Abstract
Background
The purpose of this study was to investigate the long-term mortality rates of patients with obstructive sleep apnea (OSA) who received an overnight polysomnogram (PSG) for obtaining the diagnosis and to determine the relationship between PSG parameters and overall mortality.
Methods
Between 2007 and 2013, patients who had overnight PSG and were diagnosed with OSA were included in the study. Factors which are thought to influence mortality were assessed for 5-year and overall survival using the log rank test and Kaplan-Meier survival curves. Using multivariable Cox regression analysis, a model was constructed for factors influencing 5-year and overall survival.
Results
A total of 762 patients with a mean age of 52.7 (±10.8) and a dominance of men (74.7%) were studied. Gender, OSA severity subgroups, and apnea hypopnea index (AHI) were not statistically significantly associated with either 5-year or overall mortality (p<0.05 for both). Age, having a cardiovascular comorbidity, proportion of rapid eye movement (%REM), and total sleep time with an oxyhemoglobin saturation of less than 90% (T90) all showed a significant correlation with overall all-cause mortality in the model. For 5-year mortality and overall mortality, the hazard ration (HR) for T90 was 3.6 (95% CI (1.6–8.0) p=0.001) and 3 (95% CI (1.6–5.7) p=0.001), respectively.
Conclusion
The study findings suggest that not AHI but PSG parameters of hypoxia, mainly T90, having cardiovascular comorbidity, and %REM sleep were significant risk factors for all-cause mortality in patients with OSA. The association of OSA, hypoxia, and mortality is an area that deserves further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a significant health issue which is recognized as a separate risk factor for mortality and morbidity [1]. Sleep fragmentation and intermittent hypoxia are the hallmarks of the condition. Every system, including the cardiovascular, nervous, respiratory, and endocrine systems, is impacted by OSA. The relative risks of major adverse cardiac events, stroke, and all-cause mortality increase by 2.04, 2.15, and 1.54 respectively, when OSA is untreated [2]. A 1.9-fold elevated risk of all-cause mortality and a 2.65-times increased risk of cardiovascular mortality have both been linked to severe OSA [3]. Aging and comorbidity, such as cardiovascular diseases, chronic kidney disease, and moderate-to-severe chronic obstructive pulmonary disease, have been suggested as significant factors in increased mortality in OSA, in addition to the severity of the disease [4].
The sum of the apnea and hypopnea indexes per hour is used to calculate the apnea hypopnea index (AHI), which is used to categorize the severity of OSA [5]. There is growing evidence that AHI does not accurately estimate the risk of CV diseases, even though AHI is used to diagnose and evaluate the severity of OSA. Hypoxic burden (HB) specific to OSA and heart rate variability have recently been found to be powerful indicators of overall CV morbidity and mortality in OSA [6]. There is evidence that a desaturation rate of 2% is linked to all-cause mortality and a desaturation rate of 4% is related to an increased risk of hypertension [7, 8]. However, not all published studies have consistently shown an association between OSA parameters and all-cause mortality [6]. We therefore hypothesize that in individuals with OSA identified by overnight PSG, AHI is not a reliable indicator of all-cause mortality.
The goal of this study was to look for the 5- to 8-year mortality rates of patients with OSA by overnight PSG and the correlation between PSG parameters and all-cause mortality.
Methods
Study design
In this retrospective cohort study, the demographic characteristics, body mass index (BMI), Epworth score, and polysomnographic findings were collected from the inpatient reports during 2007–2013 in our hospital sleep laboratory. This research study followed the guidelines of the Declaration of Helsinki and was conducted using information obtained for clinical purposes. Our University Hospitals Ethics Committee provided its approval.
Participant characteristics
Patients hospitalized for OSA having overnight PSG during 2007–2013 in our hospital sleep laboratory were considered for inclusion in the study. The hospital archive contains the data of every patient who underwent PSG for one night in our clinic. Patients’ symptoms, family history, associated diseases, and Epworth survey results are noted while they are hospitalized. But if the patient’s file contained missing data, that patient was excluded from the trial. BMI and number of comorbidities were obtained from the medical records. Diagnosis of coronary heart disease and those with cardiovascular disease risk factors like hypertension, diabetes, and dyslipidemia, or their combination, were referred to as cardiovascular (CV) comorbidity. Other rare comorbidities were not included in the analysis. Participants were divided into two groups according to survival (deceased and survived). OSA severity was calculated with AHI score and the severity of OSA was classified as mild, moderate, and severe (5≤ AHI <15, 15≤ AHI <30, AHI ≥30) respectively.
