Abstract
Purpose
Patients with obstructive sleep apnea (OSA) may experience apneas and hypopneas primarily during stage R (REM) sleep when end-expiratory lung volume (EELV) reaches its nadir. The purpose of this study was to determine if REM-related reductions in EELV persist in the presence of continuous positive airway pressure (CPAP) prescribed during non-stage REM (NREM) sleep.
Methods
We prospectively recruited 17 subjects referred to the sleep laboratory for CPAP titration. CPAP was titrated per AASM protocol to control respiratory events. The change in EELV was measured using magnetometry.
Results
Of the 17 subjects, 12 (71%) had moderate to severe OSA. Despite the application of CPAP, there was a significant reduction in EELV between NREM and REM sleep (− 105.9 ± 92.2 to − 325.0 ± 113.1 mL, respectively, p < 0.01). The change in EELV between non-stage R (NREM) and REM significantly correlated with overall apnea-hypopnea index (AHI) (r = 0.5, p = 0.04), the number of respiratory arousals during REM (r = 0.5, p = 0.04), and prescribed level of CPAP (r = 0.7, p < 0.01).
Conclusion
REM-related reductions in EELV are associated with worsening sleep disordered breathing and occur despite the presence of CPAP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a disease characterized by repetitive upper airway closure during sleep resulting in intermittent nocturnal hypoxemia, sleep fragmentation, hypercapnia, sympathetic activation, and impaired cardiac function due to the mechanical effects of more negative intrathoracic pressures. Sleep disordered breathing (SDB) is often most pronounced in the supine position or during stage R (REM) sleep [1]. Associated morbidities include hypertension, diabetes, myocardial infarction, atrial fibrillation, heart failure, and stroke [2]. Furthermore, moderate to severe OSA is an independent risk factor for all-cause mortality [3, 4].
Treatment of OSA with continuous positive airway pressure (CPAP) reduces the number of apneas and hypopneas and improves oxygenation during sleep [5]. CPAP counteracts airway collapse through two possible mechanisms: (1) increasing upper airway transmural pressure (pneumatic splinting of the upper airway) and (2) increasing end-expiratory lung volume (EELV) (increasing longitudinal traction of the upper airway). However, the amount of CPAP needed to reduce respiratory events during sleep is difficult to predict, varies from individual to individual, depends on body position, and the presence or absence of REM sleep.
We previously found a significant reduction in EELV during REM (stage R) compared to non-stage R sleep (NREM). In our prior study, individuals with moderate to severe OSA had greater reductions in EELV than those with no or mild OSA and the REM-related reductions in EELV became greater as body mass index (BMI) increased [6]. The reduction in EELV may worsen SDB by increasing pharyngeal critical closing pressure (Pcrit), leading to airway narrowing and eventual airway collapse during inspiration [7]. For the above reasons, we speculated that REM-related reductions in EELV may be one mechanism accounting for the predominance of SDB during REM noted in some individuals [8]. Two possible mechanisms related to central drive to the upper airway and respiratory muscles may account for the predominance of SDB with REM sleep: (1) REM-related hypotonia of the upper airway muscles would decrease upper airway compliance and make the upper airway more collapsible. (2) REM-related hypotonia of the rib cage muscles would reduce EELV and lessen radial traction of the lung on the upper airway thereby making the upper airway more collapsible. The purpose of this study was to determine if CPAP prescribed during NREM sleep eliminates the reduction in EELV during REM sleep. We hypothesized CPAP would eliminate the REM-related reduction in EELV and minimize SDB. Any residual SDB could then be attributed to REM-related reductions in upper airway muscle hypotonia.
Methods
Subjects
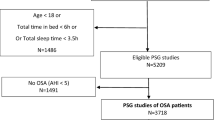
We prospectively enrolled 17 adult subjects who were previously diagnosed with OSA and referred to the sleep laboratory for overnight CPAP titration. They were recruited randomly during the night of polysomnography (PSG). Those who presented for baseline PSG were excluded from the study. The institutional review board at the Memorial Hospital of Rhode Island approved this study.
