Abstract
Fine particulate matter (PM2.5) exposure is associated with morbidity and mortality induced by respiratory diseases and increases the lung cancer risk. However, the mechanisms therein involved are not yet fully clarified. In this study, the PM2.5 suspensions at different dosages (0.375, 1.5, 6.0, and 24.0 mg/kg body weight) were respectively given to rats by the intratracheal instillation. The results showed that PM2.5 exposure induced inflammatory cell infiltration and hyperemia in the lung tissues and increased the inflammatory cell numbers in bronchoalveolar lavage fluid. Furthermore, PM2.5 significantly elevated the levels of pro-inflammatory mediators including tumor necrosis factor-α (TNF-α), interleukin (IL)-6, IL-1β, and intercellular adhesion molecule 1 (ICAM-1) and the expression of c-fos and c-jun in rat lungs exposed to higher dose of PM2.5. These changes were accompanied by decreases of activities of superoxide dismutase and increases of levels of malondialdehyde, inducible nitric oxide synthase, nitric oxide, cytochrome P450s, and glutathione S-transferase. The results implicated that acute exposure to PM2.5 induced pathologically pulmonary changes, unchained inflammatory and oxidative stress processes, activated metabolic enzyme activity, and enhanced proto-oncogene expression, which might be one of the possible mechanisms by which PM2.5 pollution induces lung injury and may be the important determinants for the susceptibility to respiratory diseases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ambient fine particulate matter (PM2.5) with an aerodynamic diameter less than 2.5 μm is easily inhaled into the airway and deposited in lung alveoli, where the toxic particles may affect pulmonary structures and functions. Recent studies have revealed that ambient PM2.5 exposure increases the morbidity/mortality of pulmonary diseases and the risk of lung cancer in urban areas (Vinikoor-Imler et al. 2011; Li et al. 2013). PM2.5 is a complex mixture of organic and inorganic components including metals, salts, polycyclic aromatic hydrocarbons (PAHs), and carbonaceous material (Li et al. 2014; Cao et al. 2014). PM2.5 toxicity is related to pollution sources and its composition (Shi et al. 2015), and the water-soluble and organic-soluble extracts of urban airborne PM2.5 may induce DNA damage in a human lung epithelial cell line (Gutiérrez-Castillo et al. 2006; Bonetta et al. 2009). Epidemiologic study showed that ambient PAHs increased lung cancer risk of Chinese population (Zhang et al. 2009). PAHs, the important compositions of PM2.5, can be metabolically activated by two enzymes, cytochrome P450s (CYP450s), phase I enzymes, and glutathione S-transferases (GSTs), phase II enzymes (Ada et al. 2007).
It is noticed that chronic inflammation-induced production of reactive oxygen species (ROS) in the lung may predispose individuals to lung diseases including lung cancer (Azad et al. 2008; Rosanna and Salvatore 2012). Further, inhaled toxic agents stimulate the generation of reactive oxygen/nitrogen species (ROS/RNS), which in turn provoke inflammatory responses resulting in the release of proinflammatory cytokines including tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and IL-1β, leading to chronic inflammation and lung injury. During inflammation, enhanced ROS/RNS production may induce recurring DNA damage, inhibition of apoptosis, and activation of proto-oncogenes by initiating signal transduction pathways. Activation of proto-oncogenes, such as c-fos and c-jun, always occurs at an early stage of tumor development induced by the chemical carcinogens (Spandidos 2007). Increasing evidences have indicated that the production of oxidative stress, DNA breakage, micronucleus formation, 8-hydroxy-deoxyguanosine (8-OHdG) formation, and inflammatory responses are involved in PM2.5-mediated lung injury (Oh et al. 2011; Vattanasit et al. 2014).
However, further studies aiming at the elucidation of pathological injury, inflammation, oxidative stress, metabolizing enzyme activity, and expression of c-fos and c-jun in lungs of rats have hitherto not been fully established. In this work, we determined the histopathological changes, the levels of oxidative stress markers (superoxide dismutase, SOD; malondialdehyde, MDA; inducible nitric oxide synthase, iNOS; nitric oxide, NO), activities of CYP450s and GST, and the alterations of inflammatory cell numbers and inflammatory cytokines [TNF-α, IL-6, IL-1β, and intercellular adhesion molecule 1 (ICAM-1)] as well as the mRNA and protein expression of c-fos and c-jun in lungs of rats exposed to PM2.5 using real-time quantitative RT-PCR, Western blot, enzyme-linked immunosorbent assay (ELISA), hematoxylin-eosin staining (HE staining), and biochemical analysis methods, respectively.
Materials and methods
Sampling and preparation of particle samples
The sampling site and methods were performed as described in our previous study (Li et al. 2014). During PM2.5 concentration monitoring, aerosol samples were collected on quartz fiber filters (QFFs) for 24 h/day using a PM2.5 high-volume air sampler (Thermo Anderson, USA). The pump flow rate was about 1.13 m3/min. The QFFs after sampling were packed in clean aluminum foil and stored at −20 °C until analysis. The QFFs loading PM2.5 during the sampling time were, respectively, cut and surged in Milli-Q water with sonication. The PM2.5 suspensions of each filter were obtained and frozen dried in vacuum. Prior to use, the dried samples were mixed, weighted, and then diluted with sterilized 0.9 % physiological saline and swirled for 10 min.
