Abstract
Purpose
Sleep surgery and mandibular advancement devices (MAD) are treatments for obstructive sleep apnea (OSA), but their comparative efficacy remains unclear. We compared their efficacy using various parameters.
Methods
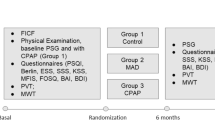
Subjects treated for OSA with sleep surgery or MAD (n = 30/group)—matched for sex, body mass index (BMI), and baseline apnea–hypopnea index (AHI)—were enrolled. The efficacy of these treatments according to polysomnographic parameters, sleep quality questionnaires, and heart rate variability (HRV) time- and frequency-domain parameters were compared between pre-treatment and 3-month post-treatment.
Results
Polysomnographic and sleep quality questionnaire parameters improved significantly in both groups. In time-domain HRV analysis, average normal-to-normal intervals increased significantly in the surgery (942.2 ± 140.8 to 994.6 ± 143.1, P = 0.008) and MAD (901.1 ± 131.7 to 953.7 ± 123.1, P = 0.002) groups. Low frequency (LF) decreased significantly in the surgery group (P = 0.012); high frequency (HF) remained unchanged in both groups. The LF/HF ratio decreased in both groups (2.9 ± 1.8 to 2.3 ± 1.7, P = 0.017, vs. 3.0 ± 1.8 to 2.4 ± 1.4, P = 0.025). Normalized high frequency increased significantly in both groups (31.0 ± 13.2 to 36.8 ± 13.7, P = 0.009, vs. 29.1 ± 10.7 to 33.7 ± 12.5, P = 0.024), in contrast to normalized low frequency. However, no HRV parameter changes differed significantly between the groups after adjusting for age, BMI, and AHI.
Conclusion
Sleep surgery and MAD are equally effective treatments for OSA according to cardiac autonomic activity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a prevalent disorder that affects 2% to 4% of the adult population [1]. Patients with OSA experience partial or complete cessation of respiratory flow due to periodic collapse of the upper respiratory tract during sleep, and the condition has been associated with cardiovascular morbidities, such as hypertension, ischemic heart disease, congestive heart failure, arrhythmias, as well as with cardiovascular mortality [2,3,4,5]. Continuous positive airway pressure (CPAP) is a treatment of choice for OSA, regardless of severity. Oral appliances and surgical treatments may be individual alternative treatments in OSA patients, who despite all efforts are not treatable with CPAP therapy, such as when patients decline CPAP therapy or CPAP therapy is ineffective in eliminating OSA. Evidence of clinical efficacy for sleep surgery and mandibular advancement devices (MAD) is limited and their efficacy is inferior to the gold standard of CPAP, but sleep surgery and MAD may represent a therapeutic option in individual patients with good compliance [6, 7].
MAD are a type of oral appliance that can effectively reduce the collapsibility of the upper airway during sleep for mild to moderate OSA [8], and as sleep surgery and mandibular advancement devices are not directly comparable, they may have significance in selected cases. Many previous studies have reported that sleep surgery and MAD could lower risk of cardiovascular mortality in OSA patients by reducing the respiratory flow limitation during sleep [9, 10]. However, it is difficult to define which of sleep surgery or MAD is a more effective alternative for OSA.
Classically, polysomnography (PSG) and sleep questionnaires are objective and subjective methods, respectively, for evaluating the efficacy of treatments for OSA although sleep questionnaires are known to be imprecise in cardiovascular patients [11]. Heart rate variability (HRV), which can be measured from a single-lead electrocardiography (ECG) signal, reflects cardiac autonomic activity and reflects the quantitative variation between normal-to-normal heartbeats [12]. The clinical implications of HRV were first proposed in 1965, and since then, the association between OSA and increased sympathetic activity in HRV has been well described [13, 14]. Moreover, adequate treatment of OSA may reverse the deterioration in cardiac autonomic activity [15, 16]. Therefore, evaluation of HRV could be used to assess treatment efficacy in OSA. However, cardiac autonomic activity has rarely been used to evaluate treatment efficacy between sleep surgery and MAD for OSA.