Mortality data of patients with OSA were obtained from the hospital online data system, and these data were also checked over the data of the social insurance institution.
Polysomnography
Using the Epworth sleepiness scale higher than 10, excessive daytime sleepiness was determined [9]. All patients underwent overnight PSG using an Astro-Med Inc. Product Group, Grass Technologies Comet Series EEG/PSG and Grass Technologies Twin software version 4. The overnight PSG included four electroencephalography channels, four tibialis anterior electromyography channels, a finger pulse oximeter, and one chin electromyography channel. A nasal thermistor, a digital microphone to detect snoring, a nasal airflow, strain gauges to detect thoracoabdominal movements, and a single electrocardiography lead were also included in the PSG system. The American Academy of Sleep Medicine’s (AASM) standard criteria were applied to PSG recordings, which were measured for oxygenation, breathing, and sleep in 30-s intervals (epochs) [10]. A 90% cessation of oro-nasal airflow for at least 10 s was considered to be obstructive apnea, while there was chest wall motion. Hypopnea was defined by AASM criteria. The total number of apneas and hypopneas per hour of sleep was used to calculate AHI. PSG findings were used for the diagnosis of OSA, according to guidance of the International Classification of Sleep Disorders 2 [11]. Patients with an AHI <5 were excluded, and the severity of OSA was classified as mild, moderate, and severe (5≤ AHI <15, 15≤ AHI <30, AHI ≥30) respectively.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS, Inc., Chicago IL), version 22 Windows software was used to analyze the data. To ascertain whether the data were normally distributed or not, the Shapiro-Wilk test was applied. The results were presented as mean (±standard deviation) and median (min–max). Mann-Whitney U test and Student t test were used for comparing continues parameters between the groups. To compare categorical data between groups, the chi square and exact tests were used, and the results were presented in number and percentage (%). Cut-off values for the continuous variables affecting mortality in the comparisons between mortality groups were determined by evaluating the AUC and Youden index values using the ROC analysis method. According to these cut-off values, patients were grouped for mortality risk. With these risk groups whose cut-off values were determined, comorbidity, gender, OSA severity, and AHI value groups, which are thought to have an effect on mortality, were evaluated for 5-year survival and overall survival using the log rank test in Kaplan-Meier survival curves. For multivariable modeling, in univariable analysis and in intergroup comparisons, parameters such as age, BMI, comorbidity, REM%, Min O2 Sat, and desaturation time with an alpha value of less than 0.1 were used. This model was then analyzed to determine risk factors for 5-year and overall mortality in multivariable Cox regression analysis. The results were presented with 95% CI. In all statistical analyses, p value of <0.05 was accepted as statistical significance.
Results
After exclusions, 762 patients were enrolled in the study. There was a male dominancy (74.7%) with a mean age of 52.7 (±10.8) in our cohort. Baseline characteristics and polysomnographic results of the participants are shown in Table 1. In this population, mean AHI was 43.4 (±31.5), 5-year survival rate was 91.9%, and 8-year survival rate was 88.2%. When we compared the demographic and clinical characteristics of survived and deceased patients, we found that age, BMI, and having a CV comorbidity were significantly different between two groups (p<0.001, p=0.001, p<0.001 respectively). In addition, PSG parameters %REM, minimum oxygen saturation during sleep, and T90 were significantly different between survived and deceased patients (p<0.001, p<0.001, p<0.001 respectively.) AHI was not statistically significantly different between survived and deceased patients (p=0.99) (Table 2).
