Abstract
Around 2.7 billion people in the world cook with polluting fuels, such as wood, crop residue, animal dung, charcoal, coal, and kerosene. Household air pollution from cooking with polluting fuels is recognized as a major risk factor for the disease burden. In this study, we examine the effect of using polluting fuels for cooking on the respiratory health of children in Pakistan. This study uses cross-sectional data from Pakistan Demographic and Health Survey 2012–13, with the sample size of 11,040 children under 5 years of age. Using logistic regression model, we control for factors such as averting activities, child characteristics, household characteristics, mother characteristics, and the unobserved factors using fixed effects. The results show that children in households using polluting fuels are 1.5 times more likely to have symptoms of acute respiratory infection (ARI) than children in households using cleaner fuels.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With advancements in almost all aspects of our life, it is hard to imagine that around 2.7 billion people in the world still rely on solid fuels such as wood, crop residue, animal dung, charcoal, and coal to meet their energy needs for cooking (International Energy Agency 2016; Watts et al. 2017). Smoke from burning these polluting fuels inside homes has profound negative impact on respiratory health. The respiratory illness from such exposures would not only raise morbidity but also reduce productivity and life expectancy (Duflo et al. 2008). Household air pollution from solid fuels is the leading risk factor for the disease burden in South Asia and the fourth largest risk factor for the global burden of disease (Lim et al. 2012). Worldwide, around 2.854 million people each year die prematurely from illness attributable to household air pollution from solid fuels according to the Global Burden of Disease study (GBD 2016).
Household air pollution from the use of solid fuels for cooking is a major threat to children’s health. Exposure to high level of cooking smoke leads to high incidence of respiratory morbidity, especially in infants and children, who mostly stay at home (Das et al. 2018; Horne et al. 2018). In developing countries, most women spend a great amount of time in kitchen while keeping infants and young children with them (Toman and Bluffstone 2017). A research study conducted in Pakistan finds that particulate matter (PM10) concentrations can reach up to 8555 μg/m3 in the kitchens where solid fuel is used for cooking (Colbeck et al. 2008). Thus, the use of solid fuels poses a serious threat to health, especially for women and children (Colbeck et al. 2010). Furthermore, smoke-driven respiratory diseases may also hamper cognitive growth and thus may lead to other diseases and illnesses in children as their immune system becomes vulnerable (Munroe and Gauvain 2012).
The issue of household air pollution from cooking fuel has been recognized in the literature since 1960s (Jacbos et al. 1962; Wohlers et al. 1967; Wilson 1968). Study by Lawther et al. (1970) is one of the pioneer studies in epidemiological literature establishing a relationship between health and indoor air pollution using data from London. Other studies thereafter improved upon methodology, such as developing theoretical model and estimation methods to control for confounding variables (Spengler and Sexton 1983; Samet et al. 1987; Bruce et al. 1998; Freeman et al. 2014).
As the literature on evaluating the impacts of household air pollution grows, increasingly there is a focus on respiratory health outcomes that are directly related to the cooking smoke. A number of empirical studies have been conducted to examine the effect of household air pollution from cooking fuel on respiratory health, especially on acute respiratory infection (ARI) in children (Ezzati and Kammen 2002; Torres-Duque et al. 2008). Mishra et al. (2005) studied the effects of cooking smoke and environmental tobacco smoke on ARI in young Indian children, using data for 29,768 children aged 3 years or younger collected from the National Family Health Survey of 1998–99. They found that, after controlling for other covariates such as age, sex of child, birth order, and nutritional status of child and other factors, children in households using biofuels (wood, crop residue, and animal dung) were 1.58 times more likely to have ARI symptoms than children in households using cleaner fuels. Another study by Mishra (2003) used data for 3559 children under 5 years from the Zimbabwe Demographic and Health Survey of 1999, and found that the children in households using biofuels were more than twice as likely to have ARI symptoms as children in households using cleaner fuels. Acharya et al. (2015) used the data from Nepal Demographic and Health Survey of 2011 to study the impact of solid fuel smoke on ARI in children less than 5 years old. They found that children in households using solid fuels had 1.79 times greater odds of having ARI symptoms than children in households using cleaner fuels. Capuno et al. (2018) used the data from the Philippine Demographic Health Survey of 2013 and found that the use of clean fuels for cooking reduces the incidence of respiratory illness symptoms in young children by 2.4% points. However, the studies cited above did not take into account any variable representing averting activity, which is an important determinant of health outcome as given in theoretical models (Freeman et al. 2014).