We hypothesized that there might be a difference between sleep surgery and MAD from the perspective of improvement of cardiac autonomic activity in patients with OSA. This study aimed to compare the efficacy between sleep surgery and MAD in terms of cardiac autonomic activity, using HRV analysis.
Methods
Subjects
We retrospectively reviewed patients who underwent sleep surgery for OSA in our clinic from January 2013 to December 2017. Sleep surgery included tonsillectomy, uvulo-palato-pharyngoplasty, expansion sphincter pharyngoplasty, lateral pharyngoplasty, tongue-base resection, and a combination of these procedures. Each surgical procedure was performed according to whether the patient had upper airway collapse, which was evaluated by physical examinations, such as sleep videofluoroscopy, Muller’s maneuver, and Friedman grading system. In brief, we conducted tonsillectomy for patients with OSA who had tonsil enlargement. Enlarged tonsil and velopharyngeal collapse were indications for uvulo-palato-pharyngoplasty. Patients with observed velopharyngeal lateral collapse in physical exam underwent expansion sphincter pharyngoplasty or lateral pharyngoplasty. Tongue-base resection was applied to patients with oropharyngeal collapse by a tongue base. Furthermore, multi-level surgery was performed for patients with velopharyngeal and oropharyngeal collapse simultaneously. Among these, we selected patients according to the following inclusion and exclusion criteria. We included adult patients (age ≥ 18 years), patients diagnosed with OSA (apnea–hypopnea index, AHI > 5/h), patients who had a follow-up PSG at 3 months after treatment, and who had two PSG datasets (baseline and 3-month post-treatment) available. We excluded patients with significant arrhythmias, low-quality data (artifacts exceeding 20% of total sleep time), total sleep time < 5 h, awakening more than 30 min from midnight to 5 am, patients with combined sleep disorders (i.e., insomnia or narcolepsy), habitual use of sedatives and hypnotics, and history of specific pathology related to HRV changes (i.e., myocardial infarction, diabetic neuropathy, cardiac transplantation, myocardial dysfunction, or tetraplegia).
Forty-two patients who met the criteria were identified. During this period, 54 patients who met the inclusion and exclusion criteria were treated for OSA by MAD. These patients were matched for sex, body mass index (BMI, ± 0.5 kg/m2), and baseline AHI (± 5/h) with patients treated by sleep surgery. The matching process was performed with blinding to the result of follow-up PSG. Thirty patients were enrolled in the sleep surgery or MAD group. The ethics committee of Seoul National University Bundang Hospital (IRB No.B-1907/555-108) approved the use of the data. The need for written informed consent was waived by the institutional review board.
Classical evaluation of treatment efficacy
Embla™ N7000 (Embla, Reykjavik, Iceland), a commercially available recording PSG system with standard electrodes and sensors, was used to perform the procedure, under the supervision of a skilled technician. Apnea was defined as the complete cessation of airflow for at least 10 s. We defined hypopnea as a substantial reduction in airflow (≥ 50%) for at least 10 s or a moderate reduction in airflow for at least 10 s associated with oxygen desaturation (≥ 4%) or electroencephalographic arousals. The AHI was defined as the total number of apneas and hypopneas per hour of sleep.
Sleep questionnaires, completed by subjects, were also analyzed. Daytime sleepiness was evaluated using the Epworth sleepiness scale (ESS); subjective sleep quality was measured using the Pittsburgh sleep quality index (PSQI).
HRV analysis
The single-lead ECG data exported from the PSG system were used to measure HRV, using commercially available software (RemLogic 3.0 HRV analyzer; Embla Systems, San Carlos, CA). The ECG signal from midnight to 5 am were analyzed for comparison under identical conditions (signals from before midnight and after 5 am were not included in analysis) and interpolated and resampled at 5.0 Hz. Normal-to-normal heartbeat intervals < 400 ms and > 2400 ms were omitted. We used the standard methods of HRV measurement to calculate the time-domain and frequency-domain parameters [12].
