environment of dairy cows differs between herds. J Dairy Sci 94:2933–2944. https://doi.org/10.3168/jds.2010-3956
Roque K et al (2016) Epizootiological characteristics of viable bacteria and fungi in indoor air from porcine, chicken, or bovine husbandry confinement buildings. J Vet Sci 17:531–538. https://doi.org/10.4142/jvs.2016.17.4.531
Salkinoja-Salonen MS, Vuorio R, Andersson MA, Kämpfer P, Andersson MC, Honkanen-Buzalski T, Scoging AC (1999) Toxigenic strains of Bacillus licheniformis related to food poisoning. Appl Environ Microbiol 65:4637–4645. https://doi.org/10.1128/AEM.65.10.4637-4645.1999
Shi D, Fang D, Hu X, Li A, Lv L, Guo J, Chen Y, Wu W, Guo F, Li L (2015) Draft genome sequence of Staphylococcus gallinarum DSM 20610T, originally isolated from the skin of a chicken. Genome announcements 3:e00580–e00515. https://doi.org/10.1128/genomeA.00580-15
Staphylococcosis (2019) In: Diseases of Swine. pp 926–933. https://doi.org/10.1002/9781119350927.ch60
Vacheyrou M, Normand A-C, Guyot P, Cassagne C, Piarroux R, Bouton Y (2011) Cultivable microbial communities in raw cow milk and potential transfers from stables of sixteen French farms. Int J Food Microbiol 146:253–262. https://doi.org/10.1016/j.ijfoodmicro.2011.02.033
Wilson SC, Morrow-Tesch J, Straus DC, Cooley JD, Wong WC, Mitlohner FM, McGlone JJ (2002a) Airborne microbial flora in a cattle feedlot. Appl Environ Microbiol 68:3238–3242
Wilson SC, Morrow-Tesch J, Straus DC, Cooley JD, Wong WC, Mitlöhner FM, McGlone JJ (2002b) Airborne microbial flora in a cattle feedlot. Appl Environ Microbiol 68:3238–3242. https://doi.org/10.1128/AEM.68.7.3238-3242.2002
Xu Z, Mkrtchyan HV, Cutler RR (2015) Antibiotic resistance and mecA characterization of coagulase-negative staphylococci isolated from three hotels in London, UK. Front Microbiol 6:947–947. https://doi.org/10.3389/fmicb.2015.00947
Zucker BA, Trojan S, Muller W (2000) Airborne gram-negative bacterial flora in animal houses Journal of veterinary medicine B. Infectious diseases and veterinary public health 47:37–46
Acknowledgements
We thank the dairy farmer and the veterinary that helped us to perform the sampling and to ensure cow health. The authors would like to thank the farmer Mr. Bergeon André who devoted her time to perform this study and the Dr. Veterinary Claire A.M. Becker, Associate Professor, VetAgro Sup, Université de Lyon.
Funding
Each partner (Anses Lyon (antimicrobial analysis, isolation of strains), IMT Mines Alès, Inrae (air sampling) and International Center for Infectiology Research (characterization of isolated strains) provided funds to perform this work.
Author information
Authors and Affiliations
Contributions
The work contribution was identification and numeration of bacterial species (Antoine Drapeau, Véronique Metayer, Frederic Laurent), analysis of bioaerosol and air borne micro-organisms data (Sandrine Bayle and Janick Rocher), design of the experimental study (Charlotte Valat and Sandrine Bayle), air sampling (Antoine Drapeau, Sandrine Bayle and Charlotte Valat), analysis of antimicrobial data (Marisa Haenni, Charlotte Valat, Antoine Drapeau and Jean-Yves Madec) and analysis of pathogen bacteria (Charlotte Valat and Frederic Laurent).
Charlotte Valat and Sandrine Bayle written the draft of the article, and all the authors have corrected the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
All authors consent to the publication of the manuscript in ELA, should the article be accepted by the ESPR Editor-in-Chief.
Additional information
Responsible editor: Diane Purchase
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Impact
We report data on the exposure of dairy farmers to airborne bacteria found in a milking parlour, and those are potentially opportunistic pathogens or resistant to antibiotics.
High concentrations of cultivable bacteria were found in the milking parlour, and there were significant differences in the bacterial diversity between indoor and outdoor environments.
Most of these bacteria were opportunistic pathogens and had low levels of acquired resistance. However, resistance to tetracyclines, penicillin G and macrolides was identified in Staphylococcus sp., and a methicillin-resistant S. hominis was observed.
Rights and permissions
About this article
Cite this article
Bayle, S., Drapeau, A., Rocher, J. et al. Characterization of cultivable airborne bacteria and their antimicrobial resistance pattern in French milking parlour. Environ Sci Pollut Res 28, 11689–11696 (2021). https://doi.org/10.1007/s11356-020-11974-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-020-11974-8