Abstract
Some widely prescribed drugs are sparsely metabolized and end up in the environment. They can thus be a focal point of ecotoxicity, either themselves or their environmental transformation products. In this context, we present a study concerning furosemide, a diuretic, which is mainly excreted unchanged. We investigated its biotransformation by two environmental fungi, Aspergillus candidus and Cunninghamella echinulata. The assessment of its ecotoxicity and that of its metabolites was performed using the Microtox test (ISO 11348-3) with Vibrio fischeri marine bacteria. Three metabolites were identified by means of HPLC-MS and 1H/13C NMR analysis: saluamine, a known pyridinium derivative and a hydroxy-ketone product, the latter having not been previously described. This hydroxy-ketone metabolite was obtained with C. echinulata and was further slowly transformed into saluamine. The pyridinium derivative was obtained in low amount with both strains. Metabolites, excepting saluamine, exhibited higher toxicity than furosemide, being the pyridinium structure the one with the most elevated toxic levels (EC50 = 34.40 ± 6.84 mg L−1). These results demonstrate that biotic environmental transformation products may present a higher environmental risk than the starting drug, hence highlighting the importance of boosting toxicological risk assessment related to the impact of pharmaceutical waste.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pharmaceuticals, which are substances designed to possess biological effects, are able to affect any function of the body of man or animals and they are used in diagnosis, prevention or cure of diseases. They are produced and used in large tonnage, and their presence in the environment as hazardous contaminants is now well recognized (Agerstrand et al. 2015; Khetan and Collins 2007). Several reports have shown their presence in effluents of sewage treatment plants (STPs) (Loos et al. 2013). Indeed, most pharmaceuticals enter municipal STPs via domestic and hospital sewages or through industrial discharges, part of them escaping degradation (Al Aukidy et al. 2014; Frederic and Yves 2014). They have been unequivocally detected in surface, ground and, in some cases, even in drinking water. Despite their low concentration levels, their continuous release into the environment makes them pseudo-persistent and hence a focal point of toxicity risk (Fent et al. 2006).
Once in the environment, pharmaceuticals undergo conversion processes that can induce the formation of a great variety of transformation products (TPs). They can be metabolized by different microorganisms (biotic transformations) and/or undergo photolysis, hydrolysis or chemical oxidation (abiotic transformations). In like manner, drugs can be transformed during sewage and drinking water treatment, resulting in the generation of different biologically and chemically transformed products (Fatta-Kassinos et al. 2011). These TPs may have similar activity to the parent compound or may be biologically more active and/or more toxic (Dirany et al. 2011; Khetan and Collins 2007; Morais et al. 2014). Additionally, they are commonly present as complex mixtures, whose combined toxicity may exceed that of each isolated compounds (Backhaus and Karlsson 2014). Consequently, the presence of pharmaceuticals and their TPs in environmental water sources represent a substantial toxicological risk for living organisms and humans (Celiz et al. 2009; de Jesus Gaffney et al. 2015). Determining the toxicity and ecotoxicity of these persistent micropollutants and their TPs is thus fundamental and a prerequisite for thorough risk assessment aiming at a comprehensive protection of the environment.
Microorganisms possess multiple-enzyme systems allowing them to metabolize xenobiotics into a wide range of transformation products. Accordingly, several active microbial strains, especially fungi, have been used as a competitive and ecologically effective approach for the preparation of diverse metabolites for different purposes, including drug metabolism studies (Azerad 1999; Marvalin and Azerad 2011). Aspergillus species have been widely used for the preparation of several potentially bioactive derivatives, whence evidencing its ability to biotransform a variety of chemicals (Adelin et al. 2011; Arakawa et al. 2013; Parshikov et al. 2015). Similarly, Cunninghamella species, a filamentous fungus found in soil and plant material, particularly at Mediterranean and subtropical zones, are able to perform biotransformations using both, phase I (oxidative) and phase II (conjugative) bio-mechanisms, imitating mammalian metabolism. In fact, they have P450 monooxygenase systems comparable to those in mammals and enzymes conducting phase II metabolism of drugs (Asha and Vidyavathi 2009; Felczak et al. 2016). In this way, microbial metabolism of xenobiotics is widely used as a model for mammalian metabolism studies. Paradoxically, the use of isolated wild strains in the investigation of the fate of drugs in the environment is not widespread (Murphy 2016), in spite of the potentiality of biotransformations as a very useful tool for the preparation of drugs’ transformation metabolites, aiming to strengthen and support predictive modelling and analysis on ecotoxicity and risk assessment.