Pakistan is an energy-deficient country. According to Demographic Health Survey report, 62% of households in Pakistan cook with solid fuels, such as wood, crop residue, animal dung, charcoal, and coal (NIPS and ICF International 2013). Household air pollution is a big issue in Pakistan due to the use of solid fuels by majority of households. Siddiqui et al. (2009) compared indoor air pollution between the households using wood and those using natural gas in the kitchen. They found that wood users have much higher levels of carbon monoxide and particulate matter (PM2.5) as compared to natural gas users. According to Demographic Health Survey report, 16% of children aged less than 5 years have ARI symptoms in Pakistan (NIPS and ICF International 2013). Given the high incidence of ARI symptoms in children and high proportion of households using polluting fuels in Pakistan, there is a need to evaluate whether and to what extent the use of polluting fuels in cooking has the effect on ARI symptoms in children of Pakistan.
The existing literature on the effect of household air pollution on respiratory health outcomes in Pakistan is scarce. Janjua et al. (2012), using data for 566 children from a village in Dadu district in Sindh province, found that a higher incidence of ARI symptoms in children was associated with the use of biomass fuels for cooking. Similarly, another study by Ali Mir et al. (2012) used the data from Kashmir valley and found higher prevalence of ARI symptoms in children in households using biomass fuel for cooking as compared the households using LPG. However, these studies were limited to a very small geographical area in Pakistan. There have been no previous studies in Pakistan on examining the effect of household air pollution from cooking fuel on ARI in children using large and nationally representative data. Furthermore, it is important to control for averting activities and other factors that are important determinants of ARI in children. It may cause omitted variable bias if other factors are not controlled. Thus, controlling for other factors is particularly important for obtaining an unbiased estimate of the actual effect.
The purpose of this paper is to investigate the effect of household air pollution from cooking fuel on the prevalence of ARI in children under 5 years in Pakistan. We use data from nationally representative sample of 11,040 children under 5 years collected from Pakistan Demographic Health Survey (NIPS and ICF International 2013). Given the rich dataset, we control for not only averting activities and other observed factors but also unobserved location-specific factors such as outdoor air pollution using the fixed effects of geographic locations.
Data
This study uses data from Pakistan Demographic and Health Survey 2012–2013, conducted under the aegis of the Ministry of National Health Sciences, Regulations and Coordination and implemented by the National Institute of Population Studies (NIPS). The Pakistan Bureau of Statistics (PBS) provided technical assistance for the execution of the survey. For this survey, 14,000 households were selected from 500 primary sampling units, which are the enumeration blocks demarcated as part of the urban sampling frame in the urban domain and mouzas/dehs/villages in the rural domain. In this survey, out of an initial sample of 14,000 households, 12,943 households were interviewed with a response rate of 96%. The sampling design was a two-stage stratified cluster sampling with weights calculated based on sampling probabilities separately for each sampling stage and each block/village. The data is cross-sectional in nature, and the unit of analysis is children under the age of 5 years that are alive, as children in this age group are most vulnerable to the adverse effects of household air pollution (UNICEF 2016; Khan et al. 2017; Devakumar et al. 2018). The dataset included data for 11,040 children under 5-year age, which we use in this study. In this dataset, the age of children is reported based on birth certificate records available with relevant civil authorities of Pakistan (NIPS and ICF International 2013).
Model and estimation method
This study develops model based on the household health model, described in Freeman et al. (2014) originally formulated by Grossman (1972), and extended by Harrington and Portney (1987). Consider the case where a household has children whose health status may be affected by household air pollution from cooking fuel and other factors. A child’s health associated with the pollution level is described by a dose-response function. The econometric model of dose-response function is specified as follows:
where the outcome variable H is the status of ARI in child with H = 1 if the child has symptoms of ARI, otherwise 0. The status of ARI in child is a function of type of cooking fuel F used by the household, averting activities A undertaken by the household, and a set of other exogenous variables, denoted by vector X, including child characteristics, household characteristics, and mother characteristics. The error component ε includes the location-specific component u and the random error term e. H(.) is a function taking on values strictly between zero and one. Below, we describe the variables and discuss how the outcome variable can be affected by the explanatory variables given in Eq. (1).
Health outcome of child
In Eq. (1), the response variable is dichotomous in nature, that is, it is a dummy variable where H = 1 if the child has symptoms of ARI; otherwise 0. In the survey, mothers were asked if their child had been ill with a cough in the 2-week period preceding the survey. Those who answered in the positive to the question above were additionally asked if the child, when ill with cough, breathed faster than usual with short, rapid breaths. Children who suffered an illness related to cough accompanied by short and rapid breathing anytime during the last 2 weeks are defined as having symptoms of ARI. This measure of ARI symptoms has been used in previous studies (Mishra 2003; Mishra et al. 2005; Kilabuko and Nakai 2007).