Animal and treatment protocols
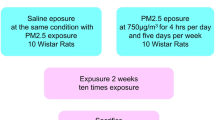
Healthy adult and clean grade male Wistar rats, weighing 180–200 g, were purchased from the Animal Center of Hebei Medical University. Animals were housed in metallic cages under standard conditions (24 ± 2 °C and 50 ± 5 % humidity) with a 12-h light–dark cycle. Rats were divided randomly into five equal groups of five animals each: (1) the control group (saline, pH 4.5), (2) 0.375 mg/kg body weight PM2.5 group, (3) 1.5 mg/kg body weight PM2.5 group, (4) 6.0 mg/kg body weight PM2.5 group, and (5) 24.0 mg/kg body weight PM2.5 group. The main doses of PM2.5 were based on our study (Li et al. 2015). The PM2.5 suspensions were respectively given to rats once by the intratracheal instillation at the first, third, fifth, seventh, and ninth day. Correspondingly, the control rats were treated with physiological saline.
Inflammatory cell counts and HE staining
The rats were narcotized by sodium pentobarbital (80 mg/kg, i.p.) 24 h after the last intratracheal instillation. Then, the right lung was ligated, and the left lung was immediately lavaged with phosphate-buffered saline (PBS pH 7.4) solution. Such process was repeated three times with 5 ml PBS as total volume. The counts of total cells in bronchoalveolar lavage fluids (BALF) were determined with a hemacytometer, and inflammatory cells were counted with Wright-Giemsa staining. After the collection of BALF, a piece of the right lungs was cut and fixed in 4 % paraformaldehyde in PBS and paraffin-embedded for the HE staining analysis, and the right lung was quickly frozen in liquid nitrogen and stored at −80 °C until analysis.
All animal procedures were approved by the Shanxi University Animal Investigational Committee and performed in accordance with the Guide for the Care and Use of Laboratory Animals published by the Ministry of Health People’s Republic of China.
Real-time quantitative RT-PCR
The frozen lung tissue samples were thawed, and mRNA was extracted using the Transzol reagent (Transgen, Beijing, China). Then, first-strand cDNA was synthesized using AMV RT First Strand cDNA Synthesis Kit (Transgen, Beijing, China) according to the manufacturer’s protocols. cDNA product was stored at −80 °C until use.
Expression levels were assessed by real-time PCR in an iCycler iQ Real-Time PCR Detection System (Bio-Rad, Richmond, CA, USA) with the Quantitect SYBR Green I PCR kit (Qiagen, Valencia, CA, USA). The PCR amplification of TNF-α, IL-6, IL-1β, ICAM-1, c-fos and c-jun was performed as described previously (Li et al. 2015). The relative quantification of the expression of the target genes was measured using the housekeeping gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH) mRNA as an internal control. The copy numbers of target gene/actin mRNA ratio were measured in all samples. The GenBank accession numbers and the primer sequences of the tested genes and actin together with the PCR product-amplified fragments are listed in Table 1.
Western blotting
Total proteins for ICAM-1, c-fos, c-jun, and actin from frozen lung tissues were respectively extracted with protein extraction kit (Beyotime, Shanghai, China) according to the manufacturer’s instructions. Protein concentrations were determined by BCA Protein Assay Kit (Beyotime, Shanghai, China). Samples were mixed with loading buffer and boiled for 5 min. Western blot analysis was performed as described previously (Li et al. 2015). The rabbit polyclonal primary antibodies for rat c-fos, c-jun, ICAM-1, and actin (Santa Cruz, CA, USA) were incubated overnight at 4 °C, whereas the infrared-labeled anti-rabbit secondary antibody (LI-COR Biosciences, USA) at a concentration of 1:5,000 were added to membranes and incubated for 1.5 h at room temperature. The membranes were scanned and the band densities were quantified using the Odyssey Infrared Imaging System (Li-COR Biosciences, USA).
Cytokine and CYP450 immunological assay
The levels of TNF-α, IL-6, and IL-1β in BALF were measured using rat ELISA kit from the R&D Company, USA, and the level of CYP450s was detected using rat ELISA kit from the Beijing Fangcheng Biochemistry, China, according to the manufacturer’s instructions.
Measurement of SOD, MDA, iNOS, NO, and GST
Lung proteins were extracted with protein extraction kit (Beyotime, Shanghai, China) according to the manufacturer’s instructions. The levels of SOD, MDA, iNOS, NO, and GST in lung tissues were measured using the corresponding kits from the Nanjing Jiancheng Biochemistry, China, according to the manufacturer’s protocols.
Statistical analysis
Statistical analyses were performed by the use of one-way analysis of variance (ANOVA) using the SPSS 19.0 package of programs for Windows. Post hoc tests were conducted to determine the difference between groups, followed by Fisher’s least significant difference (LSD) test. A level of P < 0.05 was accepted as statistically significant.
Results
Histopathological observation
Representative H&E staining images were shown in Fig. 1a–d. No histopathological abnormalities were observed in control (Fig. 1a) and 0.375 mg/kg body weight (b.w.) PM2.5 group animals (data not shown). In 1.5 mg/kg b.w. PM2.5 group, the inflammatory cells existed in the lungs (Fig. 1b). In 6.0 mg/kg b.w. PM2.5 group, the inflammatory cell infiltration, thickened alveolar walls, diminished alveolar spaces, and hyperemia were found in the lungs (Fig. 1c). Exposure to 24.0 mg/kg b.w. PM2.5 induced the more pathological changes compared to that of other treatment groups, accompanied by the bronchial epithelial hyperplasia (Fig. 1d). It was suggested that PM2.5 induced rat lung pathological damage and inflammatory responses.