Time-domain measures
The time-domain parameters included were the average normal-to-normal (NN) interval, standard deviation of NN intervals (SDNN), square root of the mean of the squared differences of adjacent NN intervals (RMSSD), and number of pairs of adjacent NN intervals greater than 50 ms (NN50).
Frequency-domain measures
The frequency-domain parameters used in the present study were total power (variance of all normal-to-normal intervals), very low frequency (VLF; power in 0.003–0.04 Hz range), low frequency (LF; power in 0.04–0.15 Hz range), high frequency (HF; power in 0.15–0.4 Hz range), normalized LF [LFnu; LF / (LF + HF) × 100], normalized HF [HFnu; HF / (LF + HF) × 100], and LF/HF ratio. LF activity reflects a mixture of both sympathetic and parasympathetic activity, while HF has been linked to parasympathetic activity. The LF/HF ratio is considered to reflect the balance between sympathetic and parasympathetic activity and is correlated with the degree of AHI in OSA [14]. LFnu and HFnu are regarded as markers of sympathetic and parasympathetic activity, respectively.
Statistical analysis
Data obtained in this study for continuous variables were presented as mean ± standard deviation (SD), while sex, a categorical variable, was presented as ratio male to female. The independent t test or chi-squared test was performed to evaluate the differences in baseline characteristics between sleep surgery and MAD groups. The paired t test was used to evaluate differences between baseline values of parameters and those at 3 months post-treatment. Differences in baseline to post-treatment HRV changes between sleep surgery and MAD groups were tested by analysis of covariance (ANCOVA), with age, BMI, and baseline AHI as covariates. In ANCOVA, values were expressed as least-squares means (LSmeans) and 95% confidence intervals. We used SPSS software, version 18 (SPSS Inc., Chicago, IL, USA) to perform the data analysis; P values < 0.05 were considered statistically significant.
Results
Patient characteristics
Most baseline characteristics between the sleep surgery group and MAD group showed no statistically significant difference; except for age and sleep stage (Table 1). Because subjects were matched, BMI and AHI were comparable, and the male to female ratio was equal to 27:3 in both groups. The age of the patients in the sleep surgery group was significantly younger than that of those in the MAD group and the N3 sleep stage was higher in the sleep surgery than in the MAD group.
Changes in polysomnography parameters
Both groups had significantly decreased BMI after treatment (from 26.8 ± 3.4 to 26.3 ± 3.1 in sleep surgery group, P = 0.013; from 26.7 ± 2.9 to 26.5 ± 2.9 in MAD group, P = 0.010). However, no difference was found between the two groups in BMI changes, (P = 0.798). We performed follow-up PSG evaluation at 3 months after treatment. Among the parameters, AHI, apnea index, oxygen desaturation index, and arousal were decreased, and minimal oxygen saturation was increased statistically significantly in both groups. In the proportion of total sleep time, stage N1 (decreased, P = 0.029), stage N2 (increased, P = 0.035), and rapid eye movement (REM) stage (increased, P = 0.034) changed significantly in the sleep surgery group at 3-month post-treatment. In the MAD group, stages N2 (P = 0.045) and N3 (P = 0.027) were significantly increased after treatment (Table 2).
Changes in sleep questionnaires
Subjective sleep quality analysis was performed using ESS and PSQI. ESS decreased in the sleep surgery group (from 7.6 ± 2.4 to 5.4 ± 2.5, P < 0.001) and PSQI decreased in both groups (from 10.9 ± 3.1 to 6.9 ± 3.4, P < 0.001 in the sleep surgery group; from 11.1 ± 5.1 to 9.2 ± 5.1, P = 0.012 in the MAD group) after treatment, as compared to baseline (Fig. 1).