We also define an alternative measure of ARI symptoms, as used in other previous studies (Acharya et al. 2015; Capuno et al. 2018). In this case, in addition to having cough and trouble breathing with short and rapid breaths, the child also has a chest-related problem. We also estimate the regression model using this alternative measure of ARI symptoms for robustness checks.
Cooking fuel
Type of cooking fuel affects the level of concentration of pollution, as Colbeck et al. (2008) found a higher level of PM10 in the kitchen where solid fuel was used for cooking. Exposure to the concentration of pollution, in turn, affects the health outcome (Freeman et al. 2014). Thus, type of cooking fuel is used as a predictor of ARI (Mishra et al. 2005; Acharya et al. 2015; Capuno et al. 2018).
Two groups were formed to categorize the cooking fuels according to their polluting behavior. One group includes all polluting fuels including solid fuels and kerosene, where solid fuels include wood, animal dung, charcoal, coal, and shrubs/grass/straw. The other group includes cleaner fuels, namely natural gas, LPG, biogas, and electricity. We define a dummy variable for the fuel type, that is, F = 1 if any polluting fuel is mainly used for cooking, otherwise 0.
Kerosene has recently been added to the list of polluting fuels (WHO 2016). We consider kerosene in the category of polluting fuels as recent research has shown that kerosene’s effect on household air pollution is highly positive (WHO 2016). We also define an alternative measure of cooking fuel type by excluding kerosene from polluting fuel. In this case, the dummy variable equals one if any of solid fuels is mainly used for cooking, and zero otherwise. For robustness checks, we also estimate the regression model using this alternative measure of cooking fuel type.
Averting activities
Averting activities are taken to reduce the exposure to pollution and thus affect the health outcome (Freeman et al. 2014). In this study, we use separate kitchen in the house and vaccination status of child as averting activities We define a dummy variable for each averting activity.
Child characteristics
Child characteristics include age, sex, birth order, and whether the child is breast-fed. Age is an important predictor of ARI. Children are most vulnerable to infections during their early months after birth, as their immune system is not fully developed (Simon et al. 2015). Sex of a child is an interesting predictor of ARI as it can indicate if there is any difference in immunity levels for each sex in the early months after birth. Birth order can highlight the high vulnerability of children those are first-borns. Children that are breastfed are less vulnerable to infections and therefore the expected relationship between ARI and breastfed children is negative (Naz et al. 2017).
Child’s age is considered in months with five equal intervals of 12 months. We define dummy variable for each age group. Sex of the child is a dummy variable where 1 is for males and 0 for females. Birth order is a categorical variable with four categories including first, second, third, and fourth order, where the fourth category represents the fourth birth or greater. For each category, a dummy variable is used for estimating the model.
Household characteristics
In this category, we use household crowding as a predictor of ARI. Household crowding means four or more people sleeping in a single room at one time. This increases the likelihood of respiratory infections (Cardoso et al. 2004; Prietsch et al. 2008; Baker et al. 2013); however, in certain cases, the evidence is not so convincing (Murray et al. 2012). This is a dummy variable equals 1 if the household is crowded, otherwise it is 0.
Mother characteristics
Mother’s characteristics include mother’s education, whether or not she smokes tobacco and her age at childbirth. Educated mothers are more likely to engage in averting activities as they are more aware of their children’s health and the risks associated with it (Gitawati 2014; Tekle et al. 2015; Tazinya et al. 2018). Children of tobacco smoking mothers are likely to be exposed to passive smoke, increasing the risk of respiratory infections including ARI symptoms, especially if children are less than 3 months old (Dahal et al. 2009; Gitawati 2014; Shibata et al. 2014). Children born to mothers older in age are likely to be at a lesser risk of ARI symptoms as such mothers are relatively healthier reproductively and pass on their stronger immune system to their children through breastfeeding (Prietsch et al. 2008). Mother’s education is a dummy variable which is equal to 1 if the mother is educated, otherwise 0. Similarly, “mother smokes tobacco” is a dummy variable which is equal to 1 if the mother smokes tobacco, otherwise 0. Mother’s age at childbirth is categorically divided into yearly brackets of 14–24, 25–35, and 36–49. For each category, a dummy variable is used for estimating the model.