HE staining results in the lungs of rats from control (a), 1.5 mg/kg b.w. (b), 6.0 mg/kg b.w. (c), and 24.0 mg/kg b.w. (d) group, ×400 magnification. The white, red, blue, yellow, and green arrows indicate sites of inflammatory cell infiltration, hyperemia, alveolar space diminishment, tissue density changes, and bronchial epithelial hyperplasia, respectively. The control group was instilled with same amount of physiological saline
Inflammatory cell counts in BALF
The numbers of total cells, alveolar macrophages (AMs), and neutrophils (NEUs) in BALF exposed to PM2.5 at the doses of 1.5, 6.0, and 24.0 mg/kg b.w. were significantly increased compared with the control (P < 0.01), whereas the number changes of total cells and inflammatory cells in 0.375 mg/kg b.w. PM2.5 group was not significant relative to the control (Fig. 2a). The counts of lymphocytes (LYMs) were significantly increased only in the 24.0-mg/kg b.w. group (P < 0.01), versus the control. Furthermore, the percentages of AM and NEU cell numbers in the total cell numbers exposed to PM2.5 at the doses of 1.5, 6.0, and 24.0 mg/kg b.w. were markedly elevated compared with the control (P < 0.01), whereas the percentages of LYM cell numbers in the total cell numbers in the all treatment group were significantly changed relative to the control.
Effects of PM2.5 on expression of inflammatory markers in lungs of rats
Figure 3 displays the gene expression of four proinflammatory cytokines (TNF-α, IL-1β, IL-6, and ICAM-1) in the lungs of different group rats. The mRNA and protein levels of TNF-α, IL-1β, IL-6, and ICAM-1 showed an obvious increase in response to the higher dose exposure to PM2.5 (6.0 and 24.0 mg/kg b.w) compared to the control (P < 0.05 or P < 0.01). Also, TNF-α and IL-6 mRNA expression as well as TNF-α protein levels were significantly increased at the 1.5-mg/kg b.w. PM2.5 group compared with the control. No significant changes of the TNF-α, IL-1β, IL-6, and ICAM-1 were observed in the rats exposed to PM2.5 at the concentration of 0.375 mg/kg b.w. compared to that in the control.
Expression of mRNA of TNF-α, IL-1β, and IL-6 in rat lungs treated with different PM2.5 concentrations (a); TNF-α, IL-1β, and IL-6 protein levels in rat lungs treated with different PM2.5 concentrations (b); and ICAM-1 mRNA and protein expression in rat lungs treated with different PM2.5 concentrations. For a and b, mean expression of mRNA in each treated group is shown as an increase compared to mean expression in control group which has been ascribed an arbitrary value of 1. The values are mean ± SD from five individual samples. Using one-way ANOVA, comparing with control group, significant difference is indicated by *P < 0.05 and **P < 0.01
Effects of PM2.5 on expression of c-fos and c-jun in lungs of rats
In Fig. 4, PM2.5 at the concentrations of 1.5, 6.0, and 24.0 mg/kg b.w. significantly induced mRNA expression of c-fos and c-jun (P < 0.05 or P < 0.01), while PM2.5 at the concentrations of 6.0 and 24.0 mg/kg b.w. significantly increased protein expression of c-fos and c-jun (P < 0.05; at 6.0 mg/kg b.w., 1.60-fold of control for c-fos, 1.83-fold of control for c-jun; 24.0 mg/kg b.w., 2.13-fold of control for c-fos, 2.09-fold of control for c-jun) in the rat lungs compared with the control.
Expression of mRNA and protein of c-fos and c-jun in lungs of rats treated with different concentrations of PM2.5. Mean expression in each treated group is shown as increase compared to mean expression in control group which has been ascribed an arbitrary value of 1. The values are means ± SD from five individual samples. Using one-way ANOVA, comparing with control group, significant difference is indicated by *P < 0.05 and **P < 0.01
Effects of PM2.5 on CYP450 and GST activity in rat lungs
As shown in Fig. 5, PM2.5 at the doses of 1.5, 6.0 and 24.0 mg/kg b.w. significantly increased the levels of CYP450 and GST in the lungs of rats compared with the control group (P < 0.05 or P < 0.01). The increases of CYP450 and GST activity in the presence of PM2.5 (0.375 mg/kg b.w.) were not statistically significant versus the control.
Activities of CYP450s and GSTs in rat lungs treated with different PM2.5 concentrations. The control group was instilled with same amount of physiological saline. The values are mean ± SD from five individual samples. Using one-way ANOVA, comparing with control group, significant difference is indicated by *P < 0.05 and **P < 0.01
Effects of PM2.5 on markers of oxidative stress in rat lungs
As shown in Fig. 6, PM2.5 at the doses of 1.5, 6.0, and 24.0 mg/kg b.w. significantly increased the levels of iNOS, NO, and MDA in the lungs of rats compared with the control group (P < 0.05 or P < 0.01). The higher dose of PM2.5 (6.0 and 24.0 mg/kg b.w.) markedly inhibited the SOD activities relative to the control (P < 0.05). The level changes of SOD, iNOS, NO, and MDA in the presence of PM2.5 (0.375 mg/kg b.w.) were not statistically significant compared with the control group.