Changes in the mean of sleep questionnaires before and 3 months after sleep surgery or mandibular advancement device. a Epworth sleepiness scale and Pittsburgh sleep quality index scores were significantly decreased after sleep surgery as compare to baseline. b The Pittsburgh sleep quality index score was significantly decreased after mandibular advancement device treatment. The Epworth sleepiness scale score tended to decrease after mandibular advancement device treatment, but this change was not statistically significant. *P < 0.05
Changes in heart rate variability
Among time-domain indices, the average NN interval significantly increased in both sleep surgery (P = 0.008) and MAD (P = 0.002) groups after treatment. However, other time-domain parameters did not change in either group.
In frequency-domain analysis, LF significantly decreased in the sleep surgery group (P = 0.012), while HF was unchanged in both groups at 3-month post-treatment. The LF/HF ratio had decreased significantly in both the sleep surgery (P = 0.017) and MAD (P = 0.025) groups after treatment, as compared to baseline. Moreover, in both groups, HFnu increased significantly (P = 0.009 in the sleep surgery group; P = 0.024 in the MAD group), and as HFnu increased, LFnu decreased (Table 3).
Comparison of changes of heart rate variability between groups
Finally, changes in HRV from baseline to post-treatment were compared between the sleep surgery and MAD groups. These changes were not significantly different between groups after adjusting for age, BMI, and baseline AHI (Table 4).
Discussion
Since CPAP was introduced by Sullivan in 1981 as a safe treatment for OSA, it has been considered as a gold-standard modality [17]. Furthermore, a recent study reported that CPAP therapy improved cardiac ventricular function through reduced pulmonary hypertension [18]. According to many studies to date, there is consensus about the efficacy and importance of CPAP for OSA, but its lower patient compliance and poor long-term acceptance have been limitations to its implementation. To overcome the limitation of CPAP, new devices, such as hypoglossal nerve stimulation, have been developed until recently [19]. Sleep surgery and MAD are the most widely used alternative treatments for patients who decline CPAP; the usefulness of these two modalities has been well described in many studies. However, to the best of our knowledge, few studies have compared the efficacy between sleep surgery and MAD for OSA. The present study evaluated the efficacy of these two treatments, which were matched for sex, BMI, and AHI at baseline, in terms of cardiac autonomic activity and identified positive effects in both groups. However, we found both sleep surgery and MAD to be equally efficacious, because there was no difference in HRV changes from baseline to 3 months after treatment between the two therapies after adjusting for confounding factors.
The cardiac autonomic nervous system consists of a parasympathetic and a sympathetic branch, and heartbeat is modulated by a balance between these two branches. If parasympathetic nerves are suppressed and sympathetic nerves are activated, the heartbeat converges to the intrinsic heart rate (approximately 100 beats/min) and results in reduced HRV. Reduced HRV is associated with congestive heart failure, diabetic neuropathy, sudden cardiac death, and post-cardiac transplant. Theoretically, HRV could be a method for evaluating the efficacy of OSA treatment, as it reflects cardiac autonomic activity. The improvement in HRV post-OSA treatment, such as sleep surgery, MAD, and CPAP, has been reported in previous studies. A study related to sleep surgery reported that VLF, LF, and LFnu changes were significant in successful upper airway surgery patients [15]. Another study demonstrated that expansion sphincter pharyngoplasty decreased the LF/HF ratio in the successful surgery group [20]. In a comparative study that was presented, even though CPAP proved to be more effective at reducing AHI, both MAD and CPAP significantly decreased the total power of HRV [21]. Moreover, CPAP significantly decreased SDNN in patients with OSA even at the first night of use [22].
A study suggested that time-domain HRV analysis was a useful index for assessing a sympathovagal balance in OSA, because OSA patients showed a shorter average NN interval than healthy subjects. Our study showed that the average NN interval significantly increased in both groups after treatment, and this reflected improvement of sympathovagal balance by both therapies. Our study results also demonstrated improvement in the frequency-domain in both groups. An increased LF/HF ratio in OSA patients compared to healthy subjects has been reported in previous studies and is considered a useful parameter to evaluate severity of the condition [23]. Moreover, adequate application of treatment modalities for OSA could correct the increased LF/HF ratio in OSA patients [24, 25]. In our study, the LF/HF ratio was significantly decreased in both sleep surgery and MAD groups, and it represented decreased OSA severity in subjects or change in the autonomic nerve system balance to a parasympathetic dominance. Among the other frequency-domain indices, we found a significant decrease in LFnu as well as an increase in HFnu by both therapies. As mentioned earlier, LFnu and HFnu are regarded as markers of sympathetic and parasympathetic modulation, respectively. Briefly, considering the frequency-domain changes, the effects of both therapies on cardiac autonomic activity were associated with an increase in parasympathetic activity and a decrease in sympathetic activity.