We control for unobserved factors such as outdoor air pollution, accessibility of fuels, and other location-specific factors using the fixed effects of geographic locations. For geographic location fixed effect, we use primary sampling units (PSU), defined in data section.
Model in Eq. (1) is estimated using logistic regression model with the fixed effects by employing the conditional logit fixed-effects model. This approach removes any underlying omitted variable bias caused by the unobserved explanatory variables that may be correlated with the other explanatory variables included in the model. Because of the large sample properties, maximum likelihood estimation technique is used to produce consistent coefficient estimates. We account for the survey design and sample weights for estimation of coefficients so that over/under sampling and non-response rates do not influence the representativeness of the sample towards the population.
Results and discussion
Descriptive statistics
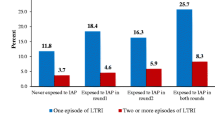
Table 1 presents the descriptive statistics of variables. The statistics show that around 22% of the children had ARI symptoms (cough with short and/or rapid breathing). Based on the alternative measure, 16% of the children had ARI symptoms (cough with short and/or rapid breathing and problem in chest). Around 68% of children are from households who mainly use polluting fuel for cooking purposes. Roughly, 51% of children are from households with a separate kitchen and on average 33.33% children are vaccinated. The distribution of children according to age and sex is equal while most of the children belong to the fourth birth order or more. A healthy 57% of the children are breastfed while 66% of children live in crowded conditions. Children belonging to educated mothers account for 44%, with some 3% of the mothers that smoked tobacco. More than half of the mothers belonged to 25–35 age group at childbirth while only 9% mothers belonged to 36–49 age group at childbirth.
Regression results
We present logistic regression results in this section. Table 2 presents the results with dependent variable health outcome of ARI symptoms (cough with short and/or rapid breathing). The table presents results for four models. In model (1), the explanatory variables include cooking fuel type and averting activities. In model (2), child characteristics are added in the explanatory variables. We add household characteristic in model (3). Finally, we add mother’s characteristics in model (4), which includes all explanatory variables. All models are estimated using fixed effects.
The results show that cooking fuel type is statistically significant at 5% level in all model specifications. We find that children belonging to households using polluting fuels are around 1.5 times more likely to have ARI symptoms as compared to households using cleaner fuels. The results match with those of India (Mishra et al. 2005). Results show that a separate kitchen is not statistically significant. Kilabuko and Nakai (2007) found that there was no significant difference in PM10 pollution levels from cooking indoors in a separate kitchen and cooking outdoors or cooking in the living room for Tanzania. Vaccination however, significantly reduces the likelihood of ARI symptoms in neonate children.
Age of child is statistically significant. The results show that children older than 2 years are less likely to have ARI symptoms as compared to those who are younger. Children that are breastfed are at a lesser risk of ARI symptoms with results at 1% significance across the four models. Household crowding is not a significant predictor of ARI symptoms. Children of educated mothers are less susceptible to have ARI symptoms. Mother’s age at child birth is statistically significant. Children of mothers between the age group of 25–35 years and 36–49 years face a lower risk of having ARI symptoms as compared to those of mothers belonging to age group of 14–24 years. Younger mothers are more susceptible to having weaker immune systems resulting in the delivery of children with weaker immune systems as well, which increases their chances of having ARI among other infections.
For robustness checks, we estimate four different models and report the estimated odds ratio for the effect of polluting fuel on ARI symptoms. Table 3 shows odds ratios, our primary definition of ARI symptoms (cough with short and/or rapid breathing), and our alternate definition of ARI symptoms (cough with short and/or rapid breathing and problem in chest), with and without sample weight adjusted coefficients. We find that polluting fuel in cooking fuel type is statistically insignificant, with the estimate of odds ratio as 1.38 and 1.30 in adjusted and unadjusted coefficients respectively. The results for other explanatory variables are similar as presented above. For robustness checks, we also estimate the regression model with solid fuels as an explanatory variable in place of polluting fuels. We find that the results were unchanged as there was only one observation where kerosene was used as main fuel for cooking. However, in Pakistan, kerosene is rarely used in cooking such as for making tea occasionally.