Activities of SOD and iNOS as well as levels of MDA and NO in rat lungs treated with different PM2.5 concentrations. The control group was instilled with the same amount of physiological saline, and the other special control group (vehicle group) was treated with same amount of suspension from extracts of “blank” filter. The values are mean ± SD from five individual samples. Using one-way ANOVA, comparing with control group, significant difference is indicated by *P < 0.05 and **P < 0.01
Discussion
Epidemiological studies show that PM2.5 exposure positively correlates with increased incidence of respiratory diseases, such as pneumonia, asthma, chronic obstructive pulmonary disease (COPD), and lung cancer (Vinikoor-Imler et al. 2011; Li et al. 2013; Tsai et al. 2014). Short-term exposure to PM2.5 has been repeatedly associated with evidence of acute airway inflammation (i.e., fractional exhaled nitric oxide increase) and decreased forced expiratory volume in 1 s (FEV1) in human studies (Strak et al. 2012). In one study, Turner et al. (2011) reported that each 10-mg/cm3 elevation in PM2.5 concentration was associated with a 15–27 % increase in lung cancer mortality. Notably, urban airborne PM2.5 contains many kinds of harmful organic pollutants. Among them, PM2.5-bound PAHs were reported to pose a potential lung cancer risk. For example, Xia et al. (2013) reported the median values of incremental lifetime cancer risk (ILCR) induced by whole year inhalation exposure to both gas and particulate phase PAHs for all population groups in Taiyuan, China were basically larger than the risk limit of 10−6, and our study showed that the individual carcinogenicity index of PM2.5-bound PAHs exceeded the unit risk of 10−5 (Li et al. 2014). However, so far, the detailed mechanisms of PM2.5 on lung injury, inflammatory responses, and potential carcinogenic properties remain unclear. Hence, in this study, we investigated the histopathological alterations, inflammatory responses, oxidative stress, changes of metabolic enzyme activity, and proto-oncogene expression in the lungs of rats exposed to PM2.5 collected from Taiyuan, China.
The lung is a prime target for a wide variety of air-borne particles. The histopathological alterations and inflammatory responses in the lungs exposed to PM2.5 were observed first. To our knowledge, inflammation is a key host defense response to cellular and tissue injury. However, excessive or persistent inflammation can contribute to the pathogenesis of disease. The previous studies found that macrophages phagocytosed silica particles, produced many inflammatory mediators and chemokines, and enhanced the permeability of the alveolar capillary barrier, which can make for NEUs to enter the alveolar space from blood vessel (Liu et al. 2003). NEUs, further, may enlarge inflammatory cascades through releasing more pro-inflammatory factors such as TNF-α, IL-1β, IL-6, and ICAM-1, recruiting AMs, NEUs, and LYMs into alveolar space and increasing the total numbers of the inflammatory cells and the numbers of AMs, NEUs, and LYMs in BALF (Dimatto et al. 1996). Besides, the inflammatory cells including AMs, NEUs, and LYMs played an important role in the early phase inflammatory reaction, and the counts of AMs, NEUs, and LYMs were elevated in BALF of rats exposed to silica dust in a dose-dependent manner (Last et al. 1986; Qu et al. 2012). The increases of the inflammatory cells and the levels of pro-inflammatory cytokines, eventually, may aggravate inflammation and cause lung damage. The literatures showed that PM2.5 exposure (8 mg/rat) elevated the total cell and NEU levels in the BALF compared with the control (Luo et al. 2014), and PM2.5 instillation (0.2, 0.8 and 3.2 mg/rat) caused dose-trend increase in TNF-α and IL-6 in the BALF compared to the control (Wang et al. 2015). From the HE experimental results in Fig. 1, the inflammatory cell infiltration and hyperemia in lungs of rats exposed to higher PM2.5 doses. Also, the numbers of total cells, AMs, NEU, and LYMs as well as the percentages of AMs and NEUs in the total cells were markedly increased in BALF of rats in the presence of 1.5, 6.0, and 24.0 mg/kg b.w. PM2.5 compared to the control. The results showed the same findings as the above reports and suggested that the stimulation of PM2.5 induced inflammatory reaction of the lung and increased the numbers of AMs, NEUs, and LYMs, and these may lead to acute lung injury. Since the change of percentage of LYMs in the total cells was not significant relative to the control, it is proposed that LYMs might make a little contribution to pulmonary inflammatory damage under current conditions of PM2.5 exposure compared with AMs and NEUs. To investigate whether the lung injury induced by PM2.5 was in relation with the increased inflammatory activity, we measured expression of the pro-inflammatory cytokines, such as TNF-α, IL-6, IL-1β, and ICAM-1, which are known to be elevated in BALF of lung disease patients (Yong et al. 1997; Singh et al. 2015). Dagher et al. (2005) reported that exposure to PM2.5 induced significant increases (in a concentration- and time-dependent manner) in protein secretion and/or gene expression of inflammatory cytokines including TNF-α, IL-6, and IL-1β in cultured human epithelial lung cells (L132). Brucker et al. (2013) pointed out that TNF-α, IL-6, and IL-1β levels in serum of the taxi drivers exposed to PM2.5 with average mass concentrations of 12.4 ± 6.9 μg/m3. Moreover, ICAM-1 is a major adhesion molecule to induce the inflammatory cell infiltrate to bronchial epithelial cells in the lung and participates in establishing and maintaining inflammation (Wegner et al. 1990). Wang et al. (2015) reported that PM2.5 increased mRNA expression of ICAM-1 in lungs and the levels TNF-α and IL-6 in BALF of rats, leading to inflammatory changes and pathological characters in rat lungs. Combining with our data of the inflammatory cells and pro-inflammatory cytokine measurement (see Figs. 1, 2, and 3), it was implied that PM2.5 elevated inflammatory cell numbers in BALF and increased the levels of TNF-α, IL-6, IL-1β, and ICAM-1 in the lungs of rat, inducing inflammatory cell infiltration and inflammatory reactions.