HRV measurement can provide information about the risk of cardiovascular diseases in patients with OSA because it is considered as a strong predictor of cardiovascular mortality [26]. Moreover, the sympathetic hyperactivity and imbalance of the cardiovascular autonomic nervous system during sleep may play a critical role in development of cardiovascular diseases [27, 28]. Therefore, both alternative OSA therapies attenuate the cardiovascular risk by re-adjustment of the imbalance of the autonomic nerve system in OSA.
PSG parameters and sleep questionnaires are representative classical evaluation methods of the efficacy of OSA treatments. In the present study, because subjects were matched in terms of sex, BMI, and AHI, the baseline PSG parameters, and HRV indices showed no differences between sleep surgery and MAD groups. However, age was younger and N3 sleep stage was increased in sleep surgery group. This might reflect the patient’s desire or the physicians’ preference for performing surgery in younger OSA patients. The difference in N3 sleep stage between groups might be associated with the age difference, because the duration of slow-wave sleep gradually decreases by 2% per decade from young to middle-age [29].
In PSG parameters, respiration-related indices, such as AHI, oxygen desaturation index, and minimal oxygen saturation, were significantly improved after treatment in both groups. AHI was decreased by more than 50% after treatment as compared to baseline (from 45 to 22 in the sleep surgery group, from 44 to 21 in the MAD group) and the change was accepted as a response to treatment in some previous studies [30,31,32]. The proportion of REM stage sleep in the sleep surgery group and N3 sleep stage in the MAD group were significantly increased, and REM and slow-wave sleep rebound was associated with successful treatment of OSA [33, 34]. Therefore, our study also confirmed the efficacy of these two alternative therapies in terms of PSG parameters.
Some studies have reported issues with inter-test reliability and a need for further validation of the ESS and PSQI; nevertheless, these are currently representative questionnaires for subjective sleep quality evaluations [35, 36]. A decrement in the ESS score reflects improvement in daytime sleepiness, which is associated with motor-vehicle accidents, work-related accidents, and increased risk of diabetes, myocardial infarction, and stroke [36]. In this study, ESS scores were significantly decreased in the sleep surgery group and PSQI scores were decreased in both groups post-treatment; thus, the subjective symptom improvement based on these questionnaires also demonstrated the efficacy of both alternative OSA treatments.
This study had several limitations. First, the study was performed with patients who underwent follow-up PSG at 3 months after treatment. The efficacy of treatment may be exaggerated because patients with better outcomes tended to participate in the follow-up test. Second, this was a retrospective study, and selection bias may have been present. A well-designed randomized control study or cross-over study would be ideal for comparing the efficacy of sleep surgery and MAD. However, a cross-over study was not possible for surgical intervention, and such experiments could have ethical implications. To minimize bias, we matched the groups for sex, BMI, and AHI after blinding the results of follow-up PSG. Third, this study did not evaluate compliance with the therapies. The compliance of sleep surgery is not a consideration, but adherence to using the MAD is an important factor in determining treatment efficacy. For a more valid analysis of the treatment efficacy for OSA, a future prospective comparative study is warranted, considering compliance. Fourth, patients who underwent heterogeneous surgery, such as tonsillectomy, uvulo-palato- pharyngoplasty, expansion sphincter pharyngoplasty, and so on, were considered among the sleep surgery group. We performed sleep surgery according to the sites of the upper airway collapse. Therefore, the purpose of each sleep surgery was homogeneous to improve autonomic nervous system imbalance by preventing upper airway collapse, same as the purpose of CPAP therapy [37].
