Abstract
Purpose
Screening commercial drivers (CDs) for obstructive sleep apnea (OSA) reduces the risk of motor vehicle accidents. We evaluated the accuracy of standard OSA questionnaires in a cohort of CDs.
Study design and methods
We enrolled consecutive male CDs at 10 discrete transportation companies during their yearly scheduled occupational health visit. The CDs had their anthropometric measures taken; completed the Berlin, STOP, STOP-BANG, OSAS-TTI, SACS, EUROSAS, and ARES questionnaires; and underwent a home sleep apnea test (HSAT) for the determination of their respiratory events index (REI). We assessed the questionnaires’ ability to predict OSA (REI ≥ 5 events/h) and moderate-to-severe OSA (REI ≥ 15 events/h).
Results
Among 315 CDs recruited, 243 (77%) completed the study protocol, while 72 subjects were excluded for inadequate HSAT quality. The demographics and clinical data were comparable in both the included and excluded subjects. The included CDs had a median age of 50 years (interquartile range (IQR) 25–70) and a mean body mass index of 27 ± 4 kg/m2. One hundred and seventy-one subjects (71%) had OSA, and 68 (28%) had moderate-to-severe OSA. A receiver operating characteristic curve of the questionnaires were 0.51–0.71 for predicting OSA and 0.51–0.66 for moderate-to-severe OSA. The STOP-BANG questionnaire had an unsatisfactory positive predictive value, while all of the other questionnaires had an inadequate negative predictive value.
Conclusions
Standard OSA questionnaires are not suited for screening among CDs. The use of the HSAT could provide an objective evaluation of for OSA in this special population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is characterized by repeated upper airway obstruction episodes during sleep, leading to frequent arousals and fragmented sleep and to excessive daytime sleepiness (EDS). This represents a serious safety risk in professions where motor vehicles need to be operated for long periods of time, such as among commercial drivers (CDs). OSA is associated with an increased motor vehicle accident (MVA) risk [1], and the OSA prevalence is around threefold higher among CDs than in the general population [2]. CDs with OSA have up to three times the MVA risk [3], and continuous positive airway pressure (CPAP) treatment has proven highly successful in reducing the MVA risk of CDs with OSA [4]. Hence, OSA screening and treatment among CDs is required by the regulatory authorities [4, 5] for public safety and cost-effectiveness reasons.
Overnight polysomnography (PSG) in a sleep center is the gold standard technique for diagnosing the presence and severity of OSA [6]. However, due to its high costs and poor availability, the systematic evaluation of the entire CD population with standard PSG is unfeasible [7], and the optimal way to manage this issue has yet to be addressed.
Several questionnaires have been developed for OSA screening in the general and high-risk populations [8]. These clinical tools consider EDS as well as OSA symptoms, anthropometric measures, and the presence of medical conditions associated with OSA. The efficacy of these questionnaires among CDs is debated. Poor symptom awareness and symptom denial [9, 10], as well as the higher OSA prevalence among CDs, may result in poor performance and in an unacceptable number of CDs with undiagnosed and untreated OSA [11].
To research this topic, we investigated the accuracy of eight standard OSA questionnaires in a cohort of CDs. We hypothesized their poor performance in this special population.
Methods
This was an unsponsored, investigator-initiated, prospective cohort study conducted by a certified sleep medicine center (Multidisciplinary Center for Sleep Medicine, IRCCS Sacro Cuore Don Calabria, Verona, IT) between July 2015 and April 2016. Participation in the study was offered to all CDs employed by 10 discrete commercial goods and people transportation companies based in the two neighboring provinces of Mantua and Verona in Northern Italy. The ethical committee of Verona and Rovigo provinces approved the study protocol (842CESC), and informed consent was obtained from all participants.