Furosemide (FRSM), a widely prescribed loop diuretic, has been unambiguously detected in aquatic environments (Besse and Garric 2008; Mendoza et al. 2015; Oliveira et al. 2015) and it has been classified by the European Medicine Agency as one of the highest risk pharmaceuticals based on its exposure criteria (Huschek et al. 2004). It has been reported to cause side effects on some species, mainly hepatotoxicity and ototoxicity. Furthermore, its carcinogenic and genotoxic potential has also been suggested (Bucher et al. 1990; Mondal et al. 2012). These toxicological effects have been associated with the formation of toxic metabolites, which are capable of disrupting cellular functions by binding relevant cell macromolecules. A metabolite, under the form of an electrophilic epoxide, has been reported to be highly cytotoxic to liver hepatocytes (Williams et al. 2007). Moreover, FRSM alone or in mixture with other pharmaceuticals was reported to show estrogenic activity, mixtures having synergistic effects (Fent et al. 2006). Recently, we reported the microbial biotransformation of FRSM by selected bacteria and fungi, which were able to metabolize FRSM into saluamine (SLMN), a pyridinium derivative (PRDN) and another product. The pyridinium derivative was reported to be more toxic than the parent drug (Laurencé et al. 2014). Moreover, both metabolites, SLMN and PRDN, were as well detected during electrochemical oxidation of the drug by electro-Fenton (EF) process (Olvera-Vargas et al. 2015), whence suggesting their high probability to be generated as environmental transformation products.
The significant progress on the ongoing regulation concerning pharmaceutical residues witnesses the increasing preoccupancy about this environmental problem. In fact, three pharmaceuticals have been included in the “watch list” of emerging pollutants within the European Water Framework Directive (Directive 2013/39/EU) (Kuster and Adler 2014; Ribeiro et al. 2015). However, data related to toxicological effects of medicines and their TPs in the environment is still scarce and sometimes ambiguous; thereby, it is of primordial importance to reinforce environmental risk assessment through ecotoxicological approaches aiming at stablishing the most appropriate strategies for environmental management and monitoring regarding pharmaceutical waste. The present work investigates the bioconversion of FRSM by the environmental fungi Aspergillus candidus and Cunninghamella echinulata for toxicological evaluation. Three main metabolites were formed: SLMN, PRDN derivative, and a hydroxy-ketone (HK), the latter being described for the first time. A mechanistic pathway for the metabolism of FRSM by C. echinulata is proposed and ecotoxicological assays using V. fischeri bacteria revealed that PRDN and HK metabolites possess higher toxicological levels than FRSM itself.
Materials and methods
Chemicals and analysis methods
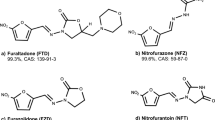
Furosemide (purity >98 %), trifluoroacetic acid and formic acid were of reagent grade from Fluka. PRDN was synthetized as described (Laurencé et al. 2011). Gradient grade HiPersSolv acetonitrile from VWR was used.
HPLC analysis was performed on Gilson system (pump 305, pump 306, gradient dynamic mixer 811B and autoinjector 234) with a Supelcosil LC-18, 3 μm (75 mm × 4.6 mm) column. The system was controlled and the results were analysed by Unipoint Gilson software. Column was eluted with an appropriate solvent system at a flow of 1.0 mL/min: (solvent A: water, 0.1 % trifluoroacetic acid; solvent B: 50 % water/50 % acetonitrile, 0.1 % trifluoroacetic acid) 0–5 min (isocratic 90/10), 5–8 min (gradient up to 50/50), 8–15 min (gradient up to 20/80), 15–20 min (isocratic 20/80). The detection was at 240 nm using an UV detector.
LC-MS analyses were performed on Nexera UHPLC chromatographer coupled with a MS2020 simple quadrupole mass spectrometer from Shimadzu, using atmospheric pressure chemical ionization (APCI). One microlitre of sample solutions was injected through a Nexera autosampler. A Kinetex column, 2.7 μm, C18 100 Å, 100 × 2.1 mm, from Phenomenex, was used, and a 10-min program was developed for these analyses using a binary A/B solvent system at a flow rate of 0.5 mL/min (solvent A: methanol, 0.01 % formic acid; solvent B: water, 0.01 % formic acid): 0–2 min (isocratic 5/95), 2–7 min (gradient up to 80/20), 7–8 min (isocratic 80/20). Eluted compounds were detected between m/z 50 and 600. Optimal MS settings were fixed as follows: drying gas: nitrogen, 15 L min−1; nebulizing gas: nitrogen, 1.5 L min−1; Qarray RF: 60 V; Qarray DC: 0 V; DL voltage and temperature: 0 V and 250 °C; detector voltage: 1.1 kV; APCI interface voltage: +4.5 kV; event time: 200 ms.
Preparative HPLC was performed on an Agilent system, using an Agilent PrepHT XDB-C18 column (21.2 × 150 mm; 5 μm; USA). Sample was injected and separated using the same gradient program for HPLC analysis. Three main peaks were obtained and collected in separated fractions.
Mass spectra data were recorded using an electrospray time of flight mass spectrometer (ESI-TOF-MS) operating in positive and negative modes (QSTAR Pulsar I of Applied Biosystems). NMR experiments were recorded on Bruker Avance III HD 400 MHz spectrometers (Wissembourg, France) equipped with a BBFO Plus Smartprobe.
