Abstract
Introduction
Non-traumatic osteonecrosis of the femoral head (NTONFH) is a progressive disease, always leading to hip dysfunction if no early intervention was applied. The difficulty for early diagnosis of NTONFH is due to the slight symptoms at early stages as well as the high cost for screening patients by using magnetic resonance imaging.
Objective
The aim was to detect biomarkers of early-stage NTONFH, which was beneficial to the exploration of a cost-effective approach for the early diagnose of the disease.
Methods
Metabolomic approaches were employed in this study to detect biomarkers of early-stage NTONFH (22 patients, 23 controls), based on the platform of ultra-performance liquid chromatography tandem quadrupole time-of-flight mass spectrometry (UPLC-QTOF-MS) and the uses of multivariate statistic analysis, putative metabolite identification, metabolic pathway analysis and biomarker analysis.
Results
In total, 33 serum metabolites were found altered between NTONFH group and control group. In addition, glycerophospholipid metabolism and pyruvate metabolism were highly associated with the disease.
Conclusion
The combination of LysoPC (18:3), l-tyrosine and l-leucine proved to have a high diagnostic value for early-stage NTONFH. Our findings may contribute to the protocol for early diagnosis of NTONFH and further elucidate the underlying mechanisms of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Osteonecrosis of the femoral head is a progressive disorder that can lead to femoral head collapse and hip dysfunction (Gangji et al. 2004). Although traumatic osteonecrosis of the femoral head has a direct cause, the pathophysiology is uncertain for most cases which are generally called non-traumatic osteonecrosis of the femoral head (NTONFH). Risk factors for osteonecrosis include corticosteroids use, alcohol intake, smoking, and several chronic diseases, etc (Mont et al. 2006). Despite NTONFH can be induced by various individual or multiple causes, the prognosis is not closely related to its subtype unless some idiopathic diseases accompanied, but hugely dependent on the stage of the disease and whether early intervention is applied (Mont et al. 2010). Treatments for early-stage NTONFH with core decompression or autologous implantation of mesenchymal stem cells turn out to be effective in delaying or avoiding femoral head collapse (Floerkemeier et al. 2011; Zhao et al. 2012), while patients have to be faced with total hip arthroplasty once it progresses to advanced or end stage. There is therefore an urgent need for early diagnosis in order to undertake relevant actions to prevent further progression.
The diagnosis of NTONFH is primarily based upon imaging findings (Choi et al. 2015). Plain radiographs are commonly obtained, but magnetic resonance imaging (MRI) is now considered the best diagnostic approach as it has highest sensitivity and specificity for the early-stage osteonecrosis (Pierce et al. 2015; Zalavras and Lieberman 2014). However, the high costs and complexities make it unrealistic to perform MRI for all patients with less-severe symptoms or signs, which have led to an increasing probability of missed diagnosis. Fortunately, meaningful proteins found in serums of NTONFH patients indicated that the involved might be discriminated by detecting some specific substances which were significantly different in individuals with or without NTONFH (Tan et al. 2006; Wu et al. 2008).
Rapid developments in metabolomics have renewed hopes in discovering blood-borne biomarkers for early detection of diseases. As one of the most widely used technologies of metabolomics, ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS) technique, with high sensitivity, good reproducibility of retention time, wide dynamic range, and coverage of a wide chemical diversity (Zhao et al. 2012), has been proved appropriate for metabolic profiling. Based on the platform of UPLC-MS/MS, this serum metabolomic study was aimed to exploit potential serum molecular biomarkers of early-stage NTONFH, which might contribute to the protocol of early diagnosis of NTONFH.
2 Materials and methods
2.1 Chemical and materials
HPLC-grade methanol was purchased from Tedia (Fairfield, OH, USA); HPLC-grade acetonitrile and formic acid were purchased from Sigma-Aldrich (St.Louis, MO, USA). Ultrapure water was acquired by a Milli-Q Ultra-pure water system (Millipore, Billerica, USA). All of the involved standards were purchased from MCGBW (Beijing, China). Pressure blowing concentrator MTN-2800D was manufactured by AUTO & SCIENCE (Tianjing, China).