Subjects and setting
Consecutive subjects were recruited at their facility office during their yearly scheduled occupational health visit. Only actively working individuals aged 18–65 years with a regular driver’s license were included. Those who did not give formal consent, refused to undertake the home sleep apnea test (HSAT), lacked comprehension of the Italian language used in the questionnaires, and had a previous OSA diagnosis were excluded. Female drivers were excluded since only four were identified. All subjects were interviewed by qualified sleep technicians at the coordinating center. Demographic data, anthropometric parameters (body mass index (BMI), Mallampati score [12], and neck circumference), as well as the presence of OSA risk factors (essential hypertension, alcohol use, diabetes, and smoking) were collected. The Berlin [13], STOP [14], STOP-Bang [15], sleep apnea clinical score [16], apnea risk evaluation system [17], OSAS-Tavolo Tecnico Intersocietario [18], and European Obstructive Sleep Apnea Screening (EUROSAS) [19, 20] questionnaires were sequentially administered by the sleep technicians.
Home sleep apnea test (HSAT)
All subjects, irrespective of their questionnaire findings, underwent an HSAT investigation (type IIII PSG, SCOPER classification S4C4O1P2E2R2 [21]) using a commercial device (Alice NightOne, Philips SpA – Respironics, IT). The sleep technicians delivered the equipment to the participating subjects immediately after the clinical interview, providing full instructions for its use. The HSAT recording, in conjunction with a sleep diary, was collected from the subjects’ place of sleep, home, or work vehicle. Nasal airflow, chest respiratory efforts, sleep position, pulse oximetry, heart rate, and snoring events were monitored. After completing the HSAT, the participants returned the device to their facility’s office. Their participation in the study did not interrupt the CDs’ work activity.
The HSAT data were analyzed offline using ProFusion PSG 3 Lite (Compumedics Europe, Germany) by a sleep center medical staff member who was blinded to the questionnaire results. Apnea was defined as an airflow cessation ≥ 90% from baseline lasting ≥ 10 s, while hypopnea was defined as an airflow reduction of 30–90% for ≥ 10 s followed by ≥ 3% in oxygen desaturation [7]. A diagnosis of OSA was made if a respiratory events index (REI) value of ≥ 5 events/h was calculated for the total sleep period reported in the diary. The severity of OSA was classified, depending on the REI value, as normal (REI < 5), mild (REI ≥ 5 and < 15), moderate (REI ≥ 15 and ≤ 30), or severe (REI > 30) [22]. CDs with a HSAT recording lasting ≤ 5 h were excluded from the study because of the low reliability of the calculated REI [23].
As per protocol, individual HSAT reports were not disclosed to anyone other than the investigated subject. Each facility’s occupational health office was only told the total number of OSA-positive and OSA-negative CDs.
Statistical analysis
The demographic and clinical data were summarized using descriptive statistics, measures of variability, and precision plots. All parameters were reported with 95% confidence intervals. When necessary, the statistical models and estimations were adjusted for covariates.
Differences between CDs with and without a valid HSAT were assessed using the Chi-squared test, Fisher exact test, Mann–Whitney U test, or t-test, as appropriate. Contingency tables, for the assessment of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV), as well as the area under the receiver operating characteristic curve (AUC) values were calculated for both the REI value thresholds of ≥ 5 and ≥ 15. Two independent univariate regression models (one for each REI threshold) were used to select the variables included in the multivariate logistic regression model for identifying independent predictors of OSA.
All analyses were performed using STATA 15 (StataCorp, 2017; Stata Statistical Software, Release 15; College Station, TX: StataCorp LLC.). A P value < 5% was set for statistical significance.
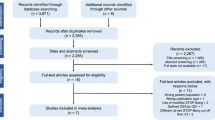
Results
All employed CDs in 7 out of the 10 transportation companies participated in our study, while, in the remaining 3, the participation rate was 15–29% (Online Resource 1). Three hundred and fifteen subjects were enrolled, but 72 (23%) CDs had to be excluded from the analysis due to their insufficient HSAT recording length or a technical failure. There were no differences in the demographic data between the included and excluded CDs except for smoking and hypertension rates (Table 1).