Conclusion
Both treatment modalities were considered useful for OSA in terms of cardiac autonomic activity. The observed changes in HRV indices may indicate that both therapies could attenuate OSA-related cardiovascular mortality. However, the superiority of sleep surgery or MAD in terms of cardiac autonomic activity was not identified. Further studies are needed to compare the efficacy between sleep surgery and MAD for OSA.
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235. https://doi.org/10.1056/NEJM199304293281704
Bliwise DL, Bliwise NG, Partinen M, Pursley AM, Dement WC (1988) Sleep apnea and mortality in an aged cohort. Am J Public Health 78(5):544–547. https://doi.org/10.2105/ajph.78.5.544
Hung J, Whitford EG, Parsons RW, Hillman DR (1990) Association of sleep apnoea with myocardial infarction in men. Lancet 336(8710):261–264. https://doi.org/10.1016/0140-6736(90)91799-g
Kales A, Bixler EO, Cadieux RJ, Schneck DW, Shaw LC 3rd, Locke TW, Vela-Bueno A, Soldatos CR (1984) Sleep apnoea in a hypertensive population. Lancet 2(8410):1005–1008. https://doi.org/10.1016/s0140-6736(84)91107-3
McNicholas WT, Bonsigore MR, Management Committee of ECAB (2007) Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J 29(1):156–178. https://doi.org/10.1183/09031936.00027406
Holley AB, Lettieri CJ, Shah AA (2011) Efficacy of an adjustable oral appliance and comparison with continuous positive airway pressure for the treatment of obstructive sleep apnea syndrome. Chest 140(6):1511–1516. https://doi.org/10.1378/chest.10-2851
Lam B, Sam K, Mok WY, Cheung MT, Fong DY, Lam JC, Lam DC, Yam LY, Ip MS (2007) Randomised study of three non-surgical treatments in mild to moderate obstructive sleep apnoea. Thorax 62(4):354–359. https://doi.org/10.1136/thx.2006.063644
Huang Y, White DP, Malhotra A (2005) The impact of anatomic manipulations on pharyngeal collapse: results from a computational model of the normal human upper airway. Chest 128(3):1324–1330. https://doi.org/10.1378/chest.128.3.1324
Gotsopoulos H, Kelly JJ, Cistulli PA (2004) Oral appliance therapy reduces blood pressure in obstructive sleep apnea: a randomized, controlled trial. Sleep 27(5):934–941. https://doi.org/10.1093/sleep/27.5.934
Pang KP, Pang EB, Pang KA, Vicini C, Chan YH, Rotenberg BW (2018) Upper airway surgery for obstructive sleep apnea reduces blood pressure. Laryngoscope 128(2):523–527. https://doi.org/10.1002/lary.26759
Reuter H, Herkenrath S, Treml M, Halbach M, Steven D, Frank K, Castrogiovanni A, Kietzmann I, Baldus S, Randerath WJ (2018) Sleep-disordered breathing in patients with cardiovascular diseases cannot be detected by ESS, STOP-BANG, and Berlin questionnaires. Clin Res Cardiol 107(11):1071–1078. https://doi.org/10.1007/s00392-018-1282-7
Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996). Circulation 93 (5):1043–1065
Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T, American Heart Association Council for High Blood Pressure Research Professional Education Committee CoCC, American Heart Association Stroke C, American Heart Association Council on Cardiovascular N, American College of Cardiology F (2008) Sleep apnea and cardiovascular disease: an American Heart Association/american college of Cardiology Foundation scientific statement from the American Heart Association Council for high blood pressure research professional education committee, council on clinical cardiology, stroke council, and council on cardiovascular nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on sleep disorders research (National Institutes of Health). Circulation 118(10):1080–1111. https://doi.org/10.1161/CIRCULATIONAHA.107.189375
