Abstract
Occupational exposure to inhalational anesthetics has been associated with health problems, including reproductive issues. Considering the scarcity and outdated nature of reviews concerning this relevant topic, which has implications for indoor pollution/environmental science/public health, this critical review aimed to systematically evaluate whether exposure to inhalational anesthetics is associated with abortion. Seven databases were searched with no language or year restrictions. Of the 3881 search results, 18 observational studies were included. Some studies demonstrated a significant association between occupational exposure to inhalational anesthetics and spontaneous abortion, especially among professionals who work for longer periods and/or in an environment without gas scavenging/ventilation systems, which may favor the occurrence of abortion in this population. Due to considerable heterogeneity and limitations, it cannot be concluded whether an association exists between occupational exposure to anesthetics and the occurrence of abortion. However, more well-designed studies should be performed, especially in less economically developed countries that do not have access to quality anesthetic gas scavenging/ventilation systems, thereby bringing this issue into sharp focus. This review highlights the need for scientific knowledge in this area and the extensive use of scavenging equipment and in the workplace to minimize exposure and reduce the risk of abortion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Health care workers are exposed to various hazards in the workplace, including biological, chemical, and physical agents, in addition to factors related to their work organization and workload. Due to the worldwide use of anesthetic agents and their possible toxic effects, studies have been carried out to evaluate the possible risks associated with occupational exposure to inhalational anesthetics in operating room professionals, including human and veterinary anesthesiologists, surgeons, technicians, nurses, and dentists and their assistants. Accordingly, occupational exposure to inhalational anesthetics has been linked to many health issues related to immunosuppression, mutagenicity, and oxidative stress (Braz et al. 2018; Chaoul et al. 2015; Lucio et al. 2018; Souza et al. 2016).
Additionally, reproductive issues, such as reduced fertility, premature births, congenital anomalies, and spontaneous abortion/miscarriage, have been reported to be associated with occupational exposure to inhalational anesthetics (Cohen et al. 1980; Nagella et al. 2015; Rowland et al. 1992; Shirangi et al. 2009; Warembourg et al. 2017). The first study concerning this issue was published in the 1960s and reported that 18 of 31 (58%) pregnancies ended in spontaneous abortion in female anesthesiologists exposed to diethyl ether, halothane, and nitrous oxide (N2O) (Vaĭsman 1967). However, this author also associated the increased spontaneous abortion rate with other possible factors other than anesthetic exposure, such as excessive workload and stress.
Inspired by this finding, other researchers conducted studies to verify the association between occupational exposure to anesthetics and spontaneous abortion; however, controversial findings have been described (Allweiler and Kogan 2013; Cohen et al. 1974; Pharoah et al. 1977; Rosenberg and Kirves 1973). A systematic review and meta-analysis of the risk of spontaneous abortion in women occupationally exposed to inhalational anesthetics was published in the late 1990s (Boivin 1997). However, the analysis was restricted to the period between 1980 and the beginning of the 1990s, used only one database, and only included papers written in English and French. Another review of the general effects of inhalational anesthetics on health, including pregnancy outcomes, using a systematic approach restricted the analysis to papers written in English, German, or Scandinavian published from the late 1990s to 2002 (Nilsson et al. 2005). In addition, a meta-analysis showed high heterogeneity among studies with a weak association between occupational exposure to anesthetics and spontaneous abortion in a systematic review focusing on English-language papers that evaluated occupational exposures and adverse pregnancy outcomes among nurses based on only two databases (Quansah and Jaakkola 2010).
Therefore, considering the scarce and outdated systematic reviews available in the literature concerning this important and relevant topic, which has implications for human and veterinary medicine, nursing, dentistry, environmental health, and women’s health, and considering that millions of female professionals in different areas around worldwide are occupationally exposed to several inhalational anesthetics, this critical review aimed to systematically evaluate whether occupational exposure to inhalational anesthetics is associated with spontaneous abortion. Thus, this review included different types of exposed females, searched several databases, and set no language or year restrictions.
Methods
Search strategy and selection criteria
Our review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al. 2015). The search strategy was performed using Medical Subject Heading (MeSH) terms and an exhaustive list of synonyms (Supplementary information 1) as word variants for “inhalation anesthetic” and “occupational exposure” and “spontaneous abortion” and “human” to identify all studies that reported occupational exposure to inhalational anesthetics and spontaneous abortion. The MEDLINE, EMBASE, LILACS, SciELO, Web of Science, Scopus, and CINAHL databases were analyzed, and the search strategy was adapted to each electronic database.
To select the studies, all obtained reports were reviewed, and the titles and abstracts were screened for relevance. The full text of the relevant abstracts was obtained and selected for screening. Two investigators independently screened and retrieved references to identify the studies to be included in the systematic review according to prespecified inclusion criteria. Subsequently, disagreements between the examiners were discussed with the other authors to reach a consensus. Additionally, we manually reviewed the review papers and references in different studies to identify relevant papers. There were no language or period restrictions, and translation services were used when necessary. The date of the final search was November 22, 2019.
Studies were included if they fulfilled all of the following criteria: (1) observational studies; (2) studies evaluating women occupationally exposed to any inhalational anesthetic who worked in human/animal operating rooms or dental offices/clinics (exposed group) and women who were not occupationally exposed to inhalational anesthetics (control group) who reported spontaneous abortion, as defined in each study; and (3) studies presenting spontaneous abortion rates in exposed and control groups.