Even though this study is the first of its kind for Pakistan, it has some limitations. This study is based on indirect exposure assessment, which reduces the strength of causality. Using cooking fuel as a proxy for pollution exposure ignores the causal linkage between smoke inhalation and its impact on the respiratory health of children. In addition, many households, especially in rural areas do not consume a single type of cooking fuel, rather they use a combination of fuels for their cooking needs. For example, the wood from the trees does not make an attractive fuel choice in winter as the moisture in the wood limits its burning potential, so households combine animal dung and wood to cook food. Even though we have tried to control for the confounding factors by using the fixed-effects approach, there may well be certain variables such as ambient air pollution or the distance of market from the household, which may influence the risk of ARI symptoms indirectly. Lastly, our response variable of health outcome is ARI symptoms as reported by the mother, not a laboratory diagnosis, due to limitations in available dataset from DHS. Even though DHS offers a large nationally representative dataset, it lacks the holistic framework, which can allow for a more integrated assessment of exposure-response studies. For example, questions on type of cook stove used and duration of cooking can allow for better research studies.
This paper argues that there is a need for better alternatives for household energy consumption in Pakistan. Improved cook stoves have proven to dampen the harmful effects of cooking smoke on the respiratory system of women in Pakistan (Jamali et al. 2017). Efficient use of biomass fuels has also shown to reduce the burden of respiratory diseases among children in Pakistan (Butt et al. 2013). However, at a policy level, there is a need for direct exposure assessment studies (Clark et al. 2013), randomized controlled trials (RCTs) and a more comprehensive DHS survey which accounts for combined cooking fuel usage. Execution of initiatives such as the inclusion of pneumococcal vaccine in the index of Pakistan’s Expanded Program on Immunization (EPI) in October 2012 help in reducing the vulnerability of children under the age of 5 to respiratory infections and diseases.
Conclusion
This study finds that children living in households using polluting fuels for cooking purposes are 1.5 times more likely to have ARI symptoms than children living in households consuming cleaner fuels. Solid fuel consumption for cooking accounts for 62% in Pakistan. The burden of disease from household air pollution is likely to increase in Pakistan if counter-measures are not taken. The relationship between household air pollution and respiratory infections in young children is well established. Vaccination at childbirth, breastfeeding, education of mothers, and giving birth at a later age are factors, which reduce the risk of ARI in young Pakistani children. Informing and educating the young girls in Pakistan about the negative effects of household air pollution may be an effective short-term strategy to reduce incidence of ARI cases in the future.
References
Acharya P, Mishra SR, Berg-Beckhoff G (2015) Solid fuel in kitchen and acute respiratory tract infection among under five children: evidence from Nepal demographic and health survey 2011. J Community Health 40:515–521. https://doi.org/10.1007/s10900-014-9965-0
Ali Mir A, Fazili AAI, Iqbal J, Jabeen R, Salathia A (2012) Prevalence and risk factor analysis of acute respiratory tract infections in rural areas of Kashmir valley under 5 years of age. Int J Med Public Heal 2:47–52. https://doi.org/10.5530/ijmedph.2.3.10
Baker M, McDonald A, Zhang J, Howden-Chapman P (2013) Infectious diseases attributable to household crowding in New Zealand: a systematic review and burden of disease estimate, 2013 / Professor Michael G. Baker, Dr. Andrea McDonald, Jane Zhang, Professor Philippa Howden-Chapman. 1–80. http://www.healthyhousing.org.nz/wp-content/uploads/2010/01/HH-Crowding-ID-Burden-25-May-2013.pdf