In the evaluation of possible risk factors for mortality prediction (in the ROC analysis), age and BMI were statistically significantly associated with 5-year mortality (p<0.001, p=0.002, respectively). Also, %REM, minimum O2 saturation, and T90 during PSG were statistically significantly associated with 5-year mortality (p<0.001, p=0.003, p<0.001 respectively). Likewise, age, BMI, %REM, and minimum O2 saturation, T90 (p<0.001 for all) were significantly correlated with 8-year mortality in patients with OSA. In addition, Epworth score was not correlated with 5-year mortality (p=0.22) but found to be correlated with 8-year mortality (p=0.047). AUC, sensitivity, and specificity of these possible risk factors for mortality prediction are summarized in Table 3.
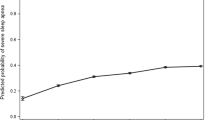
Regarding the factors affecting 5-year survival and overall survival using Kaplan-Meier curves and the log rank test, we found that gender, OSA severity subgroups, and AHI were not statistically significantly related with mortality both 5-year and overall all-cause mortality (Table 4). Age, CV comorbidity, BMI, %REM, and hypoxemic features (T90 and minimum oxygen saturation) were found related both with 5-year and 8-year mortality (Table 4). Patients younger than 58.5 years of age compared to older ones (≥59) (147.3 (95% CI 145.0–149.5) vs 125.6 (95% CI 118.9–132.2), p<0.001) had a longer overall survival. Also, patients with BMI< 34 compared to patients with BMI ≥ 34 (145.1 (95% CI 142.3–147.8) vs 133.8 (95% CI 128.6–139.0), p<0.001) had a longer overall survival. In addition, patients without CV comorbidities compared to patients with CV comorbidities had a longer overall survival (147.9 (95% CI 145.2–150.7) vs 134.4 (95% CI 130.1–138.6), p<0.001) (Table 4 and Figs. 1 and 2). Other factors affecting 5-year and overall mortality are summarized in Figs. 1 and 2. There was no difference in 5-year and overall survival between the OSA severity groups and the AHI groups (Table 4, Figs. 1 and 2).
In our cohort, AHI and OSA severity groups were not correlated with survival; therefore, we did not put these variables into the multivariable Cox regression analysis. In our model, there was a statistically significant association between age (HR 3.6, 95% CI 2–6.5, p<0.001), REM% (HR 1.9, 95% CI 1.1–3.3, p=0.024), and T90 (HR 3.6, 95% CI 1.6–8.0, p=0.001) and 5-year all-cause mortality (Table 5). In our overall mortality model, there was a statistically significant association between age (HR 2.7, 95% CI 1.7–4.2, p<0.001), Cv comorbidity (HR 2.6, 95% CI 1.4–4.5, p=0.001), REM% (HR 1.7, 95% CI 1.1–2.7, p=0.019), and T90 (HR 3, 95% CI 1.6–5.7, p=0.001) and overall all-cause mortality (Table 5). HR for total sleep time with oxyhemoglobin saturation below 90% under PSG was 3.6 (95% CI 1.6–8.0) for 5-year mortality and 3 (95% CI 1.6–5.7) for overall mortality (Table 5).
Discussion
In our study, we examined the factors affecting 5–8-year mortality in patients with OSA. The findings suggest that having a CV comorbidity, T90%, and %REM sleep were associated with mortality in patients with OSA.
Previous research has linked OSA to an increased risk of death from any cause. In a metanalysis done by Pan et al., it was shown that patients with OSA had a significantly higher risk of death from any cause [12]. They included twelve prospective cohort studies involving 34,382 participants and showed OSA is a separate risk factor for all-cause mortality. The main contributing factors of the link between OSA risk and all-cause mortality are not clearly identified. The relationship can be explained by some pathophysiological mechanisms associated with OSA. OSA may cause intermittent hypoxia with sleep fragmentation, fluid redistribution, swings in negative intrathoracic pressure, alterations in sympathetic activity, and increased systemic inflammation, Also aging, having more comorbidities and obesity may play a role in the mechanisms underlying mortality risk. All these components may foster multi-organ damage and may cause patient death [12].