2.2 Study participants
The study subjects consisted of 50 outpatients and 25 volunteers. Patients diagnosed with NTONFH and healthy controls were respectively recruited from Orthopaedic Outpatient Department and Health Examination Center, the First Affiliated Hospital of Chongqing Medical University between December 23rd, 2015 and April 22nd, 2016. Diagnostic criteria for NTONFH were according to the recommended standards for Japanese population (Sugano et al. 1999), and the stage of the disease was based on the modified Ficat-Arlet classification of osteonecrosis of the femoral head (Banaszkiewicz 1985). Erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), X-ray of pelvis, and MRI of both hip joints were performed in all of the participants. Inclusive criteria for NTONFH group were as followed: (1) diagnosed with osteonecrosis of the femoral head; (2) no history of hip trauma; (3) staged between 0 and II using Ficat-Arlet classification; (4) not any inflammatory arthritis complicated (e.g., rheumatic arthritis); (5) not any metabolic disease complicated (e.g., rickets); (6) no drug taken in last 4 weeks. Inclusive criteria for control group were as followed: (1) never suffered from hip pain or dysfunction; (2) no osteonecrosis or any other joint diseases observed on radiographs or MRI scans; (3) with normal values of ESR and CRP; (4) not any inflammatory or metabolic disease complicated. Finally, there were 22 NTONFH patients and 23 healthy controls eligible to be included under above criteria.
This study was approved by the Ethics Committee of Chongqing Medical University. Written informed consents were obtained from all participants. This work was in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
2.3 Sample preparation
Blood samples (2-mL) were collected using vacuum tubes without any coagulants or anticoagulants. General information of all participants was recorded simultaneously. After 30-min standing at 4 °C, samples were centrifuged at 3000 rpm for 10 min and then serums were obtained and stored at −80 °C. Before extraction, serums were thawed at 4 °C for 60 min and 200-μL aliquots of them were transferred into 2-mL microtubes. Acetonitrile (600-μL for each) was added to precipitate proteins. Subsequently, the mixtures were vortex-mixed at 4 °C for 2 min, incubated at −20 °C for 30 min, and then centrifuged at 10,000 rpm for 10 min. Supernate (400-μL for each) was transferred to new microtubes and blow-dried under continuous nitrogen at 40 °C, and then ultrapure water (200-μL for each) was added to redissolve dried samples. Solutions were further centrifuged at 12,000 rpm for 10 min and then supernate (60-μL for each) was transferred into auto-sampler vials. A mixture of all samples (20-μL for each) constitutes a quality-control (QC) sample.
2.4 UPLC-MS/MS analysis
UPLC-QTOF-MS/MS analysis was performed by using a Shimadzu UFLC-equipped AB-Sciex Triple TOF 4600 mass spectrometry in both positive and negative ionization mode using the Turbo V ESI ion source. Samples were injected into a Kinetex XB-C18 column (100 mm × 2.1 mm, 2.6 µm, Phenomenex) and a Kinetex HILIC column (100 mm × 2.1 mm, 2.6 µm, Phenomenex) respectively with a same flow rate of 0.35 mL/min. The mobile phase for reversed phase liquid chromatography (RPLC) methods consisted of 0.1% formic acid in purified water and 0.1% formic acid in purified acetonitrile. The constituent ratio of the mobile phase was according to formic acid acetonitrile solution which was changed by time (held constant at 5% for 1 min, increased from 5 to 85% by 8 min, held constant at 85% by 12 min, decreased to 5% by 12.1 min, held constant at 5% by 15 min). The mobile phase for hydrophilic interaction liquid chromatography (HILIC) methods consisted of acetonitrile and ammonium acetate/acetic acid, and the latter was changed by time (held constant at 5% for 1 min, increased from 5 to 30% by 2 min, increased from 30 to 40% by 10 min, returned to 5% by 12.1 min, and held constant at 5% by 15 min). The ion spray voltage was set to 5500 V for ESI (+) and −4500 V for ESI (−). The nebulizer gas (air) and turbo gas (air) were set to 55 psi, and the heater temperature was set at 600 °C. The curtain gas (nitrogen) was set at 25 psi, and the rolling collision energy was set at (40 ± 15) V for positive ion mode and (−40 ± 15) V for negative ion mode. Full scan analysis was performed in the electrospray ionization mass spectrometry mode using electrospray ionization technique with coverage of mass ranged 50 to 1000 Da by using scan rate of 0.25 s, and the MS/MS screening was accomplished in the combinational mode of information dependent acquisition with a scan rate of 0.1 s. Ten QCs (10-μL for each) were successively injected to adjust and guarantee the system’s consistency, and then 10-µL aliquot of each experimental sample was injected to analyze in turn. One QC was used to estimate system reproducibility and one blank was used to flush the column after each five samples injected (Dunn et al. 2012). Experimental samples analyzed in same ion mode were completed continuously to decrease inter-day error, and same QC samples were analyzed in same ion mode throughout the whole procedure.