The following exclusion criteria were adopted: (1) studies that did not include a control group related to the outcome (spontaneous abortion); (2) studies that did not present the abortion rates in the exposed and unexposed groups; and (3) reviews or only published abstracts.
Data extraction
The data extraction was performed using a standard form to record the authors, publication year, study location, type of study, sample size and target populations, participants’ age, study time, workplace description, information regarding occupational exposure to anesthetic(s) in the exposed group, inclusion criteria and confounding factors in the exposed and control groups, and the outcomes of spontaneous abortion, including definition, unit analysis and rates in both groups.
Assessment of the methodological quality
The methodological quality of the retrieved studies was assessed by three independent reviewers prior to inclusion in the review. We used the Joanna Briggs Institute (JBI) methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data to assess the following nine domains: target population, sampling, sample size, description of participants and setting, coverage of identified sample, methods used to identify the outcome, reliability of the outcome measurement, appropriate statistical analysis, and response rate (Munn et al. 2015). The cutoff point for the inclusion of a study in the review was a “yes” answer to at least five questions (more than 50%).
Results
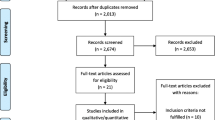
In total, the initial literature search yielded 3881 articles. We excluded 20 duplicates and manually identified ten titles. After the first screening (3871 papers) based on the title and abstract, the full text of 45 articles was read, and 27 articles were excluded. The methodological quality of all studies meeting the inclusion criteria was assessed, and all studies obtained five or more “yes” answers among the nine questions, indicating that the studies had a reasonable/good quality (Supplementary information 2). Thus, this systematic review included 18 studies (Fig. 1).
Seven studies were published in the 1970s (Cohen et al. 1971, 1974; Knill-Jones et al. 1972; Mirakhur and Badve 1975; Pharoah et al. 1977; Rosenberg and Kirves 1973; Rosenberg and Vänttinen 1978), five studies were published in the 1980s (Axelsson and Rylander 1982; Cohen et al. 1980; Ericson and Källén 1985; Heidam 1984; Lauwerys et al. 1981), four studies were published in the 1990s (Guirguis et al. 1990; Rowland et al. 1995; Saurel-Cubizolles et al. 1994; Schenker et al. 1990), one study covered the period from 1973 to 1990 (Lindbohm and Taskinen 2000), and only one study was published after 2000 (Allweiler and Kogan 2013). Of the 18 included studies, ten studies were conducted in Europe (Axelsson and Rylander 1982; Ericson and Källén 1985; Heidam 1984; Knill-Jones et al. 1972; Lauwerys et al. 1981; Lindbohm and Taskinen 2000; Pharoah et al. 1977; Rosenberg and Kirves 1973; Rosenberg and Vänttinen 1978; Saurel-Cubizolles et al. 1994), six studies were conducted in North America—largely in the USA (Cohen et al. 1971, 1974, 1980; Guirguis et al. 1990; Rowland et al. 1995; Schenker et al. 1990), one study covered North America (USA and Canada) and Europe (Allweiler and Kogan 2013), and only one study was conducted in Asia (Mirakhur and Badve 1975) (Table 1).
Of the 18 epidemiological studies investigating the association between maternal occupational exposure to inhalational anesthetics and risk of spontaneous abortion, most studies were designed as questionnaire-based surveys (Allweiler and Kogan 2013; Axelsson and Rylander 1982; Cohen et al. 1974, 1980; Guirguis et al. 1990; Heidam 1984; Knill-Jones et al. 1972; Lauwerys et al. 1981; Mirakhur and Badve 1975; Pharoah et al. 1977; Rosenberg and Kirves 1973; Rosenberg and Vänttinen 1978; Rowland et al. 1995; Saurel-Cubizolles et al. 1994; Schenker et al. 1990). The study with the largest response rate included a total of 21,202 participants, and the study with the lowest number of respondents included 98 participants. Considering all included studies, ten studies (55%) showed an association between occupational exposure to inhalational anesthetics and spontaneous abortion, while eight studies (45%) did not show this association.
The unit of analysis used to assess the frequency of abortion included the total number of pregnancies (most studies) or the total number of participants in each exposed and non-exposed group (Allweiler and Kogan 2013; Guirguis et al. 1990; Rowland et al. 1995). Spontaneous abortion was defined as fetal loss up to the 16th, 20th, 21st, or even 28th gestational week (Allweiler and Kogan 2013; Cohen et al. 1971, 1980; Guirguis et al. 1990; Rowland et al. 1995; Saurel-Cubizolles et al. 1994; Schenker et al. 1990). The other studies did not report definitions of abortion.