Vanninen E, Tuunainen A, Kansanen M, Uusitupa M, Lansimies E (1996) Cardiac sympathovagal balance during sleep apnea episodes. Clin Physiol 16(3):209–216. https://doi.org/10.1111/j.1475-097x.1996.tb00569.x
Choi JH, Yi JS, Lee SH, Kim CS, Kim TH, Lee HM, Lee BJ, Lee SH, Chung YS (2012) Effect of upper airway surgery on heart rate variability in patients with obstructive sleep apnoea syndrome. J Sleep Res 21(3):316–321. https://doi.org/10.1111/j.1365-2869.2011.00978.x
Glos M, Penzel T, Schoebel C, Nitzsche GR, Zimmermann S, Rudolph C, Blau A, Baumann G, Jost-Brinkmann PG, Rautengarten S, Meier JC, Peroz I, Fietze I (2016) Comparison of effects of OSA treatment by MAD and by CPAP on cardiac autonomic function during daytime. Sleep Breath 20(2):635–646. https://doi.org/10.1007/s11325-015-1265-0
Sullivan CE, Issa FG, Berthon-Jones M, Eves L (1981) Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1(8225):862–865. https://doi.org/10.1016/s0140-6736(81)92140-1
S Sharma, H Fox, F Aguilar, U Mukhtar, L Willes, B Bozorgnia, T Bitter, O Oldenburg (2019) Auto positive airway pressure therapy reduces pulmonary pressures in adults admitted for acute heart failure with pulmonary hypertension and obstructive sleep apnea. The ASAP-HF Pilot Trial. Sleep 42 (7). https://doi.org/10.1093/sleep/zsz100
Eastwood PR, Barnes M, MacKay SG, Wheatley JR, Hillman DR, Nguyên XL, Lewis R, Campbell MC, Pételle B, Walsh JH, Jones AC, Palme CE, Bizon A, Meslier N, Bertolus C, Maddison KJ, Laccourreye L, Raux G, Denoncin K, Attali V, Gagnadoux F, Launois SH (2019) Bilateral hypoglossal nerve stimulation for treatment of adult obstructive sleep apnea. Eur Respir J 10. Pii: 1901320. doi: https://doi.org/10.1183/13993003.01320-2019
Süslü AE, Pamuk G, Pamuk AE, Özer S, Jafarov S, Önerci TM (2017) Effects of expansion sphincter Pharyngoplasty on the apnea-hypopnea index and heart rate variability. J Oral Maxillofac Surg 75(12):2650–2657. https://doi.org/10.1016/j.joms.2017.06.005
Dal-Fabbro C, Garbuio S, D'Almeida V, Cintra FD, Tufik S, Bittencourt L (2014) Mandibular advancement device and CPAP upon cardiovascular parameters in OSA. Sleep Breath 18(4):749–759. https://doi.org/10.1007/s11325-014-0937-5
Kufoy E, Palma JA, Lopez J, Alegre M, Urrestarazu E, Artieda J, Iriarte J (2012) Changes in the heart rate variability in patients with obstructive sleep apnea and its response to acute CPAP treatment. PLoS One 7(3):e33769. https://doi.org/10.1371/journal.pone.0033769
Gula LJ, Krahn AD, Skanes A, Ferguson KA, George C, Yee R, Klein GJ (2003) Heart rate variability in obstructive sleep apnea: a prospective study and frequency domain analysis. Ann Noninvasive Electrocardiol 8(2):144–149
Coruzzi P, Gualerzi M, Bernkopf E, Brambilla L, Brambilla V, Broia V, Lombardi C, Parati G (2006) Autonomic cardiac modulation in obstructive sleep apnea: effect of an oral jaw-positioning appliance. Chest 130(5):1362–1368. https://doi.org/10.1378/chest.130.5.1362
Sumi K, Chin K, Takahashi K, Nakamura T, Matsumoto H, Niimi A, Mishima M (2006) Effect of nCPAP therapy on heart rate in patients with obstructive sleep apnoea-hypopnoea. QJM 99(8):545–553. https://doi.org/10.1093/qjmed/hcl074
La Rovere MT, Pinna GD, Hohnloser SH, Marcus FI, Mortara A, Nohara R, Bigger JT Jr, Camm AJ, Schwartz PJ, Tone AIA, Reflexes After Myocardial I (2001) Baroreflex sensitivity and heart rate variability in the identification of patients at risk for life-threatening arrhythmias: implications for clinical trials. Circulation 103(16):2072–2077. https://doi.org/10.1161/01.cir.103.16.2072