In the current study, the PM2.5 samples were collected during the heating season from a representative of the coal combustion polluted city, Taiyuan, and the daily mean mass concentration of PM2.5 had reached high pollution levels (161 μg/m3; Li et al. 2014). Besides, the benzo(a)pyrene equivalent (BaPeq) concentration of total PAHs in PM2.5 was 28.6 ng/m3, higher than the risk limit (10 ng/m3), and the individual carcinogenic index of total PAHs was 3.14 × 10−5, exceeding the recommendation (10−5), suggesting the urban PAHs in PM2.5 pose a potential lung cancer risk in Taiyuan. Hence, we specifically focused on the effects of PM2.5 on proto-oncogene expression and metabolic enzyme activity in rat lungs. Some studies indicated that PM2.5 had a positive relationship with lung cancer incidence and mortality (Vinikoor-Imler et al. 2011; Li et al. 2013). Occupational exposure to PAHs was associated with a risk of lung cancer (Armstrong et al. 2004), while PM2.5-bound PAHs have a potential cancer risk (Xia et al. 2013). As we know, overexpression of proto-oncogene c-fos and c-jun plays an important role in proliferation, and they are possible end points of exposure to reactive metabolites in lung (Janssen et al. 1997). They may encode the activator protein (AP)-1 transcription complex, while the activation of AP-1 may mediate inflammation and contribute to the highly malignant transformation in lung cancer (Ichiki et al. 2000; Zenz et al. 2008). As for the present study, the c-fos and c-jun mRNA and protein levels were increased in lungs of rats exposed to PM2.5 with higher concentrations (1.5, 6.0, and 24.0 mg/kg b.w., see Fig. 4), which implied that PM2.5, especially including PAHs in PM2.5, might promote cell proliferation, increasing the potential risk of lung cancer. On the other hand, in the metabolic activation of PAHs, they are initially catalyzed by CYP450s in the phase I metabolic reactions (Shimada and Fujii-Kuriyama 2004), and then the products from phase I reaction can be detoxified by phase II enzymes such as GSTs (Ketterer and Mulder 1990). CYP450 enzymes are central to the metabolic activation of PAHs to epoxide intermediates, which are converted with the aid of epoxide hydrolase to the ultimate carcinogenic metabolites, diol-epoxides (Shimada and Fujii-Kuriyama 2004), suggesting that activation of CYP450s may accumulate more harmful metabolites in the presence of PAHs. GSTs may take the metabolites from phase I and further metabolizes them by catalyzing the conjugation of the tripeptide glutathione with the xenobiotics such as PAHs in the phase II of the biotransformation process promoting its elimination from the organism (Nakamura et al. 2003). To some extent, they may counteract the potential toxicity of PAHs by its role in PAH detoxification (Kabler et al. 2009). A high level of activity of GSTs might be an adaptation or regulation to detoxify the excess of harmful metabolites from phase I reaction. In the present study, PM2.5 at the doses of 1.5, 6.0, and 24.0 mg/kg b.w. particles markedly increased the activities of CYP450s and GSTs in rat lung (see Fig. 5), thus modifying the lung toxication/detoxication potential and promoting the toxicity induced by PM2.5 or PM2.5-bound PAHs. Abbas et al. (2009) demonstrated that PAH-coated onto PM2.5 induced the gene expression of CYP1A1, CYP2E1, GST-pi1, and/or GST-mu3 in cultured human alveolar macrophage cells, while Chan et al. (2013) reported ultrafine premixed flame particle induced expression of certain isozymes in the cytochrome P-450 superfamily, such as CYP1A1 and CYP1B1, in rat lungs, which indirectly support our results.