Microorganisms and culture conditions
Fungal strains were obtained from the American Type Culture Collection (C. echinulata ATCC 9245, and A. candidus ATCC 20023). Cultures were maintained on agar slants (containing in g L−1: bactopeptones 5, yeast extract 5, malt extract 5, glucose 20 and agar 20) and stored at 4 °C. Liquid culture media containing (g L−1) glucose 16, yeast extract 4, malt extract 10, and soybean peptones 5 (YMS medium) were sterilized without glucose at 120 °C for 20 min. Separately sterilized glucose solution (40 %) was added afterwards. Flasks (100 mL) containing 50 mL of YMS culture medium were inoculated with glycerol suspension of microorganisms and incubated at 30 °C and 200 rpm (orbital shaker) for 60 h.
Biotransformations
For time-course studies of biotransformation, biomass was filtered, suspended in citrate or phosphate buffer and substrate was added in DMF solution for a final concentration of 0.4 g L−1. Biotransformations were performed in light. Samples were taken at regular intervals of time: 200 μL of methanol were added to 800 μL of biomass-containing sample, which was further stirred, sonicated and centrifuged prior to injection. A control experiment without biomass addition was conducted under the same conditions. No decrease in the concentration of FRSM was observed after 24 h, showing that photolysis of the drug is not significant.
Production of hydroxy-ketone and saluamine
C. echinulata ATTC 9245 was cultured in YMS medium (2 L) as described above. Biomass (300 g) was harvested by filtration and suspended in citrate buffer (0.5 L, 0.1 M pH 5). Furosemide was added (200 mg) in DMF solution, final concentration 0.4 g L−1. Incubation was performed under an air atmosphere at 27 °C and 200 rpm for 72 h. Cell suspension was filtered and incubation medium was extracted with ethyl acetate (3 times). Crude extract was re-dissolved in methanol and purified by preparative HPLC, giving SLMN (64 mg) in 42 % yield and HK (34 mg) in 17 % yield.
HK: HRMS (ESI-TOF) M-H+: m/z calc mass for C12H14ClNO6S 349.0261 g mol−1, found 349.0141 g mol−1. 1H NMR (400 MHz, DMSO-d6) δ (ppm): 8.69 (t, J = 4.8 Hz, 1H, N-H), 8.38 (s, 1H, H-10), 6.82 (s, 1H, H-7), 4.3 (d, J = 4.8, 2H, H-5), 3.39 (t, j = 6.4 Hz, 2H, H-1), 2.53 (t, J = 7.3 Hz, 2H, H-3), 1.68 (m, 2H, H-2). 13C NMR (100 MHz, DMSO-d6) δ (ppm): 206.04 (C-4), 168.8 (C-12), 152.4 (C-6), 136.7 (C-8), 133.7 (C-10), 127.1 (C-9), 114.4 (C-7), 108.4 (C-11), 60.5 (C-1), 52.4 (C-5), 36.7 (C-3), 27.03 (C-2).
Ecotoxicological tests
Toxicity tests were conducted with the photo-luminescent bacteria V. fischeri. The bioassay measures the decrease in bioluminescence induced in the cell metabolism by the presence of chemicals and it was performed in accordance with ISO 11348-3 procedure (Microtox@). The bacteria and the activation reagent, LCK 487 LUMISTOX, were provided by Hach Lange France SAS. A dilution series of the standard solutions of furosemide and the isolated metabolites: pyrimidium derivative, saluamine and hydroxyl-ketone, were prepared in 2 % NaCl and pH was adjusted to a value of 7. Bioluminescence intensity was measured using a luminometer Berthold™ Autolumat Plus LB 953, at time zero and after 15 min of exposure to the samples at 15 °C and compared to the measured value of the control solution (NaCl 2 %). Concentration of the toxicants produces a dose-response relationship from which the results as the 50 and 20 % inhibition effective concentration (EC20 and EC50, respectively) were deduced by nonlinear regression curves with variable Hill slope. Reported toxicity values are the average of 3 replicates of each sample with 95 % confidence limits. Phenol was tested as a control and it was found to be within the Microtox@ set parameters, EC50 between 13 and 26 mg L−1.
Results
Identification of furosemide metabolites
Biotransformation of FRSM by C. echinulata was conducted in preparative scale during 72 h. The chromatograms obtained by HPLC analysis showed the presence of two peaks apart from that of FRSM (Fig. 1a). The corresponding products were purified by preparative chromatography and analysed by LC-MS (Fig. 2). The MS spectrum in negative mode of the more polar compound M1 (Rt = 4.0 min) showed a molecular ion m/z 249, corresponding to the [M-H+]− ion (Fig. 2b, d). Along with the 1H NMR analysis, where protons from the furan ring were not observed, this product was identified as SLMN, whose formation by this fungus was confirmed.