Hedner J, Darpo B, Ejnell H, Carlson J, Caidahl K (1995) Reduction in sympathetic activity after long-term CPAP treatment in sleep apnoea: cardiovascular implications. Eur Respir J 8(2):222–229. https://doi.org/10.1183/09031936.95.08020222
Mark AL, Victor RG, Nerhed C, Wallin BG (1985) Microneurographic studies of the mechanisms of sympathetic nerve responses to static exercise in humans. Circ Res 57(3):461–469. https://doi.org/10.1161/01.res.57.3.461
Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV (2004) Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 27(7):1255–1273. https://doi.org/10.1093/sleep/27.7.1255
Lee WH, Hong SN, Kim HJ, Rhee CS, Lee CH, Yoon IY, Kim JW (2016) A comparison of different success definitions in non-continuous positive airway pressure treatment for obstructive sleep apnea using cardiopulmonary coupling. J Clin Sleep Med 12(1):35–41. https://doi.org/10.5664/jcsm.5388
Lee WH, Wee JH, Lee CH, Kim MS, Rhee CS, Yun PY, Yoon IY, Kim JW (2013) Comparison between mono-bloc and bi-bloc mandibular advancement devices for obstructive sleep apnea. Eur Arch Otorhinolaryngol 270(11):2909–2913. https://doi.org/10.1007/s00405-013-2417-0
Tanyeri H, Polat S, Kirisoglu CE, Serin GM (2012) Long-term efficacy of submucosal uvulopalatopharyngoplasty for obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 269(9):2069–2074. https://doi.org/10.1007/s00405-011-1919-x
Brillante R, Cossa G, Liu PY, Laks L (2012) Rapid eye movement and slow-wave sleep rebound after one night of continuous positive airway pressure for obstructive sleep apnoea. Respirology 17(3):547–553. https://doi.org/10.1111/j.1440-1843.2012.02147.x
Koo BB, Wiggins R, Molina C (2012) REM rebound and CPAP compliance. Sleep Med 13(7):864–868. https://doi.org/10.1016/j.sleep.2012.03.019
Manzar MD, BaHammam AS, Hameed UA, Spence DW, Pandi-Perumal SR, Moscovitch A, Streiner DL (2018) Dimensionality of the Pittsburgh sleep quality index: a systematic review. Health Qual Life Outcomes 16(1):89. https://doi.org/10.1186/s12955-018-0915-x
Kendzerska TB, Smith PM, Brignardello-Petersen R, Leung RS, Tomlinson GA (2014) Evaluation of the measurement properties of the Epworth sleepiness scale: a systematic review. Sleep Med Rev 18(4):321–331. https://doi.org/10.1016/j.smrv.2013.08.002
Spiesshoefer J, Aries J, Giannoni A, Emdin M, Fox H, Boentert M, Bitter T, Oldenburg O (2019) APAP therapy does not improve impaired sleep quality and sympatho-vagal balance: a randomized trial in patients with obstructive sleep apnea and systolic heart failure. Sleep Breath 25:273–280. https://doi.org/10.1007/s11818-017-0124-6
Funding
This study was funded by 2019 Kangwon National University Hospital Grant (#2019-02-004), SNUBH grant (#18-2018-013), and the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (# NRF-2015M3A9D7066973).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The need for written informed consent was waived by the institutional review board. For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, W.H., Kwon, S.O. & Kim, JW. Effectiveness of sleep surgery versus a mandibular advancement device for obstructive sleep apnea in terms of nocturnal cardiac autonomic activity. Sleep Breath 24, 1695–1703 (2020). https://doi.org/10.1007/s11325-020-02048-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02048-7