The period of occupational exposure to inhalational anesthetics varied as follows: before and/or during pregnancy (Cohen et al. 1974; Ericson and Källén 1985; Knill-Jones et al. 1972; Lauwerys et al. 1981; Rosenberg and Kirves 1973; Schenker et al. 1990) or during pregnancy only (Allweiler and Kogan 2013; Axelsson and Rylander 1982; Guirguis et al. 1990; Lindbohm and Taskinen 2000; Mirakhur and Badve 1975; Pharoah et al. 1977; Rosenberg and Vänttinen 1978; Rowland et al. 1995; Saurel-Cubizolles et al. 1994). The exposed populations included different professionals, and the medical anesthesiologists/nurse anesthetists and scrub nurses had the highest rates of abortion among the analyzed jobs, namely, 37.8% (Cohen et al. 1971), 19.5% (Rosenberg and Kirves 1973), 18.4% (Mirakhur and Badve 1975), 18.2% (Knill-Jones et al. 1972), 17% (Cohen et al. 1974), 13.8% (Pharoah et al. 1977), 10.1% (Rosenberg and Vänttinen 1978), 8.5% (Lauwerys et al. 1981), and 6.1% (Ericson and Källén 1985), followed by veterinarians with rates of 15.6% (Lindbohm and Taskinen 2000), 15.1% (Schenker et al. 1990), and 12.4% (Allweiler and Kogan 2013), and operating room personnel with rates of 15.6% (Guirguis et al. 1990), 12.4% (Axelsson and Rylander 1982), and 12.3% (Saurel-Cubizolles et al. 1994). The lowest rates were found among dentist assistants, namely, 10.5% (Heidam 1984) and 10.2% (Rowland et al. 1995), except for one study revealing a rate of 19.1% (Cohen et al. 1980).
Regarding working hours, the exposed groups were separated into high (> 3 h per week) and low (< 3 h per week) groups, and the study found a significantly increased spontaneous abortion rate in the group with the longer exposure period (Rowland et al. 1995). In another study, women who worked in areas with high exposure showed an abortion rate of 15.8% in comparison to those who worked in areas without exposure (9.1%), but the difference was not statistically significant (Axelsson and Rylander 1982).
In addition, the decade also seems to influence the abortion rate. In the 1970s, veterinarians had a higher risk of spontaneous abortion (15.6%) than the general population (9.7%) and controls (9.0%), but in the 1980s, these women no longer presented an elevated risk, i.e., the risk was below 10% (Lindbohm and Taskinen 2000).
Some studies utilized strict inclusion criteria, i.e., women who worked during the first trimester of pregnancy (Cohen et al. 1974; Lindbohm and Taskinen 2000; Saurel-Cubizolles et al. 1994), those who spent at least one (Cohen et al. 1980) or two (Guirguis et al. 1990) hours per week in the operating room, those with more than 5 years of experience in anesthetic practice (Mirakhur and Badve 1975), or those ranging in age 18 to 39 years old, who had been pregnant at least once and worked full time, i.e., 30 or more hours per week (Rowland et al. 1995). Other studies included female personnel who worked for at least 3 months with inhalational anesthetics (Axelsson and Rylander 1982) or worked in an operating room within the past 5 years (Cohen et al. 1971). Pregnant anesthetists who were working had a significantly higher rate of spontaneous abortion (18.2%) than pregnant anesthetists who were not working (13.7%) and unexposed pregnant women (control group; 14.7%) (Knill-Jones et al. 1972).
Most control groups consisted of professionals with jobs similar to those of the exposed individuals (e.g., nurses/physicians/veterinarians/dentists/dentist assistants who worked at the same location as those exposed but without exposure to waste anesthetic gases), but some studies included women registered in a hospital record or a national database (Axelsson and Rylander 1982; Ericson and Källén 1985). Individuals with different occupations were also included in the control groups (Heidam 1984; Lindbohm and Taskinen 2000; Schenker et al. 1990).
The most frequently mentioned anesthetics were N2O and halothane, and only seven articles described the types of anesthetics to which the population was exposed to (Cohen et al. 1980; Guirguis et al. 1990; Lauwerys et al. 1981; Mirakhur and Badve 1975; Rosenberg and Kirves 1973; Rosenberg and Vänttinen 1978; Rowland et al. 1995). The minimum anesthetic exposure time required varied from any exposure (Cohen et al. 1971) to at least 5 years (Mirakhur and Badve 1975); only one maximum exposure limit was reported, i.e., 65 hours per week (Guirguis et al. 1990). Scavenging systems in the workplaces (veterinarian operating rooms and dental offices) were only reported in two studies (Allweiler and Kogan 2013; Rowland et al. 1995). No significant differences in abortion rates were detected between veterinary anesthetists who worked in scavenging workplaces and wore charcoal filter masks when they become pregnant and women who worked in veterinary critical care (Allweiler and Kogan 2013). One study showed that dental assistants who worked in unscavenged workplaces had a higher abortion rate than those who worked in scavenged workplaces (Rowland et al. 1995). These authors divided unscavenged N2O exposure according to hours per week and observed that the women who worked 3–9 hours per week had elevated relative risks (2.5 to 5.1) of spontaneous abortion. Additionally, the same authors detected that professionals with three or more hours of weekly unscavenged N2O exposure had a substantially higher rate of loss than women with low exposure or unexposed women. Other studies mentioned that scavenging systems were important for the protection of professionals; however, no measurements were provided (Cohen et al. 1974, 1980; Ericson and Källén 1985; Guirguis et al. 1990; Lindbohm and Taskinen 2000; Mirakhur and Badve 1975; Rosenberg and Kirves 1973; Saurel-Cubizolles et al. 1994; Schenker et al. 1990).