Polysomnography and magnetometry
The subjects presented at the sleep laboratory 2 h prior to the start of the study to complete paperwork. The sleep technologist utilized the American Academy of Sleep Medicine (AASM) protocols to attach all sensors and flow-measuring devices. The PSG was scored for sleep stage and respiratory events using the following AASM criteria: apneas were defined as a greater than 90% drop in the peak thermal sensor excursion lasting 10 or more seconds. Hypopneas were defined as a greater than 30% drop from baseline in nasal pressure lasting 10 or more seconds associated with a 4% or greater oxygen desaturation from pre-event baseline. The change in EELV (ΔEELV) was non-invasively measured using a custom-built magnetometer system as previously described and validated [9]. The magnetometer system consists of two pairs of magnetic coils that are first attached to the skin with micro-foam tape and then secured with hypoallergenic, silk tape. One pair of coils was attached to the chest above the xiphoid process and to the mid-upper back. The second pair of coils was attached 2 cm above the umbilicus and to the lower back. The flow meter connected to the magnetometer system was first calibrated with a 3-L calibration syringe. Next, the subject was requested to lie supine in bed and breathe through a flow meter at varying tidal volumes (five breaths at varied tidal volumes totaling 15 to 20 breaths). The magnetometer signals were sampled at a rate of 15 Hz. This was repeated for the right lateral and left lateral decubitus positions. This data was used to calculate coefficients for the following equation:
where α, β, and ϒ are coefficients for the rib cage (RC), the abdomen (Ab), and the axial displacement of the chest wall (Xi), respectively. Regression coefficients for Eq. 1 were determined for the supine, left, and right lateral decubitus positions. Magnetometer readings acquired during the overnight PSG were used post-acquisition to construct a spirogram of VT versus time.
After magnetometer calibration, the sleep technologist requested the subject to wear a CPAP mask to demonstrate comfortable fit. PSG data collection was initiated shortly after completion of the magnetometer calibration process and selecting the best fitting CPAP mask. Data recording continued until the completion of the PSG in the morning. CPAP pressure was set to start at 5 cm of water. The sleep technologist increased the pressure as needed throughout the night to reduce respiratory events, such as snoring, apneas, and hypopneas per AASM protocol. Data recording for both PSG and magnetometry continued for the full night of sleep.
Epochs of sleep with acceptable magnetometer signals were selected for each subject. Position-specific regression coefficients were applied to the matching magnetometer segment, and magnetometer derived values of VT were used to construct a spirogram. As subjects were instructed to sleep in the supine position, this was the position from which the vast majority of data was acquired. ∆EELV for each breath was calculated as the difference between the EELV at sleep onset and the EELV for subsequent breaths. The total number of observations (breaths) varied across subjects and sleep stage. Mean ∆EELV and standard deviation for each sleep stage were calculated from the selected magnetometer segment for each subject. The CPAP pressure applied during the corresponding PSG and magnetometer segments was recorded.
Pulmonary function testing
All subjects were scheduled for pulmonary function testing shortly before or after completing their CPAP titration study. Forced vital capacity (FVC) was determined in the seated position using a rolling seal spirometer (Collins Medical; Braintree, MA/ Ferraris Comprehensive Pulmonary Laboratory; Louisville, CO), and functional residual capacity (FRC) was determined by body plethysmography according to the American Thoracic Society/European Respiratory Journal guidelines [10].
Statistical analyses
Mean ΔEELV ± standard deviation was calculated for each sleep stage. The category of NREM sleep was defined as the mean of the mean ΔEELV for sleep stages N1, N2, and N3. Welch analysis of variance was used to compare the means across sleep stages. To account for multiple comparisons, Tukey–Kramer adjustment was performed post hoc.
Pearson correlation was used to determine the linear association of ΔEELV during NREM and REM sleep and the following measurements: BMI, neck circumference, apnea-hypopnea index (AHI), prescribed positive airway pressure, respiratory arousals during REM, and FRC during wakefulness. To determine the statistical significance of mean ΔEELV and of the number of respiratory events between NREM and REM, we performed an unpaired, two-sample t test with equal variance for each comparison. A two-tailed p value of < 0.05 was considered to be significant.
All statistical analyses were performed using Stata 13.0 SE (StataCorp LP, College Station, TX).
Results
Baseline characteristics and EELV of the 17 subjects who presented for CPAP titration are presented in Table 1 and Table 2. We recruited 12 males and 5 females. The cohort on average was obese, had a large neck size, and had severe OSA. The seated FRC was 2.32 ± 0.5 L (mean ± SD). Out of the 17 subjects, 12 (71%) had moderate to severe OSA. CPAP was increased during REM in 9 of 17 subjects.
The change in EELV during sleep stages N1, N2, N3, and REM was − 62.7 ± 62.9 mL, − 117.8 ± 92.1 mL, − 321.2 ± 52.7 mL, and − 325.0 ± 113.1 mL, respectively. The reduction in EELV during REM was significantly greater than the reduction in EELV for all NREM stages combined (− 325.0 ± 113.1 mL vs − 105.9 ± 92.2 mL, respectively, p < 0.01) (Fig. 1). There were more respiratory arousals during REM (16.6 ± 22.0 events per hour) compared to NREM (4.8 ± 13.3 events per hour), but the difference was not statistically significant (p = 0.07). However, the difference in EELV between NREM and REM strongly correlated with respiratory arousals during REM (r = − 0.5, p = 0.04) (Fig. 2), baseline AHI (r = − 0.5, p = 0.04) (Fig. 3) and the level of prescribed CPAP (r = 0.7, p < 0.01) (Fig. 4). The difference in EELV between NREM and REM sleep did not correlate with BMI, neck circumference, or seated FRC.