Long-term mortality is affected by many factors like age, gender, and obesity. There are different results in the literature regarding gender and OSA mortality. Female patients with OSA had a lower mortality than males in some studies. However, in Labarca’s study, gender did not influence all-cause, cardiovascular, or cancer mortality [13, 14]. We believe that aging increases OSA mortality, although different results have been obtained in different studies. Patients with severe hypoxemic OSA were statistically significantly older compared to patients with mild hypoxemic OSA [14, 15]. Age turned out to be a significant risk factor affecting mortality in this study, as was expected. Another significant risk factor for the development of OSA and the progression of diseases is obesity. Theoretically, a higher BMI could worsen OSA and raise mortality. However, there is still disagreement regarding how obesity affects all-cause mortality based on BMI [12]. In this study, although BMI was considered a potential risk factor, it was not found to affect all-cause mortality in the multivariable regression analysis model.
In most of the previous studies, AHI was used as the indicator of the severity of sleep apnea [16,17,18]. In this study, T90, not AHI, was shown to be an independent risk factor for OSA all-cause mortality. He and colleagues analyzed mortality and the severity of OSA using only the apnea index. They discovered that an apnea index of 20 was linked to a higher mortality rate in patients under 50 but was less clearly linked to a higher mortality rate in patients over 50 [19]. This may be because younger patients typically have fewer complicating medical conditions, making it simpler to detect the comparatively lower association between OSA severity and all-cause mortality. The significance of the AHI in the categorization of OSA severity has been questioned in light of new data on etiology, epidemiology, and prognosis. A multicomponent grading system decision, the Baveno classification, incorporating symptoms and comorbidities was recently presented to define OSA and direct treatment options [20]. Because it integrates patient-related symptoms on the one hand and prognostic factors on the other, compared to the traditional OSA classification based on AHI, the Baveno classification method is probably preferable. According to Baveno groups, percentage of sleep time with T90 and mean oxygen saturation were statistically significantly different between groups. Additionally, Azarbarzin et al.’s study demonstrated that patients with OSA who present an increased heart rate response are more susceptible to experiencing cardiovascular morbidity and mortality [21]. Trzepizur et al. demonstrated that patients with OSA who have a high level of OSA-specific hypoxic burden are more likely to develop a cardiovascular event and have a high overall mortality rate [6]. Labarca et al. included 889 patients in the analysis describing four clinical phenotypes of patients with moderate to severe OSA and concluded that in addition to the AHI, oximetric parameters are useful for describing a different phenotype that has a high risk of mortality [14]. Over the past 3 years, hypoxic burden (HB) has shown promise across these metrics in both community and clinical populations. HB consistently enhanced risk prediction for cardiovascular events, compared to conventional measures of OSA severity [22]. Long-term prospective studies are needed to predict which hypoxemic parameter can better determine mortality and OSA severity, and to understand its effect with comorbidities.
It is clearly known that OSA is linked to a variety of disorders and in comparison, to patients without comorbidities, patients with OSA and any comorbidity may have a higher risk of death. In a large-scale cohort study, it was revealed that the most predominant cause of death was cardiovascular events, followed by infection and cancer [23]. It is obvious that the best-defined health outcomes of OSA relate to the cardiovascular system. Hypertension, arrhythmias, cerebrovascular events, cardiac failure, and coronary artery disease have a strong association with OSA. Patients with these comorbidities should be evaluated for the possibility of OSA, especially if they exhibit the recognizable symptoms and physical exam findings of OSA. The treatment of OSA also contributes to the treatment of concomitant diseases [24]. The diagnosis and treatment of OSA are an important point in the context of the relationship between comorbid diseases and mortality.
REM sleep has drawn attention in terms of its relationship with increased sympathetic activity and cardiovascular instability in healthy people compared to non-rapid eye movement (NREM) sleep, and this association is even stronger in patients with OSA. Contrary to NREM sleep, significant changes to the autonomic nervous system and the cardiorespiratory system take place during REM sleep. All evidence points to the possibility that REM sleep-related OSA may have more negative cardiometabolic effects than non-REM sleep [25]. Although the patients in this study were not classified as REM-related OSA, it can be suggested that patients with OSA and low REM% may have higher mortality due to the pathophysiological process described above. In this study, %REM was associated with long-term mortality but not with 5-year mortality. Although not enough studies have been done to support this, lower %REM during sleep may be a metric indicating that the REM sleep cycle may have an impact on longer-term mortality.