In several papers, confounding factors, such as fertility treatments, smoking, medication, alcohol and drug consumption, diseases, exercise, an advanced maternal age, stress, co-exposures (mercury from amalgams, formaldehyde, antineoplastic drugs, and ionizing radiation), were reported in the exposed group (Allweiler and Kogan 2013; Axelsson and Rylander 1982; Cohen et al. 1971, 1974, 1980; Guirguis et al. 1990; Heidam 1984; Lauwerys et al. 1981; Pharoah et al. 1977; Rosenberg and Kirves 1973; Rosenberg and Vänttinen 1978; Rowland et al. 1995; Saurel-Cubizolles et al. 1994; Schenker et al. 1990). Some of these factors were adjusted in more than a half of the studies. The greatest age difference found between the exposed and non-exposed groups was 17 years (Lauwerys et al. 1981), and the lowest difference was approximately 3 years (Cohen et al. 1971).
In addition to an advanced maternal age, it was demonstrated that heavy tobacco consumption (10 or more cigarettes/day) increased the rate of spontaneous abortion in professionals who worked in anesthesiology departments (Axelsson and Rylander 1982). The same result was found among dentists and their assistants with co-exposure to mercury amalgam (Cohen et al. 1980; Rowland et al. 1995). Nurses exposed to waste anesthetic gases and co-exposed to formaldehyde and ionizing radiation during the first trimester of pregnancy presented a higher abortion rate than those not exposed or those exposed to only one or two of these agents (Saurel-Cubizolles et al. 1994).
Discussion
In the reproductive field, spontaneous abortion is a great concern among women, especially those occupationally exposed to inhalational anesthetics. A meta-analysis published more than 20 years ago indicated an increased risk of spontaneous abortion in women occupationally exposed to inhalational anesthetics (Boivin 1997). Another systematic review and meta-analysis published a decade ago evaluated adverse pregnancy outcomes exclusively among nurses and showed high heterogeneity among the studies with a weak association between occupational exposure to anesthetics and spontaneous abortion when only well-designed studies were considered (Quansah and Jaakkola 2010). Thus, this critical and systematic review aimed to synthesize and update the literature concerning the relationship between occupational exposure to waste anesthetic gases among health care workers and spontaneous abortion.
A slight association between occupational exposure to waste anesthetic gases and spontaneous abortion was found, but the significance of the findings is limited by the heterogeneity among the studies. Importantly, even those studies that found no significant association between the use of inhalational anesthetics in the workplace and occupational risks recommend the wide use of scavenging systems and the establishment of standard limits for waste anesthetic gases in the workplace to minimize occupational exposure.
The evaluation of the relationship between occupational exposure to waste anesthetic gases and the occurrence of spontaneous abortions is difficult due to methodological biases, and due to the lack of important information in several papers, it is challenging and difficult to properly analyze the data. Relevant data, such as the characteristics of the included subjects and exposure information (e.g., age of the participants/maternal age, unit of analysis of the abortion rate, abortion definition, period and type of anesthetic exposure, workplace, known concentrations of waste anesthetic gases, scavenging systems in the workplace, anesthesia equipment and flow of fresh gases used), are unclear or, in most studies, are not even reported by the authors. Additionally, confounding factors, such as an advanced gestational age, previous abortions, co-exposures, cigarette/alcohol use, and workload/stress, can also influence the findings.
Precise information related to abortion is lacking as abortion can occur outside the hospital and may not be registered or even noticed by the mother depending on the week of gestation; therefore, the incidence may be underreported. This lack of information significantly contributes to the inconclusive/conflicting results, and, as demonstrated in this review, occupational exposure to inhalational anesthetics involves many factors other than the actual exposure. In addition, it seems that women with fertility problems appear to be more likely to respond to research questionnaires than “healthy” women, which can also influence the results. Some studies had a small sample size and small percentage of included professionals. Notably, in particular, only a few studies measured the trace concentrations of inhalational anesthetics and reported whether there were scavenging/ventilation systems in the workplace.
Most reviewed studies were published from the 1970s to 1990, and only a few studies were published after 1990, demonstrating the lack of recent studies concerning this important topic. Nearly half of the studies conducted before 2000 reported a positive association between exposure to waste anesthetic gases and spontaneous abortion, while the study performed after 2000 did not find such an association.
One study that assessed the risk of spontaneous abortion found no difference between veterinarians exposed to inhalational anesthetics and control women (Lindbohm and Taskinen 2000). However, when the abortion rates were divided into decades, the frequency (15.6%) observed in the exposed professionals who worked in the 1970s was higher than that in the control group. In contrast, exposed professionals who worked in the 1980s had a risk of spontaneous abortion below 10%, which was similar to the rate in the unexposed group (9.0%). This result can be attributed to the types of anesthetics used in different decades and the implantation of scavenging systems in operating rooms.
In the 1960s and 1970s, the anesthetics used mainly included halothane, methoxyflurane, and enflurane in addition to N2O and ether. However, there were concerns regarding the toxicity of the halogenated agents because they were very fat-soluble and produced reactive metabolites, and N2O highly polluted the ambient atmosphere. In the 1970s, the National Institute of Occupational Safety and Health (NIOSH 1977) provided guidelines to limit occupational exposure to inhalational anesthetics to minimize risks, including exposure time, quantities of waste anesthetic gases, and use of scavenging and ventilation systems. Workers should not be exposed to N2O ≥ 25 parts per million (ppm) for more than 8 h/day or halogenated halothane and methoxyflurane at 2 ppm for more than 1 h.