The MS spectrum in negative mode of the second compound M2 (Rt = 5.01 min) showed a molecular ion [M-H+]− at m/z 349 (Fig. 2c, e) corresponding to an increase of 20 u compared to furosemide, which resulted from the addition of one oxygen and four hydrogen atoms. The presence of the chlorine atom in this metabolite was confirmed by the fact that the MS spectrum showed three peaks at m/z 349.0141, 351.0120 and 353.018 with relative intensity of 100, 30 and 10, respectively (Fig. S1). Additionally, the interpretation of the 1H NMR and 13C NMR spectra (Figs. S2 and S3), along with the two dimensional COSY, HSQS and HMBC spectra, allowed the unambiguous identification of the HK product with a molecular mass of 350.77 g mol−1. The MS/MS daughter ion spectrum (negative ion) showed two main fragmentation ions: at m/z 305 (loss of 44 u, CO2) and m/z 227 (loss of 35 + 87 u), the latter indicating the loss of chlorine and the COCH2CH2CH2OH group, which corresponds to cleavage of the bound next to the keto group. This fragmentation pattern is consistent with the metabolic transformation of the furan ring giving the γ-hydroxy-ketone. Moreover, the MS spectrum in negative mode of the HK solubilized in methanol revealed a protonated molecular ion m/z 363.0105 (Fig. S4), which corresponds to the ketal adduct resulting from intramolecular cyclization and addition of one molecule of methanol.
Regarding the biotransformation of FRSM by A. candidus, the chromatograms obtained in HPLC analysis during incubation also showed the presence of two peaks apart from that of FRSM (Fig. 1b), one of them having the same retention time of SLMN. The presence of the latter was confirmed by LC-MS analysis since an m/z peak of 249 in negative mode was observed (Fig. 3c, e). Compound M3 showed a Rt of 1.2 min and an m/z peak of 329 in positive mode in LC-MS, which corresponded to PRDN (Fig. 3b, c). Its formation was confirmed by the HRMS spectrum of the brut extract, which showed a peak at m/z 328.9975.
Effect of incubation conditions
The time courses of the bioconversion of FRSM were investigated in two different buffers, 0.1 M citrate buffer pH 5 and 0.1 M phosphate buffer pH 7. The results were illustrated in Figs. 4 and 5 for representative biotransformation. Figure 4 shows the evolution of FRSM and its metabolites SLMN and HK in terms of the percentage of peak area, assuming that all metabolites have a similar molar absorption coefficient. The evolution of PRDN, which was formed in much lesser amounts, is given in Fig. 5. It can be seen from Fig. 4a that FRSM was almost completely metabolized by C. echinulata when incubation was performed in phosphate buffer, while during incubations with A. candidus (Fig. 4b), only 50 % of FRSM was converted into SLMN as the main product. HK was the main metabolite produced by C. echinulata; however, its disappearance was observed after a long incubation time, as it was progressively transformed into SLMN. This fact was verified by incubation of purified HK with C. echinulata, which resulted in the formation of SLMN (Fig. S5). A control experiment was carried out in the absence of biomass, in which no significant decay on the concentration of HK was perceived, hence confirming that HK was not altered by abiotic factors. Moreover, an increase in the pH of the solution was observed during biotransformation (Figs. 4 and 5), especially for the incubations carried out in citrate buffer. In all cases, pH reached a value of 8 after 168 h of incubation, which can be attributed to the progressive metabolism of citrate by the microorganism. It may be noted that this increase of pH coincided with the appearance of SLMN.
Concerning PRDN (Fig. 5), this metabolite was produced by both microorganisms in all conditions, but in greater amount when using A. candidus. It is noteworthy that for both strains, PRDN appeared until the medium reached a pH value of 6 (Fig. 5) when citrate buffer was utilized (pH 5), thus suggesting that its formation is pH dependent, also taking into account that it was generated from the first stages of incubation when phosphate buffer (pH 7) was used. Finally, the influence of PRDN on FRSM biotransformation by A. candidus was assessed. The addition of PRDN in the incubation medium was found to entail inhibition of FRSM metabolism; hence, formation of SLMN did not take place.
Ecotoxicological assessment
Toxicity evaluation was carried out by means of the V. fischeri bioluminescence acute test. Toxicity values are expressed in terms of the effective concentration (EC50 and EC20), which represents the concentration causing 50 and 20 % of inhibition of luminescence, respectively (Fig. 6). These values were determined by fitting the experimental data to dose-response curves with variable Hill slope. The concentration-response curves are depicted in Fig. 7. Toxicity of FRSM and HK product are only expressed as EC20 being that they did not provoke more than 30 and 50 % of luminescence inhibition, respectively, at the tested concentrations. Only the data at 15-min contact were considered, as negligible difference was observed between the other exposure times.
The most remarkable issue is that metabolites HK and PRDN presented the highest toxicity levels, with EC50 = 34.40 ± 6.84 mg L−1 and EC20 = 18.94 ± 3.81 mg L−1 for PRDN, and EC20 = 37.42 ± 7.96 mg L−1 for HK.
Discussion
Biotransformation
Three metabolites have been observed during the biotransformations of FRSM, whose identification allowed proposing the metabolic pathway described in Scheme 1. SLMN was formed by both microorganisms and it resulted from FRSM N-dealkylation, which occurs through hydroxylation in the α-position of the amino group involving monooxygenase like cytochrome P450 enzyme, followed by hydrolysis of the hemiaminal intermediate (Hezari and Davis 1992; Williams et al. 2007). SLMN has also been detected as stable metabolite during the incubation of FRSM in the presence of river sediments (Li et al. 2014). These findings demonstrate that the use of microorganisms for the synthesis of TPs from pharmaceuticals is a potential approach for assessing the fate of drugs in environmental organisms.