2.5 Data analysis
All of the raw data were initially processed and normalized by Markerview software (version 1.2.1, ABScix). Features detected in more than 80% samples in either group were selected for multivariate statistical analysis by simca-P software (version 13.0, Umetrics) (Bijlsma et al. 2006). Unsupervised principal component analysis (PCA) was employed to depict an overview of the two groups after pareto scaling. Supervised orthogonal partial least-squares discriminant analysis (OPLS-DA) was applied to model all features (peaks of intensity) of the two groups, and the sevenfold cross-validation was carried out to avoid overfitting. Model parameters were adjusted repeatedly to ensure that the models were both appropriate and predicable, and permutation tests were performed to further validate the OPLS-DA models by simca-P software (version 14.1, Umetrics) (Triba et al. 2015). Values of variable important in the projection (VIP) of all variables were exported from the best fitted OPLS-DA models. In addition, univariate statistical analysis was performed by using Wilcoxon rank sum test with a statistical significance of 0.05 (Diaz et al. 2011), and Bonferroni correction was adopt to reduce false positives (Vashi et al. 2016). Variables with both multivariate statistical significance (VIP >1) and univariate statistical significance (P < 0.05) were considered markedly different between the two groups (Gao et al. 2016; Tan et al. 2013; Zhao et al. 2009).
Potential altered variables were putatively identified by matching them with known substances acquired from databases of endogenous metabolites (HMDB, http://www.hmdb.ca/; Massbank, http://www.massbank.jp), and those failed to match any known metabolite were deleted while matched ones were further validated by using standards. Validated altered metabolites were selected for pathway analysis by searching KEGG database (http://www.kegg.jp/) and MetaboAnalyst database (http://www.metaboanalyst.ca/). In addition, receiver operating characteristic (ROC) curve analysis was utilized to determine the diagnostic value of the above metabolites, and when the area under curve (AUC) was much closer to 1, the diagnostic performance was better.
3 Results
3.1 Clinical characteristics
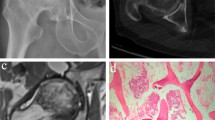
There were 23 NTONFH patients and 22 healthy controls included eventually with 27 patients (21 classfied Ficat III or IV, four influenced by recent NSAIDs intake, one accompanied with rheumatoid arthritis, and one with uncertain history of trauma) and three controls (with abnormal levels of both ESR and CRP) excluded. No statistical significance was detected in terms of age (NTONFH 51.86 ± 12.2, control 53.43 ± 16.78, p = 0.72), sex (NTONFH 16M + 6F, control 15M + 8F, p = 0.75), or BMI (NTONFH 23.23 ± 3.27, control 24.53 ± 3.64, p = 0.22) between the two groups. Image manifestations of the two groups were displayed in Fig. 1.
3.2 Stability evaluation
The stability and repeatability of the tandem instruments was evaluated by performing PCA analysis and calculating relative standard deviations (RSDs) including all QC samples which were from the same vial and analyzed repeatedly throughout the process. Variations within QC samples analyzed in same ion mode reflected the instability of the instruments which must be controlled within a permissible range. PCA analysis showed that QC samples clustered together significantly but other samples scattered over a large area (Fig. 2). The maximum values of RSDs of the four ion modes were respectively 6.29%, 9.05%, 4.11%, and 7.83%, which were calculated by using a random sampling strategy. Both results revealed a good repeatability and stability of the instruments.
3.3 Data processing
Variable features between the two groups were picked out by using multivariate statistical analysis combined with univariate statistical analysis. PCA analysis of the four ion modes was firstly carried out (Fig. S1), but no significant difference was found in sample distribution. In Fig. 3, NTONFH samples and healthy controls were significantly distinguished in all ion modes by using OPLS-DA analysis. With R2 and Q2 both scoring more than 0.5, the four models were further evaluated by permutation tests and proved valid (Fig. S2, 999 permutations, one component). Variables with VIP >1 in the validated OPLS-DA models were exported, and then Wilcoxon rank sum test was carried out to determine univariate statistical significance of the variables. Finally, the metabolic variations were putatively identified based on the results of MS match, MS/MS match, and standard match. In total, 33 variations were identified matching well with known metabolites (Table 1). A heatmap including all these substances was performed and displayed in Fig. 4.