A study showed that when dental assistants exposed to old-fashioned halogenated anesthetics and N2O were analyzed according to the exposure period (“light”, i.e., one to eight hours of exposure per week and “heavy”, i.e., more than eight hours per week), the rates of spontaneous abortion were 19.1% among the highly exposed professionals, 14.2% among those with low exposure, and 8.1% among the unexposed professionals, with a statistically significant difference (Cohen et al. 1980). Thus, a relationship seems to exist between an increase in the incidence of spontaneous abortion and a greater exposure time to waste anesthetic gases. Additionally, professionals only exposed to N2O had increased spontaneous abortion rates by twofold compared with unexposed women, suggesting that this anesthetic gas may negatively influence the pregnancy outcome. In addition, a study reported that professionals exposed to N2O in dental offices without a gas scavenging system for more than 3 h per week presented a higher abortion rate (2.6-fold increase) than the control group/low-exposure group (Rowland et al. 1995). These data may be attributable to the lack of a scavenging system since the evaluated workload was not excessive, highlighting the importance of implementing a proper gas scavenging system in the workplace.
The use of more modern halogenated anesthetics in the 1990s, such as isoflurane and sevoflurane, followed by desflurane, especially in high-income countries, and the addition of waste anesthetic gas scavenging systems in operating rooms certainly improved the safety of work environments. Indeed, the adoption of NIOSH or national recommendations in developed countries significantly reduced the concentration of waste anesthetic gases in the workplace, which greatly contributed to reduced abortion rates over time (Boivin 1997). In fact, the adverse effects related to spontaneous abortions observed in the older decades were no longer observed after the implementation of the recommendations intended to reduce occupational exposure to waste anesthetic gases in developed countries (Figà-Talamanca 2000; Warembourg et al. 2017). However, even in high-income countries, such as Australia, a study found that long working hours and the absence of scavenger systems for anesthetic gases are important risk factors for preterm birth in female veterinarians (Shirangi et al. 2009). Unfortunately, the epidemiological studies published to date provide very limited information regarding the relationship between the amount of exposure and magnitude of risk.
According to a meta-analysis (Boivin 1997), data obtained from a prescavenging area indicated an increased risk of spontaneous abortion. Conditions, especially in operating rooms, have changed since most reviewed epidemiological studies were performed. Intravenous anesthetics have been increasingly used, and the scavenging of waste anesthetic gases is applied in Canada, the USA, and most developed European countries. These measures have significantly reduced the concentrations of anesthetic gases relative to previous concentrations. Whether low levels of exposure remain associated with an increased risk of spontaneous abortion is unknown. However, the limited available data suggest that reproductive effects can be reduced and even eliminated by controlling the dispersion of gases by efficient scavenging devices. In fact, the most recent study included in this analysis involved women who worked in a veterinary anesthesia environment in which the American guidelines for scavenging waste anesthetic gases were applied, and the study showed no significant differences in reproductive issues between anesthesia and critical care faculty and staff despite the small sample size (Allweiler and Kogan 2013).
Notably, all studies evaluated in this review were conducted in European and North American countries (except for one Asian study), which do not reflect the situation in low-income countries that still use older and, therefore, less safe inhalational anesthetics. Furthermore, several developed countries, such as the USA, the UK, Germany, the Netherlands, Italy, and Scandinavian countries, have recommendations regarding exposure limits for inhalational anesthetics and also scavenging systems. However, these recommendations do not exist in less developed countries. For example, Brazil does not have recommendations regarding limits of occupational exposure to anesthetics or environmental monitoring. Therefore, it is very important for health professionals that hospitals and clinics provide a safe working environment to ensure the health of their own employees.
Data concerning reproductive outcomes following occupational exposure to anesthetics in less economically developed countries are lacking. Thus, studies investigating this topic are urgently needed, especially in low-income countries, since many of these countries do not use modern anesthetics and do not have modern anesthesia machines, and workplaces are inadequate since recommendations and laws do not even exist or are not applied.
High-income countries that have been following the recommended guidelines regarding occupational exposure to anesthetics for decades have minimal concern related to reproductive effects since most of these countries have scavenging systems, while a significant concern regarding the risk of spontaneous abortion likely exists in low-income countries. Currently, more modern halogenated anesthetics, such as isoflurane, sevoflurane, and desflurane, are widely used, but older and more toxic anesthetics, such as halothane, are still used in undeveloped and some developing countries, indicating a real problem in these countries. Additionally, N2O is used worldwide regardless of the economic development in the country. Therefore, all the waste anesthetic gases lead to workplace pollution, impairing health.
While modern scavenging systems have minimized this problem, numerous hospitals worldwide, including human and veterinary operating rooms and postanesthesia care units, do not have access to proper scavenging/ventilation systems, thereby bringing this issue into sharp focus. A study conducted in a developing South American country showed that in a public tertiary university hospital, half of the operating rooms had no scavenging system, and the levels of halogenated anesthetics largely exceeded the values recommended by NIOSH, while the other operating rooms had only “partial” scavenging systems (seven air changes/hour with air recirculation and a turbulent flow system), and the halogenated concentrations were lower than those in operating rooms without a scavenging system, but the exposure, particularly to sevoflurane, still exceeded the recommended limit (Braz et al. 2017). An Indian study showed that scavenging systems were present in only 33.5% of hospitals (Amma et al. 2016) due to the high initial investment cost of scavenging systems in resource-limited countries. Moreover, anesthesia workstations with safety features for low-flow fresh gases are not available in most such places, requiring the use of high-flow halogenated anesthetics, thereby increasing exposure. Indeed, this situation is the reality in most countries worldwide that do not have strict recommendations regarding limiting occupational exposure to anesthetics. In addition, very few studies investigating the possible detrimental effects of occupational exposure to inhalational anesthetics on the reproductive outcomes have been performed in these countries, certainly worsening the scenario and likely contributing to a public/women health issue due to negligence. Thus, due to their awareness of the possible toxic effects of waste anesthetic gases and because of the non-availability of scavenging systems, when available, female anesthesia providers working in operating rooms prefer total intravenous anesthesia over inhalational anesthetics during their pregnancy (Sharma et al. 2019). Studies conducted in developing countries should consider the specifications of human and veterinary anesthesia practice in these countries to contribute to a better understanding of exposed personnel since results in a specific population may not alert populations that are actually at risk of this possible hazard.