Discussion
Changes in EELV are important in the pathogenesis and treatment of OSA. Variations in EELV during REM in OSA subjects who are treated with CPAP have not been previously described. We found that EELV significantly decreased from NREM to REM sleep despite the presence of CPAP. The reduction in EELV in REM sleep was associated with an increased frequency of arousals during REM, an increase in overall AHI, and the need for higher levels of CPAP. Thus, REM-related reductions in EELV may play a role in worsening SDB and increasing CPAP requirements.
During REM sleep, central drive to the upper airway and chest wall muscles is reduced [11]. A reduction in central drive to upper airway muscles has the direct effect of reducing upper airway muscle tone and rending the upper airway more collapsible. A reduction in central drive to the chest wall muscles can indirectly affect upper airway collapsibility by causing atonia of rib cage muscles. A marked reduction in rib cage muscle tone reduces passive outward recoil of the chest wall thereby lowering EELV. A reduced EELV, in turn, decreases radial traction on the upper airway making it more collapsible. CPAP eliminates SDB by increasing intra-airway pressure (pneumatic splinting of the upper airway) and by increasing intra-alveolar pressure (increasing EELV). We found that the level of CPAP during non-REM sleep was inadequate to prevent reductions in EELV during REM sleep. A PSG technician typically follows AASM guidelines and will increase CPAP to eliminate snoring and SDB. Our finding is a significant association between the change in EELV and final prescribed CPAP pressure support the notion that SDB worsens as EELV decreases. Because CPAP did not eliminate the REM-related reduction in EELV, we cannot distinguish between the effect of CPAP on providing a pneumatic splint for the upper airway and its effect stabilizing the upper airway by increasing radial traction. However, the positive associations between the magnitude of reduction in EELV and respiratory-related arousals during REM and the association between the reduction in EELV and the final CPAP pressure prescribed indicate that changes in EELV importantly affect SDB.
In our previous study evaluating changes in EELV during sleep, we found that untreated OSA subjects had, approximately, a 300-mL reduction in EELV during REM sleep. We would expect this reduction in EELV would be less in the presence of CPAP. However, we found similar reductions in EELV during REM sleep in our current study. One explanation for this may be differences in study populations. In the current study, most subjects had moderate to severe OSA whereas in the prior study, most subjects had mild or no OSA. Since the reduction in EELV would be greater in those with more severe OSA [6], the observation that EELV was reduced to a similar degree in both studies suggests that CPAP mitigated further reductions in EELV in the cohort of individuals with more severe SDB. Furthermore, the strong correlation between ∆EELV from NREM and REM and AHI in this study provided support for this premise. Therefore, it is possible that in the absence of CPAP, we may have seen a greater REM-related reduction in EELV in the current study subjects with more severe OSA.
End-expiratory lung volume can be increased either by applying CPAP or by lowering extra-thoracic pressure. Heinzer et al. increased EELV by using a rigid head-out shell in which extrathoracic pressure could be manipulated to change EELV [12]. When EELV was increased by decreasing extrathoracic pressure, markers of SDB, including AHI, 3% oxygen desaturation index, and arousal index, all improved as lung volume increased. These findings suggest that increasing EELV plays a role in reducing upper airway collapse. In our study, we found that when EELV is reduced in REM sleep, subjects required an increase in CPAP pressures. This finding is consistent with the observation by Heinzer et al. that AHI is increased at lower EELV [12].
When compared to subjects with no SDB or mild OSA, a population of subjects with moderate to severe OSA is expected to be more obese, have larger neck circumference, and have a lower-seated FRC due to larger abdominal girth [13]. However, in the presence of CPAP, we did not find an association between BMI, neck circumference, or seated FRC (% predicted) with baseline AHI or REM-related reductions in EELV. This observation suggests that CPAP may attenuate these associations by blunting REM-related reductions in EELV.
The clinical relevance of our findings includes noting the importance of achieving REM sleep when determining optimal CPAP. This finding supports the use of polysomnography to determine REM sleep when initiating patients with OSA on CPAP therapy. To extend this consideration further, an automatic titrating CPAP device (auto CPAP) may potentially deliver an inadequately low range of pressures resulting in persistent REM-related SDB. Clinicians may consider referring individuals with residual daytime sleepiness who were titrated and treated with auto CPAP for polysomnography to determine if SDB has been adequately treated in REM sleep.