3.4 Metabolic pathway analysis
Pathway analysis including all of the identified metabolites showed that two pathways were associated with the serum variation of NTONFH (Fig. S3). Both glycerophospholipid metabolism and pyruvate metabolism achieved a high pathway impact (>0.1) of enrichment analysis and a low P value (<0.05) of topology analysis. A list of the first four pathways was showed in Table S1.
3.5 Biomarker analysis
All of the altered metabolites were analyzed individually by using ROC curve in Metaboanalyst (http://www.metaboanalyst.ca). A metabolite was regarded as a potential biomarker for NTONFH when its corresponding AUC was not <0.8. To obtain a high diagnostic value, a combination of three biomarkers [LysoPC (18:3), l-tyrosine and l-leucine] was proposed and an overall ROC analysis was performed (Fig. 5a). The results of the three individual biomarkers were displayed in Fig. 5b–d, and the results of remaining biomarkers were showed in Fig. S4.
4 Discussion
Numerous metabolomic studies were proved significantly helpful to determine diagnostic biomarkers and to study metabolic mechanisms of diseases (Beauclercq et al. 2016; RoyChoudhury et al. 2016; Zafeiridis et al. 2016). This study was carried out based on the platform of UPLC-MS/MS as well as the accepted methodology of substance selecting and identifying. In total, 33 metabolic variations and two pathways were identified associated with the serum metabolic changes of NTONFH. Glycerophospholipid metabolism and pyruvate metabolism were found relevant to the progressive and irreversible disease. The combination of LysoPC(18:3), l-tyrosine and l-leucine had a high diagnostic value among these metabolites.
Glycerophospholipids, the overwhelming majority of the metabolic variations, were essential in constituting cell membranes and mediating signal transduction (Castro-Gomez et al. 2015). Phosphatidylcholines (PC) are ubiquitous in nature and are key components of the lipid bilayer of cells, as well as being involved in metabolism and signaling, and lysophospholipids (LysoPC) have a role in lipid signaling by acting on lysophospholipid receptors. Apoptosis was always accompanied by changes in the composition of glycerophospholipids in various cells (Farooqui et al. 2007; Fuchs et al. 2007; Lee et al. 2006), and the widespread programmed cell death of osteoblasts and osteocytes was observed in steroid- and alcohol-induced osteonecrosis patients (Calder et al. 2004). It was therefore reasonable that many kinds of glycerophospholipids were detected altered in the serums of NTONFH patients. Specifically, a cell experiment uncovered that LysoPC could induce a cytotoxicity effect on osteoblast-like cells by the involvement of transient receptor potential vanilloid 2 channels (Fallah et al. 2013), which implied that the elevated lysoPC due to NTONFH might further inhibit the bone regeneration of the necrosis area.
Three amino acids were detected elevated in the early-stage NTONFH patients’ serums, which was in accordance with the results of our previous study on bone tissues of advanced NTONFH patients (Zhu et al. 2016). The first elevated amino acid was l-tyrosine which was critical for the activity of tyrosine kinases and phosphatases, involved in the control of osteoblast and osteocyte metabolism (Pallu et al. 2012). Protein tyrosine kinase activation proved, in genetic studies, to be associated with alcoholism that could increase the risk of NTONFH (Pastor et al. 2009; Schumann et al. 2003), while receptor tyrosine kinase was found positive in osteoblast differentiation in vivo and bone formation ex vivo (Liu et al. 2007). Animal experiments showed protein tyrosine phosphatases were essential to osteoblast differentiation and bone formation as well (Chengalvala et al. 2001; Schinke et al. 2008). The other two amino acids were branched chain amino acids (BCCAs), l-leucine and l-valine. They had different metabolic routes, with valine going solely to carbohydrates and leucine solely to fats. Leucine could stimulate insulin release, which in turn stimulate protein synthesis and inhibit protein breakdown. Small leucine-rich proteins were considered as a kind of mineralized tissue-specific protein complicated in controlling collagen fibrillogenesis, matrix mineralization and osteoblast differentiation (Chen et al. 2004; Mochida et al. 2011; Sugars et al. 2013). Similarly, the substitution from some amino acids to valine in receptor-related proteins would achieve a higher bone mass in mutants than controls (Akhter et al. 2004; Kasten et al. 2010), indicating that valine was also related to bone formation. In addition, over-expression of a tripeptide of leucine-proline-valine could stimulate the export of secretory dentin matrix protein 1 which played a role in bone homeostasis because of its high calcium ion-binding capacity (Liang et al. 2016; Toyosawa et al. 2001). Therefore, the above three amino acids, detected elevated in NTONFH patients’ serums as well as bone tissues, all turned out to be highly associated with the progressive disease of osteonecrosis, especially in osteoblast differentiation. However, the remaining amino acids found altered in bone tissues were not detected increased or decreased in serums as before. This could result from the different stages of the disease, substances being metabolized in situ, or they being limited to pass through the blood capillaries.