We also paid attention to the relationships between lung injury and oxidative stress. ROS include a wide variety of molecules and free radicals derived from molecular oxygen, such as superoxide (O2 .−), hydroxyl radical (.OH), hydrogen peroxide (H2O2), etc. RNS mainly include NO and peroxynitrite (Snyder and Bredt 1999), which is a very powerful oxidant (Virág et al. 2003). Oxidative stress is an expression used to describe various deleterious processes resulting from an imbalance between the formation and elimination of ROS and/or RNS by antioxidant defenses. Overproduction ROS or RNS can damage to cellular components and biomolecules, including DNA, enzymes, and lipids, inducing oxidative/nitrosative stress and cell dysfunction, which have been suggested to be involved in the etiology of several chronic diseases including cancer and aging (Poljšak and Fink 2014). ROS and RNS can result from exposure to environmental pollutants, such as PM2.5 and PAHs (Sagai et al. 1993; Dellinger et al. 2001; Briedé et al. 2004; Chauhan et al. 2004; Gehling et al. 2014). Under stress conditions, activities of anti-oxidative enzymes such as SOD may be inhibited, whereas excessive ROS are easy to attack the cell membrane and form MDA, which is a typical product of lipid peroxidation (LPO). Also, excessive NO regulated by iNOS may form a more toxic peroxynitrite anion (Snyder and Bredt 1999), causing oxidative damage and cytotoxicity (Virág et al. 2003). The SOD activity decrease and MDA, iNOS, and NO level increase in this study (see Fig. 6) suggest that PM2.5 may trigger oxidative stress via the accumulation of ROS and RNS, which may be suggested as an important mechanism of PM2.5-mediated lung injury. Except SOD, GST plays a key role in conjugating GSH to the products of endogenous LPO and inactivating organic hydroperoxides, thus protecting the cell from the severe effects of oxidative stress as an important enzyme for quenching and detoxifying ROS (Sharma et al. 2004). A high level of GSTs induced by PM2.5 in this study implied the antioxidative ability of the organism. Luo et al. (2014) revealed that PM2.5 exposure (8 mg/rat) increased MDA levels and reduced SOD and glutathione peroxidase activity in BALF of Wistar rats, consistent with the results obtained in this study. What is more, on the other hand, the generation of ROS/RNS in turn may provoke inflammatory responses and induce the release of proinflammatory cytokines and chemokines, leading to inflammation and lung injury. During inflammation, enhanced ROS/RNS production may induce recurring DNA damage, inhibition of apoptosis, and activation of proto-oncogenes by initiating signal transduction pathways (Azad et al. 2008). Accordingly, the role of ROS/RNS in lung inflammation and carcinogenesis should be highlighted.
Summary
The results in this study demonstrated that (1) the lung inflammatory injury was induced by the exposure to PM2.5, accompanied by inflammatory cell infiltration and increase of inflammatory cell numbers and pro-inflammatory cytokine levels; (2) the mRNA and protein expression of c-fos and c-jun were raised in the lungs of rats exposed to PM2.5 along with the activation of CYP450s and GSTs; and (3) PM2.5-caused pathological injury had relations with oxidative stress via inhibiting SOD activity and elevating activity of iNOS and levels of MDA and NO. These data suggest that PM2.5-induced inflammatory responses and proto-oncogene high expression in lungs of rats are mediated, in part, by both ROS- and NO-mediated pathways and activation of the metabolic enzymes, which may be one of the important mechanisms by which PM2.5 pollution aggravates respiratory disease.
References
Abbas I, Saint-Georges F, Billet S, Verdin A, Mulliez P, Shirali P, Garçon G (2009) Air pollution particulate matter (PM2.5)-induced gene expression of volatile organic compound and/or polycyclic aromatic hydrocarbon-metabolizing enzymes in an in vitro coculture lung model. Toxicol In Vitro 23(1):37–46
Ada AO, Yilmazer M, Suzen S, Demiroglu C, Demirbag AE, Efe S, Alemdar Y, Burgaz S, Iscan M (2007) Cytochrome P450 (CYP) and glutathione S-transferases (GST) polymorphisms (CYP1A1, CYP1B1, GSTM1, GSTP1 and GSTT1) and urinary levels of 1-hydroxypyrene in Turkish coke oven workers. Genet Mol Biol 30(3):511–519
Armstrong B, Hutchinson E, Unwin J, Fletcher T (2004) Lung cancer risk after exposure to polycyclic aromatic hydrocarbons: a review and meta-analysis. Environ Health Perspect 112:970–978
Azad N, Rojanasakul Y, Vallyathan V (2008) Inflammation and lung cancer: roles of reactive oxygen/nitrogen species. J Toxicol Environ Health B Crit Rev 11(1):1–15
Bonetta S, Gianotti V, Bonetta S, Gosetti F, Oddone M, Gennaro MC, Carraro E (2009) DNA damage in A549 cells exposed to different extracts of PM2.5 from industrial, urban and highway sites. Chemosphere 77(7):1030–1034