HK, formed by C. echinulata, resulted from the oxidation of the furan ring. Such oxidation reactions involving cytochromes P450 have been reported through the formation of a cis-enedicarbonyl intermediate. Two mechanisms have been proposed: the formation of an epoxide followed by hydrolysis, or direct formation of cis-enedicarbonyl compound through the addition of the high valent iron (IV)-oxospecies to the π-system of the furan ring (Guengerich 2003). The double bond and the aldehyde group of the resulting cis-enedicarbonyl compound can be further reduced to form HK (Scheme 1). Indeed, it has been reported that aldehydes can be either reduced into the corresponding alcohol by microorganisms or oxidized into the corresponding carboxylic acid in animals (Lacroix et al. 1997). Interestingly, Antoine et al. detected a similar compound as one of the major biliary metabolites of FRSM in rats, a γ-keto-carboxylic acid derivative (Antoine et al. 2007). This γ-keto-carboxylic acid compound was also found during the electrochemical degradation of FRSM by means of the EF process (Olvera-Vargas et al. 2015).
Regarding PRDN, it was first reported by Chen et al. (Chen and Burka 2007), who explained its formation through intramolecular condensation of the amino group with the aldehyde of the generated cis-enedicarbonyl intermediate, this intermediate being common in the formation route of both, HK and PRDN metabolites (Scheme 1). In the case of C. echinulata, reduction of the aldehyde group resulted to be faster than its condensation with the amino group, hence mostly generating HK. Laurencé et al. (Laurencé et al. 2014) also described the generation of this compound during both, the microbial bioconversion of FRSM and its electrochemical oxidation.
The dependency of FRSM’s bioconversion on pH is an important fact being as it suggests that environmental conditions play a relevant role on the biodegradation of drugs. It is thus important to take into consideration these factors when assessing ecotoxocological and environmental risk.
Ecotoxicological aspects
Ecotoxicity assessment of furosemide and its microbial metabolites was carried out, firstly because furosemide and its metabolites have been described as having toxicological effects towards different organisms (Peterson 2013), and secondly because its occurrence in the environment with its concomitant biotic transformation (Jakimska et al. 2014) may degenerate into potential ecotoxic metabolites such as the PRDN derivative.
A low toxicity value was found for FRSM, EC20 = 72.29 mg L−1, evidencing its limited acute toxicity on V. fischeri. This result slightly differs from that found by Isidori et al. (Isidori et al. 2006), who reported no lethal risk for the same marine bacterium, and for the rotifers Brachionus calyciflorus. Similarly, a toxicological assessment conducted on this drug employing cnidarian Hydra vulgaris deployed an absent toxicity at concentrations up to 1 mg L−1 (Pascoe et al. 2003). Likewise, in a recent study, a moderate environmental risk was reported for FRSM, which was associated principally to its persistence and bioaccumulation, rather than to its toxicity (Mendoza et al. 2015). Nonetheless, these results contrast with the toxicological evaluation conducted on rodents and fish, which demonstrated the elevated hazard represented by this diuretic drug. Furthermore, FRSM was recently reported to present high toxicological risk for invertebrates and moderate risk for fish, according to its risk quotient (RQ) (Papageorgiou et al. 2016).
On the other hand, results demonstrate that the TPs resulting from the biotransformation of FRSM are more toxic that FRSM itself, a fact that has been previously suggested by some authors as discussed below.
PRDN gave the greatest ecotoxicity values, EC50 = 34.40 ± 6.84 mg L−1. Furthermore, its inhibitory effects on fungal oxidative enzymes were demonstrated since its presence hindered FRSM’s metabolism. This detrimental effect could also cause ecotoxicity as formerly described for other drugs (Barra Caracciolo et al. 2015). Previous toxicological evaluation reports also revealed PRDN’s noxious effects with an EC50 = 973 ± 46 μM according to the MTT test, as well as induction of cell death by the caspase-3 assay. Moreover, its use to induce symptoms associated to Parkinson’s disease for a chemical model of this neurodegenerative disorder has been recently patented (Martens et al. 2014).
Regarding HK derivative, which has not hitherto been identified, it exhibited higher ecotoxicity than the parent drug (EC20 = 36.60 mg L−1), however being less toxic than PRDN. HK is a reactive intermediate resulting from the oxidation of FRSM’s furan ring, whose progressive enzymatic oxidation was found to yield SLMN. The latter did not show any effect towards V. fischeri bacteria, which is in agreement with a previous toxicity study on SLMN that also evidenced a lack of hazardous effects (Laurencé et al. 2014). These findings suggest that toxicological effects can be attributed mainly to the highly active aromatic moieties: the furan and pyridinium rings.