There were three of the other altered metabolites recognized to be associated with energy metabolism, palmitoylcarnitine, l-lactic acid and l-acetic acid. The disturbance in energy metabolism resulting from ischemic insult could contribute to the occurrence and development of osteonecrosis (Dai et al. 2008). Palmitoylcarnitine is a kind of long-chain acyl fatty acid derivative ester of carnitine that facilitates the transfer of long-chain fatty acids from cytoplasm into mitochondria during the oxidation of fatty acids. So the up-regulated oxidation of fatty acids induced by the elevated palmitoylcarnitine could be aimed to guarantee sufficient energy supply for tissues, possibly due to the abnormality of carbohydrate metabolism which was reflected by the excess lactic acid being detected, and meanwhile, more pyruvic acid was generated. The accumulation of pyruvic acid would facilitate the conversion to lactic acid under hypoxia condition, leading to the overproduction of lactic acid again. Acetic acid is central to the metabolism of carbohydrates and fats when bound to coenzyme A, and the decrease of the metabolite will be discussed later.
Pathway analysis revealed potential relation between NTONFH and two pathways, glycerophospholipid metabolism and pyruvate metabolism. In glycerophospholipid metabolism, phosphatidylethanolamine (PE) and PC both played an important role with either value of pathway impact larger than 0.1. However, the composition of glycerophospholipids always changed significantly in various diseases (Lin et al. 2016; Peterson et al. 2016; Rao et al. 2016), leading to a relatively low specificity of PEs or PCs. In pyruvate metabolism, l-lactic acid could be converted into d-lactic acid, pyruvic acid, and acetic acid. Over-produced l-lactic acid that might derive from partly ischemia femoral head indicated that early-stage NTONFH tissues could have been suffering from insufficient oxygen supply. The elevated lactic acid and decreased acetic acid suggested that the process of indirect conversion (from lactic acid to pyruvic acid to acetic acid) could be inhibited, as the direct one required specific enzymes that human lacked of. In addition, much acetic acid could be utilized to generate enough acetyl-CoA.
According to the above evidences, we proposed a combination of serum LysoPC(18:3), l-tyrosine and l-leucine to serve as an early-diagnosis strategy for NTONFH after integrating the sensitivity and specificity of individual biomarkers, the overall diagnostic yield, and the economic cost. The scheme required a simplified process of sample preparation, followed by HILIC only, for the three biomarkers were all detected by using HILIC column. To validate the value of the scheme, 20 new participants (ten patients and ten controls) were recruited and their serums were analyzed by using HILIC-MS/MS under the same experimental condition. A sensitivity of 0.9 and a specificity of 1.0 were achieved when adopting the strategy that all of the three biomarkers should be in accordance with their profiles in the previous two groups. However, there were still some limitations in this study. First, all of the samples were collected and stored at −80 °C for analyzing within limited days to guarantee a high stability of the instruments, so that some of them had to be stored for a relatively long time. Second, the sample size was small. It was because that the symptom of early-stage NTONFH was not severe enough to force patients to go to hospital, and a MRI scan was too costly to be contained in a routine physical examination. Therefore few patients were qualified to be recruited even though more than 200 patients were engaged daily in our department. Third, the putative process could be faulty as no approach for structure identification was applied. Lastly, the metabolic profiles of NTONFH migh share some in common with other chronic diseases, but we were unable to collect various kinds of serums of patients suffering these diseases and then distinguish them by using metabolomic approaches. Thus, more studies were needed to identify the results and to further optimize the diagnostic scheme.
5 Conclusions
In this UPLC-MS/MS based metabolomic study, NTONFH serums showed different profiles from controls, which might provide us with a feasible approach to pick out underlying biomarkers for the early diagnosis of the disease. There were 33 substances detected altered in serums of NTONFH patients, and among these, LysoPC(18:3), l-tyrosine and l-leucine were found elevated significantly. The combination of the three biomarkers had also achieved a high diagnostic value. In addition, glycerophospholipid metabolism and pyruvate metabolism were found highly associated with early-stage NTONFH, especially in osteoblast differentiation and anaerobic metabolism.