There are limitations to the current study. This is a single-center retrospective cohort study and may not represent the whole population of patients with OSA. Our center is one of the biggest sleep centers in the region and works as a referee center. Therefore, we may represent more severe patients and this knowledge cannot be generalized to patients with mild OSA. Despite the study’s large sample size and extensive follow-up period, there may still be several confounding factors that affect mortality, such as the effect of treatment on mortality results, which this study was unable to demonstrate due to the challenges and unpredictability in gathering PAP adherence data. A strength of this study is that all patients underwent overnight PSG in-hospital settings with direct observation during the night. Therefore, the diagnosis of the patients is certain and documented by objective data.
Conclusion
This study showed a strong correlation between hypoxemic features, having CV comorbidity, %REM sleep, and long-term all-cause mortality in patients with OSA diagnosed by overnight PSG. AHI was not determined to be a risk factor for 5- to 8-year all-cause mortality in individuals with OSA. Additional studies are needed to explain the link between OSA patients’ polysomnographic characteristics and all-cause mortality.
Data availability
The corresponding author will provide the datasets produced and/or analyzed during the current study upon reasonable request.
References
Veasey SC, Rosen IM (2019) Obstructive sleep apnea in adults. N Engl J Med 380(15):1442–1449
Xie C, Zhu R, Tian Y, Wang K (2017) Association of obstructive sleep apnoea with the risk of vascular outcomes and all-cause mortality: a meta-analysis. BMJ Open 7:e013983
Ge X, Han F, Huang Y et al (2013) Is obstructive sleep apnea associated with cardiovascular and all-cause mortality? PLoS One 8:e69432. https://doi.org/10.1371/journal.pone.0069432
Scrutinio D, Guida P, Aliani M, Castellana G, Guido P, Carone M (2021) Age and comorbidities are crucial predictors of mortality in severe obstructive sleep apnoea syndrome. Eur J Intern Med. 90:71–76. https://doi.org/10.1016/j.ejim.2021.04.018
Punjabi NM (2016) Counterpoint: is the apnea-hypopnea in- dex the best way to quantify the severity of sleep-disordered breath- ing? No Chest 149(1):16–19
Trzepizur W, Blanchard M, Ganem T, Balusson F, Feuilloy M, Girault JM, Meslier N, Oger E, Paris A, Pigeanne T, Racineux JL, Sabil A, Gervès-Pinquié C, Gagnadoux F (2022) Sleep apnea-specific hypoxic burden, symptom subtypes, and risk of cardiovascular events and all-cause mortality. Am J RespirCritCareMed 205(1):108–117. https://doi.org/10.1164/rccm.202105-1274OC
Stamatakis K, Sanders MH, Caffo B, Resnick HE, Gottlieb DJ, Mehra R, Punjabi NM (2008) Fasting glycemia in sleep disordered breathing: lowering the threshold on oxyhemoglobin desaturation. Sleep 31(7):1018–1024
Butler MP, Emch JT, Rueschman M, Sands SA, Shea SA, Wellman A, Redline S (2019) Apnea-hypopnea event duration predicts mor- tality in men and women in the Sleep Heart Health Study. Am J Respir Crit Care Med 199(7):903–912
Johns MW (1994) Sleepiness in different situations measured by the Epworth sleepiness scale. Sleep 17:703–710
Iber C, Ancoli-Israel S, Chesson AL, Quan SF (2007) The AASM manual for the scoring of sleep and associated events: rules, termi- nology, and technical specifications. American academy of sleep medicine, Westchester IL, USA
AASM (2005) International classification of sleep disorders: diagnostic and coding manual, 2nd ed. American Academy of Sleep Medicine, Westchester
Pan L, Xie X, Liu D et al (2016) Obstructive sleep apnoea and risks of all-cause mortality: preliminary evidence from prospective cohort studies. Sleep Breath 20:345–353. https://doi.org/10.1007/s11325-015-1295-7