Bruce N, Neufeld L, Boy E, West C (1998) Indoor biofuel air pollution and respiratory health: the role of confounding factors among women in highland Guatemala. Int J Epidemiol 27:454–458
Butt S, Hartmann I, Lenz V (2013) Bioenergy potential and consumption in Pakistan. Biomass Bioenergy 58:379–389. https://doi.org/10.1016/j.biombioe.2013.08.009
Capuno JJ, Tan CAR, Javier X (2018) Cooking and coughing: estimating the effects of clean fuel for cooking on the respiratory health of children in the Philippines. Glob Public Health 13:20–34. https://doi.org/10.1080/17441692.2016.1202297
Cardoso MRA, Cousens SN, De Góes Siqueira LF et al (2004) Crowding: risk factor or protective factor for lower respiratory disease in young children? BMC Public Health 4:1–8. https://doi.org/10.1186/1471-2458-4-19
Clark ML, Peel JL, Balakrishnan K, et al. (2013) Health and household air pollution from solid fuel use: the need for improved exposure assessment. 1120:1120–1129
Colbeck I, Nasir ZA, Hasnain S, Sultan S (2008) Indoor air quality at rural and urban sites in Pakistan. Water, Air, Soil Pollut Focus 8:61–69. https://doi.org/10.1007/s11267-007-9139-5
Dahal GP, Johnson FA, Padmadas SS (2009) Maternal smoking and acute respiratory infection symptoms among young children in Nepal: multilevel analysis. J Biosoc Sci 41:747–761. https://doi.org/10.1017/S0021932009990113
Das I, Pedit J, Handa S, Jagger P (2018) Household air pollution (HAP), microenvironment and child health: strategies for mitigating HAP exposure in urban Rwanda. Environ Res Lett 13:045011. https://doi.org/10.1088/1748-9326/aab047
Devakumar D, Qureshi Z, Mannell J, Baruwal M, Sharma N, Rehfuess E, Saville N, Manandhar D, Osrin D (2018) Women’s ideas about the health effects of household air pollution, developed through focus group discussions and artwork in southern Nepal. Int J Environ Res Public Health 15:1–13. https://doi.org/10.3390/ijerph15020248
Duflo E, Greenstone M, Hanna R (2008) Indoor air pollution, health and economic well-being. Surv Perspect Integr Environ Soc 1:1–9. https://doi.org/10.5194/sapiens-1-1-2008
Ezzati M, Kammen DM (2002) The health impacts of exposure to and data needs the health impacts of exposure to indoor air pollution from solid fuels in developing countries: knowledge, gaps, and data needs. Environ Health Perspect 110:1057–1068
Freeman MA, Herriges JA, Kling CL (2014) The measurement of environmental resource values, Third edn. RFF Press, Taylor & Francis, Oxon
GBD (2016) Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet 388:1659–1724. https://doi.org/10.1016/S0140-6736(16)31679-8
Gitawati R (2014) Bahan aktif dalam kombinasi obat flu dan batuk-pilek, dan pemilihan obat flu yang rasional Active ingredients in common cold fixed-dose combination products and analysis of its rationale. Media Litbangkes 24:10–18. https://doi.org/10.4172/2161-0711.1000176
Grossman M (1972) On the concept of health capital and the demand for health. J Polit Econ 80:223–255. https://doi.org/10.1086/259880
Harrington W, Portney P (1987) Valuing the benefits of health and safety regulations. J Urban Econ 22:101–112
Horne BD, Joy EA, Hofmann MG, et al. (2018) Short-term elevation of fine particulate matter air pollution and acute lower respiratory infection. Am J Respir Crit Care Med 1–39. https://doi.org/10.1164/rccm.201709-1883OC
International Energy Agency (2016) Energy and air pollution. World Energy Outlook - Spec Rep 266:133–156. https://doi.org/10.1021/ac00256a010
Jacbos MB, Manoharan A, Goldwater LJ (1962) Comparison of dust counts of indoor and outdoor air. Int J Air Water Pollut 6:205–213
Jamali T, Fatmi Z, Shahid A, Khoso A, Kadir MM, Sathiakumar N (2017) Evaluation of short-term health effects among rural women and reduction in household air pollution due to improved cooking stoves: quasi experimental study. Air Qual Atmos Heal 10:809–819. https://doi.org/10.1007/s11869-017-0481-0
Janjua NZ, Mahmood B, Dharma VK, Sathiakumar N, Khan MI (2012) Use of biomass fuel and acute respiratory infections in rural Pakistan. Public Health 126:855–862. https://doi.org/10.1016/j.puhe.2012.06.012
Khan MN, Nurs CZB, Islam MM et al (2017) Household air pollution from cooking and risk of adverse health and birth outcomes in Bangladesh: a nationwide population-based study. Environ Health 16:57. https://doi.org/10.1186/s12940-017-0272-y