References
Akhter, M. P., et al. (2004). Bone biomechanical properties in LRP5 mutant mice. Bone, 35, 162–169. doi:10.1016/j.bone.2004.02.018.
Banaszkiewicz, P. A. (1985). Idiopathic bone necrosis of the femoral head. early diagnosis and treatment. Journal of Bone & Joint Surgery British, 67, 3–9.
Beauclercq, S., et al. (2016). Serum and muscle metabolomics for the prediction of ultimate pH, a key factor for chicken-meat quality. Journal of Proteome Research, 15, 1168–1178. doi:10.1021/acs.jproteome.5b01050.
Bijlsma, S., et al. (2006). Large-scale human metabolomics studies: A strategy for data (pre-) processing and validation. Analytical Chemistry, 78, 567–574. doi:10.1021/ac051495j.
Calder, J. D., Buttery, L., Revell, P. A., Pearse, M., & Polak, J. M. (2004). Apoptosis–a significant cause of bone cell death in osteonecrosis of the femoral head. The Journal of Bone and Joint Surgery. British Volume, 86, 1209–1213.
Castro-Gomez, P., Garcia-Serrano, A., Visioli, F., & Fontecha, J. (2015). Relevance of dietary glycerophospholipids and sphingolipids to human health. Prostaglandins, Leukotrienes, and Essential Fatty Acids, 101, 41–51. doi:10.1016/j.plefa.2015.07.004.
Chen, X. D., Fisher, L. W., Robey, P. G., & Young, M. F. (2004). The small leucine-rich proteoglycan biglycan modulates BMP-4-induced osteoblast differentiation. FASEB J, 18, 948–958. doi:10.1096/fj.03-0899com.
Chengalvala, M. V., et al. (2001). Biochemical characterization of osteo-testicular protein tyrosine phosphatase and its functional significance in rat primary osteoblasts. Biochemistry, 40, 814–821.
Choi, H. R., Steinberg, M. E., & Cheng, E. Y. (2015). Osteonecrosis of the femoral head: Diagnosis and classification systems. Current Reviews in Musculoskeletal Medicine, 8, 210–220. doi:10.1007/s12178-015-9278-7.
Dai, X. L., et al. (2008). Association analysis of tissue factor pathway inhibitor polymorphisms and haplotypes with osteonecrosis of the femoral head in the Korean population. Molecules and Cells, 26, 490–495.
Diaz, S. O., et al. (2011). Metabolic biomarkers of prenatal disorders: An exploratory nmr metabonomics study of second trimester maternal urine and blood plasma. Journal of Proteome Research, 10, 3732–3742.
Dunn, W. B., Wilson, I. D., Nicholls, A. W., & Broadhurst, D. (2012). The importance of experimental design and QC samples in large-scale and MS-driven untargeted metabolomic studies of humans. Bioanalysis, 4, 2249–2264.
Fallah, A., Pierre, R., Abed, E., & Moreau, R. (2013). Lysophosphatidylcholine-induced cytotoxicity in osteoblast-like MG-63 cells: Involvement of transient receptor potential vanilloid 2 (TRPV2) channels. Molecular Membrane Biology, 30, 315.
Farooqui, A. A., Horrocks, L. A., & Farooqui, T. (2007). Interactions between neural membrane glycerophospholipid and sphingolipid mediators: A recipe for neural cell survival or suicide. Journal of Neuroscience Research, 85, 1834–1850. doi:10.1002/jnr.21268.
Floerkemeier, T., et al. (2011). Core decompression and osteonecrosis intervention rod in osteonecrosis of the femoral head: Clinical outcome and finite element analysis. International Orthopaedics, 35, 1461–1466. doi:10.1007/s00264-010-1138-x.
Fuchs, B., Schiller, J., & Cross, M. A. (2007). Apoptosis-associated changes in the glycerophospholipid composition of hematopoietic progenitor cells monitored by 31P NMR spectroscopy and MALDI-TOF mass spectrometry. Chemistry and Physics of Lipids, 150, 229–238. doi:10.1016/j.chemphyslip.2007.08.005.