Regarding the unit of analysis of spontaneous abortion, the use of the total number of pregnancies could be more reasonable than the total number of participants since the comparison occurs between two outcomes of pregnancy, namely, aborted pregnancies and live births. More importantly, we noted that the abortion definition varied among the studies. In addition, among anesthesiologists, abortions occurred approximately 2 weeks earlier than they occurred in the control group (Cohen et al. 1971; Rosenberg and Vänttinen 1978). Nurses exposed to anesthetics experienced abortions at approximately the 9th week of gestation, while among non-exposed nurses, abortions occurred latter at approximately the 13th week (Rosenberg and Kirves 1973). This result demonstrates that abortions among professionals exposed to inhalational anesthetics may occur earlier than those among non-exposed professionals. It is important to differentiate between early and late abortion since spontaneous abortions occurring after the 7th week are usually due to chromosomal abnormalities (Burgoyne et al. 1991), which can be caused by occupational exposure to inhalational anesthetics (Shaker et al. 2011).
Confounding factors, such as the maternal age, previous abortions, smoking and/or alcohol consumption, and co-exposures, may also influence the abortion rates. Some factors were adjusted in most studies, suggesting that the authors were concerned that these factors could potentially interfere with the results. The age of the participants and maternal age reported in these studies widely varied. As expected, women aged ≥ 35 years have a higher frequency of abortions (Nybo Andersen et al. 2000); thus, maternal age can be an important confounding factor that should be considered in these types of study.
Along with an advanced maternal age, heavy tobacco consumption increased the rate of spontaneous abortion (Axelsson and Rylander 1982; Cohen et al. 1980). The co-exposure of professionals to other chemical and/or physical agents may also contribute to the abortion rate. Therefore, women with different jobs may have more or less exposure to other agents. For example, anesthesiologists are mainly exposed to anesthetics, and to a lower degree, radiation; dentists and their assistants are more frequently exposed to mercury because of amalgam. However, notably, several professionals properly protect themselves from radiation by using leaded aprons and cervical lead shields. Supporting the existence of these biases in the abortion outcome and the adjustments performed by some authors, three studies found that increased abortion rates in the presence of an advanced maternal age, smoking, formaldehyde, ionizing radiation, and/or mercury amalgam were also present (Axelsson and Rylander 1982; Cohen et al. 1980; Saurel-Cubizolles et al. 1994).
However, epidemiological research in this domain presents several methodological challenges, such as problems in selecting groups of exposed and unexposed women who are comparable with respect to risk factors of abortion other than exposure to anesthetics; inadequate controls for confounding effects; and potential biases arising from imperfect response rates to survey questionnaires or other research instruments. Future studies should be conducted using more elaborated methods to address specific exposure issues, such as assessing the role of anesthetics in the pregnancy outcome, describing whether the exposure is acute or long-term, using adequate control groups, comparing the abortion rates found with national records if available, providing a better definition of spontaneous abortion, measuring the levels of anesthetic gases, describing the types of anesthetics used in the assessed population, and reporting whether the studied population worked with or without scavenger/ventilation systems and/or with individual dosimeters, which could also contribute to the evaluation of the exposure and protection of these professionals. Studies conducted in less economically developed countries already reported that inhalational anesthetics lead to genetic damage in exposed professionals (Braz et al. 2018, 2020; Chandrasekhar et al. 2006; El-Ebiary et al. 2013; Izdes et al. 2010; Kargar Shouroki et al. 2019; Souza et al. 2016).
Interestingly, both female anesthesiologists and spouses of male anesthesiologists had a greater risk of first trimester abortion than the general population (Nagella et al. 2015). In addition, the wives of male dentists and doctors who were occupationally exposed to anesthestics also showed an increase risk of spontaneous abortion compared to the wives of professionals who were not exposed to anesthetics (Cohen et al. 1980; Guirguis et al. 1990). These results demonstrate that occupational exposure to inhalational anesthetics may also indirectly interfere with reproductive issues without the direct exposure of women. Thus, work exposures of parents to potentially hazardous agents, such as the inhalational anesthetics, may not only affect their own health, including that of their reproductive systems, but may also harm the health of their unborn children. Therefore, this issue continues to be a topic of scientific interest and public concern, and many open questions remain (Figà-Talamanca 2000).
All women, particularly those of childbearing age, should be fully informed of the possible reproductive effects of unscavenged anesthetic gases and should reduce their exposure by using protective devices when they are planning to become pregnant and during pregnancy. It seems prudent to reduce exposure to waste anesthetic gases to the lowest level possible. The rapid development of more efficient scavenging systems for use in dental surgery and in human and veterinarian operating/recovery rooms should have a high priority since the use of scavenging equipment in anesthetic systems may reduce the risk of adverse reproductive outcomes in exposed women.