Toxicity values indicate that the formed metabolites have a restricted acute toxicity on bacteria V. fischeri even at concentration ranges above the environmental levels. Nevertheless, the identification of metabolites having higher adverse effects than the parent drug denotes the necessity of investigating not only parent compounds but also potential TPs when assessing environmental impact, mostly taking into account that these hazardous compounds represent a potential risk for aquatic life by the long-term at low-level exposure, causing more subtle effects in growth, fertility, sex ratios or reproductive anomalies (Khetan and Collins 2007). Therefore, these findings point out the urgency of intensifying toxicological assessment facing the increasingly worrying ecological and health risk posed by pharmaceutical residues and their TPs.
Conclusion
It has been confirmed that the environmental fungi C. echinulata and A. candidus are capable of metabolizing FRSM into three main transformation products: saluamine, a pyridinium derivative and a hydroxy-ketone product, the latter having been described for the first time. Toxicity acute essays demonstrated that pyridinium and hydroxy-ketone metabolites have higher toxicity levels towards V. fischeri bacteria than FRSM. These results highlight the capacity of different microorganisms to transform pharmaceutical residues into stable metabolites, which are highly probable to be found in environmental water sources, therefore representing an ecotoxicological risk for both, ecosystems and human beings, as some of them can be even more toxic that the departing drug. Accordingly, this integral work gives a general perspective of the fate of drugs and their pernicious effects in the environment, which is essential for assessing environmental risk with the goal of developing the most convenient strategies for environmental management, including water control. Furthermore, this study can be regarded as a tool for the assessment of biotic transformation products from pharmaceutical pollutants, in response to the urgent necessity of reinforcing the evaluation of environmental hazard. Moreover, it contributes with valuable information with respect to the effects of drugs on environmental microbial communities, which is crucial for the comprehension of the biodegradation mechanisms drugs suffer in natural environments, as well as the harmful impacts on microbes.
References
Adelin E, Servy C, Cortial S, Levaique H, Gallard JF, Martin MT, Retailleau P, Bussaban B, Lumyong S, Ouazzani J (2011) Biotransformation of natural compounds. Oxido-reduction of Sch-642305 by Aspergillus ochraceus ATCC 1009. Bioorg Med Chem Lett 21:2456–2459. doi:10.1016/j.bmcl.2011.02.063
Agerstrand M, Berg C, Bjorlenius B, Breitholtz M, Brunstrom B, Fick J, Gunnarsson L, Larsson DG, Sumpter JP, Tysklind M, Ruden C (2015) Improving environmental risk assessment of human pharmaceuticals. Environ Sci Technol 49:5336–5345. doi:10.1021/acs.est.5b00302
Al Aukidy M, Verlicchi P, Voulvoulis N (2014) A framework for the assessment of the environmental risk posed by pharmaceuticals originating from hospital effluents. Sci Total Environ 493:54–64. doi:10.1016/j.scitotenv.2014.05.128
Antoine DJ, Williams DP, Regan SL, Park BK (2007) Formation of cytotoxic protein reactive metabolites from furosemide: biological consequences of drug metabolism. Toxicology 240:157–157. doi:10.1016/J.Tox.2007.06.079
Arakawa NS, Gobbo-Neto L, Ambrosio SR, Antonucci GA, Sampaio SV, Pupo MT, Said S, Schmidt TJ, Da Costa FB (2013) Unusual biotransformation products of the sesquiterpene lactone budlein A by Aspergillus species. Phytochemistry 96:92–100. doi:10.1016/j.phytochem.2013.09.022
Asha S, Vidyavathi M (2009) Cunninghamella—a microbial model for drug metabolism studies—a review. Biotechnol Adv 27:16–29. doi:10.1016/j.biotechadv.2008.07.005
Azerad R (1999) Microbial models for drug metabolism. Adv Biochem Eng Biotechnol 63:169–218
Backhaus T, Karlsson M (2014) Screening level mixture risk assessment of pharmaceuticals in STP effluents. Water Res 49:157–165. doi:10.1016/j.watres.2013.11.005
Barra Caracciolo A, Topp E, Grenni P (2015) Pharmaceuticals in the environment: biodegradation and effects on natural microbial communities a review. J Pharm Biomed Anal 106:25–36. doi:10.1016/j.jpba.2014.11.040
Besse JP, Garric J (2008) Human pharmaceuticals in surface waters implementation of a prioritization methodology and application to the French situation. Toxicol Lett 176:104–123. doi:10.1016/J.Toxlet.2007.10.012
Bucher JR, Huff J, Haseman JK, Eustis SL, Davis WE Jr, Meierhenry EF (1990) Toxicology and carcinogenicity studies of diuretics in F344 rats and B6C3F1 mice. 2. Furosemide. J Appl Toxicol 10:369–378. doi:10.1002/jat.2550100510