Kilabuko JH, Nakai S (2007) Effects of cooking fuels on acute respiratory infections in children in Tanzania. Int J Environ Res Public Health 4:283–288. https://doi.org/10.3390/ijerph200704040003
Lawther PJ, Waller RE, Henderson M (1970) Air pollution and exacerbations of bronchitis. Thorax 25:525–539. https://doi.org/10.1136/thx.25.5.525
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, AlMazroa MA, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, Bahalim AN, Balakrishnan K, Balmes J, Barker-Collo S, Baxter A, Bell ML, Blore JD, Blyth F, Bonner C, Borges G, Bourne R, Boussinesq M, Brauer M, Brooks P, Bruce NG, Brunekreef B, Bryan-Hancock C, Bucello C, Buchbinder R, Bull F, Burnett RT, Byers TE, Calabria B, Carapetis J, Carnahan E, Chafe Z, Charlson F, Chen H, Chen JS, Cheng ATA, Child JC, Cohen A, Colson KE, Cowie BC, Darby S, Darling S, Davis A, Degenhardt L, Dentener F, Des Jarlais DC, Devries K, Dherani M, Ding EL, Dorsey ER, Driscoll T, Edmond K, Ali SE, Engell RE, Erwin PJ, Fahimi S, Falder G, Farzadfar F, Ferrari A, Finucane MM, Flaxman S, Fowkes FGR, Freedman G, Freeman MK, Gakidou E, Ghosh S, Giovannucci E, Gmel G, Graham K, Grainger R, Grant B, Gunnell D, Gutierrez HR, Hall W, Hoek HW, Hogan A, Hosgood HD III, Hoy D, Hu H, Hubbell BJ, Hutchings SJ, Ibeanusi SE, Jacklyn GL, Jasrasaria R, Jonas JB, Kan H, Kanis JA, Kassebaum N, Kawakami N, Khang YH, Khatibzadeh S, Khoo JP, Kok C, Laden F, Lalloo R, Lan Q, Lathlean T, Leasher JL, Leigh J, Li Y, Lin JK, Lipshultz SE, London S, Lozano R, Lu Y, Mak J, Malekzadeh R, Mallinger L, Marcenes W, March L, Marks R, Martin R, McGale P, McGrath J, Mehta S, Memish ZA, Mensah GA, Merriman TR, Micha R, Michaud C, Mishra V, Hanafiah KM, Mokdad AA, Morawska L, Mozaffarian D, Murphy T, Naghavi M, Neal B, Nelson PK, Nolla JM, Norman R, Olives C, Omer SB, Orchard J, Osborne R, Ostro B, Page A, Pandey KD, Parry CDH, Passmore E, Patra J, Pearce N, Pelizzari PM, Petzold M, Phillips MR, Pope D, Pope CA III, Powles J, Rao M, Razavi H, Rehfuess EA, Rehm JT, Ritz B, Rivara FP, Roberts T, Robinson C, Rodriguez-Portales JA, Romieu I, Room R, Rosenfeld LC, Roy A, Rushton L, Salomon JA, Sampson U, Sanchez-Riera L, Sanman E, Sapkota A, Seedat S, Shi P, Shield K, Shivakoti R, Singh GM, Sleet DA, Smith E, Smith KR, Stapelberg NJC, Steenland K, Stöckl H, Stovner LJ, Straif K, Straney L, Thurston GD, Tran JH, van Dingenen R, van Donkelaar A, Veerman JL, Vijayakumar L, Weintraub R, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams W, Wilson N, Woolf AD, Yip P, Zielinski JM, Lopez AD, Murray CJL, Ezzati M (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 380:2224–2260. https://doi.org/10.1016/S0140-6736(12)61766-8
Mishra V (2003) Indoor air pollution from biomass combustion and acute respiratory illness in preschool age children in Zimbabwe. Int J Epidemiol 32:847–853. https://doi.org/10.1093/ije/dyg240
Mishra V, Smith KR, Retherford RD (2005) Effects of cooking smoke and environmental tobacco smoke on acute respiratory infections in young Indian children. Popul Environ 26:375–396. https://doi.org/10.1007/s11111-005-0005-y
Munroe RL, Gauvain M (2012) Exposure to open-fire cooking and cognitive performance in children. Int J Environ Health Res 22:156–164. https://doi.org/10.1080/09603123.2011.628642
Murray EL, Klein M, Brondi L et al (2012) Rainfall, household crowding, and acute respiratory infections in the tropics. Epidemiol Infect 140:78–86. https://doi.org/10.1017/S0950268811000252
Naz S, Page A, Agho KE (2017) Household air pollution from use of cooking fuel and under-five mortality: the role of breastfeeding status and kitchen location in Pakistan. PLoS One 12:1–14. https://doi.org/10.1371/journal.pone.0173256
NIPS and ICF International (2013) Pakistan Demographic and Health Survey 2012–13. https://dhsprogram.com/pubs/pdf/FR290/FR290.pdf
Prietsch SOM, Fischer GB, César JA et al (2008) Acute lower respiratory illness in under-five children in Rio Grande, Rio Grande do Sul State, Brazil: prevalence and risk factors. Cad Saúde Pública 24:1429–1438