The link between occupational exposure to inhalational anesthetics and reproductive effects, including spontaneous abortion, is a good example of how research can provide a basis for hazard prevention in the workplace. Considering that the literature concerning the subject is quite heterogeneous and presents some methodological limitations, whether an association exists between occupational exposure to waste anesthetic gases and the occurrence of spontaneous abortion in exposed women cannot be definitively determined. However, some studies demonstrated a significant association, especially among professionals who work for a longer time in an environment without gas scavenging/ventilation systems, which may favor the occurrence of spontaneous abortion in this population. Although no definitive conclusion was reached, this critical review aimed to illuminate the methodological difficulties encountered in these studies. This review highlights the need for scientific knowledge in this area and the extensive use of scavenging equipment and in the workplace, especially in low-income countries. Therefore, this systematic review could be useful for indoor pollution and public health policy and occupational risk prevention.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Allweiler SI, Kogan LR (2013) Inhalation anesthetics and the reproductive risk associated with occupational exposure among women working in veterinary anesthesia. Vet Anaesth Analg 40:285–289
Amma RO, Ravindran S, Koshy RC, Jagathnath Krishna KM (2016) A survey on the use of low flow anaesthesia and the choice of inhalational anaesthetic agents among anaesthesiologists of India. Indian J Anaesth 60:751–756
Axelsson G, Rylander R (1982) Exposure to anaesthetic gases and spontaneous abortion: response bias in a postal questionnaire study. Int J Epidemiol 11:250–256
Boivin JF (1997) Risk of spontaneous abortion in women occupationally exposed to anaesthetic gases: a meta-analysis. Occup Environ Med 54:541–548
Braz LG, Braz JRC, Cavalcante GAS, Souza KM, Lucio LMC, Braz MG (2017) Comparison of waste anesthetic gases in operating rooms with or without an scavenging system in a Brazilian University Hospital. Rev Bras Anestesiol 67:516–520
Braz MG, Souza KM, Lucio LMC, di Renzo GCC, Feliciano LM, Marcondes JPC, Chen CYO, Braz JRC, Braz LG (2018) Detrimental effects detected in exfoliated buccal cells from anesthesiology medical residents occupationally exposed to inhalation anesthetics: an observational study. Mutat Res 832-833:61–64
Braz MG, Carvalho LIM, Chen CO et al (2020) High concentrations of waste anesthetic gases induce genetic damage and inflammation in physicians exposed for three years: a cross-sectional study. Indoor Air 30:512–520
Burgoyne PS, Holland K, Stephens R (1991) Incidence of numerical chromosome anomalies in human pregnancy estimation from induced and spontaneous abortion data. Hum Reprod 6:555–565
Chandrasekhar M, Rekhadevi PV, Sailaja N, Rahman MF, Reddy JP, Mahboob M, Grover P (2006) Evaluation of genetic damage in operating room personnel exposed to anaesthetic gases. Mutagenesis 21:249–254
Chaoul MM, Braz JR, Lucio LM, Golim MA, Braz LG, Braz MG (2015) Does occupational exposure to anesthetic gases lead to increase of pro-inflammatory cytokines? Inflamm Res 64:939–942
Cohen EN, Bellville JW, Brown BW Jr (1971) Anesthesia, pregnancy and miscarriage: a study of operating room nurses and anesthetists. Anesthesiology 35:343–347
Cohen E, Brown BW, Bruce DL et al (1974) Occupational disease among operating room personnel: a national study. Anesthesiology 41:321–340
Cohen EN, Gift HC, Brown BW et al (1980) Occupational disease in dentistry and chronic exposure to trace anesthetic gases. J Am Dent Assoc 101:21–31
El-Ebiary AA, Abuelfadl AA, Sarhan NI, Othman MM (2013) Assessment of genotoxicity risk in operation room personnel by the alkaline comet assay. Hum Exp Toxicol 32:563–570
Ericson HA, Källén AJB (1985) Hospitalization for miscarriage and delivery outcome among Swedish nurses working in operating rooms 1973-1978. Anesth Analg 64:981–988
Figà-Talamanca I (2000) Reproductive problems among women health care workers: epidemiologic evidence and preventive strategies. Epidemiol Rev 22:249–260
Guirguis SS, Pelmear PL, Roy ML, Wong L (1990) Health effects associated with exposure to anaesthetic gases in Ontario hospital personnel. Occup Environ Med 47:490–497
Heidam LZ (1984) Spontaneous abortions among dental assistants, factory workers, painters, and gardening workers: a follow up study. J Epidemiol Community Health 38:149–155
Izdes S, Sardas S, Kadioglu E, Karakaya AE (2010) DNA damage, glutathione, and total antioxidant capacity in anesthesia nurses. Arch Environ Occup Health 65:211–217
Kargar Shouroki F, Neghab M, Mozdarani H, Alipour H, Yousefinejad S, Fardid R (2019) Genotoxicity of inhalational anesthetics and its relationship with the polymorphisms of GSTT1, GSTM1, and GSTP1 genes. Environ Sci Pollut Res Int 26:3530–3541
Knill-Jones RP, Rodrigues LV, Moir DD, Spence AA (1972) Anaesthetic practice and pregnancy. Controlled survey of women anaesthetists in the United Kingdom. Lancet 1:1326–1328