The median age, mean BMI (± standard deviation), and median neck circumference of the included CDs were 50 (interquartile range (IQR) 25–70) years, 27 ± 5 kg/m2, and 38 (IQR = 32–53) cm, respectively. In total, 45 (18.5%) CDs had hypertension, 66 (32.1%) were smokers, and 105 (44.2%) denied any alcohol intake. We found a REI value of ≥ 5 events/h in 172 (71%) subjects and ≥ 15 events/h in 68 (28%) subjects.
In the univariate analysis (Online Resources 2 and 3), OSA and severe OSA were associated with age, BMI, neck circumference, hypertension (only for moderate-to = severe OSA), and Class IV Mallampati score. In the multivariate analysis, only age and neck circumference were associated with any degree of OSA, while Class IV Mallampati score was associated with moderate-to-severe OSA.
All questionnaires demonstrated a high specificity (89–100%) in identifying the OSA risk; however, this led to a rather limited sensitivity (1–36%) (Fig. 1; Online Resource 4). Due to the high OSA prevalence in CDs, the questionnaires’ NPV was unsatisfactory, as it ranged 74–80% for predicting moderate-to-severe OSA. The STOP-BANG (using the ≥ 3 score cutoff) made an exception, showing, inversely, a high sensitivity (88–99%) and a poor specificity (29–44%). Accordingly, compared with all of the other questionnaires, the STOP-BANG exhibited the highest NPV (87–99%) and the lowest PPV (30–44%). The questionnaires’ AUC values ranged 0.51–0.71 for the prediction of OSA and 0.52–0.66 for the prediction of moderate-to-severe OSA. Combining the Mallampati score with the STOP-BANG questionnaire did not increase the overall accuracy in determining the OSA risk.
Discussion
Given the association with the MVA risk, OSA identification and treatment among professional drivers are a public health issue. Due to the limited availability of PSG testing and sleep medicine resources, CDs screening in occupational health practice are often limited to the administration of standard OSA questionnaires.
In our cohort of CDs, where OSA was found at the expected prevalence in this population [24], we demonstrated the poor performance of these questionnaire tools. The main finding of this study is that, although the questionnaires had a high specificity, a large number of CDs with a negative questionnaire had OSA. The STOP-BANG exhibited the opposite limitation, providing a high number of false-positive subjects. The AUC values confirmed the questionnaires’ overall unsuitability as reliable OSA screening tools in this population.
Several investigators have previously researched the accuracy of EDS and OSA questionnaires among CDs [11, 25]. With the exception of the following three studies, previous work tested with PSG only those subjects (and sometimes only a proportion of them) who were ranked at high risk by the questionnaires themselves.
Ueyama et al. [26] retrospectively investigated 1309 CDs employed by a single transportation company using the Epworth sleepiness scale (ESS) and a type IV PSG. They found OSA in 60% of the subjects and moderate-to-severe OSA in 24%, but only 9% had an ESS score ≥ 11 due to the poor awareness of subjective sleepiness symptoms. Firat et al. [27] examined 85 highway bus drivers from two transportation companies with the Berlin, OSA50, STOP, and STOP-BANG questionnaires and a standard PSG. Although the authors did not provide information on their screening method, they found the STOP-BANG to be the best-performing questionnaire (PPV 67%, NPV 76%) in a CD sample characterized by an increased rate (54%) of moderate-to-severe OSA. Popević and colleagues [15] assessed the accuracy of the STOP-BANG questionnaire in a sample of 100 CDs already preselected from an unspecified larger sleepiness study. They found better performance in the use of the STOP-BANG questionnaire than in our study, as the AUC values were 0.80 for OSA and 0.92 for moderate-to-severe OSA. The different screening strategies and population characteristics (since the CDs in the Popević cohort were more hypertensive and had an increased BMI and neck circumference) might account for the discrepancy between the two studies.