Samet JM, Marbury MC, Spengler JD (1987) Health effects and sources of indoor air pollution. Part I. Am Rev Respir Dis 136:1486–1508. https://doi.org/10.1164/ajrccm/136.6.1486
Shibata T, Wilson JL, Watson LM, LeDuc A, Meng C, Ansariadi, la Ane R, Manyullei S, Maidin A (2014) Childhood acute respiratory infections and household environment in an eastern indonesian urban setting. Int J Environ Res Public Health 11:12190–12203. https://doi.org/10.3390/ijerph111212190
Siddiqui AR, Lee K, Bennett D, Yang X, Brown KH, Bhutta ZA, Gold EB (2009) Indoor carbon monoxide and PM2.5 concentrations by cooking fuels in Pakistan. Indoor Air 19:75–82. https://doi.org/10.1111/j.1600-0668.2008.00563.x
Simon AK, Hollander GA, McMichael A (2015) Evolution of the immune system in humans from infancy to old age. Proc R Soc B Biol Sci 282:20143085. https://doi.org/10.1098/rspb.2014.3085
Spengler JD, Sexton K (1983) Indoor air pollution: a public health perspective. Science (80- ) 221:9–17
Tazinya AA, Halle-Ekane GE, Mbuagbaw LT, Abanda M, Atashili J, Obama MT (2018) Risk factors for acute respiratory infections in children under five years attending the Bamenda Regional Hospital in Cameroon. BMC Pulm Med 18:1–8. https://doi.org/10.1186/s12890-018-0579-7
Tekle AG, Worku A, Berhane Y (2015) Factors associated with acute respiratory infection in children under the age of 5 years: evidence from the 2011 Ethiopia Demographic and Health Survey. Pediatr Heal Med Ther 9. https://doi.org/10.2147/PHMT.S77915
Toman M, Bluffstone R (2017) Challenges in assessing the costs of household cooking energy in lower-income countries. World Bank Group, Policy Res Work Pap 25. https://doi.org/10.1596/1813-9450-8008
Torres-Duque C, Maldonado D, Perez-Padilla R, Ezzati M, Viegi G, on behalf of the Forum of International Respiratory Societies (FIRS) Task Force on Health Effects of Biomass Exposure (2008) Biomass fuels and respiratory diseases: a review of the evidence. Proc Am Thorac Soc 5:577–590. https://doi.org/10.1513/pats.200707-100RP
UNICEF (2016) Clear the air for children—the impact of air pollution on children. https://www.unicef.org/publications/index_92957.html
Watts N, Amann M, Ayeb-Karlsson S, Belesova K, Bouley T, Boykoff M, Byass P, Cai W, Campbell-Lendrum D, Chambers J, Cox PM, Daly M, Dasandi N, Davies M, Depledge M, Depoux A, Dominguez-Salas P, Drummond P, Ekins P, Flahault A, Frumkin H, Georgeson L, Ghanei M, Grace D, Graham H, Grojsman R, Haines A, Hamilton I, Hartinger S, Johnson A, Kelman I, Kiesewetter G, Kniveton D, Liang L, Lott M, Lowe R, Mace G, Odhiambo Sewe M, Maslin M, Mikhaylov S, Milner J, Latifi AM, Moradi-Lakeh M, Morrissey K, Murray K, Neville T, Nilsson M, Oreszczyn T, Owfi F, Pencheon D, Pye S, Rabbaniha M, Robinson E, Rocklöv J, Schütte S, Shumake-Guillemot J, Steinbach R, Tabatabaei M, Wheeler N, Wilkinson P, Gong P, Montgomery H, Costello A (2017) The Lancet countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet 391:581–630. https://doi.org/10.1016/S0140-6736(17)32464-9
WHO (2016) Clean Household Energy for Health, Sustainable Development, and Wellbeing of Women and Children. In: WHO Guidel. http://apps.who.int/iris/bitstream/10665/204717/1/9789241565233_eng.pdf?ua=1. Accessed 16 Mar 2017
Wilson H (1968) Indoor air pollution. Publ online OurWorldInDataorg 307:215–221. https://doi.org/10.1098/rspa.1968.0185
Wohlers HC, Newstein H, Daunis D (1967) Carbon monoxide and sulfur dioxide adsorption on— and desorption from glass, plastic, and metal tubings. J Air Pollut Control Assoc 17:753–756. https://doi.org/10.1080/00022470.1967.10469068
Acknowledgements
Special thanks to Dr. Christopher Baum, Professor of Economics and Social Work at Boston College for his input regarding economic modeling and estimation process.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible editor: Philippe Garrigues
Rights and permissions
About this article
Cite this article
Khan, M.S.B., Lohano, H.D. Household air pollution from cooking fuel and respiratory health risks for children in Pakistan. Environ Sci Pollut Res 25, 24778–24786 (2018). https://doi.org/10.1007/s11356-018-2513-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-018-2513-1