Briedé JJ, Godschalk RW, Emans MT, De Kok TM, Van Agen E, Van Maanen J, Van Schooten FJ, Kleinjans JC (2004) In vitro and in vivo studies on oxygen free radical and DNA adduct formation in rat lung and liver during benzo[a]pyrene metabolism. Free Radic Res 38:995–1002
Brucker N, Moro AM, Charão MF, Durgante J, Freitas F, Baierle M, Nascimento S, Gauer B, Bulcão RP, Bubols GB, Ferrari PD, Thiesen FV, Gioda A, Duarte MM, de Castro I, Saldiva PH, Garcia SC (2013) Biomarkers of occupational exposure to air pollution, inflammation and oxidative damage in taxi drivers. Sci Total Environ 463–464:884–893
Cao L, Geng H, Yao C, Zhao L, Duan P, Xuan Y, Li H (2014) Investigation of chemical compositions of atmospheric fine particles during a wintertime haze episode in Taiyuan City. China Environ Sci 34:259–265
Chan JK, Vogel CF, Baek J, Kodani SD, Uppal RS, Bein KJ, Anderson DS, Van Winkle LS (2013) Combustion derived ultrafine particles induce cytochrome P-450 expression in specific lung compartments in the developing neonatal and adult rat. Am J Physiol Lung Cell Mol Physiol 304(10):L665–L677
Chauhan V, Breznan D, Goegan P, Nadeau D, Karthikeyan S, Brook JR, Vincent R (2004) Effects of ambient air particles on nitric oxide production in macrophage cell lines. Cell Biol Toxicol 20(4):221–239
Dagher Z, Garçon G, Gosset P, Ledoux F, Surpateanu G, Courcot D, Aboukais A, Puskaric E, Shirali P (2005) Pro-inflammatory effects of Dunkerque city air pollution particulate matter 2.5 in human epithelial lung cells (L132) in culture. J Appl Toxicol 25(2):166–175
Dellinger B, Pryor WA, Cueto R, Squadrito GL, Hegde V, Deutsch WA (2001) Role of free radicals in the toxicity of airborne fine particulate matter. Chem Res Toxicol 14:1371–1377
Dimatto M, Antonini JM, Van Dyke K, Reasor MJ (1996) Characteristics of the acute-phase pulmonary response to silica in rats. J Toxicol Environ Health 47(1):93–108
Gehling WM, Khachatryan L, Dellinger B (2014) Hydroxyl radical generation from environmentally persistent free radicals (EPFRs) in PM2.5. Environ Sci Technol 48(8):4266–4272
Gutiérrez-Castillo ME, Roubicek DA, Cebrián-García ME, De Vizcaya-Ruíz A, Sordo-Cedeño M, Ostrosky-Wegman P (2006) Effect of chemical composition on the induction of DNA damage by urban airborne particulate matter. Environ Mol Mutagen 47(3):199–211
Ichiki K, Mitani N, Doki Y, Hara H, Misaki T, Saiki I (2000) Regulation of activator protein-1 activity in the mediastinal lymph node metastasis of lung cancer. Clin Exp Metastasis 18:539–545
Janssen YM, Matalon S, Mossman BT (1997) Differential induction of c-fos, c-jun, and apoptosis in lung epithelial cells exposed to ROS or RNS. Am J Physiol 273(4 Pt 1):L789–L796
Kabler SL, Seidel A, Jacob J, Doehmer J, Morrow CS, Townsend AJ (2009) Differential protection by human glutathione S-transferase P1 against cytotoxicity of benzo[a]pyrene, dibenzo[a, l]pyrene, or their dihydrodiol metabolites, in bi-transgenic cell lines that co-express rat versus human cytochrome P4501A1. Chem Biol Interact 179:240–246
Ketterer B, Mulder GJ (1990) Glutathione conjugation. In: Mulder GJ (ed) Conjugation reactions in drug metabolism. Taylor and Francis, London, pp 307–364
Last JA, Reiser KM, Ciba FS (1986) Effects of silica on lung collagen. Ciba Found Symp 121:180–193
Li P, Xin J, Wang Y, Wang S, Li G, Pan X, Liu Z, Wang L (2013) The acute effects of fine particles on respiratory mortality and morbidity in Beijing, 2004–2009. Environ Sci Pollut Res Int 20(9):6433–6444
Li R, Kou X, Geng H, Dong C, Cai Z (2014) Pollution characteristics of ambient PM2.5-bound PAHs and NPAHs during winter time in Taiyuan. Chin Chem Lett 25:663–666
Li R, Kou X, Geng H, Xie J, Yang Z, Zhang Y, Cai Z, Dong C (2015) Effect of ambient PM2.5 on lung mitochondrial damage and fusion/fission gene expression in rats. Chem Res Toxicol 28(3):408–418
Liu Y, Du HK, Gao MJ, Chang AH (2003) The relationship between pathology of lung and change of inflammatory cells in bronchoalveolar lavage fluid in rats exposed to silica early. Acta Acad Med CPAPF 12(5):332–335
Luo B, Shi H, Wang L, Shi Y, Wang C, Yang J, Wan Y, Niu J (2014) Rat lung response to PM2.5 exposure under different cold stresses. Int J Environ Res Public Health 11(12):12915–12926
Nakamura Y, Miyamoto M, Murakami A, Ohigashi H, Osawa T, Uchida KA (2003) Phase II detoxification enzyme inducer from lemongrass: identification of citral and involvement of electrophilic reaction in the enzyme induction. Biochem Biophys Res Commun 302:593–600
Oh SM, Kim HR, Park YJ, Lee SY, Chung KH (2011) Organic extracts of urban air pollution particulate matter (PM2.5)-induced genotoxicity and oxidative stress in human lung bronchial epithelial cells (BEAS-2B cells). Mutat Res 723(2):142–151
Poljšak B, Fink R (2014) The protective role of antioxidants in the defence against ROS/RNS-mediated environmental pollution. Oxidative Med Cell Longev 2014:671539
Qu J, Wang R, Zhou XB, Zhang W, Zhang HD, Liu HJ (2012) Study on changes of inflammatory cells in BALF of rats exposed to silica dust. Prev Med Tribune 18(1):1–4