Jennum P, Tønnesen P, Ibsen R, Kjellberg J (2015) All-cause mortality from obstructive sleep apnea in male and female patients with and without continuous positive airway pressure treatment: a registry study with 10 years of follow-up. Nat Sci Sleep. 7:43–50. https://doi.org/10.2147/NSS.S75166
Labarca G, Jorquera J, Dreyse J, Salas C, Letelier F (2021) Hypoxemic features of obstructive sleep apnea and the risk of mortality: a clusteranalysis. Sleep Breath 25(1):95–103. https://doi.org/10.1007/s11325-020-02064-7
Mashaqi S, Gozal D (2020) The impact of obstructive sleep apnea and PAP therapy on all-cause and cardiovascular mortality based on age and gender e a literature review. Respir Investig 58(1):7–20. https://doi.org/10.1016/j.resinv.2019.08.002
Young T, Finn L, Peppard P (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of he Wisconsin sleep cohort. Sleep 31:1071–1078
Marshall N, Wong KKH, Liu PY, Cullen SRJ, Knuiman MW, Grunstein R (2008) Sleep apnea as an independent risk factorforall-causemortality: the Busselton Health Study. Sleep 31:1079–1085
Punjabi NM, Caffo BS, Goodwin JL (2009) Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 6:1–9
He J, Kryger MH, Zorick FJ, Conway W, Roth T (1988) Mortality and apnea index in obstructive sleep apnea. Chest 94:9–14
Randerath WJ, Herkenrath S, Treml M, Grote L, Hedner J, Bonsignore MR, Pépin JL, Ryan S, Schiza S, Verbraecken J, McNicholas WT, Pataka A, Sliwinski P, Basoglu ÖK (2021) Evaluation of a multi component grading system for obstructive sleep apnoea: the Baveno classification. ERJ Open Res 7(1):00928-2020. https://doi.org/10.1183/23120541.00928-2020
Azarbarzin A, Sands SA, Younes M, Taranto-Montemurro L, Sofer T, Vena D, Alex RM, Kim SW, Gottlieb DJ, White DP, Redline S, Wellman A (2021) The sleepapnea-specific pulse-rate response predicts cardiovascular morbidity and mortality. Am J Respir Crit Care Med 203(12):1546–1555. https://doi.org/10.1164/rccm.202010-3900OC
Martinez-Garcia MA, Sánchez-de-la-Torre M, White DP, Azarbarzin A (2022) Hypoxic burden in obstructive sleep apnea: presentand future. Arch Bronconeumol 59(1):36–43. https://doi.org/10.1016/j.arbres.2022.08.009
Chiang CL, Chen YT, Wang KL, Su VY, Wu LA, Perng DW, Chang SC, Chen YM, Chen TJ, Chou KT (2017) Comorbidities and risk of mortality in patients with sleep apnea. Ann Med 49(5):377–383. https://doi.org/10.1080/07853890.2017.1282167
Stansbury RC, Strollo PJ (2015) Clinical manifestations of sleep apnea. J Thorac Dis 7(9):E298–E310. https://doi.org/10.3978/j.issn.2072-1439.2015.09.13
Alzoubaidi M, Mokhlesi B (2016) Obstructive sleep apnea during rapid eye movement sleep: clinical relevance and therapeutic implications. Curr Opin Pulm Med 22(6):545–554. https://doi.org/10.1097/MCP.0000000000000319
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The Suat Seren Chest Diseases and Surgery Education and Training Hospital’s institutional and national research committees, as well as the 1964 Helsinki Declaration and its later amendments or comparable ethical standards, were all followed when conducting studies involving human subjects. Formal consent is not required because the demographic data, BMI, Epworth score, and polysomnographic results were obtained from inpatient reports that were analyzed retrospectively. The article contains no information that could be used to identify any participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Varol, Y., Uçar, Z.Z., Oktay Arslan, B. et al. Apnea-hypopnea index and the polysomnographic risk factors for predicting 5- to 8-year mortality in patients with OSA. Sleep Breath 28, 103–112 (2024). https://doi.org/10.1007/s11325-023-02868-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02868-3