Apart from the larger sample of CDs included, several methodological differences from previous studies characterize this study. A higher number of OSA and EDS questionnaires were tested, and all CDs underwent the HSAT study irrespective of their questionnaire results. Screening CDs during their occupational health visit provided a probabilistic sampling of the participating subjects from the entire cohort. Greater acceptance of study participation was ensured by obtaining the HSAT at home or in the work vehicle without disrupting the CDs’ busy schedule and maintaining anonymity of the subjects HSAT results. Sleep technicians played a major role, by being available at the transportation facilities, explaining the benefit of OSA diagnosis to the drivers, and ensuring the quality of the data collection and analysis as much as possible.
The use of the HSAT instead of overnight PSG made this field study feasible. Although it lacks the EEG signals, the HSAT is based on total recording time rather than actual sleep time, and this may lead to REI underestimation. However, except for the presence of select comorbid conditions such as moderate-to-severe pulmonary disease or the extremely obese, HSAT is a reliable alternative to standard PSG [28, 29] and is routinely used in sleep centers, generally without the need for confirmatory PSG. Outcome studies conducted in non-occupational settings have shown a similar efficacy between overnight PSG and the HSAT [30]. Regulatory authorities are thus increasingly recognizing the role of the HSAT for the diagnosis of OSA among CDs, as long as the chain of custody of the investigated subject is provided [31].
Limitations
We cannot exclude the possibility that using standard PSG would have yielded different results on the questionnaires’ accuracy. The involvement of sleep technicians experienced in the use of both the HSAT and standard PSG helped minimize the differences between the two techniques. The study protocol did not include the subjects’ chain of custody. Some CDs could have therefore cheated by avoiding or misreporting sleep or by using a substitute during the HSAT recording. Moreover, subjective questionnaires are open to bias by CDs who may be motivated to underestimate their OSA and EDS symptoms due to the legal consequences. We sought to minimize this issue as much as possible by guaranteeing the anonymity of the HSAT report and excluding from the study CDs with a previous OSA diagnosis.
Conclusions
OSA and EDS questionnaires do not seem to provide an acceptable level of accuracy for the screening of OSA among CDs. Objective OSA measures, as well as fitness to drive tests, are undoubtedly needed in this context. The HSAT could improve the investigation of OSA in this population.
Data availability
The original data are available upon reasonable request.
References
Tregear S, Reston J, Schoelles K, Phillips B (2009) Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med 5(6):573–581
Sunwoo JS, Shin DS, Hwangbo Y, Kim WJ, Chu MK, Yun CH, Jang T, Yang KI (2019) High risk of obstructive sleep apnea, insomnia, and daytime sleepiness among commercial motor vehicle drivers. Sleep Breath 23(3):979–985. https://doi.org/10.1007/s11325-019-01805-7
Meuleners L, Fraser ML, Govorko MH, Stevenson MR (2015) Obstructive sleep apnea, health-related factors, and long distance heavy vehicle crashes in Western Australia: a case control study. J Clin Sleep Med 11(4):413–418. https://doi.org/10.5664/jcsm.4594
Gurubhagavatula I, Sullivan S, Meoli A, Patil S, Olson R, Berneking M, Watson NF (2017) Management of obstructive sleep apnea in commercial motor vehicle operators: recommendations of the AASM sleep and transportation safety awareness task force. J Clin Sleep Med 13(5):745–758. https://doi.org/10.5664/jcsm.6598