Lauwerys R, Siddons M, Misson CB, Borlee I, Bouckaert A, Lechat MF, de Temmerman P (1981) Anaesthetic health hazards among Belgian nurses and physicians. Int Arch Occup Environ Health 48:195–203
Lindbohm ML, Taskinen H (2000) Spontaneous abortions among veterinarians. Scand J Work Environ Health 26:501–506
Lucio LMC, Braz MG, do Nascimento Junior P, Braz JRC, Braz LG (2018) Occupational hazards, DNA damage, and oxidative stress on exposure to waste anesthetic gases. Rev Bras Anestesiol 68:33–41
Mirakhur RK, Badve AV (1975) Pregnancy and anaesthetic practice in India. Anaesthesia 30:18–22
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C (2015) Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 213:147–153
Nagella AB, Ravishankar M, Hemanth Kumar VR (2015) Anaesthesia practice and reproductive outcomes: facts unveiled. Indian J Anaesth 59:706–714
National Institute for Occupational Safety and Health (NIOSH). Criteria for a recommended standard: occupational exposure to waste anesthetic gases and vapors. 1977. Department of Health, Education, and Welfare, Public Health Service, Center for Disease Control
Nilsson R, Björdal C, Andersson M, Björdal J, Nyberg A, Welin B, Willman A (2005) Health risks and occupational exposure to volatile anaesthetics – a review with a systematic approach. J Clin Nurs 14:173–186
Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M (2000) Maternal age and fetal loss: population based register linkage study. BMJ 320:1708–1712
Pharoah PO, Alberman E, Doyle P, Chamberlain G (1977) Outcome of pregnancy among women in anaesthetic practice. Lancet 1:34–36
Quansah R, Jaakkola JJ (2010) Occupational exposures and adverse pregnancy outcomes among nurses: a systematic review and meta-analysis. J Women's Health (Larchmt) 19:1851–1862
Rosenberg P, Kirves A (1973) Miscarriages among operating theatre staff. Acta Anaesthesiol Scand 18:37–42
Rosenberg PH, Vänttinen H (1978) Occupational hazards to reproduction and health in anaesthetists and paediatricians. Acta Anaesthesiol Scand 22:202–207
Rowland AS, Baird DD, Weinberg CR, Shore DL, Shy CM, Wilcox AJ (1992) Reduced fertility among women employed as dental assistants exposed to high levels of nitrous oxide. N Engl J Med 327:993–997
Rowland AS, Baird DD, Shore DL, Weinberg CR, Savitz DA, Wilcox AJ (1995) Nitrous oxide and spontaneous abortion in female dental assistants. Am J Epidemiol 141:531–538
Saurel-Cubizolles MJ, Hays M, Estryn-Behar M (1994) Work in operating rooms and pregnancy outcome among nurses. Int Arch Occup Environ Health 66:235–241
Schenker MB, Samuels SJ, Green RS, Wiggins P (1990) Adverse reproductive outcomes among female veterinarians. Am J Epidemiol 132:96–106
Shaker DA, Samir AM, Hagag HA, Abd El-Aal AA, Afify RA (2011) Cytogenetic damage in operating room nurses exposed to anesthetic gases. Med J Cairo Univ 79:237–244
Sharma A, Bhatia P, Vyas V, Sethi P, Kaloria N, Sharma L (2019) Should total intravenous anesthesia be used to prevent the occupational waste anesthetic gas exposure of pregnant women in operating rooms? Anesth Analg 128:188–190
Shirangi A, Fritschi L, Holman CDJ (2009) Associations of unscavenged anesthetic gases and long working hours with preterm delivery in female veterinarians. Obstet Gynecol 113:1008–1017
Souza KM, Braz LG, Nogueira FR, Souza MB, Bincoleto LF, Aun AG, Corrente JE, Carvalho LR, Braz JRC, Braz MG (2016) Occupational exposure to anesthetics leads to genomic instability, cytotoxicity and proliferative changes. Mutat Res 791-792:42–48
Vaĭsman AI (1967) Working conditions in the operating room and their effect on the health of anesthetists. Eksp Khir Anesteziol 12:44–49
Warembourg C, Cordier S, Garlantézec R (2017) An update systematic review of fetal death, congenital anomalies, and fertility disorders among health care workers. Am J Ind Med 60:578–590
Acknowledgments
The authors would like to thank Marluci Betini for her help during the search strategy.
Funding
LAO received a fellowship (#129769/2016-9) from the National Council for Scientific and Technological Development (CNPq), Brazil.
Author information
Authors and Affiliations
Contributions
MGB, RPED, and LGB designed the study; LAO and MGB performed the searches and screened studies for eligibility; LAO and DBSF extracted the data; LGB, DBSF, and MGB assessed the quality of the papers; LAO and MGB drafted the manuscript; and LGB critically revised the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethical approval
Not applicable (there was no need for ethical approval due to the type of study, i.e., a systematic review).
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information may be found online.
ESM 1
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Oliveira, L.A., P. El Dib, R., Figueiredo, D.B.S. et al. Spontaneous abortion in women occupationally exposed to inhalational anesthetics: a critical systematic review. Environ Sci Pollut Res 28, 10436–10449 (2021). https://doi.org/10.1007/s11356-020-11684-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-020-11684-1