Limitations
There are some limitations to our study. First, due to the severity of OSA, most of the subjects did not have REM sleep until near the end of the titration study when higher levels of CPAP were delivered. Per AASM protocol, our PSG technicians did not lower CPAP during REM to levels that were used at the beginning of the titration study. Thus, we could not determine if EELV would have been further reduced during REM at lower levels of CPAP. For similar reasons, we could not measure the reduction in EELV during REM at the same level of CPAP for all subjects. This limitation in controlling for potentially confounding variables reflects the “real world” circumstances of clinical CPAP titration studies. Second, our study population primarily consisted of subjects who had moderate to severe OSA. Our findings may not be applicable to those with mild OSA. The reduction in EELV during REM may be less or be completely negated in the presence of CPAP in those with mild OSA. Third, our PSG technicians instruct our subjects to sleep in the supine position. Thus, only supine REM was analyzed. We have insufficient data to determine if there are similar REM-related changes in EELV in other body positions. Finally, baseline AHI in NREM was not available. The reduction in EELV with REM-related OSA may affect airway collapsibility differently compared to NREM-related OSA.
Conclusions
We are the first to describe changes in EELV during REM sleep in the presence of CPAP; specifically, EELV further decreases during REM when compared to non-REM sleep. Thus, it is important to achieve REM sleep during CPAP titration studies when determining optimal levels of CPAP. In addition, our finding of an association of REM-related reductions in EELV and worsening AHI supports prior studies highlighting the important relationship between EELV and SDB.
Abbreviations
- AASM:
-
American Academy of Sleep Medicine
- Ab:
-
Abdomen
- AHI:
-
Apnea-hypopnea index
- auto CPAP:
-
An automatic titrating CPAP device
- BMI:
-
Body mass index
- CPAP:
-
Continuous positive airway
- ΔEELV:
-
Change in end-expiratory lung volume
- EELV:
-
End-expiratory lung volume
- FRC:
-
Functional residual capacity
- NREM:
-
Non-stage R sleep
- OSA:
-
Obstructive sleep apnea
- Pcrit:
-
Pharyngeal critical pressure
- PSG:
-
Polysomnography
- RC:
-
Rib cage
- REM:
-
Stage R/rapid eye movement sleep
- SDB:
-
Sleep-disordered breathing
- Stage R:
-
REM sleep
- VT:
-
Tidal volume
- Xi:
-
Axial displacement
References
Hudgel DW, Devadatta P (1984) Decrease in functional residual capacity during sleep in normal humans. J Appl Physiol 57:1319–1322
Young T, Peppard PE, Gottlieb DJ (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165(9):1217–1239
Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR (2008) Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 31(18):1079–1085
Young T, Finn L, Peppard PE, Szkio-Coxe M, Austin D, Nieto FJ, Stubbs R, Hla KM (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31(8):1071–1078
Gay P, Weaver T, Loube D, Iber C (2006) Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep 29(3):381–401
Koo P, Gartman EJ, Sethi JM, Kawar E, McCool FD (2017) Changes in end-expiratory lung volume during sleep in patients at risk for obstructive sleep apnea. J Clin Sleep Med 13(8):941–947
Squier SB, Patil SP, Schneider H, Kirkness P, Smith PL, Schwartz AR (2010) Effect of end-expiratory lung volume on upper airway collapsibility in sleeping men and women. J Appl Physiol 109(4):977–985
Neilly JB, Gaipa EA, Maislin G, Pack AI (1991) Ventilation during early and late rapid-eye-movement sleep in normal humans. J Appl Physiol 71(4):1201–1215
McCool FD, Wang J, Ebi KL (2002) Tidal volume and respiratory timing derived from a portable ventilation monitor. Chest 122(2):684–691
Wagner J, Clausen JL, Coates A et al (2005) Standardisation of the measurement of lung volumes. Eur Respir J 26(3):511–522
Penzel T, Wessel N, Riedl M, Kantelhardt JW, Rostig S, Glos M, Suhrbier A, Malberg H, Fietze I (2007) Cardiovascular and respiratory dynamics during normal and pathological sleep. Chaos 17:015116. https://doi.org/10.1063/1.2711282
Heinzer RC, Stanchina ML, Malhotra A, Jordan AS, Patel SR, Lo YL, Wellman A, Schory K, Dover L, White DP (2006) Effect of increased lung volume on sleep disordered breathing in patients with sleep apnoea. Thorax 61(5):435–439
Jones RL, Nzekwu MM (2006) The effects of body mass index on lung volumes. Chest 130(3):827–833
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
All authors have seen and approved the manuscript.
Work for this study was performed at Alpert Medical School of Brown University, Memorial Hospital of Rhode Island.
Conflict of interest
The authors declare that they have no conflict of interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koo, P., Gartman, E.J., Sethi, J.M. et al. End-expiratory lung volume decreases during REM sleep despite continuous positive airway pressure. Sleep Breath 24, 119–125 (2020). https://doi.org/10.1007/s11325-019-01857-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01857-9