Bonsignore MR, Randerath W, Riha R, Smyth D, Gratziou C, Goncalves M, McNicholas WT (2016) New rules on driver licensing for patients with obstructive sleep apnea: European Union Directive 2014/85/EU. J Sleep Res 25(1):3–4. https://doi.org/10.1111/jsr.12379
Malhotra RK, Kirsch DB, Kristo DA, Olson EJ, Aurora RN, Carden KA, Chervin RD, Martin JL, Ramar K, Rosen CL, Rowley JA, Rosen IM, American Academy of Sleep Medicine Board of D (2018) Polysomnography for obstructive sleep apnea should include arousal-based scoring: an American Academy of Sleep Medicine Position Statement. J Clin Sleep Med 14(7):1245–1247. https://doi.org/10.5664/jcsm.7234
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine Clinical Practice guideline. J Clin Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506
Kee K, Dixon J, Shaw J, Vulikh E, Schlaich M, Kaye DM, Zimmet P, Naughton MT (2018) Comparison of commonly used questionnaires to identify obstructive sleep apnea in a high-risk population. J Clin Sleep Med 14(12):2057–2064. https://doi.org/10.5664/jcsm.7536
Talmage JB, Hudson TB, Hegmann KT, Thiese MS (2008) Consensus criteria for screening commercial drivers for obstructive sleep apnea: evidence of efficacy. J Occup Environ Med 50(3):324–329. https://doi.org/10.1097/JOM.0b013e3181617ab8
Parks P, Durand G, Tsismenakis AJ, Vela-Bueno A, Kales S (2009) Screening for obstructive sleep apnea during commercial driver medical examinations. J Occup Environ Med 51(3):275–282. https://doi.org/10.1097/jom.0b013e31819eaaa4
Berger M, Varvarigou V, Rielly A, Czeisler CA, Malhotra A, Kales SN (2012) Employer-mandated sleep apnea screening and diagnosis in commercial drivers. J Occup Environ Med 54(8):1017–1025. https://doi.org/10.1097/JOM.0b013e3182572e16
Sutherland K, Keenan BT, Bittencourt L, Chen NH, Gislason T, Leinwand S, Magalang UJ, Maislin G, Mazzotti DR, McArdle N, Mindel J, Pack AI, Penzel T, Singh B, Tufik S, Schwab RJ, Cistulli PA, Investigators S (2019) A global comparison of anatomic risk factors and their relationship to obstructive sleep apnea severity in clinical samples. J Clin Sleep Med 15(4):629–639. https://doi.org/10.5664/jcsm.7730
Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP (1999) Using the Berlin questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 131(7):485–491. https://doi.org/10.7326/0003-4819-131-7-199910050-00002
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, Khajehdehi A, Shapiro CM (2008) STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 108(5):812–821. https://doi.org/10.1097/ALN.0b013e31816d83e4
Popevic MB, Milovanovic A, Nagorni-Obradovic L, Nesic D, Milovanovic J, Milovanovic APS (2017) Screening commercial drivers for obstructive sleep apnea: validation of STOP-Bang questionnaire. Int J Occup Med Environ Health 30(5):751–761. https://doi.org/10.13075/ijomeh.1896.00906
Flemons WW, Whitelaw WA, Brant R, Remmers JE (1994) Likelihood ratios for a sleep apnea clinical prediction rule. Am J Respir Crit Care Med 150(5 Pt 1):1279–1285. https://doi.org/10.1164/ajrccm.150.5.7952553
Westbrook PR, Levendowski DJ, Cvetinovic M, Zavora T, Velimirovic V, Henninger D, Nicholson D (2005) Description and validation of the apnea risk evaluation system: a novel method to diagnose sleep apnea-hypopnea in the home. Chest 128(4):2166–2175. https://doi.org/10.1378/chest.128.4.2166
Pneumologia SId (2014) Questionario OSAS TTI. http://www.sipirs.it/cms/tavolo-tecnico-interdisciplinare-lo-screening-clinico-dellosas/. Accessed Jan 2021
McNicholas WT New standards and guidelines for drivers with obstructive sleep apnoea syndrome: report of the obstructive sleep apnoea working group. University College Dublin Library
Peker Y, Ozaydin AN, Cetinkaya R, Kabadayi E, Karakucuk AG, Celik Y, McNicholas WT (2020) Reliability of the Turkish version of the European Obstructive Sleep Apnea Screening (EUROSAS) questionnaire for drivers. Sleep Breath. https://doi.org/10.1007/s11325-020-02201-2