Celiz MD, Tso J, Aga DS (2009) Pharmaceutical metabolites in the environment: analytical challenges and ecological risks. Environ Toxicol Chem 28:2473–2484. doi:10.1897/09-173.1
Chen LJ, Burka LT (2007) Chemical and enzymatic oxidation of furosemide: formation of pyridinium salts. Chem Res Toxicol 20:1741–1744. doi:10.1021/tx700262z
de Jesus GV, Almeida CM, Rodrigues A, Ferreira E, Benoliel MJ, Cardoso VV (2015) Occurrence of pharmaceuticals in a water supply system and related human health risk assessment. Water Res 72:199–208. doi:10.1016/j.watres.2014.10.027
Dirany A, Efremova Aaron S, Oturan N, Sires I, Oturan MA, Aaron JJ (2011) Study of the toxicity of sulfamethoxazole and its degradation products in water by a bioluminescence method during application of the electro-Fenton treatment. Anal Bioanal Chem 400:353–360. doi:10.1007/s00216-010-4441-x
Fatta-Kassinos D, Vasquez MI, Kummerer K (2011) Transformation products of pharmaceuticals in surface waters and wastewater formed during photolysis and advanced oxidation processes—degradation, elucidation of byproducts and assessment of their biological potency. Chemosphere 85:693–709. doi:10.1016/j.chemosphere.2011.06.082
Felczak A, Bernat P, Rozalska S, Lisowska K (2016) Quinoline biodegradation by filamentous fungus Cunninghamella elegans and adaptive modifications of the fungal membrane composition. Environ Sci Pollut Res Int. doi:10.1007/s11356-016-6116-4
Fent K, Weston AA, Caminada D (2006) Ecotoxicology of human pharmaceuticals. Aquat Toxicol 76:122–159. doi:10.1016/j.aquatox.2005.09.009
Frederic O, Yves P (2014) Pharmaceuticals in hospital wastewater: their ecotoxicity and contribution to the environmental hazard of the effluent. Chemosphere 115:31–39. doi:10.1016/j.chemosphere.2014.01.016
Guengerich FP (2003) Cytochrome P450 oxidations in the generation of reactive electrophiles: epoxidation and related reactions. Arch Biochem Biophys 409:59–71. doi:10.1016/S0003-9861(02)00415-0
Hezari M, Davis PJ (1992) Microbial models of mammalian metabolism. N-dealkylation of furosemide to yield the mammalian metabolite CSA using Cunninghamella elegans. Drug Metab Dispos 20:882–888
Huschek G, Hansen PD, Maurer HH, Krengel D, Kayser A, European C (2004) Environmental risk assessment of medicinal products for human use according to European Commission recommendations. Environ Toxicol 19:226–240. doi:10.1002/tox.20015
Isidori M, Nardelli A, Parrella A, Pascarella L, Previtera L (2006) A multispecies study to assess the toxic and genotoxic effect of pharmaceuticals: furosemide and its photoproduct. Chemosphere 63:785–793. doi:10.1016/j.chemosphere.2005.07.078
Jakimska A, Sliwka-Kaszynska M, Reszczynska J, Namiesnik J, Kot-Wasik A (2014) Elucidation of transformation pathway of ketoprofen, ibuprofen, and furosemide in surface water and their occurrence in the aqueous environment using UHPLC-QTOF-MS. Anal Bioanal Chem 406:3667–3680. doi:10.1007/s00216-014-7614-1
Khetan SK, Collins TJ (2007) Human pharmaceuticals in the aquatic environment: a challenge to green chemistry. Chem Rev 107:2319–2364. doi:10.1021/cr020441w
Kuster A, Adler N (2014) Pharmaceuticals in the environment: scientific evidence of risks and its regulation. Philos Trans R Soc Lond Ser B Biol Sci 369. doi:10.1098/rstb.2013.0587
Lacroix I, Biton J, Azerad R (1997) Microbial biotransformations of a synthetic immunomodulating agent, HR325. Bioorg Med Chem 5:1369–1380. doi:10.1016/S0968-0896(97)00094-1
Laurencé C, Rivard M, Lachaise I, Bensemhoun J, Martens T (2011) Preparative access to transformation products (TPs) of furosemide: a versatile application of anodic oxidation. Tetrahedron 67:9518–9521. doi:10.1016/J.Tet.2011.10.006
Laurencé C, Rivard M, Martens T, Morin C, Buisson D, Bourcier S, Sablier M, Oturan MA (2014) Anticipating the fate and impact of organic environmental contaminants: a new approach applied to the pharmaceutical furosemide. Chemosphere 113:193–199. doi:10.1016/J.Chemosphere.2014.05.036
Li Z, Maier MP, Radke M (2014) Screening for pharmaceutical transformation products formed in river sediment by combining ultrahigh performance liquid chromatography/high resolution mass spectrometry with a rapid data-processing method. Anal Chim Acta 810:61–70. doi:10.1016/j.aca.2013.12.012
Loos R, Carvalho R, Antonio DC, Comero S, Locoro G, Tavazzi S, Paracchini B, Ghiani M, Lettieri T, Blaha L, Jarosova B, Voorspoels S, Servaes K, Haglund P, Fick J, Lindberg RH, Schwesig D, Gawlik BM (2013) EU-wide monitoring survey on emerging polar organic contaminants in wastewater treatment plant effluents. Water Res 47:6475–6487. doi:10.1016/j.watres.2013.08.024