Gangji, V., Hauzeur, J. P., Matos, C., De Maertelaer, V., Toungouz, M., & Lambermont, M. (2004). Treatment of osteonecrosis of the femoral head with implantation of autologous bone-marrow cells. A pilot study. The Journal of Bone and Joint Surgery. American Volume, 86-a, 1153–1160.
Gao, K., et al. (2016). Doses Lactobacillus reuteri depend on adhesive ability to modulate the intestinal immune response and metabolism in mice challenged with lipopolysaccharide. Scientific Reports, 6, 28332. doi:10.1038/srep28332.
Kasten, P., Beyen, I., Bormann, D., Luginbuhl, R., Ploger, F., & Richter, W. (2010). The effect of two point mutations in GDF-5 on ectopic bone formation in a beta-tricalciumphosphate scaffold. Biomaterials, 31, 3878–3884. doi:10.1016/j.biomaterials.2010.01.109.
Lee, C., et al. (2006). Secretory phospholipase A2 induces apoptosis through TNF-alpha and cytochrome c-mediated caspase cascade in murine macrophage RAW 264.7 cells. European Journal of Pharmacology, 536, 47–53. doi:10.1016/j.ejphar.2006.02.043.
Liang, T., Meng, T., Wang, S., Qin, C., & Lu, Y. (2016). The LPV motif is essential for the efficient export of secretory DMP1 from the endoplasmic reticulum. Journal of Cellular Physiology, 231, 1468–1475. doi:10.1002/jcp.25265.
Lin, L., et al. (2016). In vivo HMRS and lipidomic profiling reveals comprehensive changes of hippocampal metabolism during aging in mice. Biochemical and Biophysical Research Communications, 470, 9–14. doi:10.1016/j.bbrc.2015.12.009.
Liu, Y., et al. (2007). The orphan receptor tyrosine kinase Ror2 promotes osteoblast differentiation and enhances ex vivo bone formation. Molecular Endocrinology (Baltimore, Md.), 21, 376–387. doi:10.1210/me.2006-0342.
Mochida, Y., Kaku, M., Yoshida, K., Katafuchi, M., Atsawasuwan, P., & Yamauchi, M. (2011). Podocan-like protein: A novel small leucine-rich repeat matrix protein in bone. Biochemical and Biophysical Research Communications, 410, 333–338. doi:10.1016/j.bbrc.2011.05.150.
Mont, M. A., Jones, L. C., & Hungerford, D. S. (2006). Nontraumatic osteonecrosis of the femoral head: Ten years later. Journal of Bone & Joint Surgery American, 88, 1117–1132.
Mont, M. A., Zywiel, M. G., Marker, D. R., McGrath, M. S., & Delanois, R. E. (2010). The natural history of untreated asymptomatic osteonecrosis of the femoral head: A systematic literature review. The Journal of Bone and Joint Surgery. American Volume, 92, 2165–2170. doi:10.2106/jbjs.i.00575.
Pallu, S., et al. (2012). Synchrotron ultraviolet microspectroscopy on rat cortical bone: Involvement of tyrosine and tryptophan in the osteocyte and its environment. PLoS ONE, 7, e43930. doi:10.1371/journal.pone.0043930.
Pastor, I. J., Laso, F. J., Ines, S., Marcos, M., & Gonzalez-Sarmiento, R. (2009). Genetic association between -93A/G polymorphism in the Fyn kinase gene and alcohol dependence in Spanish men. European Psychiatry: The Journal of the Association of European Psychiatrists, 24, 191–194. doi:10.1016/j.eurpsy.2008.08.007.
Peterson, C. T., et al. (2016). Identification of altered metabolomic profiles following a panchakarma-based ayurvedic intervention in healthy subjects: The self-directed biological transformation initiative (SBTI). Scientific Reports, 6, 32609. doi:10.1038/srep32609.
Pierce, T. P., Jauregui, J. J., Cherian, J. J., Elmallah, R. K., & Mont, M. A. (2015). Imaging evaluation of patients with osteonecrosis of the femoral head. Current Reviews in Musculoskeletal Medicine, 8, 221–227. doi:10.1007/s12178-015-9279-6.
Rao, S., et al. (2016). Early lipid changes in acute kidney injury using SWATH lipidomics coupled with MALDI tissue imaging. American Journal of Physiology Renal Physiology, 310, F1136–F1147 doi:10.1152/ajprenal.00100.2016.
RoyChoudhury, S., et al. (2016). Serum metabolomics of Indian women with polycystic ovary syndrome using 1 H NMR coupled with a pattern recognition approach. Molecular Biosystems. doi:10.1039/c6mb00420b.