Collop NA, Tracy SL, Kapur V, Mehra R, Kuhlmann D, Fleishman SA, Ojile JM (2011) Obstructive sleep apnea devices for out-of-center (OOC) testing: technology evaluation. J Clin Sleep Med 7(5):531–548. https://doi.org/10.5664/Jcsm.1328
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep M (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8(5):597–619. https://doi.org/10.5664/jcsm.2172
Wittine LM, Olson EJ, Morgenthaler TI (2014) Effect of recording duration on the diagnostic accuracy of out-of-center sleep testing for obstructive sleep apnea. Sleep 37(5):969–975. https://doi.org/10.5665/sleep.3672
Gurubhagavatula I, Tan M, Jobanputra AM (2020) OSA in professional transport operations: safety, regulatory, and economic impact. Chest 158(5):2172–2183. https://doi.org/10.1016/j.chest.2020.05.582
Schiza SE, Bouloukaki I (2020) Screening for obstructive sleep apnoea in professional drivers. Breathe 16(1):29364. https://doi.org/10.1183/20734735.0364-2019
Ueyama M, Kokuto H, Sugihara H, Oikawa S, Suzuki F, Goto H, Kudoh S (2018) Investigation of obstructive sleep apnea using portable monitors and health check data in Japanese drivers. J Atheroscler Thromb 25(11):1118–1127. https://doi.org/10.5551/jat.41806
Firat H, Yuceege M, Demir A, Ardic S (2012) Comparison of four established questionnaires to identify highway bus drivers at risk for obstructive sleep apnea in Turkey. Sleep Biol Rhythms 10(3):231–236. https://doi.org/10.1111/j.1479-8425.2012.00566.x
Zhang C, Berger M, Malhotra A, Kales SN (2012) Portable diagnostic devices for identifying obstructive sleep apnea among commercial motor vehicle drivers: considerations and unanswered questions. Sleep 35(11):1481–1489. https://doi.org/10.5665/sleep.2194
Kundel V, Shah N (2017) Impact of portable sleep testing. Sleep Med Clin 12(1):137–147. https://doi.org/10.1016/j.jsmc.2016.10.006
El Shayeb M, Topfer LA, Stafinski T, Pawluk L, Menon D (2014) Diagnostic accuracy of level 3 portable sleep tests versus level 1 polysomnography for sleep-disordered breathing: a systematic review and meta-analysis. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne 186 (1):E25–E51. https://doi.org/10.1503/cmaj.130952
Colvin LJ, Dace GA, Colvin RM, Ojile J, Collop N (2016) Commercial motor vehicle driver positive airway pressure therapy adherence in a sleep center. J Clin Sleep Med 12(4):477–485. https://doi.org/10.5664/jcsm.5670
Acknowledgements
The authors are grateful to Professor Maria Rosaria Bonsignore for her valuable suggestions and comments that contributed to improving the quality of this manuscript.
Author information
Authors and Affiliations
Contributions
AA, DT, AC, DT, and GR were involved in the design of the study, data collection, and interpretation and provided critical revision of the manuscript and intellectual discussion.
GC, MG, and NDS were involved in the data analysis and interpretation.
All authors were substantially involved in drafting the article and approved this final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Ethical Committee of Verona and Rovigo Provinces (842CESC), and informed consent was obtained from all participants. All included subjects gave informed consent to participate in the study. Anonymity of personal data and reports was guaranteed by the study protocol.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material. .
Rights and permissions
About this article
Cite this article
Adami, A., Tonon, D., Corica, A. et al. Poor performance of screening questionnaires for obstructive sleep apnea in male commercial drivers. Sleep Breath 26, 541–547 (2022). https://doi.org/10.1007/s11325-021-02414-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02414-z