Rosanna DP, Salvatore C (2012) Reactive oxygen species, inflammation, and lung diseases. Curr Pharm Des 18(26):3889–3900
Sagai M, Saito H, Ichinose T, Kodama M, Mori Y (1993) Biological effects of diesel exhaust particles. I. In vitro production of superoxide and in vivo toxicity in mouse. Free Radic Biol Med 14:37–47
Sharma A, Sharma JK, Murthy NS, Mitra AB (2004) Polymorphisms at GSTM1 and GSTT1 gene loci and susceptibility to cervical cancer in Indian population. Neoplasma 51(1):12–16
Shi GL, Zhou XY, Jiang SY, Tian YZ, Liu GR, Feng YC, Chen G, Liang-Yang KX (2015) Further insights into the composition, source and toxicity of PAHs in size-resolved PM in a megacity in China. Environ Toxicol Chem 34(3):480–487
Shimada T, Fujii-Kuriyama Y (2004) Metabolic activation of polycyclic aromatic hydrocarbons to carcinogens by cytochromes P450 1A1 and 1B1. Cancer Sci 95(1):1–6
Singh S, Grover V, Christie L, Charles P, Kelleher P, Shah PL (2015) A comparative study of bronchoscopic microsample probe versus bronchoalveolar lavage in patients with burns-related inhalational injury, acute lung injury and chronic stable lung disease. Respiration 6:19–26
Snyder S, Bredt HDS (1999) Biological roles of nitric oxide. Sci Am 266:68–71
Spandidos DA (2007) Oncogenes and tumor suppressor genes as paradigms in oncogenesis. J BUON 12(Suppl 1):S9–S12
Strak M, Janssen NA, Godri KJ, Gosens I, Mudway IS, Cassee FR, Lebret E, Kelly FJ, Harrison RM, Brunekreef B, Steenhof M, Hoek G (2012) Respiratory health effects of airborne particulate matter: the role of particle size, composition, and oxidative potential-the RAPTES project. Environ Health Perspect 120:1183–1189
Tsai SS, Chiu HF, Liou SH, Yang CY (2014) Short-term effects of fine particulate air pollution on hospital admissions for respiratory diseases: a case-crossover study in a tropical city. J Toxicol Environ Health A 77(18):1091–1101
Turner MC, Krewski D, Pope CA 3rd, Chen Y, Gapstur SM, Thun MJ (2011) Long-term ambient fine particulate matter air pollution and lung cancer in a large cohort of never-smokers. Am J Respir Crit Care Med 184(12):1374–1381
Vattanasit U, Navasumrit P, Khadka MB, Kanitwithayanun J, Promvijit J, Autrup H, Ruchirawat M (2014) Oxidative DNA damage and inflammatory responses in cultured human cells and in humans exposed to traffic-related particles. Int J Hyg Environ Health 217(1):23–33
Vinikoor-Imler LC, Davis JA, Luben TJ (2011) An ecologic analysis of county-level PM2.5 concentrations and lung cancer incidence and mortality. Int J Environ Res Public Health 8(6):1865–1871
Virág L, Szabó E, Gergely P, Szabó C (2003) Peroxynitrite-induced cytotoxicity: mechanism and opportunities for intervention. Toxicol Lett 140–141:113–124
Wang G, Zhao J, Jiang R, Song W (2015) Rat lung response to ozone and fine particulate matter (PM2.5) exposures. Environ Toxicol 30(3):343–356
Wegner CD, Gundel RH, Reilly P, Haynes N, Letts LG, Rothlein R (1990) Intercellular adhesion molecule-1 (ICAM-1) in the pathogenesis of asthma. Science 247:456–459
Xia Z, Duan X, Tao S, Qiu W, Liu D, Wang Y, Wei S, Wang B, Jiang Q, Lu B, Song Y, Hu X (2013) Pollution level, inhalation exposure and lung cancer risk of ambient atmospheric polycyclic aromatic hydrocarbons (PAHs) in Taiyuan, China. Environ Pollut 173:150–156
Yong CL, Ki TC, Yang KR (1997) Changes of soluble ICAM-1 levels in serum and bronchoalveolar lavage fluid from patients with atopic bronchial asthma after allergen challenge. J Asthma 34(5):405–412
Zenz R, Eferl R, Scheinecker C, Redlich K, Smolen J, Schonthaler HB, Kenner L, Tschachler E, Wagner EF (2008) Activator protein 1 (Fos/Jun) functions in inflammatory bone and skin disease. Arthritis Res Ther 10(1):201
Zhang YX, Tao S, Shen HZ, Ma JM (2009) Inhalation exposure to ambient polycyclic aromatic hydrocarbons and lung cancer risk of Chinese population. Proc Natl Acad Sci U S A 106(50):21063–21067
Acknowledgments
This research was supported by the National Natural Science Foundation of China (No. 21177078), Environmental Protection Public Welfare Research Funds (No. 201309009), Research Project Supported by Shanxi Scholarship Council of China (No. 2013-16), Nature Science Foundation of Shanxi Province in China (No. 2014011036-2), Foundation of Educational Committee of Shanxi Province in China (No. 2014110), and International Science and Technology Collaborative Project of Shanxi Province of China (No. 2012081010).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Responsible editor: Philippe Garrigues
Rights and permissions
About this article
Cite this article
Li, R., Kou, X., Xie, L. et al. Effects of ambient PM2.5 on pathological injury, inflammation, oxidative stress, metabolic enzyme activity, and expression of c-fos and c-jun in lungs of rats. Environ Sci Pollut Res 22, 20167–20176 (2015). https://doi.org/10.1007/s11356-015-5222-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-015-5222-z