Schinke, T., et al. (2008). The protein tyrosine phosphatase Rptpzeta is expressed in differentiated osteoblasts and affects bone formation in mice. Bone, 42, 524–534. doi:10.1016/j.bone.2007.11.009.
Schumann, G., et al. (2003). Analysis of genetic variations of protein tyrosine kinase fyn and their association with alcohol dependence in two independent cohorts. Biological Psychiatry, 54, 1422–1426.
Sugano, N., et al. (1999). Diagnostic criteria for non-traumatic osteonecrosis of the femoral head. A multicentre study. Acoustics Speech & Signal Processing Newsletter IEEE, 81, 590–595.
Sugars, R. V., Olsson, M. L., Marchner, S., Hultenby, K., & Wendel, M. (2013). The glycosylation profile of osteoadherin alters during endochondral bone formation. Bone, 53, 459–467. doi:10.1016/j.bone.2013.01.022.
Tan, B., et al. (2013). Metabonomics identifies serum metabolite markers of colorectal cancer. Journal of Proteome Research, 12, 3000–3009. doi:10.1021/pr400337b.
Tan, X., et al. (2006). Comparative analysis of serum proteomes: Discovery of proteins associated with osteonecrosis of the femoral head. Translational Research: The Journal of Laboratory and Clinical Medicine, 148, 114–119. doi:10.1016/j.trsl.2006.05.001.
Toyosawa, S., et al. (2001). Dentin matrix protein 1 is predominantly expressed in chicken and rat osteocytes but not in osteoblasts. Journal of Bone and Mineral Research: The Official Journal of the American Society for Bone and Mineral Research, 16, 2017–2026. doi:10.1359/jbmr.2001.16.11.2017.
Triba, M. N., et al. (2015). PLS/OPLS models in metabolomics: The impact of permutation of dataset rows on the K-fold cross-validation quality parameters. Molecular Biosystems, 11, 13–19.
Vashi, N., et al. (2016). Genetic markers of inflammation may not contribute to metabolic traits in Mexican children. PeerJ, 4, e2090. doi:10.7717/peerj.2090.
Wu, R. W., Wang, F. S., Ko, J. Y., Wang, C. J., & Wu, S. L. (2008). Comparative serum proteome expression of osteonecrosis of the femoral head in adults. Bone, 43, 561–566.
Zafeiridis, A., et al. (2016). Global metabolic stress of isoeffort continuous and high intensity interval aerobic exercise: A comparative 1 H NMR metabonomic study. Journal of Proteome Research. doi:10.1021/acs.jproteome.6b00545.
Zalavras, C. G., & Lieberman, J. R. (2014). Osteonecrosis of the femoral head: Evaluation and treatment. The Journal of the American Academy of Orthopaedic Surgeons, 22, 455–464. doi:10.5435/jaaos-22-07-455.
Zhao, D., et al. (2012). Treatment of early stage osteonecrosis of the femoral head with autologous implantation of bone marrow-derived and cultured mesenchymal stem cells. Bone, 50, 325–330. doi:10.1016/j.bone.2011.11.002.
Zhao, T., et al. (2009). Trace element profiling using inductively coupled plasma mass spectrometry and its application in an osteoarthritis study. Analytical Chemistry, 81, 3683–3692. doi:10.1021/ac900311q.
Zhao, Y. Y., et al. (2012). Serum metabonomics study of adenine-induced chronic renal failure in rats by ultra performance liquid chromatography coupled with quadrupole time-of-flight mass spectrometry. Biomarkers: Biochemical Indicators of Exposure, Response, and Susceptibility to Chemicals, 17, 48–55. doi:10.3109/1354750x.2011.637180.
Zhu, W., et al. (2016). Metabolomic study of the bone trabecula of osteonecrosis femoral head patients based on UPLC–MS/MS. Metabolomics, 12, 1–14.
Acknowledgements
This work was funded by National Natural Science Foundation of China (Grant No. 89011060), and with the help of Department of Orthopaedics of the First Affiliated Hospital of Chongqing Medical University and Department of Life Science of Chongqing Medical University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures associated with involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consents were obtained from all participants.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xu, Z., Xu, K., Ding, S. et al. Serum metabolomic study for detecting biomarkers of non-traumatic osteonecrosis of the femoral head. Metabolomics 13, 73 (2017). https://doi.org/10.1007/s11306-017-1208-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11306-017-1208-9