Martens T, Rivard M, Laurence C, Morin C, Lehri-Boufala S (2014) Chemical model of a neurodegenerative disease, method for preparation and uses of same. WO 2014076439
Marvalin C, Azerad R (2011) Microbial production of phase I and phase II metabolites of propranolol. Xenobiotica 41:175–186. doi:10.3109/00498254.2010.535219
Mendoza A, Acena J, Perez S, Lopez de Alda M, Barcelo D, Gil A, Valcarcel Y (2015) Pharmaceuticals and iodinated contrast media in a hospital wastewater: a case study to analyse their presence and characterise their environmental risk and hazard. Environ Res 140:225–241. doi:10.1016/j.envres.2015.04.003
Mondal SC, Tripathi DN, Vikram A, Ramarao P, Jena GB (2012) Furosemide-induced genotoxicity and cytotoxicity in the hepatocytes, but weak genotoxicity in the bone marrow cells of mice. Fundam Clin Pharmacol 26:383–392. doi:10.1111/j.1472-8206.2011.00927.x
Morais SA, Delerue-Matos C, Gabarrell X (2014) An uncertainty and sensitivity analysis applied to the prioritisation of pharmaceuticals as surface water contaminants from wastewater treatment plant direct emissions. Sci Total Environ 490:342–350. doi:10.1016/j.scitotenv.2014.04.082
Murphy CD (2016) Microbial degradation of fluorinated drugs: biochemical pathways, impacts on the environment and potential applications. Appl Microbiol Biotechnol 100:2617–2627. doi:10.1007/s00253-016-7304-3
Oliveira TS, Murphy M, Mendola N, Wong V, Carlson D, Waring L (2015) Characterization of pharmaceuticals and personal care products in hospital effluent and waste water influent/effluent by direct-injection LC-MS-MS. Sci Total Environ 518-519:459–478. doi:10.1016/j.scitotenv.2015.02.104
Olvera-Vargas H, Oturan N, Buisson D, van Hullebusch ED, Oturan MA (2015) Electro-oxidation of the pharmaceutical furosemide: kinetics, mechanism, and by-products. CLEAN – Soil, Air, Water 43:1455–1463. doi:10.1002/clen.201400656
Papageorgiou M, Kosma C, Lambropoulou D (2016) Seasonal occurrence, removal, mass loading and environmental risk assessment of 55 pharmaceuticals and personal care products in a municipal wastewater treatment plant in Central Greece. Sci Total Environ 543:547–569. doi:10.1016/j.scitotenv.2015.11.047
Parshikov IA, Woodling KA, Sutherland JB (2015) Biotransformations of organic compounds mediated by cultures of Aspergillus niger. Appl Microbiol Biotechnol 99:6971–6986. doi:10.1007/s00253-015-6765-0
Pascoe D, Karntanut W, Muller CT (2003) Do pharmaceuticals affect freshwater invertebrates? A study with the cnidarian Hydra vulgaris. Chemosphere 51:521–528. doi:10.1016/S0045-6535(02)00860-3
Peterson LA (2013) Reactive metabolites in the biotransformation of molecules containing a furan ring. Chem Res Toxicol 26:6–25. doi:10.1021/tx3003824
Ribeiro AR, Nunes OC, Pereira MF, Silva AM (2015) An overview on the advanced oxidation processes applied for the treatment of water pollutants defined in the recently launched directive 2013/39/EU. Environ Int 75:33–51. doi:10.1016/j.envint.2014.10.027
Williams DP, Antoine DJ, Butler PJ, Jones R, Randle L, Payne A, Howard M, Gardner I, Blagg J, Park BK (2007) The metabolism and toxicity of furosemide in the Wistar rat and CD-1 mouse: a chemical and biochemical definition of the toxicophore. J Pharmacol Exp Ther 322:1208–1220. doi:10.1124/Jpet.107.125302
Acknowledgments
The authors wish to thank S. Amand for technical assistance, L. Dubost for mass spectra and A. Deville for NMR spectra.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Funding
This study was funded by the European Commission through the Erasmus Mundus Joint Doctorate Programme (Environmental Technologies for Contaminated Solids, Soils and Sediments) (grant number FPA n°2010–0009), and CONACyT, Mexico.
Additional information
Responsible editor: Philippe Garrigues
Electronic supplementary material
ESM 1
(PDF 2243 kb)
Rights and permissions
About this article
Cite this article
Olvera-Vargas, H., Leroy, S., Rivard, M. et al. Microbial biotransformation of furosemide for environmental risk assessment: identification of metabolites and toxicological evaluation. Environ Sci Pollut Res 23, 22691–22700 (2016). https://doi.org/10.1007/s11356-016-7398-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-016-7398-2








 ), pH buffer phosphate (
), pH buffer phosphate ( )
)
 ) and pH phosphate buffer (
) and pH phosphate buffer ( )
)
 ) and EC50 (
) and EC50 ( ) toxicity values (mg L−1) for V. fischeri luminescence acute tests with 95 % confidence limits. NE no effect
) toxicity values (mg L−1) for V. fischeri luminescence acute tests with 95 % confidence limits. NE no effect
